Abstract
Nutrition facts panels (NFPs) contain a rich assortment of nutrition information and are available on most food packages. The importance of this information is potentially even greater among older adults due to their increased risk for diet-related diseases, as well as those with goals for dietary modifications that may impact food choice. Despite past work suggesting that knowledge and motivation impact attitudes surrounding and self-reported use of NFPs, we know little about how (i.e., strategies used) and how well (i.e., level of accuracy) younger and older individuals process NFP information when evaluating healthful qualities of foods. We manipulated the content of NFPs and, using eye tracking methodology, examined strategies associated with deciding which of two NFPs, presented side-by-side, was healthier. We examined associations among strategy use and accuracy as well as age, dietary modification status, knowledge, and motivation. Results showed that, across age groups, those with dietary modification goals made relatively more comparisons between NFPs with increasing knowledge and motivation; but that strategy effectiveness (relationship to accuracy) depended on age and motivation. Results also showed that knowledge and motivation may protect against declines in accuracy in later life and that, across age and dietary modification status, knowledge mediates the relationship between motivation and decision accuracy.
Keywords: decision making processes, nutrition knowledge, motivation, dietary modifications, food labels, nutrition facts panels, aging
Greater adherence to a healthy diet may reduce the impact of numerous diseases that increase in frequency in later life such as osteoporosis, obesity, high blood pressure, diabetes, heart disease, and certain cancers (Department of Agriculture, 2004; U.S. Department of Health and Human Services, 2000). One of the goals of U.S. federal regulation of the 1990s was to expand the ability of food labels to communicate health information thereby improving dietary quality and reducing the incidence of chronic disease and related healthcare costs. The nutrition facts panel (NFP) was designed to help carry out these goals by communicating information on key nutrients, as well as other important information such as calories, serving size, and percent daily values. However, nutrition facts tables are common in many other countries as well. In the US and abroad, researchers are concerned about food label communication and the extent to which food labels can improve diet and prevent chronic disease (Grunert & Wills, 2007; Mhurchu & Gorton, 2007; van Trijp & van der Lans, 2007). Consumers in 56 countries report misunderstanding and mistrusting food labels (Neilsen Company, 2012).
There is some evidence that NFP use is associated with healthy dietary behaviors. Individuals who use labels are more likely to seek nutrition information and to eat healthy foods (Choinière & Lando, 2008; Golan, Kuchler, & Krissoff, 2007; Lin, Lee, & Yen, 2004; Neuhouser, Kristal, & Patterson, 1999; Ollberding, Wolf, & Contento, 2010; Post, Mainous Iii, Diaz, Matheson, & Everett, 2010; Teisl & Levy, 1997; Variyam, 2008; Variyam & Golan, 2002). However, most studies rely on correlational data, making it unclear whether food labels are responsible for healthier diets. Indeed, some evidence suggests that NFPs fall short of their potential to impact behavior (Balasubramanian & Cole, 2002; Golan et al., 2007; Kristal, Levy, Patterson, Li, & White, 1998; Wills, Schmidt, Pillo-Blocka, & Cairns, 2009). According to one estimate, only 54% of consumers read a product’s label when purchasing a food for the first time (Choinière & Lando, 2008) and proportions are comparable across age groups (Ollberding et al., 2010). Given these data are based on self-report measures, actual use could be far lower. In general, there appears to remain a good deal of opportunity to increase label communication and use. Although past research has increased our understanding of perceived and actual difficulty surrounding NFP use (Burton & Andrews, 1996; Byrd-Bredbenner & Kiefer, 2000; Levy & Fein, 1998), as well as our understanding of the frequency with which individuals report using NFPs (Lin et al., 2004; Post, Mainous, Diaz, Matheson, & Everett, 2010), we still know little about how NFPs are processed when making decisions.
The goal of the present study was to add to the literature by examining strategies that individuals use to make decisions based on NFP information and the extent to which strategies are influenced by person factors of age, dietary modification status, knowledge, and motivation. To assess strategies, we conducted a laboratory study in which we manipulated NFP information and tracked eye movements as individuals decided which of two NFPs was healthier. Eye tracking has been used to examine search behaviors of adults who are asked to make food purchasing decisions or locate information on food labels (Goldberg, Probart, & Zak, 1999b; Graham & Jeffery, 2011; van Herpen & van Trijp, 2011; Visschers, Hess, & Siegrist, 2010). Still, we know little about possible strategies used to evaluate NFP information and factors that affect strategy and accuracy. Eye tracking methodology is a useful way to measure strategies associated with NFP use because attentional processes can be assessed objectively as individuals evaluate and make decisions based on information in NFPs.
