Abstract
Objective
To determine the prevalence and impact of placental malaria on maternal and fetal outcome.
Design
Cross sectional observational.
Setting
The Department of Obstetrics of Government NSCB Medical College Hospital, Jabalpur (Madhya Pradesh).
Population
Five hundred parturient women with fever or history of fever during the present pregnancy.
Method(s)
Subjects were tested for peripheral and placental malaria by thick and thin smear examination. Maternal and perinatal outcome correlated with malaria results.
Results(s)
The mean age of the studied subjects was 24.5 ± 2.6 years, 60.6 % were primigravida, 87.2 % had unsatisfactory antenatal care. 89.2 % were not using effective malaria prevention measures. Peripheral smear positivity for malaria was detected in 1.8 % subjects and placental malaria positivity in 2.2 % subjects. The mean Hb was lower in malaric subjects (χ2 = 14.47, p < 0.05). Maternal mortality and prematurity was significantly higher in malaria +ve subjects (p < 0.001). The mean birth weight in malaria +ve subjects was significantly less (p < 0.001). Poor 5 min APGAR (p < 0.0001) and perinatal mortality (p < 0.05) was significantly more common in malaria +ve subjects.
Conclusion(s)
Malaria, particularly placental infestation with malarial parasites significantly increases maternal and perinatal morbidity and mortality.
Keywords: Malaria, Anemia, Low birth weight, Prematurity
Introduction
Malaria imposes great socio-economic burden on humanity, accounting for 85 % of global infectious disease [1]. It afflicts 90 countries and territories in the tropical and subtropical regions and about 36 % of the world population (i.e., 2020 million) is exposed to the risk of contracting malaria [1]. It affects all ages but pregnant women and children are at high risk because of low immunity. It is estimated that 1.2 billion people out of the 1.4 billion people of South East Asia region live in malarious areas [2]. India contributes about 76 % of total malaria cases in South East Asia Region [1].
Malaria in pregnancy imposes additional burden on mother and also affects fetal outcome adversely [3, 4]. Pregnant women with little or no pre-existing immunity are at high risk of cerebral malaria, hypoglycaemia, pulmonary edema and hemolytic anemia. Malaria infection in pregnancy can cause low birth weight (LBW), abortion, stillbirth, premature delivery and infant death [3, 5, 6]. Fetal and perinatal loss can be as high as 60–70 % [7–9]. In areas of stable malaria transmission, maternal morbidity is mainly represented by anemia [3] and the major effect on the fetus is a reduction in birth weight [10, 11].
The diagnosis of malaria during pregnancy requires laboratory confirmation [12–14]. The histological examination of the placenta is the most sensitive indicator of maternal infection [15]. Examination can show signs of active infection (presence of infected erythrocytes in the intervillous space), past or chronic infection (malarial pigment), or both [7]. Again, expertise and workload has meant that such tests are available only at select centres for research purposes.
The prevalence of malaria in the city of Jabalpur is low (<2/1,000 population). The Government NSCB Medical College Hospital Jabalpur is a tertiary Referral Hospital catering to a large number of surrounding districts; some of them are predominantly tribal and have a high prevalence of malaria. As many as 40–50 % of patients seen in the Obstetric department have some complications, by far anemia, with haemoglobin levels as low as 1.5–2 g% reported in 0.6 % subjects and <5 g% in as many as 10–12 % subjects. In a vast majority of them, the anemia doesn’t seem to be simply nutritional or due to any prepregnancy or pregnancy blood loosing diseases. Also, fever is a common morbidity (6 %) for which patients are referred to this hospital. As a result, the work load in the obstetric unit is high and the resources are meagre. Considering that this is a malaria endemic zone and at times investigations are not feasible (mostly due to financial constraints), subjects are put on antimalarial therapy on the basis of history and clinical examination. We therefore undertook this study to find out the burden of malaria amongst subjects with fever or history of febrile illness in pregnancy and to correlate it with placental malaria to find if chronic malaria is in any way responsible for the high prevalence of severe maternal anemia and poor maternal and perinatal outcome.
