Abstract
Background
Many studies have linked weather to mortality; however, role of such critical factors as regional variation, susceptible populations, and acclimatization remain unresolved.
Methods
We applied time-series models to 107 US communities allowing a nonlinear relationship between temperature and mortality by using a 14-year dataset. Second-stage analysis was used to relate cold, heat, and heat wave effect estimates to community-specific variables. We considered exposure timeframe, susceptibility, age, cause of death, and confounding from pollutants. Heat waves were modeled with varying intensity and duration.
Results
Heat-related mortality was most associated with a shorter lag (average of same day and previous day), with an overall increase of 3.0% (95% posterior interval: 2.4%–3.6%) in mortality risk comparing the 99th and 90th percentile temperatures for the community. Cold-related mortality was most associated with a longer lag (average of current day up to 25 days previous), with a 4.2% (3.2%–5.3%) increase in risk comparing the first and 10th percentile temperatures for the community. Mortality risk increased with the intensity or duration of heat waves. Spatial heterogeneity in effects indicates that weather–mortality relationships from 1 community may not be applicable in another. Larger spatial heterogeneity for absolute temperature estimates (comparing risk at specific temperatures) than for relative temperature estimates (comparing risk at community-specific temperature percentiles) provides evidence for acclimatization. We identified susceptibility based on age, socioeconomic conditions, urbanicity, and central air conditioning.
Conclusions
Acclimatization, individual susceptibility, and community characteristics all affect heat-related effects on mortality.
Several studies have identified associations between mortality and temperature, identifying nonlinear J- or U-shaped relationships.1–11 Extreme events such as the 2003 European heatwave12,13 and concern regarding climate change have increased interest in the impact of weather on health. Most previous work has investigated a single city or a small number of cities; however, several multicity US studies have been conducted, including investigations of cardiovascular mortality for the elderly in 107 communities,1 effect modification in 7 cities,2 and effect modification of ozone on cardiovascular mortality for 95 cities.3 Study designs vary widely. For example, research on 50 US cities evaluated effects above or below a specified temperature,4,5 whereas a study of 11 eastern US cities estimated the nonlinear response across the entire temperature range.6 The relationship seems to vary by region, with an 11-city study identifying higher heat effects in the northeast with lower or negligible effects in the southeast.6 Several studies have indicated variation in effects by race, education level, population density, and air conditioning (AC).2,4,5,14 European studies found that cold effects occur up to 2 weeks after exposure15,16; however, to date large multicity US studies have applied short-term lags of 6 days or less.1,3–5,7,10,11
A better understanding of how temperature affects mortality and susceptible populations is crucial not only to the medical community, but to policymakers and community leaders who develop intervention strategies for temperature extremes. Weather mortality relationships and variation by region and populations are likely to be of growing importance as climate change is anticipated to alter temperature patterns, possibly including increased frequency and magnitude of heat waves.17
This study analyzes temperature-related mortality for 107 US communities, considering exposure timeframes, heat waves, cause of death, age, susceptible populations, regional variation, acclimatization, and air pollution. Ozone is of particular importance given its formation’s temperature de-pendence.18 We estimated community-specific nonlinear exposure–response curves and combined estimates accounting for their statistical uncertainty to generate national effects.
METHODS
Data
The study includes 107 urban communities for 1987–2000. Each community is a county or set of adjacent counties. Mortality, weather, and pollution data were based on the publicly available National Morbidity, Mortality, and Air Pollution Study,19 originally obtained from the National Center for Health Statistics, National Climatic Data Center, and US Environmental Protection Agency.19
Daily mortality excluded nonresidents and deaths from injuries and external causes (International Classification of Diseases, Ninth Revision (ICD-9) Codes 800 and above, ICD-10 Codes S and above). Mortality counts were stratified by cause as cardiovascular (ICD-9 codes 390 – 448) and respiratory (ICD-9 codes 480 – 486, 490 – 497, or 507) and age (<65, 65–74, ≥75 years).
Weather variables were community-specific daily mean, maximum, and minimum temperature, and mean apparent temperature. Dew point temperature was adjusted for mean daily temperature to avoid collinearity.20 Days missing weather data (<2.5% of total days) were excluded.
Daily community-specific concentrations of ozone and particulate matter with aerodynamic diameter <10 μm (PM10) were available for 97 and 101 communities, respectively. In some communities ozone was measured only during the warm season (eg, April–October). In most communities PM10 was measured every 6 days.
Community-level variables (income, unemployment, education, public transportation, race, urbanicity, and population) were estimated by weighted combination of 1990 and 2000 US census values.21 Data on central AC, available for 53 communities, was obtained from the American Housing Survey.22
Analysis of Temperature–Mortality Relationships
Within each community, the relationship between daily mortality and temperature was estimated using an overdispersed Poisson generalized additive model:
| (1) |
where = expected mortality rate for community c on day t; β0 = model intercept; yc = vector of regression coefficients for day of the week for community c; DOWt = categorical variable for day of the week; ns (timet) = natural cubic spline of time, with 7 degrees of freedom (df) per year; ns(Tclag) = natural cubic spline of a temperature metric for community c for a specific lag from day t, with 3 df and knots at quantiles; ns(Dct) = natural cubic spline of adjusted dew point temperature for community c on day t, with 3 df.
