Abstract
The rapid identification and antibiotic susceptibility testing of Yersinia pestis is paramount for a positive prognosis. We previously engineered a Y. pestis-specific ‘bioluminescent’ reporter phage for the identification of Y. pestis. In this study, we generated an improved reporter phage and evaluated the ability of this phage to provide direct and rapid susceptibility testing. Compared to the first generation reporter, the second generation reporter exhibited a 100-fold increase in signal strength, leading to a 10-fold increase in assay sensitivity. Y. pestis antimicrobial testing in the presence of the reporter elicited bioluminescent signals that were drug concentration-dependent, and produced susceptibility profiles that mirrored the standard CLSI method. The phage-generated susceptibility profiles, however, were obtained within hours in contrast to days with the conventional method.
Keywords: plague, reporter phage, detection, bioluminescence, antibiotic susceptibility testing
Yersinia pestis is a category A bacterial pathogen and the etiological agent of the plague. This contagious disease has important bioterrorism implications and is considered a reemerging disease (Galimand et al., 2006, Higgins, 2004, Stenseth et al., 2008). Following symptom onset, rapid diagnosis is essential since the plague is usually fatal if not treated within the first 24-36 h (Woods, 2005). Y. pestis isolates are not typically drug resistant; however, a streptomycin-resistant strain, and a multidrug resistant (MDR) strain were isolated from bubonic plague patients in Madagascar (Galimand, Carniel and Courvalin, 2006, Guiyoule et al., 2001). The MDR strain was resistant to antibiotics (e.g. streptomycin, tetracycline, chloramphenicol) that are frequently used in therapy or prophylactic antibiotic regimes for the plague. Resistance was mediated by a transmissible plasmid that is common to other MDR pathogens such as Escherichia coli, Klebsiella sp., and Salmonella serotypes (Welch et al., 2007). Although the MDR plasmid backbone has not been detected in Y. pestis isolates from the U.S. (Wagner et al., 2010), the plasmid could be potentially transferred to Y. pestis from other common MDR zoonotic pathogens and thus is a significant public health concern (Galimand, Carniel and Courvalin, 2006, Galimand et al., 1997). In addition, the threat exists of deliberately engineered resistant strains being released during a bioterrorist event. Unfortunately, Y. pestis is inherently slow growing (doubling time of 1.25 h at 28°C), and thus antibiotic susceptibility profile determination using the standard culture techniques can take up to 48 h (Frean et al., 2003). Therefore, methods that can rapidly diagnose, and simultaneously determine whether the isolate is resistant or sensitive to different antibiotics, are of value.
Phage lysis assays using the phage ϕA1122 are used by the CDC and the USAMRIID for the confirmed identification of Y. pestis (Chu, 2000). Although the phage lysis assays provide definitive identification, the assays require bacterial isolation, cultivation, and take approximately 48 h to complete. In order to simplify the detection procedure and reduce the time to positive identification, we previously created a Y. pestis reporter phage by integrating the bacterial luxAB reporter genes into the genome of the CDC plague diagnostic phage ϕA1122 (Schofield et al., 2009). The “light-tagged” reporter phage, when incubated in the presence of viable Y. pestis cells, specifically infected the host, and then used the host’s transcriptional and translational machinery to elicit a bioluminescent response. Since the phage infection process and signal generation is strictly dependent on the host, only phage-sensitive and metabolically active cells can elicit a bioluminescent response. Herein, we investigate the ability of the reporter phage to transduce a bioluminescent signal to Y. pestis in the presence of antibiotics, and demonstrate that cell fitness, and hence signal response is correlated to antibiotic susceptibility. Moreover, the antibiotic susceptibility profile determined by the bioluminescent response is comparable to the Clinical and Laboratory Standards Institute (CLSI) microdilution method with the exception that the profile can be obtained within hours instead of days.