Material and Methods
Place of Study and Study Design
This is a cross-sectional study carried out in the Department of Obstetrics of Government NSCB Medical College Hospital, Jabalpur from July 2008 to June 2009. A total of 9,086 pregnant subjects attended the OPD during this period. Of a total of 3,894 subjects admitted in labor, 589 were either febrile or had history of febrile illness during the present pregnancy. Of them, 500 consented to participate in the study. Trained study personnel interviewed the enrolled women and collected information on socio-demographic characteristics (i.e. date of birth, socio-economic status, literacy), reproductive history including gravidity, history of fever and anti-malarial drug use and use of malaria prevention measures through questionnaire and the health records of the subjects. A complete physical examination including the determination of gestational age from the height of fundus, measurement of axillary temperature with digital thermometer, and other vital signs was also performed. Blood was obtained by finger-stick for malaria blood film preparation (thick and thin), rapid diagnostic test for P. vivax and P. falciparum and hemoglobin determination. Women with positive results or who were anaemic were put on appropriate treatment.
The enrolled parturient women were closely monitored and all requisite information regarding intranatal and post natal events were systematically recorded Placenta was immediately washed with phosphate buffer solution (PBS). A 2 cm long shallow incision was made in the basal plate. Blood pooling in the incision was collected with a 1 cc blunt syringe and a thick and thin smear prepared. Cord blood was collected by squeezing and another smear prepared and labelled. The smears were air dried and stained with Geimsa stain and microscopically examined.
Shortcomings of the Study
As a pilot study, 22 women who were febrile during the antenatal period were enrolled. However, only 6 of them reported to the obstetric unit for delivery. Therefore, we decided to carry out the study on subjects admitted in labour so that the Malaria tests on cord blood and placenta could be carried out.
Statistical Analysis
Data was analysed using SPSS 11.5. Appropriate statistical analysis using t test, Chi square test and Fishers exact test was applied and the critical level of significance was considered at 0.05 level.
Results
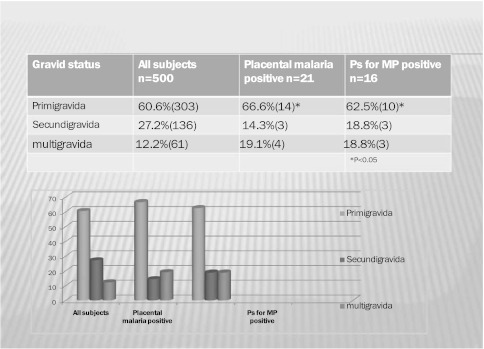
The mean age of the studied subjects was 24.5 ± 2.6 years, 81.4 % were from rural areas and 86.4 % belonged to low socio-economic status. A substantial 87.2 % had unsatisfactory antenatal care in terms of less number of antenatal visits or poor quality of antenatal care or both. 89.2 % were not using effective malaria prevention measures. History of malaria was present in 5 % and blood transfusion in 5.4 % subjects (Table 1) 60.6 % were primigravida (Fig. 1). Anemia was the most frequent morbidity (92.2 %) followed by pregnancy induced hypertension (15.6 %) and Jaundice (1 %).
Table 1.
Maternal profile in malaric and non-malaric subjects
| Peripheral smear +ve (n = 16) | Placental smear +ve (n = 21) | Smear −ve (n = 479) | |
|---|---|---|---|
| Age (Years) | 24.62 ± 3.75 | 24.71 ± 2.61 | 24.53 ± 2.62 |
| Primipara | 62.5 % | 66.6 % | 60.6 % |
| Mean Hb in gms% | 7.18 ± 2.31* | 5.6 ± 2.3* | 8.46 ± 1.60 |
| PIH & Eclampsia | 31.2 % | 33.3 % | 14.8 % |
| Average hospital stay | 9 ± 4 days* | 12 ± 6 days* | 3 ± 2 days |
| Blood transfusions | 43 % | 67 %* | 19.3 % |
| Maternal deaths | 18.8 %** | 28.6 %** | 2.5 % |
* p < 0.05; ** p < 0.001
Fig. 1.
