Introduction
Gestational trophoblastic diseases (GTD) presents most commonly as molar pregnancy or complete mole in the form of fluid filled vesicles, looking like a bunch of grapes and snow storm appearance on USG. The commonest symptom being irregular vaginal bleeding preceded by amenorrhoea. Uterine arteriovenous malformation with GTD is a very uncommon disorder and can be diagnosed by arteriography or color doppler. We present a case of GTD which was diagnosed as an invasive mole with a unique and unusual morphologic feature of arteriovenous malformation.
Case Report
In 2004 a 19-year-old primigravigda presented with 6 weeks of amenorrhoea followed by slight vaginal bleeding. She consulted a doctor who treated her conservatively in the line of threatened abortion. But after 1 week when she started having profuse bleeding she was attended to district hospital where dilatation and curettage was done as a case of incomplete abortion. Following this operation she had two more episodes of 2 month amenorrhoea and bleeding and each time dilatation and curettage was done but fortunately in the last episode as the bleeding was so profuse, the procedure was stopped and USG performed showed vascular malformation present at the uterine wall with presence of blood clot with in the uterine cavity. She was transfused two units of blood and referred to a tertiary center.
She reported with bleeding per vaginum on 26.11 05 she was thoroughly evaluated. From the history possibility of gestational trophoblastic disease was thought of and detailed investigations were carried out.
General examination revealed marked pallor, mild tachycardia with blood pressure of 100/60 mmHg. Systemic examination revealed no abnormality. On vaginal examination uterus was 6–8 weeks size, no adnexal mass was felt.
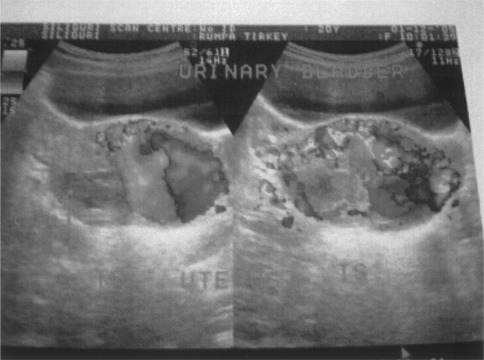
Investigations showed hemoglobin 6 g/dl, and serum Beta HCG 30,000 mlU/ml with LFT, X-ray chest and ECG were within normal limits. On USG with color doppler, uterus was bulky with large vascular malformation within the myometrium (Figs. 1, 2) near the left cornu. Uterine cavity was filled with echogenic material, no gestational sac was found. A clinical diagnosis of invasive mole was made.
Fig. 1.
Fig. 2.
Her general condition improved after giving 4 units of blood transfusion. It was decided to give her chemotherapy and accordingly she was investigated. However, on 3.12.05 at 10 pm she experienced slight lower abdominal pain and had a bout of severe vaginal bleeding and went into a state of shock. She was resuscitated with all available means and all conservative attempts which failed to control bleeding. Ultimately decision for hysterectomy was taken to save her life. At laparotomy no defect was found in the serosal layer of the uterus, no uterine perforation was detected but an area of hyperemia and contusion was discovered on die posterior aspect of left cornu.
She received 4 units of blood transfusion. Her postoperative period was uneventful. She has been put on multiagent chemotherapy (EMACO). Histopathological report showed invasive mole. Her serum beta HCG level became normal (2.6 mIU/ml) within 2 months of therapy. She had regular follow up and was well after 1 year.
Discussion
Uterine arteriovenous malformations (AVM) are very uncommon [1]. Successful conservative treatment with subsequent pregnancy is rarely reported [1, 2]. Previous trophoblastic neoplasia is a common predisposing factor [3]. The need for hysterectomy in a case of GTD in young women where family is not completed is very limited. Life threatening hemorrhage is the indication in such a case. Selective embolisation of complex and large AVM is feasible for the treatment of uterine bleeding and reproductive capability [1, 2, 4]. In the present case we initially thought of the possibility of perforating mole and hemoperitoneum but it turned out to be a case of ruptured AVM which resulted in relentless life threatening hemorrhage. The patient had to sacrifice her uterus due to lack of facilities of arterial embolisation in our set up.
References
- 1.Tsai CC, Cheng YF, Changchein CC, et al. Succesful term pregnancy after selective embolisation of a large post molar uterine arteriovenous malformation. 2006;1:439–41. [DOI] [PubMed]
- 2.Kelly FW. Forceps delivery after molar pregnancy in a woman with arteriovenous malformation. A case report. J Reprod Med. 2001;46:1013–1016. [PubMed] [Google Scholar]
- 3.MaLachln MS, Bird CC, Naiem EA et al. Uterine cirsoid aneurysm. Br J Obstet Gynaecol. 1978;85:390–5. [DOI] [PubMed]
- 4.Yang JJ, Xlang Y, Wan XR, et al. Diagnosis and management of uterine arteriovenous fistula with massive vaginal bleeding. 2004;39:797–800. [PubMed]