The CLSI broth microdilution method for determining antibiotic susceptibility requires a fairly low initial bacterial concentration (~5 × 105 CFU/mL), cells which have been harvested directly from a plate, and a non-optimal Y. pestis growth temperature of 35°C (Chu, 2001). The magnitude of the reporter phage mediated bioluminescent response is correlated to bacterial concentration, and 105 CFU/mL is near the lower limit of detection of the reporter phage. Therefore, in order to increase the bioluminescent signal response and hence the detection sensitivity of viable Y. pestis, a second generation reporter phage was constructed. Unlike our initial reporter phage, which relied on transcription from host promoters on the phage genome to drive luxAB expression, the new construct has the luxAB genes placed under the transcriptional control of a strong ϕA1122 promoter. LuxAB was integrated by homologous recombination between the capsid protein gene 10 and the transcription terminator Tϕ at position 21781 bp of ϕA1122 (GenBank Accession # AY247822). Gene 10 codes for the most abundant ϕA1122 protein, and its gene is transcribed not only from its own promoter ϕ10 but also from all upstream phage promoters. We therefore reasoned that placing luxAB downstream of gene 10, with an additional late promoter, would maximize transcription and elicit a strong bioluminescent phenotype after infection of Y. pestis. PCR analysis using primers spanning the 5′ and 3′ integration junctions was used to demonstrate that the luxAB genes were integrated at the predicted site (data not shown).
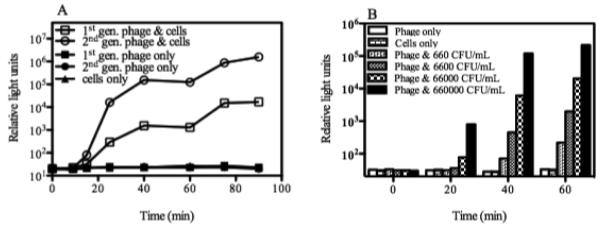
In the current report, the ability of the first and second generation reporter phages to elicit a bioluminescent response upon infection of the attenuated Y. pestis A1122 strain was compared. The approach described previously for assaying the signal response mediated by the first generation phage was employed (Schofield., 2009). Y. pestis A1122 is specified as an exempt select agent strain, which lacks the pgm locus and the pCD1 plasmid; A1122 is therefore commonly used in research laboratories to avoid select agent restrictions. Infection of Y. pestis with either the first or second generation reporter phages gave comparable signal response times of 20 min or less (Fig. 1A). At each time point analyzed, however, the magnitude of the signal strength (relative light units) of the second generation reporter phage was approximately 100-fold higher than our initial reporter (Fig. 1A), enabling detection of a bacterial concentration of 660 CFU/mL in 40 min (Fig. 1B). This corresponds to about a 10-fold increase in sensitivity of our new reporter phage (Schofield., 2009). The human infectious aerosolized dose for Y. pestis is estimated to be 100-15,000 CFU (Woods, 2005) and 102 CFU/mL in the blood can be fatal (Butler et al., 1976), this improvement in assay sensitivity is therefore essential for both antimicrobial susceptibility testing and the development of the reporter phage into a clinical diagnostic.
Fig. 1.
Reporter phage-mediated bioluminescent detection of Y. pestis. A. Signal response time and signal strength. The ability of the first and second generation (1st gen., and 2nd gen.) reporter phages to transduce a bioluminescent signal response to Y. pestis was compared. Y. pestis was grown in Luria Bertani broth at 28°C to an A600 of approximately 0.2. At time 0, cells (~1 × 108 CFU/mL) were mixed with the reporter phage (multiplicity of infection [MOI] of 0.5) and incubated at 28°C. Bioluminescence (RLU) was measured over time following the addition of the substrate n-decanal. Numbers are the mean (n=3) ± SD. B. Dose-dependent detection. 10-fold serial dilutions of a Y. pestis culture were mixed with the second generation reporter phage and incubated at 28°C. Bioluminescence (RLU) was measured over time following the addition of n-decanal. Numbers are the mean (n=3) ± SD.