This approach was originally developed to study air pollution20,23 and temperature for 11 eastern US communities.6 We assessed several temperature metrics: daily average, minimum, and maximum temperature, and apparent temperature,24 which incorporates humidity (in this case, adjusted dew point temperature was omitted).
We estimated community-specific temperature–mortality response curves and summary measures of the heat- and cold-related portions of this relationship by estimating effects of relative and absolute temperature changes. To quantify effects of relative temperature changes, we calculated the change in mortality risk comparing the 1st to 10th percentile (cold effect) and the 99th to 90th percentile (hot effect) of the community’s temperature distribution. To quantify effects of absolute temperature changes, we calculated the change in mortality risk at 80°F (26.7°C) compared with 60°F (15.6°C) (heat effect) and at 40°F (4.4°C) compared with 60°F (cold effect) for all communities with temperature data available in this range (101 communities for hot effects; 80 for cold effects). These temperatures (40°F, 60°F, and 80°F) approximate the average 10th, 50th, and 90th percentiles of mean daily temperature across communities. Heat and cold effects were modeled separately. These effects reflect a portion of the overall exposure–response curve and are a possible estimation of the heat and cold effect estimates that could be taken from the nonlinear temperature-mortality curves.
We used sensitivity analyses to examine inclusion of same-day ozone and previous-day PM10. Pollutant lag structures were chosen as the single-day lag with the strongest mortality association based on earlier research.20,25 We tested robustness of results to the df for temporal splines (4, 7, and 14 df/y).
Heat waves were categorized by intensity and duration following methods developed to study 3 European cities.26 This approach considers 6 heat wave types: periods of 2 or more or 4 or more days of continuous temperatures more than 98.5th, 99th, or 99.5th percentile of the community’s temperature distribution. For 2-day heat wave definitions, we compared mortality on the second and later days of a heat wave to non-heat wave days; for the 4-day definitions, we compared mortality on the fourth and later days of a heat wave to nonheat-wave days. For all heat-wave analysis, models included control for lag 0–1 temperature.
Community-specific estimates of absolute and relative heat and cold effects and heat wave effects were combined to generate national and regional estimates using a Bayesian hierarchical model, as in earlier studies.20 Regional estimates were calculated for 7 regions (industrial midwest, northeast, northwest, southern California, southeast, southwest, and upper midwest).1 We used 2-Level Normal Independent Sampling Estimation with noninformative priors (Jeffreys prior).27,28
| (2) |
| (3) |
where β̂c = estimated effect of temperature on mortality in community c; β̂c = true effect of temperature on mortality in community c; v̂c = statistical variance of β̂c; μ = true average effect across all communities; τ2 = between-community variance of the true effect; n = number of communities.
Second-stage analysis evaluated whether community-specific variables (mean yearly and seasonal temperature and unadjusted dew point temperature) modified community-specific temperature-mortality effects.
| (4) |
where = community-level variable j for community c: x̄j = mean community-level variable j across communities; α0 = average ln(relative rate) when ; α1,j = change in ln(relative rate) for unit increase in ( ).
Similar analysis examined how community-specific variables affect ozone mortality effects.29
Equation 4 was used to explore sensitivity of subpopulations by race, socioeconomics, urbanicity, and AC prevalence. We applied stratified models (Equations 2 and 3) to explore susceptibility by age and cause of death (respiratory, cardiovascular, and noncardiorespiratory). All analysis was performed in R-2.6.2.
RESULTS
Weather and mortality summary statistics are provided in eTable 1 and distributions in eFigure 1 in the supplemental material (http://links.lww.com/A720). We first calculated relative effects with each temperature metric: minimum, maximum, and mean temperature, and apparent temperature (eFig. 2, http://links.lww.com/A720). All metrics were strongly correlated (eTable 2, http://links.lww.com/A720). Mean daily temperature and apparent temperature estimates were similar. Mean daily temperature was chosen for subsequent analysis given its high correlation to other metrics as this measure provides more easily interpreted results in a policy context.
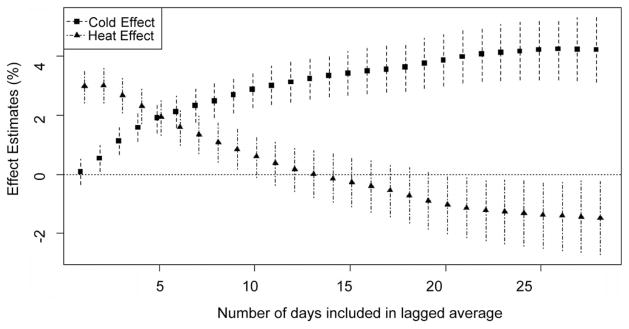
We considered lag structures of the same day and the average of the same day and up to 28 days previous. Figure 1 presents relative effect estimates and shows how this estimate changes as more days of lagged temperature are included. First the relative effects were calculated separately for each community and then combined to generate an overall effect. Although Figure 1 shows the effect of lag structure on national heat and cold effects, the lag with the strongest effect varied by community. eFigure 3 (http://links.lww.com/A720) shows these effects for the 4 largest communities. The association of heat with mortality was limited to recent days of exposure and estimates declined when longer time periods were considered. For cold-related mortality a longer exposure time-frame is relevant. Results indicate that use of identical exposure timeframes for heat and cold response is inappropriate. For subsequent analysis, we estimated heat-related mortality based on the same and previous day (Tlag0–1), and cold-related mortality based on the same day and past 25 days (Tlag0–25).