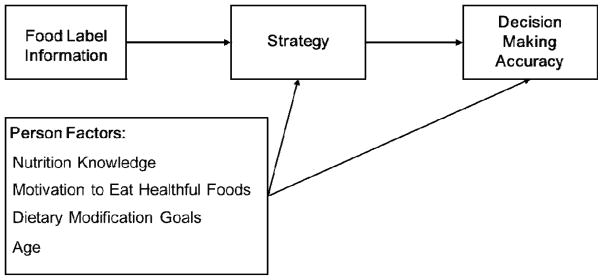
Knowledge and motivation have been identified as being important for nutrition information processing (Balasubramanian & Cole, 2002; Fitzgerald, Damio, Segura-Pérez, & Pérez-Escamilla, 2008; Grunert, Wills, & Fernández-Celemín, 2010; Miller, Gibson, & Applegate, 2010; Miller, Gibson, Applegate, & de Dios, 2011). Balasubramanian and Cole (2002) proposed a model in which nutrition knowledge and motivation to process nutrition information impact memory for nutrition information. We have built upon this general idea in our model, depicted in Figure 1. The questions that we addressed are: How do food label manipulations affect nutrition information processing and decision making accuracy; How do person characteristics impact processing and decision making accuracy? In addition to knowledge and motivation, we consider two additional person factors, dietary modification status and age. Decision making strategies and person factors are described below.
Figure 1.
Model of nutrition information processing as it pertains to decision accuracy.
Decision Making Strategies
Johnson’s (1990) framework for decision making strategies distinguishes between noncompensatory and compensatory strategies. Noncompensatory strategies are those that consider one type of information across options, for example, comparing total fat content on NFP 1 with total fat content on NFP 2 to determine which of two foods is more healthful. In contrast, compensatory strategies are those that consider more than one type of information within each food option such that one option compensates for another, for example, considering total fat and fiber in one NFP compared to comparing total fat across both NFP 1 and 2. Johnson found that older adults were more likely to use noncompensatory decision making strategies when making a laboratory-based mock car purchase decision and argued that they did so because this approach is less effortful than compensatory strategies. Although noncompensatory strategies could be easier in situations in which there are a small number of possible comparisons, this strategy could be cognitively demanding when many comparisons available. When using noncompensatory strategies to decide which of two NFPs is the more healthful choice, one could potentially make a large number of comparisons (a comparison between each nutrient value, for grams [/milligrams] as well as percent Daily Value), making the task effortful. Thus, when using noncompensatory strategies, the effects of dietary goals may be important for older adults in particular, and may rely on prior nutrition knowledge or motivation.
Person-Level Factors
Knowledge
Knowledge, both declarative and procedural, plays a critical role in virtually all areas of information processing. It facilitates exchanges from short-term/working memory to long-term memory (Ericsson & Kintsch, 1995), aides conceptual integration (Sharkey & Sharkey, 1987) and increases efficiency (Miller, 2009). Not surprisingly, evidence suggests that nutrition knowledge is important for a variety of health and diet decisions (Worsley, 2002). In fact, past research has shown that prior levels of knowledge are positively related to dietary quality, even after controlling for sociodemographic factors (Variyam & Golan, 2002; Wardle, Parmenter, & Waller, 2000). Knowledge of nutrition is related to perceptions of food healthfulness (Crites & Aikman, 2005), accuracy of label use (Burton, Garretson, & Velliquette, 1999; Fitzgerald et al., 2008; Grunert et al., 2010; Moorman, 1996), careful shopping behavior (Fusillo & Beloian, 1977), as well as food choice (Fitzgerald et al., 2008; Guenther, Jensen, Batres-Marquez, & Chen, 2005). Knowledge eliminated the Black-White differences in cancer-prevention behaviors, including diet (Jepson, 1990). Research shows that individuals with more years of education experienced the greatest improvement in diet quality over the course of several years (Popkin, Zizza, & Siega-Riz, 2003) which may be due to an increase in nutrition knowledge (Beydoun & Wang, 2008). Similarly, higher levels of baseline knowledge were more predictive of weight loss among obese, low-income mothers than were increases in knowledge as a result of an intervention (Klohe-Lehman et al., 2006). Importantly, Howlett et al. (2008) found that, among individuals who were interested in using label information, misinterpretation of nutrient information occurred when prior knowledge levels were low. In the present study, we expected that nutrition knowledge would support decision accuracy, a benefit that may be even greater among older adults (Miller, Gibson, et al., 2011).
Motivation
Although attempts to increase NFP use and improve dietary quality through nutrition knowledge are important (Ammerman, Lindquist, Lohr, & Hersey, 2002; Patterson, Frank, Kristal, & White, 2004; Posner, Jette, Smith, & Miller, 1993), knowledge alone is unlikely to be sufficient to encourage individuals to make healthful food choices (Nebeling, Yaroch, Seymour, & Kimmons, 2007) and may also be insufficient to support accurate healthfulness decisions in a laboratory task. Motivational factors pertaining to health behaviors may be necessary for compliance with what individuals already know to be important for health (Bandura, 2005; Leventhal & Mora, 2005). The Transtheoretical Model (Prochaska & DiClemente, 2005) emphasizes the importance of an individual’s readiness to change when considering how to approach changes in health behaviors. In the present study, we explored whether individuals in more advanced stages of change pertaining to dietary quality (e.g., have been eating healthy foods for 6 months or more, compared to those who have not thought about eating healthy foods) would be more motived to make informed decisions than those in less advanced stages.