The time required to determine the antibiotic susceptibility profile of Y. pestis isolates using the standard CLSI microdilution method requires up to 48 h (Frean et al., 2003). Since the phage-mediated bioluminescent signal response is correlated to the fitness of the host cell, we investigated the ability of the second generation phage to elicit a bioluminescent signal response in the presence of antibiotics to determine if the reporter phage could rapidly provide a susceptibility profile. Y. pestis A1122 cells were prepared according to the standard broth microdilution method (Institute, 2009) to a concentration of 5 × 105 CFU/mL in cation-adjusted Mueller Hinton broth. The three main antimicrobial drugs that are recommended to treat plague infections are chloramphenicol, tetracycline, and streptomycin (Bames and Quan, 1992). These drugs are also suggested by CLSI for testing against bioterrorist agents (Institute, 2010). Cells were incubated with a range of chloramphenicol, tetracycline, or streptomycin concentrations in 96 well round bottom microtiter plates and incubated at 35°C. An internal quality control strain was used to ensure antimicrobial effectiveness (data not shown). Growth was assessed at A625 after 40 h at 35°C (Fig. 2). Y. pestis growth was susceptible to the presence of chloramphenicol, tetracycline, and streptomycin as expected and produced MICs of approximately 4, 2, and 4 μg/mL respectively (Figs. 2A, B & C); these values are consistent with those that have been reported for wild-type virulent isolates (Wong et al., 2000).
Fig. 2.
Antibiotic susceptibility profiles of Y. pestis grown in the presence of chloramphenicol (A), tetracycline (B), or streptomycin (C). Inocula (~5 × 105 CFU/mL prepared directly with colonies from a freshly grown plate) and antibiotics were prepared according to the CLSI microdilution method. Cells were incubated at 35°C and assessed for growth (A625) after 40 h (right axis). Reporter phage were mixed with cells 60 min (A, B) or 120 min (C) after the addition of antibiotic. Bioluminescence (relative light units, left axis) was measured 30-40 minutes following the addition of n-decanal. Numbers are the mean (n=3) ± SD.
To compare the phage-mediated bioluminescent signal response of Y. pestis incubated under the same conditions, reporter phage were added to comparably prepared Y. pestis cells either 60 min (chloramphenicol & tetracycline) or 120 min (streptomycin) after the addition of the antibiotic. Bioluminescence was subsequently measured 30-40 min after phage infection. The bioluminescence signal response profile mirrored the growth profile in the presence of the antibiotics (Figs. 2A, B & C). At antibiotic concentrations that had little to no effect on growth, the bioluminescent signal response from the reporter phage was near maximum. Conversely, at antibiotic concentrations that were at the MIC or higher, the signal responses were significantly reduced, or were comparable to background levels. Thus, in the presence of non-inhibitory or inhibitory antibiotic concentration, the bacterial growth profile and the phage-mediated bioluminescent signal response, as mediated by the ‘fitness’ of the host, were very similar. The MIC determined by the reporter phage may be defined as the lowest concentration of antibiotic that prevents phage-mediated bioluminescence. By this definition, the reporter MIC is likely to be higher than the standard method primarily because of the sensitivity of the assay. Nevertheless, the reporter phage may be used to rapidly (within 120-180 minutes) determine whether strains are susceptible or resistant to particular antibiotics. Because the phage ϕA1122 is used in confirmatory lysis assays for identification of Y. pestis, and because reporter phage can be used directly in conjunction with clinical specimens (Schofield., 2009), the potential exists for the ‘bioluminescent’ reporter phage to simultaneously detect the presence of Y. pestis, and to obtain antibiotic susceptibility information. A strategy is being employed for the identification and drug susceptibility testing of Mycobacterium tuberculosis isolates using recombinant mycobacteriophages (Jacobs et al., 1993).
In conclusion, the signal output of the Y. pestis reporter phage was improved 100-fold by re-engineering the CDC plague diagnostic phage. This modification also enabled the reporter phage system to rapidly gather antibiotic susceptibility information. In the presence of antibiotics, the bioluminescent signal response profile mirrored the growth profile. Compared to the standard CLSI method, the time required for the reporter phage to provide data was reduced from days to hours. Since plague is an infectious disease, and is usually fatal if not treated within the first 24-48 h after symptom onset, tools such as the reporter phage that can rapidly diagnose and simultaneously gather antibiotic susceptibility information, should help patient prognosis.