FIGURE 1.
Risk of mortality for heat (comparison of 99th vs. 90th percentile of mean temperature) and cold (comparison first vs. 10th percentile of mean temperature) for different lag structures. Points show central estimates and the vertical lines show 95% posterior intervals.
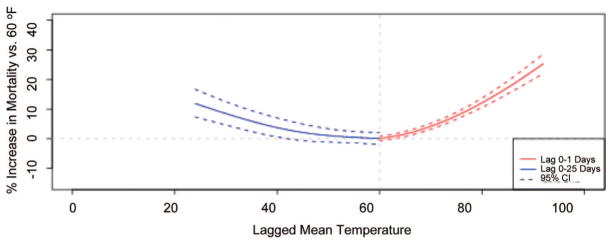
Based on the selected temperature metric and lag structures, we generated community-specific exposure–response curves. Figure 2 and eFigure 4 (http://links.lww.com/A720) provide an example, displayed as the increase in mortality risk for a given temperature (x-axis) compared with a reference temperature (60°F). eFigure 4A (http://links.lww.com/A720) shows results for a shorter exposure period (Tlag0–1), capturing the heat effect, and eFigure 4B (http://links.lww.com/A720) for a longer lag (Tlag0–25), capturing the cold effect. Figure 2 combines the heat- and cold-related portions of eFigures 4A and 4B (http://links.lww.com/A720), respectively. eFigure 5 (http://links.lww.com/A720) provides examples of other locations. This representation better captures weather-related mortality than previous research that used equal lag structures for cold and heat effects.
FIGURE 2.
Relationship between temperature and risk of mortality, comparing various temperature levels with a reference temperature of 60°F for New York City.
Slopes of exposure–response curves were summarized by comparing the risk of relative and absolute temperature changes. eFigure 6 (http://links.lww.com/A720) shows relative cold and heat effects for each community and the national effect, and eFigure 7 (http://links.lww.com/A720) provides absolute effects. The overall increase in mortality risk comparing the first and 10th percentile Tlag0–25 was 4.2% (95% posterior interval = 3.2%–5.3%). Mortality risk increased 3.0% (2.4%–3.6%) comparing the 99th and 90th percentile Tlag0–1. Results were robust to the degrees of freedom used in time splines (eTable 3, http://links.lww.com/A720). For absolute temperature changes, mortality risk at 60°F was 5.2% (3.8%–6.6%) lower than at 40°F for Tlag0–25 and 4.9% (3.8%–6.0%) lower than at 80°F for Tlag0–1.
We repeated analysis with inclusion of ozone or PM10 (Table 1 and eTable 4, http://links.lww.com/A720). A smaller dataset is available for this analysis due to the lack of pollution data for some communities and the frequency of pollution measurement. Cold effects were similar with pollution adjustment, whereas heat effects were slightly lower. eFigure 8 shows community-specific and overall results of pollution sensitivity analysis for relative heat effects (http://links.lww.com/A720).
TABLE 1.
Sensitivity of Relative Heat and Cold Effects to Inclusion of Pollution Variables in the Temperature–Mortality Model
| Pollutant Adjustment | Heat Effect
|
Cold Effect
|
||||
|---|---|---|---|---|---|---|
| Estimate % | 95% PI | No. Communities | Estimate % | 95% PI | No. Communities | |
| Without PM10 | 3.7 | 2.6–4.7 | 63 | 4.7 | 2.6–6.8 | 63 |
| With PM10 | 3.2 | 2.1–4.4 | 4.5 | 2.4–6.7 | ||
| Without O3 | 3.5 | 2.8–4.2 | 87 | 4.3 | 3.0–5.6 | 87 |
| With O3 | 3.2 | 2.5–3.9 | 4.3 | 3.0–5.7 | ||
Results without pollution adjustment include only days and communities with pollution data available. Ozone is at lag 0 days; PM10 is at lag 1 day.
PI indicates posterior interval.
eTable 5 (http://links.lww.com/A720) shows summary statistics for the occurrence of heat waves in this study. Table 2 presents results from the heat-wave analysis. Some communities had no heat waves of a specific definition and were thereby excluded from analysis. Mortality effects increased with intensity or duration of the heat wave. As previous research found lower heat-wave effects when longer lags were used for temperature control,26 we recalculated results with lag 0 to 2 temperature control (eTable 6, http://links.lww.com/A720). Effect estimates were very similar using this model structure.
