Abstract
Objectives
To compare the efficacy of intravenous single dose, less costly cefotaxime and more expensive amoxycillin–clavulanic acid combination for prophylaxis at cesarean section.
Method
A double blind randomized controlled trial was undertaken on 760 subjects with two parallel treatment groups. Data were analyzed using Graphpad Instat 3 McIntosh software by Student’s t test, Mann–Whitney U test, the Chi-squared test or fisher’s exact test.
Results
Comparatively narrow spectrum low cost cefotaxime is as effective as more expensive commonly used amoxicillin–clavulanic acid with no significant difference of infectious morbidity and hospital stay (p = 0.27 and 0.11 in elective and emergency cases respectively).
Conclusion
Less costly cefotaxime should be preferred compared to more costly amoxicillin–clavulanic acid combination for prophylaxis at cesarean section.
Keywords: Antibiotic, Prophylaxis, Cesarean section
Introduction
Women undergoing caesarean delivery (CD) are 5–20 fold greater risk of infection than women of vaginal delivery group. Infectious complications after CD are an important and substantial cause of maternal morbidity and increase in the hospital stay and cost of treatment [1]. Infectious complications following CD include fever, wound infection, endometritis, urinary tract infection and some serious complications like pelvic abscess, septic shock, and septic pelvic vein thrombophelibitis.
It has been proved that prophylactic single dose antibiotic is equally effective as compared to long term postoperative combination of antibiotics [2] If some form of prophylaxis is not administered the incidence of post operative endomyometritis is unacceptably high. Even prophylactic use of antibiotic for elective CD reduces the risk of post operative infectious complications even in the population at lower risk [3, 4]. So further placebo controlled trials for the effectiveness of antibiotics with CD are not ethically justified and antibiotic prophylaxis should be used for all CD as a routine [5, 6]. However, debate continues regarding the type of antibiotic, dose and time of administration [7]. Regarding single dose versus multiple dose, it has been established that single dose is as effective as multiple dose as prophylaxis for CD [8–10].
A few studies have compared two different drugs in a randomized controlled trial [11]. Both cefotaxime and amoxicillin–clavulanic acid are being widely used for prophylaxis in CD, but with different cost. So this study was undertaken to compare the efficacy of intravenous single dose cefotaxime and amoxycillin–clavulanic acid combination.
Material and Methods
The current study is a double blind randomized controlled trial with two parallel treatment groups. The patient screening and recruitment were carried out at the obstetrics indoor ward of a tertiary care teaching hospital in Kolkata.
Inclusion Criteria
Patients undergoing CD on elective or emergency basis
Willingness to give written informed consent.
Exclusion Criteria
Subjects known to be hypersensitive to any of the trial drugs.
Any antibiotic treatment 2 weeks prior to surgery.
Presence of chorioamnionitis
Diabetes
Malnutrition
Obesity >85 kg.
Immuno-compromised state
>3 times per vaginal examination for intrapartum cases.
Prolonged preoperative hospitalization
Duration of labor >6 h.
The sample size was estimated to detect a difference of 6 % in wound infection rate between two antibiotic regimens. A total of 366 subjects were estimated to be required per group to detect such a difference with 5 % probability of type I error (α = 0.05 and 80 % power). Randomization was done a priori by computer in blocks of 40. The randomization list remained in the custody of the principal investigator.
Approval for the study was taken from the institutional ethic committee. Patients were fully informed by the investigators, in their mother tongue about the aims and procedures of the study and its potential risks and benefits. Following this, written informed consent was obtained from the patients, to take part in the study.
Study drug regimens were either Cefotaxime 1 g single dose intravenous (Group A) or amoxicillin–clavulanic acid combination 1.2 g single dose intravenous (Group B) just after clamping the umbilical cord. Being a double blind study, the nature or medication being received by individual trial subjects was not known to the subject or the project clinician. Urinary catheter was removed just after operation. Oral temperature record was maintained 6 hourly. Post operative routine investigations like Hb%, urine routine examination, culture were sent on the morning following the surgery. Presence of breast engorgement was checked in the post operative period. If fever persisted for >96 h, blood culture was sent. In every mother, skin sutures were removed on the 5th post operative day and the wound was inspected and uninfected mothers were discharged on next day.
