Abstract
Objectives
The present study was undertaken to check the relevance of reversal of sterilization in women in the present era of test tube babies, to evaluate the Standard guidelines for sterilization, (The site of the occlusion of the fallopian tube must be always be within 2–3 cm from the uterine cornu in the isthmal portion, excision of 1 cm of the tube should be done. Use of cautery and crushing of the tube should be avoided.) are being followed universally in the institution and outside, to study the demographic patterns of women coming for reversal of sterilization and to evaluate the causes for either the inability to perform reversal of sterilization or the adversaries like ectopic pregnancy that occur after the procedure.
Methods
The present study is a retrospective study carried out in the Department of Microsurgery, Obstetrics and Gynecology, Government Kilpauk Medical College and Hospital Chennai based on the case records maintained in the institution. Three groups of women have been chosen at various periods and the various factors related have been compared. This includes the women who have come to the institution for reversal of sterilization during the years 1991–1995, 2000–2004 and 2006–2008 respectively.
Result
The demand for reversal has increased almost 81 % after 2005 whereas the standards of sterilization are actually being followed in <17 % of women. The incidence of Ectopic pregnancies has increased and the incidence of take home pregnancies has come down.
Conclusion
There is a need to stick to the standards of sterilization. Proper selection of candidates for sterilization and reversal of sterilization is important.
Keywords: Reversal of sterilization, Ectopic pregnancy, Standards of sterilization
Introduction
Centre of Excellence, Recanalisation unit, Department of Microsurgery, Government Kilpauk Medical College and Hospital, Chennai has been performing reversal of sterilization since 1989. Previous studies in the same department done in 1993 and 2001 has been the guiding factor for this study. The demand for sterilization reversal has been ever increasing since it is put into practice and recently it has shown a steep increase in the demand. As per the standards of sterilization guidelines, ministry of health, & FW, GOI, Oct. 2006, The site of the occlusion of the fallopian tube must be always be within 2–3 cm from the uterine cornu in the isthmal portion (this will improve the possibility of reversal if required in the future). Care must be taken to avoid damage to the blood vessels, ovaries, and surrounding tissues. Excision of 1 cm of the tube should be done. Use of cautery and crushing of the tube should be avoided [1].
Over time it has been noticed that the eligible women requesting for reversal of sterilization often do not have proper length of fallopian tubes required for sterilization (very little or no tube at the distal segment or only Fimbria at distal segment, no Fimbria at all, etc).
As a result reversal of sterilization is either not performed or even after the recanalisation is performed women ends up with an ectopic pregnancy or no pregnancy at all. This study is covering various factors affecting recanalisation and it also includes the demographic patterns like age, obstetric score and reason for reversal of sterilization.
Materials and Methods
This study is a retrospective study based on 811 women who have come to Department of Microsurgery, Government Kilpauk Medical College and Hospital for reversal of sterilization during the selected periods 1991–1995 (242 women), 2000–2004 (273 women) and 2006–2008 (296 women), taken as Group A, Group B and Group C respectively. Information has been taken from the case records of these patients maintained in the institution. Important aspect of case history including Age, Obstetric score, Sterilization and its reversal interval, type of sterilization and cause of sterilization has been taken into account in all the cases. In cases where reanastamosis could not be performed, its reason has been taken into account. Proximal and distal segment of fallopian tube before the reversal and the total length after reanastamosis has been taken. Type of reanastamosis including Isthamo-Isthamic, Isthamo-ampullary, etc. has been thoroughly recorded. Comparisons of various factors affecting pregnancy, ectopic pregnancy have been evaluated both within the group and among the three groups to evaluate the changing trends. While considering the type of Reanastamosis, the tube with the longer length has been selected. The fallopian tube which has longer length after recanalisation has been selected for all statistical purposes. If two tubes have same length then Isthamo-Isthamic anastamosis has been selected over Isthamo-ampullary and others. If Isthamo-Isthamic is not there then the anastamosis that involves equal diameter tubes e.g. Ampulo-ampullary has been selected. In case of ectopic pregnancies individual tubes irrespective of the type of anastamosis or length has been taken.