TABLE 2.
Increased Risk of Mortality for Later Days of a Heat-Wave Event Compared With Non-Heat-Wave Days Under Different Heat Wave Definitions
| Intensity | Duration
|
|||||
|---|---|---|---|---|---|---|
| ≥2 Days
|
≥4 Days
|
|||||
| Estimate % | 95% PI | No. Communities | Estimate % | 95% PI | No. Communities | |
| ≥98th percentile | 3.2 | 2.1–4.3 | 107 | 3.9 | 2.1–6.0 | 107 |
| ≥99th percentile | 4.3 | 2.7–5.9 | 107 | 6.5 | 2.7–10.5 | 105 |
| ≥99.5th percentile | 6.1 | 4.0–8.2 | 107 | 10.6 | 6.1–15.3 | 81 |
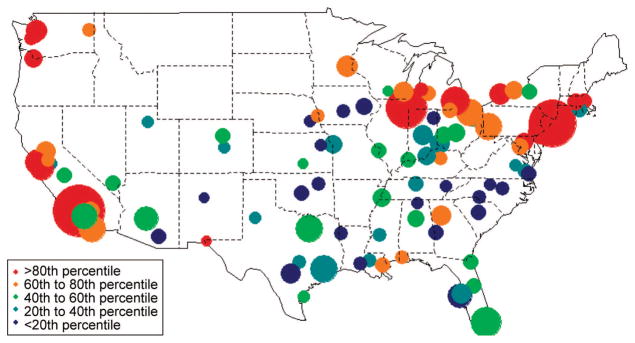
Geographic distributions of heat and cold effects for relative (comparing risk across temperature percentiles) and absolute (comparing risk at specific temperatures) effects are shown in Figure 3 and eFigure 9 (http://links.lww.com/A720). Cold effects appear to be larger in the South than in the north (eFigs. 9A, B, http://links.lww.com/A720). Conversely, heat effects generally appear larger in the north (Fig. 3 and eFig. 9C, http://links.lww.com/A720). Heat wave and heat effects showed similar geographic patterns (eFig. 10, http://links.lww.com/A720). Spatial variation was also demonstrated by regional estimates (eFig. 11, http://links.lww.com/A720). Cold effects were more similar across regions than heat effects. Regional trends are more defined for absolute rather than relative effects (Fig. 3 and eFigs. 9, 11, http://links.lww.com/A720), which could indicate that populations acclimate to a city’s weather conditions, especially heat.
FIGURE 3.
Map of the relative heat effect (percentage increase in mortality risk comparing 99th and 90th percentiles of Tlag0–1). The color of each community corresponds to the level of the estimate; the size of the circle corresponds to the inverse of the variance of the estimate (ie, larger circles are more certain). The 2 noncontinental cities included in the dataset, Honolulu HI and Anchorage AK, are not included in this regional analysis.
We evaluated whether variation in community-specific effects could be explained by long-term average temperature and dew point temperature (Table 3). Heat effects were higher in colder communities and cold effects higher in warmer communities, consistent with the observed regional patterns. For example, a 12.9°F increase in long-term temperature was associated with a 70% decrease in absolute heat effects and a 94% increase in absolute cold effects.
TABLE 3.
Increase in Heat- and Cold-Related Mortality Effect Estimates Per Interquartile (IQR) Increase in a Community-Specific Weather-Related Characteristic
| Community-specific Variable | IQR (°F) | Change in Relative Effect (%)
|
Change in Absolute Effect (%)
|
Change in Heat Wave Effect (%) | ||
|---|---|---|---|---|---|---|
| Heat | Cold | Heat | Cold | |||
| Yearly temperature | 12.9 | −39.6a | 27.0 | −69.5a | 94.0a | −45.0c |
| Summer temperature | 9.2 | −69.4a | −112.2a | −24.0 | ||
| Winter temperature | 17.7 | 27.2 | 98.0a | |||
| Dew point temperature | 9.4 | −24.0b | 27.0c | −43.2a | 86.0a | −18.1 |
| Summer dew point temperature | 8.4 | −44.4a | −59.1a | 2.7 | ||
| Winter dew point temperature | 17.5 | 34.4c | 117a | |||
Significant at P < 0.01.
Significant at P < 0.05.
Significant at P < 0.10.
The values reflect the percentage increase in each specific heat or cold effect metric for an interquartile change in the specified long-term community-specific variable.
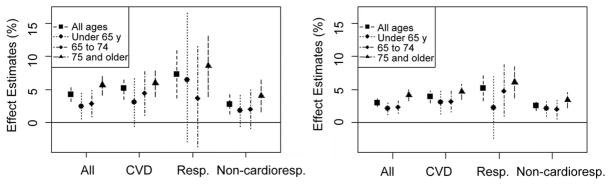
Figure 4 shows relative cold and heat effects, stratified by age and cause. Respiratory mortality effects were generally higher than cardiovascular effects. Results also indicate associations for noncardiorespiratory mortality. Heat and cold effects were highest for the oldest age category (≥75 years) for all causes; however, associations were also observed for youngest age group (<65).