There is reason to believe that motivation may be a more important factor for older relative to younger adults due to age-related decreases in the opportunities to exert direct control over one’s environment (Heckhausen, Wrosch, & Schulz, 2010). Moreover, research conducted on younger adults suggests that knowledge can remain inert without sufficient support to apply the knowledge to the immediate task at hand (Boekaerts, 1996; Bransford, Brown, & Cocking, 1999; Kintsch, 1998). Thus, for younger and older adults, motivation could be an important factor in using knowledge to make food-related decisions.
Dietary Modification Goals (DMGs)
Individuals who modify their diets to include or exclude certain foods or nutrients may be more goal-directed in their approach to food selection which may impact their decision making based on food labels. Dietary modification goals (DMGs), as defined in the present study, include any self-identified dietary goal that represents a change or modification relative to a perceived norm. DMGs of this sort could include food restrictions per a health professional’s recommendation to change one’s diet due to a chronic condition (sodium for hypertension), food allergies (nuts, wheat), values (vegetarian, “locavore”) or general health (increased fiber, decreased saturated fat). Goals can positively impact health behaviors (Artinian et al., 2010; Miller, Headings, Peyrot, & Nagaraja, 2011). Our assumption was that individuals who report having dietary restrictions are goal-directed in their approach to food choice which influences how they process nutrition information on food packages. Specifically, goal-directed individuals may have a greater propensity to use the cognitive resources they have to more fully engage in the decision making process. In this sense, goals may motivate individuals to make more informed decisions. Thus, these individuals might be more inclined to apply a) the nutrition knowledge or b) motivation that they possess to the task at hand. It is unclear whether goal-directed influences change with age. Although many dietary changes come with the onset of chronic conditions in later life (Freedman, Martin, & Schoeni, 2002), knowledge and motivation may be larger moderators of the effects of dietary modification status on food-related decision making than chronological age.
Aging
Changes in later life may also impact how nutrition information on food labels is processed. In addition to increased chronic illnesses that require changes in diet (Post, Mainous, et al., 2010), there are age-related changes in basic cognitive abilities that may alter how information is processed and decisions are made. For example, age declines in working memory, the maintenance and manipulation of information in short-term memory, may make it more difficult to activate and maintain information long enough to interpret its relevance. Older adults may compensate for challenges such as these through a goal-directed approach to food selection that may accompany dietary modification goals or through a reliance on prior knowledge or motivation (Miller et al., 2010; Miller, Gibson, et al., 2011; Morrow et al., 2005; Wrosch & Schultz, 2008).
Method
We assessed information processing strategies as individuals compared two NFPs to decide which was more healthful. Consumers often use NFPs to compare products before deciding which to purchase (Guthrie, Derby, & Levy, 1999); however, they sometimes avoid using nutrition information when evaluating food healthfulness (Aikman & Crites, 2007). Strategies were investigated using eye tracking methodology. Eye movements were monitored as individuals considered information on two NFPs presented side by side on a computer screen.
Participants
We tested a community-based, convenience sample of 43 younger adults and 32 older adults. Participants were screened for a variety of eye and vision factors that could limit our ability to obtain reliable estimates of attention from eye movements (e.g., macular degeneration, cataracts). Even so, we were unable to calibrate 3 younger and 5 older adults to the eye tracker, resulting in a sample of 40 younger (ages 19–34, M = 22.3; SD = 3.8) and 27 older adults (ages 61–78, M = 68.7; SD = 5.0).
Definitions of DMGs are varied and can be limited to recommendations from healthcare providers to change diet in response to potential or actual chronic conditions (Post, Mainous, et al., 2010). In the present study, however, we did not limit the source of DMGs under the assumption that modification goals, regardless of their source, could be important for how one approaches decision making. On a sheet of paper, participants were asked to respond to the question “Do you have any diet-related restrictions?” Participants received a 1 if they responded yes and 0 if they responded no. The final sample consisted of 12 younger and 14 older adults with dietary modification goals, DMGs, and 28 younger and 13 older adults without dietary modification goals, no-DMGs. Below, we describe dietary modification groups and age groups to determine whether groups differed in terms of health, cognition, or frequency of NFP use. Dietary modification status may reflect age-related changes in health. Therefore, we contrast groups independently then compare age differences in these variables within dietary modification groups. In general, there were few differences between DMGs and no-DMGs on these background variables. Table 1 (first two columns) shows that the only difference was that those in the DMG group had a higher number of medications than those in the no-DMG group.
Table 1.