Distribution of subjects according to gravid state
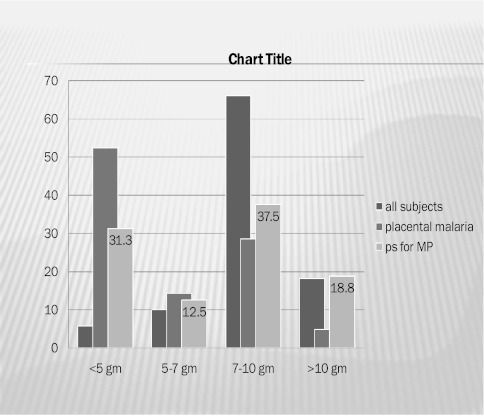
Peripheral smear positivity for malaria was detected in 1.8 % (n = 16) subjects and placental malaria positivity in 2.2 % (n = 21) subjects. 11 subjects were both peripheral and placental malaria positive. P. vivax was diagnosed in 13.8 %, P. falciparum in 70.2 % and mixed infection in 16 % subjects. The parasite load could not be estimated due to non availability of technical staff and time constraints. Similarly RDT could be carried out in only 167 subjects; the kit was unavailable in the remaining subjects. The RDT was positive in all the 7 malaria +ve patients by PS (2 were also PlS +ve). The mean Hb in peripheral smear (PS) +ve subjects was 7.18 ± 2.31 g% as compared to 8.38 ± 1.70 g% (χ2 = 20.59, p < 0.05) in peripheral smear −ve subjects. The mean Hb in placental smear (PlS) +ve subjects was 5.67 ± 2.37 g% as compared to 8.46 ± 1.60 g% (χ2 = 14.47, p < 0.05) in placental smear −ve subjects (Fig. 2).
Fig. 2.
Distrubution of subjects according to hemoglobin
The prevalence of pre-eclampsia and eclampsia was 33.3 % in PS +ve, 31.2 % in PlS +ve and 14.8 % in −ve subjects. Although intrapartum fetal distress was more frequent in MP +ve (38 %) subjects, there was no significant difference between the mode of delivery and the indication for cesarean section. A higher percentage of subjects with malaria positivity had post partum complications like post partum hemorrhage (33.3 % against 5.6 %), shock (4.76 % against 1.4 %), post partum fever (4.76 % against 0.8 %) and acute pulmonary edema (9.52 % against 0.4 %) but this difference was statistically insignificant. Maternal mortality was significantly higher in malaria +ve subjects (28.6 %, p < 0.001). The affected subjects faced multiple febrile episodes (average two episodes in the present pregnancy), headache (56 %), myalgia (78 %) and in severe cases neurological sequels (14%). Many required critical care (3 cerebral malaria, 2 hyperpyrexia with metabolic derangements), longer hospital stay (10 days ± 3 as against average hospital stay of 3 days ± 2), and blood transfusions (55 % as against an obstetric ward average of 19.3 %) (Table 1).