FIGURE 4.
Percentage increase in mortality risk for the relative cold effect (comparison of the 1st to 10th percentile temperature) (A), and heat effect (comparison of the 99th to the 90th percentile temperature) (B), by cause and age. The point represents the central estimates; the vertical lines represent 95% posterior intervals.
Heat wave effects were estimated by age and cause of death with the heat-wave definition as temperatures at the 99.5th percentile or higher and 2 days duration or longer (Table 4). Heat waves had effects on all age groups, with the largest effect for the oldest group, and for cardiovascular and noncardiorespiratory deaths, with the highest estimate for cardiovascular deaths. Results indicate an association between heat waves and respiratory mortality, although estimates are uncertain.
TABLE 4.
Percentage Increase in Mortality Risk for Heat Wave Days Compared With Non-Heat Wave Days by Age and Cause of Death
| Heat Wave Coefficient
|
||
|---|---|---|
| Estimate (%) | 95% PI | |
| Age group (yr) | ||
| <65 | 5.1 | 2.0 to 8.4 |
| 65–74 | 5.0 | 2.0 to 8.2 |
| ≥75 | 8.2 | 5.3 to 11.3 |
| Cause of death | ||
| Cardiovascular | 8.8 | 5.5 to 12.2 |
| Respiratory | 5.9 | −0.1 to 12.2 |
| Noncardiorespiratory | 5.5 | 3.2 to 7.9 |
These heat wave effects were estimated based on the heat wave definition of temperatures ≥99.5th percentile for ≥2 days.
To investigate sensitive subpopulations, we explored the relationship between community-specific weather-mortality effects and various community-specific indicators (Table 5). Many of these community-level variables were correlated (eTable 7, http://links.lww.com/A720). Communities with higher income, unemployment, population, and urbanicity were more susceptible to heat impacts. Higher susceptibility to cold was identified for communities with a higher percentage of African Americans. A higher fraction of homes with central AC was associated with lower heat-related and higher cold-related mortality risk. Results for the 65 years and older age category were similar to results for all ages (eTables 8, 9, http://links.lww.com/A720).
TABLE 5.
Increase in Heat- and Cold-Related Mortality Per IQR Increase in Community-Specific Socioeconomic and Other Selected Community Characteristics
| Community-Specific Variable | IQR | Change in Relative Effect (%)
|
Change in Absolute Effect (%)
|
Change in Heat Wave Effect (%)
|
||
|---|---|---|---|---|---|---|
| Heat | Cold | Heat | Cold | |||
| Median household income | $6,538 | 35.1a | 2.6 | 56.7a | −6.7 | −30.1 |
| Unemployed | 1.7% | 29.1b | 9.1 | 17.6 | 11.7 | 45.0b |
| Population without high school degree | 7.7% | −18.0 | −15.3 | −13.7 | −14.5 | −36.2 |
| Public transportation commuters | 3.3% | 11.1a | 0.5 | 15.7a | −0.04 | 11.7c |
| Black/African American | 18.0% | −1.2 | 10.6 | −15.7 | 29.7c | 40.3c |
| Living in urban setting | 10.6% | 22.6b | 18.8 | 17.4 | 6.7 | 34.6c |
| Population | 580,599 | 8.4a | 0.6 | 14.4a | −0.2 | 6.0 |
| Central AC | 47.1% | −87.7a | 10.2 | −110a | 72.8b | 6.7 |
Significant at P < 0.01.
Significant at P < 0.05.
Significant at P < 0.10.
The values reflect the percent increase in each specific heat or cold effect metric for an interquartile change in the specified long-term community-specific variable.
DISCUSSION
A variety of modeling decisions are made when estimating the impact of weather on mortality, including the shape of the exposure–response curve, lag structure, and temperature metric. These choices affect results and comparability across studies. Earlier work investigated several exposure–response forms, such as the temperature of lowest mortality risk (minimum mortality temperature) and constant linear relationships above (heat slope) and below (cold slope) the minimum mortality temperature,6 generating a V-shaped exposure–response curve. Although useful, these methods do not fully capture the nonlinear association and are problematic for comparing across cities, for example, a comparison of a heat slope calculated for higher than 80°F versus a slope calculated for higher than 90°F. Other studies estimated constant slopes above and below city-specific threshold hot and cold temperatures.10,11,16 When comparing communities with disparate climates, this method forces a V-shaped model that may not reflect actual temperature-mortality relationships in each community.