Means (and Standard Deviations) of Individual Difference Variables by Age and Dietary Modification Status.
| No-DMG | DMG | Younger Adults | Older Adults | No-DMG | DMG | |||
|---|---|---|---|---|---|---|---|---|
| Younger Adults (n=28) | Older Adults (n=13) | Younger Adults (n=12) | Older Adults (n=14) | |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| NFP Frequency of Use | 3.3a (0.76) | 3.3a (0.80) | 3.2a (0.76) | 3.5a (0.76) | 3.2a (0.82) | 3.7a (0.49) | 3.3a (0.62) | 3.4a (0.94) |
| Working Memory Capacity | 5.59a (1.11) | 5.63a (1.22) | 5.80a (1.14) | 5.31a (1.11) | 5.83a (1.12) | 5.07b (0.93) | 5.74a (1.22) | 5.54a (1.25) |
| Speed of Processing | 31.66a (6.56) | 30.48a (5.48) | 34.37a (5.25) | 26.50b (4.01) | 34.36a (5.79) | 25.85b (3.78) | 34.42a (3.92) | 27.11b (4.27) |
| Education (years) | 16a (2.02) | 17a (2.62) | 15a (1.65) | 17b (2.56) | 16a (1.55) | 17a (2.67) | 15a (1.86) | 18b (2.42) |
| Chronic Conditions | .05a (0.22) | .15a (0.37) | .00a (0.00) | .22b (0.42) | .00a (0.00) | .15b (0.38) | .00a (0.00) | .29b (0.47) |
| Body-Mass Index | 23.7a (3.53) | 23.3a (3.61) | 22.6a (3.77) | 25.0b (2.59) | 23.2a (3.93) | 24.7a (2.25) | 21.2a (3.05) | 25.3b (2.95) |
| Medications (number) | 1a (1.01) | 2b (1.92) | 0a (0.74) | 2b (1.74) | 0a (0.48) | 1b (1.39) | 0a (1.16) | 3b (1.91) |
| Health (general) | 2a (0.66) | 2a (0.71) | 2a (0.66) | 1b (0.56) | 2a (0.65) | 1b (0.44) | 2a (0.67) | 2b (0.65) |
| Vision (acuity) | .07a (0.06) | .08a (0.05) | .10a (0.00) | .04b (0.07) | .10a (0.00) | .02b (0.08) | .10a (0.00) | .06b (0.06) |
Note: DMG=dietary modification goals; NFP=Nutrition Facts Panel; Values in the same row and subtable not sharing the same subscript are significantly different at p< 0.05 in the two-sided test of equality for column means.
In comparing the two age groups, we found that older adults were generally high functioning and in good health relative to younger adults. The means presented in Table 1 (columns 3 and 4) show that older adults had higher self-reported general health relative to younger adults as indicated on a scale of 1 (excellent) to 5 (poor). Nevertheless, body mass index (BMI) and number of prescription medications were higher for older relative to younger adults. Similarly, older adults had a higher number of chronic conditions (based on a check list of 7 conditions) and poorer vision as assessed by a Snellen visual acuity test. Older adults had more years of education but, using one-tailed test, t(65) = 1.75, had smaller working memory capacities. A one-tailed test was used because age declines are the expected finding in the literature (Park & Scharz, 2000; Salthouse, 1991). Working memory span was assessed using a composite measure consisting of the loaded sentence span task (Stine & Hindman, 1994) and the computation span (Salthouse & Babcock, 1991) Perceptual speed, assessed using an average of the pattern and letter comparison tasks (Salthouse & Babcock, 1991), also showed the expected age declines, where higher scores indicate a greater number of correct comparisons (between two pattern or letter strings) produced within the time limit. We asked individuals about their use of NFPs to determine whether there were group differences in experience using NFPs. Frequency of NFP use was assessed using a question that asked “How frequently do you use NFPs when buying a food for the first time?” (1=never; 4=always). There were no age differences in the frequency of use.
In general, age patterns were comparable for the two DMG groups, yet there were some notable differences. First, the age differences in the no-DMG group in working memory capacity were not evident in the DMG group and, second, older adults in the DMG group had more years of education than younger adults, a difference that was not evident in the no-DMG group. Finally, BMI was similar for younger and older adults no-DMG group, but BMI was higher for older than younger in the DMG group. Certainly, one reason for modifying one’s diet could be that individuals have an underlying illness that requires changes in dietary habits. Although large differences in health were not evident between the two modification groups or two age groups, we opted to control for individual differences in health in the regression analyses below that include dietary modification status. Our rationale was that we were interested in examining the effects of modification goals on decision making processes but wanted to do so independently of possible health declines. Table 1 shows means and age differences within the two DMG groups (right-hand side).