Results
Group A, Group B and Group C includes women who have come to the institution for reversal of sterilization during the years 1991–1995, 2000–2004 and 2006–2008 respectively.
The number of women requesting reversal of sterilization has increased almost twice in the projected year 2006–2010 than the previous Group B (Table 1).
Table 1.
Number of women requesting the reversal of sterilization
| No. of women demanding reversal of sterilization | Increase in No. of women than the previous group (%) | |
|---|---|---|
| Group A (1991–1995) | 242 | – |
| Group B (2000–2004) | 273 | 12 |
| Group C (2006–2008) and Projected (2006–2010) | 292 and 493 | 7.69 and 81 |
Majority of women have come after 1 year (Table 2).
Table 2.
Sterilization reversal interval
| <1 year (%) | 1–5 year (%) | >5 year (%) | |
|---|---|---|---|
| Group A | 7 (3.07) | 121 (53.07) | 100 (43.85) |
| Group B | 1 (0.46) | 100 (46.29) | 115 (53.24) |
| Group C | 5 (2.20) | 107 (47.13) | 115 (50.66) |
Incidence of Carry home pregnancy has come down and ectopic pregnancy has gone up among Group A and Group B whereas Group C has a shorter duration of follow up and the collection of data is still in progress and more number of pregnancies are expected with time (Tables 3, 4).
Table 3.
Percentage of Carry home pregnancy and ectopic pregnancies
| Carry home pregnancy (%) | Abortions (%) | Ectopic pregnancy (%) | |
|---|---|---|---|
| Group A | 89 (39.73) | 11 (4.01) | 9 (4.01) |
| Group B | 82 (30.17) | 10 (3.75) | 21 (7.86) |
| Group C | 26 (8.9) | 4 (1.36) | 18 (6.16) |
Table 4.
Percentage of women where standard of sterilization has been followed on the longer fallopian tube
| Standards have been followed (%) | |
|---|---|
| Group A | 16.07 |
| Group B | 8.89 |
| Group C | 5.73 |
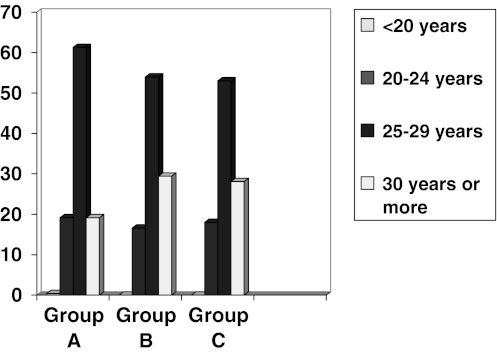
The women of age group 25–29 are the most common group in all the three groups (Chart 1).
Chart 1.
Age of women in percentage among Group A, Group B and Group C
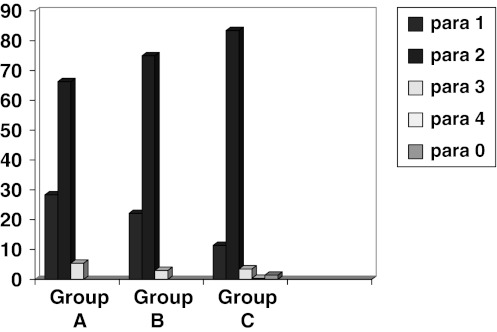
Women with Para 2 has requested for reversal most frequently in all the three groups and Group C has recorded women with Para 0 and Para 4 (Chart 2).
Chart 2.
Parity of women in the three groups
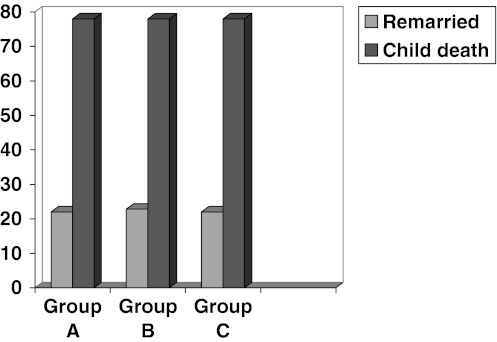
Child death has been the main cause, while Remarriage as a cause is also significant as more than 20 % of women in all the three groups have demanded sterilization reversal because of remarriage (Chart 3).