Our spline approach allows estimation of nonlinear relationships without forcing constant slopes for specific temperature ranges or similarities among communities. Similar methods were applied in a study of 7 US cities.2 For most communities the difference in mortality risk per unit temperature decrease was fairly consistent across mild cold temperatures; however, the heat effect per unit temperature increase rose significantly at higher temperatures. Furthermore, some communities did not have a unique minimum mortality temperature. Slope approximations based on specified temperatures (eg, our absolute estimates) are useful to summarize and compare temperature-response relationships, but interpretation of results should consider that such methods reflect only a portion of the nonlinear relationship. Although the heat and cold effects generated in this study summarize only part of the temperature–mortality relationship, these methods were particularly appropriate for studying such a large range of climates. Complex nonlinear functions such as those used here and in previous studies may provide a more complete assessment of temperature and mortality risk.8,15
Previous studies of weather and mortality have used a variety of temperature measurements. Several studies have recommended apparent temperature or humidex24 because these measures incorporate humidity; others suggested minimum temperature.11 We applied minimum, maximum, and mean daily temperature, and mean daily apparent temperature, and identified heat and cold effects for all metrics. Apparent temperature effects were nearly identical to those of mean daily temperature adjusted for humidity. Heat effects were highest for mean daily temperature. A multicity European study similarly found that mean daily temperature was consistently the strongest predictor of mortality from heat and heat waves,26 compared with daily minimum, maximum, and apparent temperature. Although some differences in estimates may occur, our findings indicate that the various temperature metrics are likely to produce similar results.
We investigated lag times from same day to 28 days previous. Earlier heat-mortality studies identified risk from recent exposure (ie, same day and a few days previous).5–8,11,16 Most studies applied lags of 1 or 2 days, although some used up to 3 days.30 We found the strongest heat-related mortality association for same- and previous-day exposure. The short lag required to capture the effects of heat on mortality suggests a rapid physical response. Some of the effects observed could be the result of short-term mortality displacement, and further study is warranted.
For cold-related mortality, most US studies applied 2- to 5-day lags,1,5,6,11 whereas other researchers found cold effects after 1 or more weeks for some communities.16,31 Findings indicate that longer lags are required to capture cold’s impact on mortality and that using identical lag structures for cold and heat effects is not appropriate. A limitation of longer lag structures is the introduction of more measurement error due to increased time between the exposure and event. Heat and cold effects were similar in magnitude for absolute and relative estimates, which contrasts with earlier US studies finding larger heat effects than cold effects.5,11 We hypothesize that previous studies underestimated cold-related effects through use of shorter lags. Results agree with a European study finding mortality effects occurring days to weeks after cold exposure.16 Findings suggest that cold temperatures more indirectly affect mortality than heat. Infectious diseases, which are more common in industrialized countries during colder weather (when people spend more time indoors and in proximity) could account for much of the cold-related effect. Although we found that heat effects were impacted by shorter exposures and cold effects were affected by longer exposures, the specific lag structures used here (Tlag0–25 and Tlag0–1) are intended to be representative, not to reflect the only or the exact lag measurements appropriate for temperature-mortality studies.
We took several approaches to comparing temperature effects across communities, including estimates based on each community’s temperature distribution, allowing comparison despite the wide climatic range. Studies of 2 Euro-pean,16 2 Mexican,30 and 50 US5 cities similarly estimated mortality risk for community-specific temperature quantiles. We also calculated the effect of a change in absolute temperature, from a relatively mild (60°F) to hot (80°F) or cold (40°F) temperatures. These 2 types of effect estimates have different interpretations with respect to acclimatization, an important consideration for climate-change studies and public health policy. Acclimatization can occur through physical adaptation, housing characteristics, or behavioral patterns (eg, staying indoors, clothing). With a high degree of acclimatization to weather, results would be similar across communities for relative temperature effects and different for absolute effects. Without a high degree of acclimatization, communities would have similar absolute effects and dissimilar relative effects. Although both absolute and relative temperature effect estimates showed variation across communities, absolute estimates exhibited larger variation, which implies some degree of acclimatization to weather conditions because a given temperature has different impact depending on location. Previous studies have also found some evidence of acclimatization.5,6
Heat effects were generally lower in communities with higher long-term temperatures. This supports the hypothesis that communities and individuals adapt, to some extent, to weather even during temperatures that are extremely warm for that area. Conversely, absolute cold effects were markedly higher in communities with higher temperatures, as observed previously in other areas.32,33 However, a similar association was not observed for relative cold effects. This indicates that those in colder cities seem to acclimatize to some degree, so they are less affected by temperatures of 40°F, but not to the extent of lessening effects at temperatures extremely cold for the community.
Most previous heat wave studies have analyzed specific extreme events (eg, Chicago 199534 or European 200312,13 heat waves). Fewer studies have considered more frequent, less severe heat waves. Our findings suggest that sustained periods of extreme heat present an elevated risk over single days of high temperatures, even if the heat wave period is as short as 2 days, and that duration and intensity of the heat wave affect mortality risk. Future studies might consider separate effects by heat wave duration, intensity, or time of occurrence during the summer.
We identified spatial heterogeneity in heat and cold effects, consistent with other US studies1,2,5–8,10,11 with larger cold effects in the southern US and smaller effects in the north.6,11 Similar to previous research,7,11 we found negligible or null effects for heat in many southeastern communities. Results emphasize the need for multicity studies because results from 1 location may not be applicable elsewhere.