Materials
NFPs
NFPs for the healthfulness task were created using the NutritionData website (http://www.nutritiondata.com) which produces formats that conform to the FDA format requirements (21 CFR 101.9 (d)). NFPs contained information on calories, key nutrients, vitamins, and minerals for a 2000-calorie/day diet (a serving size of 1 was kept constant across panels). Three common categories of foods were selected for manipulation across NFP pairs: bread, soup, and meat. An 8-point Helvetica Black font was used for nutrients and their percent Daily Value and each panel subtended a visual angle of 7.4° (9.3 cm) horizontally and 14.3° (18.1 cm) vertically at a viewing distance of 72.4 cm. on a Dell VGA monitor (85 Hz refresh rate, 1024 × 768 screen resolution). We created a mate for each target NFP that was either more or less healthful than its mate on one target nutrient (75% change) but varied minimally in the opposite direction (5% change) on all other nutrients. Target nutrients, defined as nutrients which were key to an accurate assessment of the healthfulness judgment, were fiber, sodium, and fat for bread, soup, and meat food categories, respectively. If participants attended to non-target nutrients, they would be more likely to make a mistake by basing their decision on an insignificant difference between the two NFPs. There were 10 trials within each food category. A fourth category, vegetables, was also included to provide greater variation in the amounts and distribution of various nutrients. Vegetable NFP pairs were not manipulated but instead were paired with other vegetable NFPs from similar vegetable families. These trials (n = 6) served to increase variability of nutrient values across NFPs. Because the nutrient values for these pairs were not manipulated, these trials did not have a correct answer and were not scored for accuracy. Decision accuracy scores were the total number correct out of 30 trials.
Knowledge
We used a 38-item test of nutrition knowledge (Miller, Gibson, et al., 2011) containing items that assessed semantic knowledge such as the relationships between nutrition and health and knowledge of nutrition principles (e.g., which foods are good sources of various nutrients), as well as procedural knowledge (e.g., knowing what to look for when shopping for cereal). The proportion of correct responses out of 38 was the score used to reflect knowledge of nutrition.
Motivation
We drew on the Transtheoretical Model of Change (Prochaska & DiClemente, 2005) in assembling 3 items that assess readiness to: reduce fat consumption, reduce junk food consumption, and increase fruits and vegetable consumption (Miller et al., 2010). For each of these categories of foods, participants were asked to select the response that “best represents your perspective/behavior on eating ___.” (1=never think about it; 6=have been doing this). The junk food item, for example, had options ranging from “I haven’t given any thought at all to cutting junk food out of my diet” (stage 1) to “I have been consciously avoiding junk food for longer than the last 6 months” (stage 6). The fruits and vegetable item was worded in the opposite direction to reflect stage of increasing intake. Therefore, we used two measures of motivation: 1) decreasing fat and junk food consumption and 2) increasing fruits and vegetable consumption. For ease of naming, we refer to stage of change for fruits and vegetables as SOC to increase healthy foods (SOC+) and stage of change for fat and junk food as SOC to avoid unhealthy foods (SOC−).
Procedure
The session began with a background demographic and health questionnaire. These were followed by an overview of the NFP task, a practice task, and the experimental tasks. The session ended with the post-task question asking participants to list the nutrients they had used to make healthfulness decisions, and the individual difference measures of speed of processing and working memory capacity. For the overview, the experimenter pointed out each of the key nutrient categories, amounts (grams, milligrams), and percent Daily Value on a sample NFP printed on an 11×14 sheet of paper.
Eye movements were monitored using an EyeLink 1000, a video-based eye tracker with a sampling rate of 2000 Hz and average accuracy of 0.25 -0.5 degrees. The eye tracker reflects an infrared light off of the participant’s left eye enabling a video camera to record time stamps and eye-position coordinates. Participants completed a nine-point calibration task on the eye-tracker followed by a NFP practice task. The practice task consisted of nine trials designed to provide participants with experience a) searching for information on an NFP and b) responding to questions using the button box. For this task, participants were asked to locate a piece of information (e.g., number of grams of fat in one serving) presented on a single NFP. Upon locating the information, participants identified their answer among four numbered options presented along the side of the screen and pressed the corresponding number on the button box. For the experimental task, participants were asked to decide which of two NFPs represented the more healthful choice. The NFPs (original and mate) were presented side-by-side and in totality (to avoid need for scrolling). The participants indicated their decision by pressing the left button to select the left NFP or the right button to select the right NFP. Correct answers were counterbalanced across left and right positions. The trial ended upon the selection of one NFP, and participants began a new trial by pressing either button. There were two practice trials followed by 36 experimental trials.
Target nutrient interest areas were defined as the nutrient name, amount (g or mg), and percent Daily Value for fiber, sodium, and fat. Compensatory and noncompensatory decision making strategies were operationalized in terms of the frequency of saccades, eye movement sequences, in which an individual fixated on one target nutrient interest area followed by another. Fixation sequences that occurred between different nutrients within one NFP (e.g., fiber on panel 2 to sodium on panel 2) were categorized as compensatory. Fixation sequences that occurred between the same nutrients on different NFPs (e.g., sodium on panel 1 to sodium on panel 2) were categorized as noncompensatory. Study participants engaged in multiple compensatory and noncompensatory sequences per trial. Strategy variables were measured in counts and were log transformed to create normal distributions. A third variable, strategy differences, was calculated as the difference between the log transformation of the two sequence types (i.e., between-NFP sequences minus within-NFP sequences) to obtain an estimate of overall strategy balance.