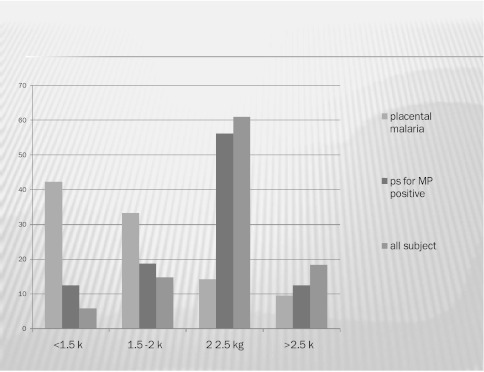
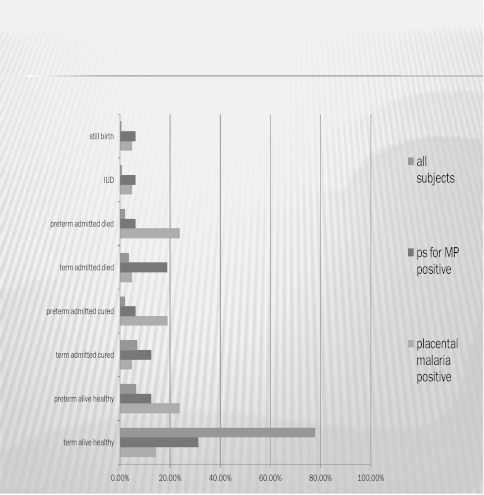
The incidence of prematurity (66.64 %) was significantly higher in malaria PlS +ve subjects (p < 0.001) as compared to PS +ve (25 %) and malaria −ve subjects (7.84%) (Table 2). The mean birth weight in malaria −ve subjects was 2.36 kg ± 0.25 while that in peripheral malaria +ve subjects was 2.21 kg ± 0.44 and placental malaria +ve subjects was 2.07 kg ± 0.29 (p < 0.001) (Fig. 3). Poor 5 min APGAR was significantly more common in malaria +ve subjects (PS +ve 37.5%; PlS +ve 14.3%) than malaria −ve subjects (4.2%, p < 0.0001). Perinatal mortality was 37.4 % in PS +ve, 38.08 % in PlS +ve and 7% in malaria −ve subjects (p < 0.05). Only one neonate born to a PlS +ve for falciparum mother was diagnosed to have congenital malaria. This newborn was treated with antimalarials but succumbed to the infection (Fig. 4).
Table 2.
Perinatal outcome in malaric and non malaric subjects
| Peripheral smear +ve (n = 16) | Placental Smear +ve (n = 21) | Smear –ve (n = 479) | |
|---|---|---|---|
| Prematurity | 25% | 66.4%** | 7.84% |
| Mean birth weight (Kg)) | 2.21 ± 0.44** | 2.07 ± 0.29** | 2.36 ± 0.25 |
| APGAR <5 at 5 mins | 37.5 %** | 14.3 %** | 4.2 % |
| Still birth | 6.25 %* | 4.76 %* | 0.4 % |
| Perinatal mortality | 37.5 %* | 38.08 %* | 7.0 % |
* p < 0.05; ** p < 0.001
Fig. 3.
Distrubution of subjects according to birth weight
Fig. 4.
Distrubution of subjects according to perinatal outcome
Discussion
In low-transmission setting such as ours, the immunity to malaria is not well developed and it has serious consequences for both the mother and foetus. Poor, young prismigravida from rural areas with unsatisfactory antenatal care bear the brunt of this disease. Similar demographic characteristics were reported by Singh et al. [16] in a study done in the same hospital in the year 1992–1995. Almost two decades have passed since, yet the lives of our poor pregnant women remain clouded by preventable miseries. The National Malaria Eradication Programme (NMEP) has been active since 1958 and the Regional Malaria Research Centre in Jabalpur is the largest centre working in the field of malaria eradication, yet a whopping 89.2 % of the subjects were not using effective malaria prevention measures. It was more due to lack of motivation and the failure to realise the serious implications of malaria, particularly in pregnancy, rather than due to scarcity of resources. Singh et al. in their study in the same department between 1992 and 1995 reported P. vivax +vity in 33 % and P. falciparum +vity in 67 % while in our study P. falciparum was +ve in 86.2 % showing that P. falciparum infection is becoming increasingly more common in pregnancy. Government efforts to take ante natal care (ANC) to the doorstep of a pregnant woman(ANC being provided by Anganwadi Workers who have extremely basic knowledge) often has the negative fallout of such subjects never coming in contact with a qualified physician in a Health Centre and many morbidities are missed until they become serious.