Heat effects were slightly lowered when models included O3 and PM10. Cold effects were essentially unchanged. In previous studies, temperature–mortality results were also robust to particles2,16,26,30 and ozone.5,26,30,35 Earlier research found ozone-mortality associations were robust to control for temperature.20 Findings of previous studies and our work imply separate and substantial mortality effects from temperature and from air pollution; however, some studies suggest possible interaction between temperature and air pollution.3,36 Observed associations between weather and noncardiorespiratory deaths indicate that weather affects mortality beyond cardiorespiratory responses. Estimates were somewhat higher for cardiovascular and respiratory deaths, especially respiratory, compared with total deaths, consistent with earlier studies.5,37
We found higher susceptibility for older populations; however, other age categories were also subject to temperature–mortality risk. Results from stratifying effect estimates by age were consistent with earlier results based on community-level and individual-level data.11,34,37,38
We found differences in susceptibility related to socioeconomic factors and urbanicity. Previous studies also found community-level socioeconomic factors to explain some variability in communities’ heat effects.6,10 This may reflect baseline health and nutrition status, access to health care, and ability to respond to extreme conditions (eg, AC). Susceptibility by urbanicity may relate to urban-heat-island effects or housing conditions. We found that heat has a lower mortality impact when communities have more central AC, as observed in smaller US studies.7,10,14 This adaptation strategy likely explains some of the regional variation in heat effects. Earlier work1,7 found that heat-related mortality decreased significantly in the southeastern US as AC prevalence increased. Over time, the number of cities without a heat effect has increased,7 especially where AC has reached almost universal prevalence. Heat wave effects, however, were not strongly associated with AC. It is possible that the protection afforded by AC is sufficient to reduce effects of high temperatures, but not to prevent more extreme heat wave effects. Heat effects were higher in communities with higher income. Although this relationship might seem surprising, a recent national study showed that median income is negatively associated with mortality in adults 65 years or younger but not with older individuals, which represents the majority of heat- and cold-related mortality.39
Socioeconomic factors were less important in explaining cold effects; however, communities with a higher percentage of black/African Americans had higher cold effects, although the relationship was uncertain. Earlier research also found insignificant impact of socioeconomic factors on cold effects,5,6 although 1 study found higher cold effects for communities with less education or a lower percentage of population identifying as black.2 A study of cold effects on the elderly found significant associations with poverty, income inequality, and deprivation rate.40 The lack of association in our study might relate to the use of community-level variables. Further investigation using individual-level data is needed. Such data could also improve exposure estimates, especially for longer lag structures.
These findings on the impact of weather on mortality have implications for policymakers and future scientific work. The identified susceptible subpopulations signify the need for targeted heat-mortality prevention efforts. The heterogeneous results across communities indicate the value of multicity research and indicate that approaches to prevent weather-related mortality might be most effective if they are community specific. Results on acclimatization and heat waves are of particular importance to research estimating weather-related mortality impacts from climate change.
Supplementary Material
Acknowledgments
Supported by an US EPA STAR Graduate Fellowship (91689201-0), a National Science Foundation Graduate Fellowship, the National Institute for Environmental Health Sciences (ES012054-03), and the US Environmental Protection Agency through the Johns Hopkins Particulate Matter Research Center (RD-83241701).
Footnotes
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
References
- 1.Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007;18:369–372. doi: 10.1097/01.ede.0000257515.34445.a0. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol. 2003;157:1074–1082. doi: 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]
- 3.Ren C, Williams GM, Morawska L, et al. Ozone modifies associations between temperature and cardiovascular mortality analysis of the NMMAPS data. Occup Environ Med. 2008;65:255–260. doi: 10.1136/oem.2007.033878. [DOI] [PubMed] [Google Scholar]
- 4.Medina-Ramon M, Zanobetti A, Cavanagh DP, et al. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114:1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medina-Ramon M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 US cities. Occup Environ Med. 2007;64:827–833. doi: 10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curriero FC, Heiner KS, Samet JM, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 7.Davis RE, Knappenberger PC, Michaels PJ, et al. Changing heat-related mortality in the United States. Environ Health Perspect. 2003;111:1712–1718. doi: 10.1289/ehp.6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 US cities. Environ Health Perspect. 2002;110:859–863. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- 10.Chestnut LG, Breffle WS, Smith JB, et al. Analysis of differences in hot-weather-related mortality across 44 US metropolitan areas. Environ Sci Policy. 1998;1:59–70. [Google Scholar]
- 11.Kalkstein LS, Davis RE. Weather and human mortality: an evaluation of demographic and interregional responses in the United States. Ann Assoc Am Geogr. 1989;79:44–64. [Google Scholar]
- 12.Filleul L, Cassadou S, Medina S, et al. The relation between temperature, ozone, and mortality in nine French cities during the heat wave of 2003. Environ Health Perspect. 2006;114:1344–1347. doi: 10.1289/ehp.8328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Le Tertre A, Lefranc A, Eilstein D, et al. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology. 2006;17:75–79. doi: 10.1097/01.ede.0000187650.36636.1f. [DOI] [PubMed] [Google Scholar]
- 14.O’Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US Cities: the role of air conditioning prevalence. J Urban Health. 2005;82:191–197. doi: 10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology. 2006;17:624–631. doi: 10.1097/01.ede.0000239732.50999.8f. [DOI] [PubMed] [Google Scholar]
- 16.Pattenden S, Nikiforov B, Armstrong BG. Mortality and temperature in Sofia and London. J Epidemiol Community Health. 2003;57:628–633. doi: 10.1136/jech.57.8.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Souch C, Grimmond CSB. Applied climatology: ‘heat waves’. Prog Phys Geogr. 2004;28:599–606. [Google Scholar]
- 18.Seinfeld JH, Pandis SN. Atmospheric Chemistry and Physics: From Air Pollution to Climate Change. New York: Wiley-Interscience; 1998. [Google Scholar]
- 19.Internet-based Health and Air Pollution Surveillance System (iHAPSS) [Accessed November 20, 2007];Mortality, air pollution, and meteorological data for 108 US cities 1987–2000. 2007 Available at: http://www.ihapss.jhsph.edu/H.