Data Analysis
Strategy Use
We used hierarchical regressions to examine multiplicative effects of person factors on decision making strategy using three dependent variables: within-NFP sequence frequency, between-NFP sequence frequency, and strategy difference scores. We were particularly interested in determining a) whether there were age differences in strategy use that were dependent on knowledge, motivation, or DMG status and b) whether knowledge, motivation, and DMG status interacted with each other to influence strategy use. We created 2- way terms crossing these person factors; variables were mean centered prior to creating interaction terms. Given the overlap among person factors of age, knowledge, and motivation, together with a relatively small sample size, we examined 2-way terms individually. Moreover, because this was an exploratory study and we had no strong justification for 3-way interactions, we omitted 3-way terms in our analyses. In the first step, we included health variables (i.e., number of chronic conditions and medication, BMI, self-reported overall health), and in the second and third steps, we entered the main effects and 2-way term, respectively. Significant interactions were explored by plotting predictors at low (1 SD below mean) and high (1 SD above the mean) values and by testing simple slopes to determine if the gradients differed significantly from zero.
Decision Accuracy
We analyzed decision accuracy using three approaches. First, we used hierarchical regressions to investigate whether person factors interacted a) with each other or b) with strategy use to predict decision accuracy. We created interaction terms that crossed person factors with strategy use to determine whether strategy effectiveness (i.e., the ability of strategy to predict accuracy), moderated the effects of knowledge, motivation, DMG status, or age on accuracy. Given the high number of possible combinations, we limited our investigation to 2-way terms only. In the first step, we included health variables, and in the second step, we entered the main effects, followed by the 2-way term in the third step. Significant interactions were explored using tests of simple slopes.
Second, we examined the protective effects of knowledge and motivation in a modified version of the migration hypothesis. The migration hypothesis states that older adults show less cognitive decline (Salthouse, 2003) when they migrate into higher knowledge (and perhaps motivation) groups with age. In step 1, we entered age and, in step 2, we entered either knowledge or SOC or both.
Third, we used Sobel tests of partial mediation to explore possible mediational relationships between knowledge and motivation. Specially, we examined a model in which knowledge partially mediated the relationship between motivation and accuracy as well as the reverse possibility, that motivation partially mediated the relationship between knowledge and accuracy. We were interested in partial mediation here because past research does not support an extreme view in which one variable would exert its influence exclusively through the other.
Results
Preliminary Analyses of Strategy, Accuracy, and Person Factors
Older adults had higher knowledge scores and higher motivation as indexed by SOC+ (stage of change to increase fruits and vegetables) and SOC− (stage of change to decrease fat and junk food) relative to younger adults. Indeed, older adults were close to ceiling on SOC+ and variability was attenuated. Therefore, we omit this motivation variable in the regressions below. DMG status was unrelated to the other variables. Decision accuracy was related to knowledge and motivation but not to age. Table 2 contains the bivariate correlations among strategy, motivation, knowledge, DMG status, and age (see appendix for means and standard deviations).
Table 2.
Bivariate Correlations among Key Variables.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|
| 1 Accuracy | .21 | .17 | .12 | .13 | −.08 | .56** | .33** | .13 |
| 2 Between-NFP Sequences | .53** | .77** | .11 | .19 | .20 | .21 | .06 | |
| 3 Within-NFP Sequences | −.14 | .23 | .04 | .13 | .27* | −.16 | ||
| 4 Strategy Difference | −.05 | .19 | .14 | .04 | .19 | |||
| 5 Age | .23 | .44** | .56** | .32** | ||||
| 6 DMG Status | .19 | −.04 | .06 | |||||
| 7 Knowledge | .28* | .33** | ||||||
| 8 SOC− (fat/junk food) | .29* | |||||||
| 9 SOC+ (fruits/vegetables) | 1 |
. Correlation is significant at the 0.01 level (2-tailed).
. Correlation is significant at the 0.05 level (2-tailed).
Appendix.
Means (and standard deviations) of accuracy, strategy, knowledge, and motivation variables by age and dietary modification status.