Chart 3.
Reason for sterilization reversal
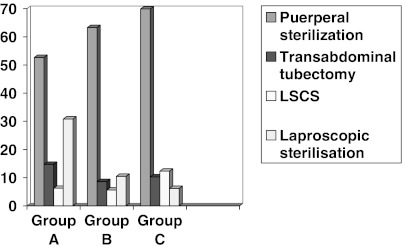
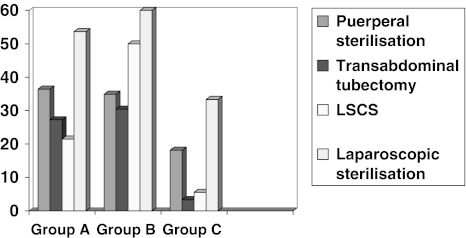
Puerperal sterilization is the most common and the laparoscopic sterilization incidence has come down (Chart 4).
Chart 4.
Percentage of type of sterilization
Laparoscopic sterilization has most of the incidences of pregnancies (Chart 5).
Chart 5.
Pregnancy percentage in various sterilization types that have undergone reanastamosis
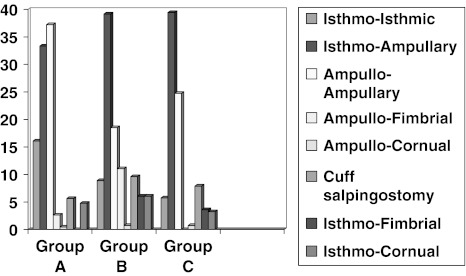
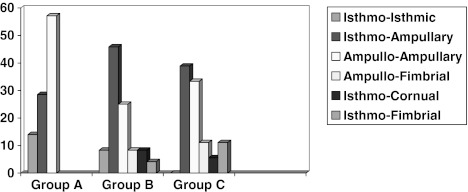
Isthmo-ampullary anastamosis has been practiced in more than 30 % of women in all the three groups whereas the percentage of isthmo-isthmic anastamosis is reducing (Chart 6).
Chart 6.
Preponderance of type of anastamosis of fallopian tube
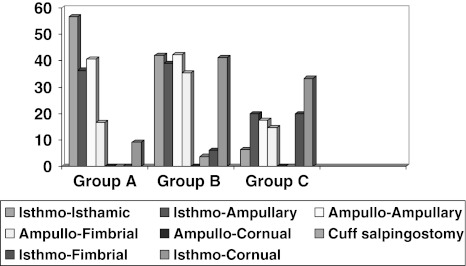
Percentage of Pregnancies among different types of anastamosis tube length (>6 cm) has come down in Group B and Group C (Chart 7).
Chart 7.
Isthmo-Isthmic anastamosis has been associated with pregnancies upto 40–58 % in the Group A
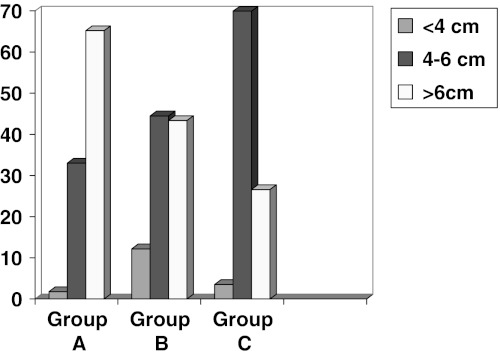
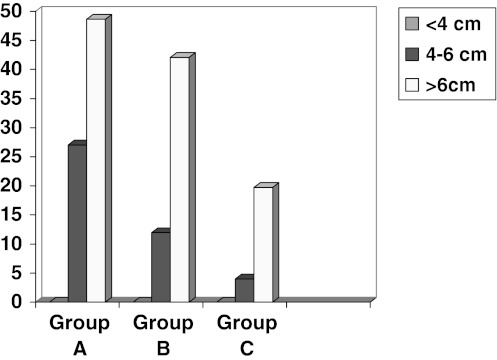
Up to 48 % of pregnancy is associated with tube length >6 cm at least on one side, (Group C has a very short duration of follow up period and more number of pregnancies are expected with time and actually many of the pregnancies are not yet reported) (Charts 8, 9).