Acknowledgement
This research was supported by award numbers R43AI082698 and R44AI082698 from the National Institute of Allergy and Infectious Diseases (to D.A.S of Guild Associates, Inc). We thank Dr. Alexander Sulakvelidze (University of Florida) and Dr. Michael Schmidt (Medical University of South Carolina) for their advice and support. We also thank the Medical University of South Carolina Biotechnology Resource laboratory for sequencing data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bames AM, Quan TJ. Plague. In: Gorbach SL, Bartlett JG, Blacklow NR, editors. Infectious diseases. W. B. Saunders Company; Philadelphia: 1992. [Google Scholar]
- Butler T, Levin J, Linh NN, Chau DM, Adickman M, Arnold K. Yersinia pestis infection in Vietnam. II. Quantiative blood cultures and detection of endotoxin in the cerebrospinal fluid of patients with meningitis. J. Infect. Dis. 1976;133:493–499. doi: 10.1093/infdis/133.5.493. [DOI] [PubMed] [Google Scholar]
- Chu MC. Laboratory manual of plague diagnostic tests. Centers for Disease Control and Prevention., CDC; Atlanta: 2000. [Google Scholar]
- Chu MC. Basic laboratory protocols for the presumptive identification of Yersinia pestis. Centers for Disease Control and Prevention; 2001. pp. 1–19. [Google Scholar]
- Frean J, Klugman KP, Arntzen L, Bukofzer S. Susceptibility of Yersinia pestis to novel and conventional antimicrobial agents. J. Antimicrob. Chemother. 2003;52:294–296. doi: 10.1093/jac/dkg363. [DOI] [PubMed] [Google Scholar]
- Galimand M, Carniel E, Courvalin P. Resistance of Yersinia pestis to antimicrobial agents. Antimicrob. Agents Chemother. 2006;50:3233–3236. doi: 10.1128/AAC.00306-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Carniel E, Courvalin P. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. New Eng. J. Med. 1997;337:677–680. doi: 10.1056/NEJM199709043371004. [DOI] [PubMed] [Google Scholar]
- Guiyoule A, Gerbaud G, Buchrieser C, Galimand M, Rahalison L, Chanteau S, Courvalin P, Carniel E. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg. Infect. Dis. 2001;7:43–48. doi: 10.3201/eid0701.010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins R. Emerging or re-emerging bacterial zoonotic diseases: bartonellosis, leptospirosis, Lyme borreliosis, plague. Rev. Sci. Tech. 2004;23:569–581. doi: 10.20506/rst.23.2.1503. [DOI] [PubMed] [Google Scholar]
- Institute. Clinical Laboratories Standard Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically. Approved Standard-Eighth Edition 2009.
- Institute. Clinical Laboratories Standard Performance Standards for Antimicrobial Susceptibility Testing. 2010.
- Jacobs WR, Jr., Barletta RG, Udani R, Chan J, Kalkut G, Sosne G, Kieser T, Sarkis GJ, Hatfull GF, Bloom BR. Rapid assessment of drug susceptibilities of Mycobacterium tuberculosis by means of luciferase reporter phages. Science. 1993;260:819–822. doi: 10.1126/science.8484123. [DOI] [PubMed] [Google Scholar]
- Schofield DA, Molineux IJ, Westwater C. Diagnostic bioluminescent phage for detection of Yersinia pestis. J. Clin. Microbiol. 2009;47:3887–3894. doi: 10.1128/JCM.01533-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenseth NC, Atshabar BB, Begon M, Belmain SR, Bertherat E, Carniel E, Gage KL, Leirs H, Rahalison L. Plague: past, present, and future. PLoS Med. 2008;5:e3. doi: 10.1371/journal.pmed.0050003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner DM, Runberg J, Vogler AJ, Lee J, Driebe E, Price LB, Engelthaler DM, Fricke WF, Ravel J, Keim P. No resistance plasmid in Yersinia pestis, North America. Emerg. Infect. Dis. 2010;16:885–887. doi: 10.3201/eid1605.090892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch TJ, Fricke WF, McDermott PF, White DG, Rosso ML, Rasko DA, Mammel MK, Eppinger M, Rosovitz MJ, Wagner D, Rahalison L, Leclerc JE, Hinshaw JM, Lindler LE, Cebula TA, Carniel E, Ravel J. Multiple antimicrobial resistance in plague: an emerging public health risk. PLoS One. 2007;2:e309. doi: 10.1371/journal.pone.0000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong JD, Barash JR, Sandfort RF, Janda JM. Susceptibilities of Yersinia pestis strains to 12 antimicrobial agents. Antimicrob. Agents Chemother. 2000;44:1995–1996. doi: 10.1128/aac.44.7.1995-1996.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods JB. USAMRIID’s Management of Biological Casualties Handbook. 2005.