| No-DMG | DMG | Younger Adults | Older Adults | No-DMG | DMG | |||
|---|---|---|---|---|---|---|---|---|
| Younger Adults (n=28) | Older Adults (n=13) | Younger Adults (n=12) | Older Adults (n=14) | |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Accuracy | 24.07a (3.71) | 23.42a (4.15) | 23.30a (3.50) | 24.59a (4.32) | 23.21a (3.56) | 25.92b (3.45) | 23.50a (3.48) | 23.36a (4.78) |
| Between-NFP Sequences | .49a (0.27) | .60a (0.32) | .51a (0.28) | .57a (0.31) | .51a (0.26) | .45a (0.30) | .51a (0.35) | .68a (0.28) |
| Within-NFP Sequences | .28a (0.15) | .29a (0.24) | .25a (0.20) | .33a (0.15) | .26a (0.17) | .32a (0.10) | .24a (0.28) | .34a (0.19) |
| Strategy Difference | .21a (0.27) | .31a (0.21) | .25a (0.21) | .24a (0.31) | .25a (0.22) | .13a (0.35) | .27a (0.17) | .34a (0.23) |
| Knowledge | .55a (0.14) | .60a (0.13) | .52a (0.10) | .65b (0.14) | .51a (0.12) | .65b (0.14) | .55a (0.05) | .65b (0.15) |
| SOC+ (fruits/vegetables) | 5.3a (1.13) | 5.5a (0.90) | 5.1a (1.16) | 5.8b (0.70) | 5.1a (1.27) | 5.8a (0.60) | 5.1a (0.90) | 5.8b (0.80) |
| SOC− (fat/junk food) | 4.68a (1.10) | 4.58a (1.28) | 4.09a (1.09) | 5.45b (0.69) | 4.20a (0.97) | 5.71b (0.45) | 3.83a (1.35) | 5.21b (0.80) |
Note: DMG=Dietary Modification Goals; NFP=Nutrition Facts Panel; SOC=Stage of Change; Values in the same row and subtable not sharing the same subscript are significantly different at p< 0.05 in the two-sided test of equality for column means.
Regressions Predicting Strategy Use from Person Factors
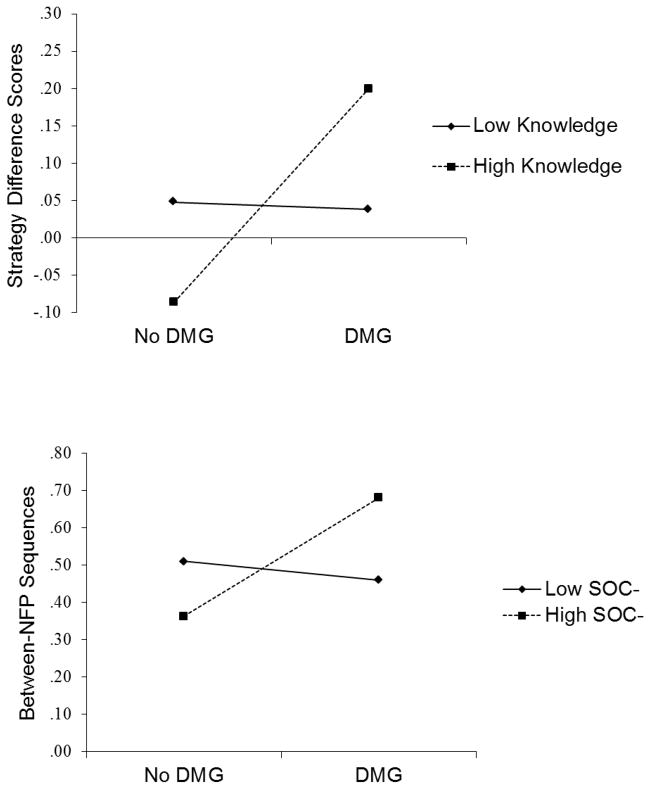
There were no significant interactions involving age on any of the three strategy variables (within-NFP sequence frequency, between-NFP sequence frequency, and strategy difference scores), suggesting that age did not moderate the effects of knowledge, motivation, or DMG status on strategy use. In addition, there were no interactions between knowledge and motivation on strategy use. However, there were two significant interactions involving DMG status. First, knowledge interacted with DMG status in predicting strategy difference scores, β = .29, p < .05, R2 change = .07. As can be seen in the top half of Figure 2, greater knowledge was associated with greater relative use of between- to within - NFP sequences for the DMG group, simple slope t test=2.8, p < .01, but not the no-DMG group, t<1. Second, SOC− interacted with DMG status in predicting between-NFP sequence frequency, β = .30, p < .05, R2 change = .09, such that higher motivation scores were associated with relatively greater use of between-NFP sequences, again, for the DMG group, simple slope t test=2.5, p < .05, but not the no-DMG group, t<1. This interaction is depicted in the bottom half of Figure 2. None of the other 2- interactions reached significance.
Figure 2.
For those with dietary modification goals (DMG), knowledge was associated with relatively greater use of between-NFP sequences (top) and motivation was associated with greater use of between-NFP sequences (bottom).
Thus, the data show that, for the DMG group, there was a positive association between 1) strategy difference scores (i.e., relatively more between- relative to within-NFP sequences) and knowledge and 2) increased use of between-NFP sequences and SOC−. However, for the no-DMG group, neither of these relationships was evident. Nonsignificant interactions with age suggest that the effects of knowledge and motivation factors on strategy use did not differ for younger and older adults.