Chart 8.
Length of the tube
Chart 9.
Longest length of tube and intra uterine pregnancy
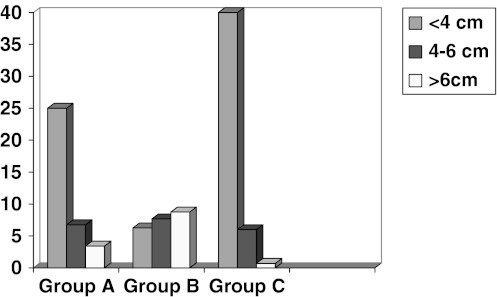
Up to 40 % ectopic pregnancies can occur in tubal length <4 cm (Chart 10).
Chart 10.
Length of tube and ectopic pregnancy
Isthmo-ampullary anastamosis has been associated with 30–45 % of total ectopic pregnancies (Chart 11).
Chart 11.
Ectopic pregnancy according to the type of tubal anastamosis
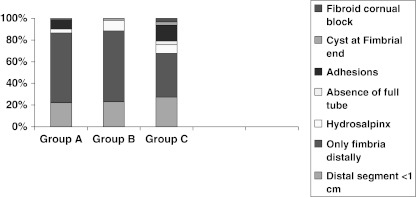
Presence of only fimbria at the distal end with no tubal part distally or no fimbria at all has been the most common cause for inability to perform reanastamosis. Evidence of fimbriectomy during sterilization, associated hydrosalpinx, cornual block, distal segment less than 1 cm are the common causes for inability to perform reanastomosis (Chart 12).
Chart 12.
Reason for inability to perform the reversal of sterilization
Discussion
The demographic pattern of women has not changed in the three groups including Age and parity over time, in the present study. Remarriage has accounted for 20–23 % in this study against 63 % according to the study of Victor Gomel 1978 [2]. Incidence of pregnancies are <40 % in this study, in comparison to 60 % given by study by James Trussell done in a period from 1980 to 1999 [2]. In this study four women with Para 0 who had Medical termination of pregnancies with sterilization have requested for reversal of sterilization in Group C (2006–2008) and one woman with Para 4 has also requested for sterilization in Group C (2006–2008). The sterilization reversal interval ranges from 20 days to 17 years. More than 70 % of women have requested for recanalisation because of death of the child. More than 50 % of ectopic pregnancies have occurred with Isthmo-ampullary and ampullo-ampullary tubal anastamosis. Only Fimbria present at distal end or no fimbria at all is the most important cause of inability to perform the procedure, in Group C (2006–2008) its number is 108 whereas it was 69 and 53 in Group A and Group B respectively in either one side fallopian tube or bilateral. This study indicates that the incidence of Isthmo-Isthmic anastamosis has come down gradually in the three groups and Cuff salpingostomy incidence has gone up in Group C (7.88) and Group B (9.62) than Group A (5.62).
Mohanalakshmi et al. (1991). reported from same centre 77.1 % reversal after Pomeroy, 22.9 % after laparoscopic fallope ring application, and in 42.8 and 50 %, sterilization done at Institutions & peripheral centres, respectively had sterilization site at fimbrial end [4]. The most common age group has been 25–29 years in the present study similar to 48.5 % in 26–30 years in the previous study [5] in the same institution. In the previous study of 1993 [6] 54.6 % of sterilization are of puerperal type, this finding corresponds with the present study Swarnalatha et al [7] from the same centre, 1993 has reported 100 % patency rate on the table, and 90.7 % patency at early second look laparoscopy and 25.4 % adhesions, and 11.8 % adhesiolysis.
The present study indicates that the chances of pregnancy after recanalisation is more if the total length of the tube is more than 6 cm with at least one fimbria intact, this is similar to the finding of the study regarding relationship between the length of the oviduct and the occurrence of the pregnancy by V. Gomel, and study done by Rouzi. A et al in 1995 [8].