Patients enrolled in the study were not administered any other intravenous or oral antibiotics. Other medications were permitted depending upon the clinical condition of the subject and need for such medication like analgesics and proton pump inhibitors.
Febrile morbidity was defined as oral temperature 100.4 °F or higher on two separate occasions 24 h apart exclusive of the first 24 h following surgery. The wound was inspected on the day of suture removal with few exceptions like soakage from the wound, persistent high fever or marked tenderness over the operated site. Wound was further classified into following groups.
Satisfactory healing—No wound discharge or erythema
-
Disturbed healing—Serous exudates with or without erythema.
It was treated by regular antiseptic dressing. Oral or parenteral antibiotic not needed.
Minor wound infection—Purulent exudates with erythema but no separation of deep tissue—managed by regular dressing.
Moderate wound infection—Separation of deep tissue with purulent exudates; treated by regular dressing followed by secondary suture.
Endometritis was diagnosed in patients with febrile morbidity, tachycardia, foul smelling lochia and uterine tenderness with or without positive high vaginal swab culture.
Side effects of antibiotics were also recorded. Adverse events, reported spontaneously by the subject or noted by the investigators during follow-up were noted in the case report form.
On an individual subject, the study was terminated in the following circumstances.
Development of complications requiring treatment with additional antibiotic.
Inadvertent use of antibiotic by any attending physician in the post operative period.
Data were collected on pre-designed case report form and analyzed for significant difference between the two groups through non parametric test and Mann–Whitney U test. Adverse event data was analyzed by Chi square or Fisher’s exact test as appropriate.
Graphpad Instat 3 McIntosh, California, software was used for analysis.
Results
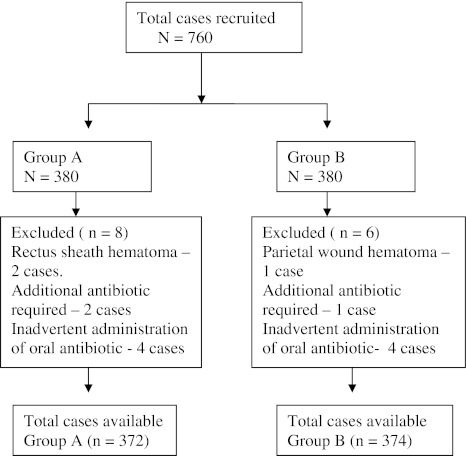
A total of 760 patients were recruited for the study. Eight patients in the cefotaxime group and six patients in the amoxicillin–clavulanic acid group had to be excluded from final analysis for various reasons (Fig. 1). So, 372 patients in the cefotaxime group and 374 patients in the amoxicillin–clavulanic acid group were compared in the study.
Fig. 1.
Recruitment of cases in two groups
Baseline characteristics like age, parity, gestational age and duration of labor are comparable in both groups (Table 1). In both groups history of previous caesarean delivery was the main indication whether CD were done as elective or emergency basis. Fetal distress was another main indication for emergency CD in both groups. Other indications for either emergency or elective CD are shown in Table 2.
Table 1.
Base line characteristics of the patients
| Group | A | B | p |
|---|---|---|---|
| Age (mean ± SD) (in years) | |||
| Elective | 24.49 ± 3.69 | 25.45 ± 4.71 | 0.051 |
| Emergency | 23.84 ± 4.71 | 23.81 ± 3.93 | 0.94 |
| Parity | |||
| Elective | 0.68 | 0.64 | 0.99 |
| Emergency | 0.51 | 0.57 | 0.99 |
| Gestational age. (in weeks) | |||
| Elective | 38.32 | 38.45 | 0.99 |
| Emergency | 38.26 | 38.29 | 0.99 |
| Labor duration (in hours) | |||
| Elective | – | – | |
| Emergency | 1.84 | 1.56 | 0.99 |
Elective: Group A (n = 145), Group B (n = 150)
Emergency: Group A (n = 227), Group B (n = 224)
Table 2.