- 20.Bell ML, McDermott A, Zeger SL, et al. Ozone and short-term mortality in 95 US urban communities, 1987–2000. J Am Med Assoc. 2004;292:2372–2378. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Census Bureau. Census 1990, Summary File 1; Census 1990, Summary File 3; Census 2000, Summary File 1; Census 2000, Summary File 3. Washington, DC: US Census Bureau; [Google Scholar]
- 22.US Department of Commerce, US Department of Housing and Urban Development. American Housing Survey, 1989, 1991, 1993, 1994, 1997, 1999. Washington, DC: US Department of Commerce, US Department of Housing and Urban Development; [Google Scholar]
- 23.Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and repiratory diseases. J Am Med Assoc. 2006;295:1127–1134. doi: 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalkstein LS, Valimont KM. An evaluation of summer discomfort in the United States using a relative climatological index. Bull Am Meteorol Soc. 1986;67:842–848. [Google Scholar]
- 25.Samet JM, Dominici F, Zeger SL, et al. The National Morbidity, Mortality, and Air Pollution Study Part I: Methods and Methodologic Issues. Health Effects Institute; Cambridge, MA: 2000. [PubMed] [Google Scholar]
- 26.Hajat S, Armstrong B, Baccini M, et al. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology. 2006;17:632–638. doi: 10.1097/01.ede.0000239688.70829.63. [DOI] [PubMed] [Google Scholar]
- 27.Everson PJ, Morris CN. Inference for multivariate normal hierarchical models. J R Stat Soc Ser B. 2000;62:399–412. [Google Scholar]
- 28.Kass RE, Wasserman L. The selection of prior distributions by formal rules. J Am Stat Assoc. 1996;91:1343–1370. [Google Scholar]
- 29.Bell ML, Dominici F. Effects modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am J Epidemiol. 2008;167:986–997. doi: 10.1093/aje/kwm396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Neill MS, Hajat S, Zanobetti A, et al. Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorol. 2005;50:121–129. doi: 10.1007/s00484-005-0269-z. [DOI] [PubMed] [Google Scholar]
- 31.Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12:662–667. doi: 10.1097/00001648-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 32.The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349:1341–1346. [PubMed] [Google Scholar]
- 33.Barnett AG, Dobson AJ, McElduff P, et al. Cold periods and coronary events: an analysis of populations worldwide. J Epidemiol Community Health. 2005;59:551–557. doi: 10.1136/jech.2004.028514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaiser R, Le Tertre A, Schwartz J, et al. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health. 2007;97(suppl 1):S158–S162. doi: 10.2105/AJPH.2006.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rainham DGC, Smoyer-Tomic KE. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ Res. 2003;93:9–19. doi: 10.1016/s0013-9351(03)00060-4. [DOI] [PubMed] [Google Scholar]
- 36.Nawrot TS, Torfs R, Fierens F, et al. Stronger associations between daily mortality and fine particulate air pollution in summer than in winter: evidence from a heavily polluted region in western Europe. J Epidemiol Community Health. 2007;61:146–149. doi: 10.1136/jech.2005.044263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aylin P, Morris S, Wakefield J, et al. Temperature, housing deprivation and their relationship to excess winter mortality in Great Britain, 1986–1996. Int J Epidemiol. 2001;30:1100–1108. doi: 10.1093/ije/30.5.1100. [DOI] [PubMed] [Google Scholar]
- 38.Stafoggia M, Forastiere F, Agostini D, et al. Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology. 2006;17:315–323. doi: 10.1097/01.ede.0000208477.36665.34. [DOI] [PubMed] [Google Scholar]
- 39.Backlund E, Rowe G, Lynch J, et al. Income inequality and mortality: a multilevel prospective study of 521 248 individuals in 50 US states. Int J Epidemiol. 2007;36:590–596. doi: 10.1093/ije/dym012. [DOI] [PubMed] [Google Scholar]
- 40.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57:784–789. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.