Studies conducted in Zaire, Blantyre and in Malawi suggest that age-associated immunity may play an important role in limiting P.falciparum to low parasite densities in areas of high and stable transmission. In our study too, mothers with malarious placentas were younger primipara (mean age 24 years) than mothers with non-malarious placentas (mean age 29-years) (Fig. 1), [16]. Pregnancy related complications in the form of preterm live birth (20 %), Intra uterine death (31.11 %), still births (13.33 %) and abortions (11.11 %) were more pronounced in primiparous women (so was malaria) as compared to multiparous women.
Even though anemia in pregnancy is multifactorial, the severity of anemia is more in malaria (placental > peripheral malaria) +ve subjects (Fig. 2). Placental malaria indicates a more long standing infection leading to lower Hb levels. Malaria and anemia together make these subjects less capable of enduring the stress of labor, resulting in increased incidence of operative intervention; they are more prone to develop post partum hemorrhage, pulmonary oedema, cardiac failure and shock and are at a high risk of requiring a blood transfusion during delivery.
Histopathology being more sensitive in identifying placental malaria, the use of placental smear in this study may have underestimated the burden of placental malaria. But the present study has shown that even when peripheral smears are −ve for malaria, patients can suffer adverse consequences due to parasitisation of the placenta. Since the overall prevalence of malaria as a cause of febrile illness in pregnancy is low in our hospital [16], the practice of treating patients with fever and anemia empirically with antimalarials before results of investigations are available is not justified. It only adds to the financial burden in a very tight economic situation, in addition to exposing the patients to the risk of potential side effects and adverse reactions. The present study had many limitations in terms of resources but these are constraints in which a middle rung Government Medical College in a developing country functions. The work conditions are presumably worse in smaller health facilities. A lot of medical actions are dictated by experience, many of them may be unjustified. There is an urgent need to generate evidence that is relevant to our population and to impart such updated knowledge to the health care providers.
In the present study we did not find any HIV positive subject with malaria which is very significant. That these subjects were under direct and regular ANC at the Medical College meant that they were spared this and other morbidities. This once again emphasises the impact that good ANC can have on improving maternal-fetal outcome in pregnancy.
The birth weight of neonates of peripheral malaria +ve subjects was 150 g less and of placental malaria +ve subjects was 290 g less than malaria −ve subjects reflecting long standing intrauterine distress (Fig. 3). LBW is the single greatest risk factor for neonatal and infant mortality in placental malaria subjects in our study. Majority had fetal distress which either resulted in increased need of neonatal intensive care or increased mortality.
Conclusion(s)
The effect of malaria, particularly placental malaria on maternal-fetal outcome is devastating. Efforts must be made to find out the constraints in the use of antimalarial measures by the population and/or its limitations and to address them effectively, in addition to raising awareness about the adverse impact of malaria in pregnancy.
The present study included only pregnant subjects with fever (present or past) during pregnancy. However, afebrile malaric subjects stand the risk of complications like chronic anemia and ill health, IUGR, prematurity, IUD, fetal distress and SB amongst others. Studies which include all pregnant subjects with adverse maternal or fetal outcome with or without fever should be carried out so that the exact burden of malaria in pregnancy may be ascertained.
Acknowledgments
I owe my sincere thanks to the Dean of Government NSCB Medical College, Jabalpur, India for permitting me to carry out this study. This study was impossible without the able guidance and help of Dr Neeru Singh, Director, Regional Malaria Research Centre for Tribals, ICMR, Jabalpur,who supported us at every step. Mr A. Kavishwar, Biostatistician ICMR, Jabalpur helped us with the mammoth task of data evaluation. I thank all my colleagues for their able guidance and help.
Conflict of interest
None declared.
Ethical Standard
The study was approved by the Ethics Approval Committee of Government NSCB Medical College and Hospital, Jabalpur in its meeting on 20 July 2008.