Indication of caesarean section
| Elective | Emergency | |||
|---|---|---|---|---|
| A (N = 145) | B (N = 150) | A (N = 227) | B (N = 224) | |
| Fetal distress | – | – | 50 | 54 |
| Post CS | 61 | 65 | 84 | 79 |
| CPD | 13 | 10 | 17 | 18 |
| PIH | 17 | 15 | 21 | 23 |
| IUGR | 12 | 11 | 19 | 16 |
| BOH | 12 | 14 | 14 | 11 |
| APH | 16 | 19 | 14 | 16 |
| Malpresentation | 6 | 7 | 8 | 7 |
| Elderly primi with unfavorable cervix | 8 | 9 | – | – |
Following single dose prophylactic antibiotic therapy, the incidence of fever, mild or moderate wound infection did not differ significantly in both groups. (Table 3) Among elective CD, seven patients in group A and six patients in group B developed fever. Again among emergency CD 13 and 11 patients developed fever in group I and group II, respectively, and neither result was statistically significant (p = 0.78 and 0.83). There was no incidence of endometritis, urinary tract infection or any serious infection. Nine patients in the cefotaxime prophylaxis group and eight patients in the amoxicillin–clavulanic acid group developed fever in the 5th post-operative period with no site of infection identified. Fever subsided after oral paracetamol tablet and no antibiotic therapy required. There were no adverse reactions to any of the antibiotics. There was no significant difference in the duration of hospital stay between the groups (p = 0.27 in elective and 0.11 in emergency group).
Table 3.
Outcome measures
| A | B | p | RR (95% CI) | |
|---|---|---|---|---|
| Fever | ||||
| Elective | 7 | 6 | 0.78 | 1.1 (0.65–1.84) |
| Emergency | 13 | 11 | 0.83 | 1.08 (0.73–1.58) |
| Minor wound infection | ||||
| Elective | 2 | 2 | 1 | 1.01 (0.37–2.73) |
| Emergency | 5 | 4 | 1 | 1.10 (0.61–1.99) |
| Moderate wound Infection | ||||
| Elective | 1 | 1 | 1 | 1.01 (0.25–4.08) |
| Emergency | 3 | 2 | 1 | 1.19 (0.58–2.46) |
| Severe infection including endometritis | – | – | – | – |
| Hospital stay (mean ± SD) | ||||
| Elective | 6.67 ± 0.82 | 6.57 ± 0.74 | 0.27 | |
| Emergency | 6.63 ± 0.81 | 6.75 ± 0.79 | 0.11 | |
Elective: Group A (n = 145), Group B (n = 150)
Emergency: Group A (n = 227), Group B (n = 224)
Discussion
Any antibiotic is effective in clean and uncontaminated cases and choice should therefore be based on other factors such as cost [3]. We desired to determine whether comparatively narrow spectrum low cost cephalosporine–cefotaxime with more expensive commonly used amoxicillin–clavulanic acid regimen and we found that narrow spectrum cefotaxime was as effective as amoxicillin–clavelunic acid.
For most surgical procedure, it is desirable to administer prophylactic antibiotic pre-operatively before tissue injury and bacterial contamination occur. If this policy were implemented for CD the neonate would be exposed to antibiotic before birth. In theory even this limited exposure might interfere with the ability of the pediatrician to evaluate the newborn for sepsis [2]. However, Thigpen et al. have concluded that there was no difference in maternal infectious morbidity whether antibiotics were given before skin incision or after cord clamping [11].
Numerous antibiotics have been used in studies evaluating prophylaxis in patients undergoing CD the most frequently used agent include penicillins and cephalosporins. Most studies have shown a significant difference between these antibiotics and placebo but no significant difference between various antibiotics used for prophylaxis. So the ideal choice of an antibiotic has not yet been defined. Similarly Parulekar et al. concluded that prophylactic single dose cefotaxime is more effective as compared to conventional 5 days gentamycin–cloxacillin combination [12]. Newer more expensive and broader spectrum cephalosporin had no extra beneficial effect than less expensive cefazoline [11]. and single dose cefazoline prophylaxis appears to be comparable to multidose prophylaxis in reducing febrile morbidity after CD [7, 14]. Again, Noyes et al. studied the incidence of postpartum endomyometritis following single dose antibiotic prophylaxis with either ampicillin/sulbactum, cefazoline or cefotetan and they concluded that no statistical significant difference of infection rate [13].