S. J. Silber and R. J. Cohen reported, among 25 women, 60 % normal intrauterine pregnancy and 4 % ectopic pregnancy were directly related to tubal length. Of 7 patients who had <3 cm of tube, none achieved pregnancy. Of 7 patients who had 3–4 cm of tube, 3 achieved a normal intrauterine pregnancy. Among 11 patients who had more than 4 cm of tube, all achieved a normal intrauterine pregnancy. No significant difference in pregnancy rate was noted in women who had short segments of ampulla so long as total tubal length was adequate. It seems that as long as there are healthy fimbriae, microsurgical reanastomosis can restore tubal patency in all cases. [9]. The cumulative intrauterine pregnancy rate was 62 % at 18 months and age was the most significant predictive factor [10].
Ideally the sterilization should be in the isthmic region but in Group B (2000–2004) and Group C (2006–2008) the sterilization involving the isthmic region has come down. In the present study the laparoscopic sterilization has highest pregnancy occurrence and least ectopic pregnancy chances stands true with the finding of the previous study done in the institution. It is found that sterilization done according to the standards of sterilization follows highest incidence of Intrauterine pregnancy following reversal.
Conclusion
There is a need to adhere to the standards of sterilization., as instructed by Technical Operations Division, Ministry Of health and family welfare, Government of India. It has been found in the present study that if the standards of sterilization is strictly followed, it will help in reducing the incidence of ectopic pregnancies and it will help in improving the chances of intrauterine pregnancies. 20–25 % of reversal are done for remarriage, around 80 % done for death of children. With natural calamities like tsunami, catastrophe like Kumbakonam fire accident, and still high infant mortality in underprivileged women, the need for reversal is present. Proper care of the tubes at the time of sterilisation go a long way in success of reversal, thereby helping the unfortunate women to have children, also instilling hope for women in family welfare procedures, that they will he helped in case of eventuality.
References
- 1.Standards for female and male sterilization services—Division of research studies & standards, Ministry of Health & family Welfare, GOI, 5th ed 2006.
- 2.Gomel V. Profile of women requesting reversal of sterilization. Fertil Steril. 1978;30(1):39–41. doi: 10.1016/s0015-0282(16)43392-3. [DOI] [PubMed] [Google Scholar]
- 3.Trussell James, Guilbert Édith, Hedley Allison. Sterilization failure, sterilization reversal and pregnancy after sterilization reversal in Quebec. Obstet Gynecol. 2003;101:677–684. doi: 10.1016/S0029-7844(02)03156-3. [DOI] [PubMed] [Google Scholar]
- 4.Mohanalakshmi TK, Kalaichelvi A, Premlatha R. Analysis of 140 cases of recanalisation. Scientific abstract, paper presented in AICOG congress Dec 27–30, 1991.
- 5.Kalaichelvi A, Swarnalatha R, Premlatha R. Is reversal of sterilization feasible. Indian J Obstet Gynecol. 2001;51(2):120–122. doi: 10.1159/000052906. [DOI] [Google Scholar]
- 6.Premlatha R, Kalaichelvi A, Swarnalatha R. Role of preoperative hysterolaproscopy in 260 cases of recanalisation. Indian J Obstet Gynecol. 1993;988–91.
- 7.Swarnalatha R, Kalaichelvi A, Mohanalakshmi TK et al. Evaluation of early second look laparoscopy, Indian J Obstet Gynecol 1993; 1010–1012.
- 8.Rouzi AA, Mackinnon M, McComb PF. Predictors of success of reversal of sterilization. Fertil Steril. 1995;64:29–36. [PubMed] [Google Scholar]
- 9.Silber SJ, Cohen R. Microsurgical reversal of female sterilization: the role of tubal length. Fertil Steril. 1980;33(6):598–601. doi: 10.1016/s0015-0282(16)44770-9. [DOI] [PubMed] [Google Scholar]
- 10.Dubuisson JB, Chapron C, Nos C, et al. Surgery, sterilization reversal, fertility results. Hum Reprod. 1995;10(5):1145–1151. doi: 10.1093/oxfordjournals.humrep.a136108. [DOI] [PubMed] [Google Scholar]