References
- 1.Murray CJL, Lopez AD. The global burden of disease 1990–1920: alternative projections of mortality and disability by cause for eight regions. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Kondrachine AV. Malaria in WHO South East Asia Region. Indian J Malariol. 1992;29:29–160. [PubMed] [Google Scholar]
- 3.Brabin BJ. An analysis of malaria in pregnancy in Africa. Bull World Health Organ. 1983;61:1005–1016. [PMC free article] [PubMed] [Google Scholar]
- 4.Das BS, Satpathy SK, Mohanty D, Mohanty, et al. Hypoglycemia in severe falciparum malaria. Trans Roy Soc Trop Med Hyg. 1988;82:197–201. doi: 10.1016/0035-9203(88)90407-5. [DOI] [PubMed] [Google Scholar]
- 5.Blacklock DB, Gordon RM. Malaria infection as it occurs in late pregnancy; its relationship to labour and early infancy. Annu Trop Med Parasitol. 1975;19:327–365. [Google Scholar]
- 6.Brabin BJ. The risks and severity of malaria in pregnant women. Applied Field Research in Malaria Reports No. 1. World Health Organization, Geneva. 1991;1:21–5.
- 7.Shulman CE, Dorman EK. Reducing childhood mortality in poor countries: importance and prevention of malaria in pregnancy. Trans Roy Soc Trop Med Hyg. 2003;97:30–35. doi: 10.1016/S0035-9203(03)90012-5. [DOI] [PubMed] [Google Scholar]
- 8.Mcgregor IA, Wilson ME, Billewicz WZ. Malaria infection in Gambia, West Africa; its incidence and relationship to stillbirth, birth weight and placental weight. Trans Roy Soc Trop Med Hyg. 1983;77:232–244. doi: 10.1016/0035-9203(83)90081-0. [DOI] [PubMed] [Google Scholar]
- 9.Nosten F, McGready R, Simpson JA, et al. Effects of Plasmodium vivax malaria in pregnancy. Lancet. 1999;354:546–549. doi: 10.1016/S0140-6736(98)09247-2. [DOI] [PubMed] [Google Scholar]
- 10.Jellife DB. Infant nutrition in the tropics and subtropics. 2nd ed. WHO monograph series; 1968. p. 29 [PubMed]
- 11.Steketee RW, Wirima JJ, Hightower AW, et al. The effect of malaria and malaria prevention in pregnancy on offspring birth weight, prematurity and intrauterine growth retardation in rural Malawi. Am J Trop Med Hyg. 1996;55:S33–S41. doi: 10.4269/ajtmh.1996.55.33. [DOI] [PubMed] [Google Scholar]
- 12.Singh N, Saxena A. Usefullness of rapid on-site Plasmodium falciparum diagnosis (ParacheckR Pf) in forest migrants and among the indigenous population at the site of their occupational activities in Central India. Am J Trop Med Hyg. 2005;72:26–29. [PubMed] [Google Scholar]
- 13.Singer LM, Newman RD, Diarra A, et al. Evaluation of a malaria rapid diagnostic test for assessing the burden of malaria during pregnancy. Am J Trop Med Hyg. 2005;72:236–242. [PubMed] [Google Scholar]
- 14.Kassam SN, Nesbitt S, Hunt LP, et al. Pregnancy outcomes in women with or without placental malaria infection. Int J Gynaecol Obstet. 2006;93:225–232. doi: 10.1016/j.ijgo.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 15.Singh N, Shukla MM, Sharma VP. Epidemiology of malaria in pregnancy in Central India. Bull World Health Organ. 1999;77:567–571. [PMC free article] [PubMed] [Google Scholar]
- 16.Singh N, Dash AP, Thimasarn K. Fighting malaria in Madhya Pradesh (Central India): are we loosing the battle? Malar J. 2009;93:26–29. doi: 10.1186/1475-2875-8-93. [DOI] [PMC free article] [PubMed] [Google Scholar]