Pitfall of the study: We have not followed the patient for further any infection related morbidity after their hospital discharge.
Conclusion
Both single dose prophylactic amoxicillin–clavulanic acid and cefotaxime have similar efficacy in reducing maternal postoperative infectious morbidity. So less costly cefotaxime should be preferred compared to more costly amoxicillin–clavulanic acid combination.
Acknowledgments
We are thankful to the Principal and Head of the department of Obstetrics and Gynaecology of R. G. Kar Medical College, Kolkata for allowing us to conduct the study and for giving necessary permission for publishing the paper.
References
- 1.Wild SM. Antibiotic prophylaxis at caesarean section. The Lancet. 2002;360:724. doi: 10.1016/S0140-6736(02)09862-8. [DOI] [PubMed] [Google Scholar]
- 2.Rouzi AA, Khalifa F, Ba’aqeel H, et al. The routine use of cefazoline in cesarean section. Int J Obst Gynecol. 2000;69:107–112. doi: 10.1016/S0020-7292(99)00225-8. [DOI] [PubMed] [Google Scholar]
- 3.Chelmow D, Ruheli MS, Huang E. Prophylactic use of antibiotics for nonlaboring patients undergoing cesarean delivery with intact membranes: a meta analysis. Am J Obstet Gynecol. 2001;184:656–661. doi: 10.1067/mob.2001.111303. [DOI] [PubMed] [Google Scholar]
- 4.Mah MW, Pyper AM, Oni GA, et al. Impact of antibiotic prophylaxis on wound infection after cesarean section in a situation of expected higher risk. Am J Infec Control. 2001;29:85–88. doi: 10.1067/mic.2001.111372. [DOI] [PubMed] [Google Scholar]
- 5.Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. The Cochrane Database Syst Rev. 2002;3:CD000933. doi: 10.1002/14651858.CD000933. [DOI] [PubMed] [Google Scholar]
- 6.Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. Oxford: The Cochrane Library; 2007. p. 4. [Google Scholar]
- 7.Hopkins L, Smaill F. Antibiotic prophylaxis regimens and drugs for cesarean section. Cochrane Database Syst Rev 1999; CD 001136. [DOI] [PubMed]
- 8.Shah S, Mazher Y, John S. Single or triple dose piperacillin prophylaxis in elective cesarean section. Int J Obstet Gynecol. 1998;62:23–29. doi: 10.1016/S0020-7292(98)00063-0. [DOI] [PubMed] [Google Scholar]
- 9.Alekwe LO, Kuti O, Orji EO, et al. Comparison of ceftriaxone verses triple drug regimen in the prevention of caesarean section infectious morbidities. J Matern Fetal Neonatal Med. 2008;21:638–642. doi: 10.1080/14767050802220490. [DOI] [PubMed] [Google Scholar]
- 10.Shetty J, Vyas NM, Kumar P, et al. Antibiotic prophylaxis for hysterectomy and caesarean section: Amoxycillin–clavulanic acid versus cefazolin. J Obstet Gynecol Ind. 2010;60:419–423. doi: 10.1007/s13224-010-0069-1. [DOI] [Google Scholar]
- 11.Thigpen BD, Hood WA, Chauhan S, et al. Timing of prophylactic antibiotic administration in the uninfected laboring gravida: a randomized clinical trial. Am J Obstet Gynecol. 2005;192:1864–1871. doi: 10.1016/j.ajog.2004.12.063. [DOI] [PubMed] [Google Scholar]
- 12.Parulekar P, Kumar S, Awasthi RT, et al. A single dose of cefotaxime: as a prophylaxis during cesarean section. J obstet Gynecol Ind. 2001;51:118–121. [Google Scholar]
- 13.Noyes N, Berkley As, Freedman K, et al. Incidence of postpartum endomyometritis following single dose antibiotic prophylaxis with either ampicillin/sulbactum, cefazoline or cefotetan in high risk cesarean section patients. Infect Dis Obstet Gynecol. 1998;6:220–223. doi: 10.1002/(SICI)1098-0997(1998)6:5<220::AID-IDOG6>3.0.CO;2-G. [DOI] [PMC free article] [PubMed] [Google Scholar]