Regressions Predicting Accuracy from Strategy and Person Factors
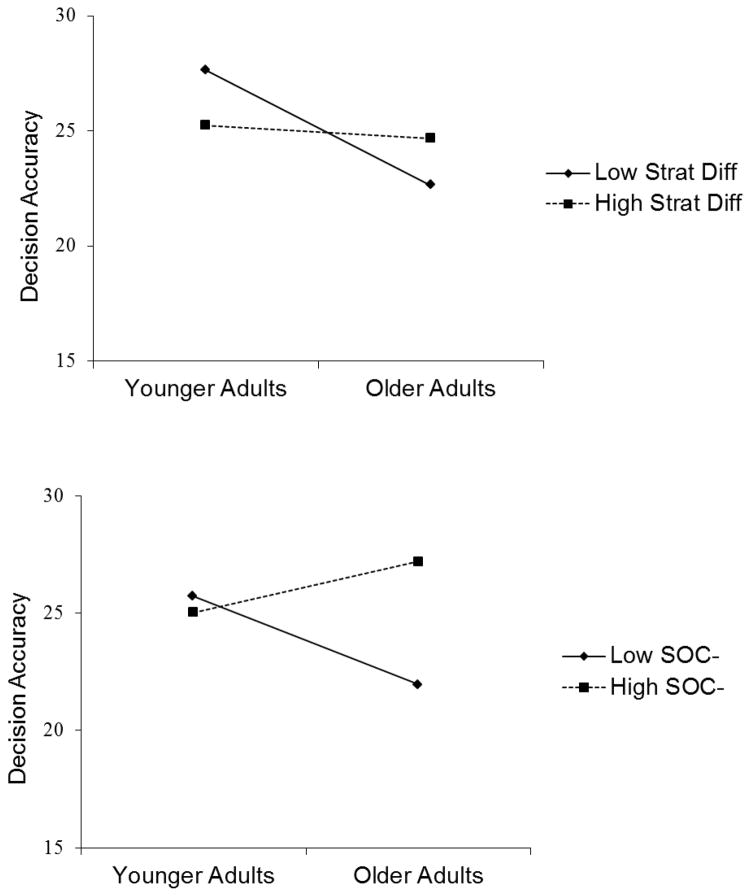
We examined whether any of the four person factors moderated the effects of the other on accuracy. We found a significant age x strategy difference interaction, β = .31, p < .05, R2 change = .07. As shown in the top half of Figure 3, age declines in accuracy were evident among those who used relatively fewer between- than within- NFP sequences, simple slope t test=2.6, p < .01, but were not evident among those who used relatively more between- than within- NFP sequences, t<1. There was also a significant age x SOC− interaction, β = .31, p < .05, R2 change = .06, which is depicted in the bottom half of Figure 3. Although the interaction was significant, there were nonsignificant age-related decreases in accuracy among those with less motivation, simple slope t<1, and nonsignificant age-related increases among those with higher levels of motivation, t test=1.5, ns. Given that neither slope gradient was significantly different from zero, the interaction appears to be due to small diverging changes at both motivation levels.
Figure 3.
Age declines in accuracy were greater among those with lower relative to higher strategy difference scores (between- relative to within- NFP sequences) (top) and lower relative to higher levels of motivation (bottom).
To summarize, age declines in accuracy were less pronounced among those who had high strategy difference scores (used relatively more between- than within-NFP sequences) relative to those who had low strategy differences scores. Age declines were also less pronounced among those who had higher- relative to lower - motivation.
Regressions Examining the Migration Hypothesis
As indicated above, both knowledge and motivation were associated with decision accuracy and both independently predicted strategy use for the DMG group. However, the two variables did not interact with each other to predict strategy use. Moreover, the two variables did not have multiplicative effects on accuracy, although motivation, but not knowledge, did appear to help older adults more than younger adults. In the analyses below, we examined the possibility that knowledge and SOC− serve as protective factors for older adults by assessing the effects of age before and after controlling for these two variables.
Age was nonsignificant but had a positive direction, β= .11, ns, when entered alone. With either knowledge or SOC−, age remained nonsignificant, but the beta was negative, β = −.14, ns, for knowledge alone; β = −.11, ns, for SOC−. When both of these variables were in the model, however, the age beta was significant and negative, β= −.33, p < .01, R2 change = .07. The finding that age declines were evident only when both knowledge and motivation were controlled suggests that both factors served to protect against declines in decision making accuracy. Thus, these findings are consistent with a version of the migration hypothesis that is expanded to include motivation: when older adults migrate into higher knowledge and motivation groups, these assets mitigate the negative effects of age on cognitive performance.
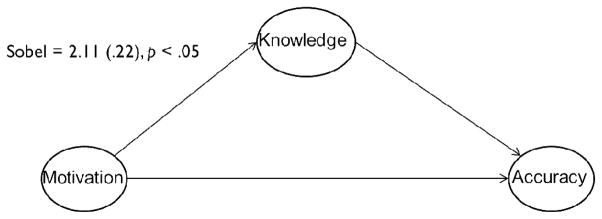
Sobel Tests of Partial Mediation
In the first model, we tested whether knowledge partially mediated the relationship between motivation and accuracy. In the second model, we tested the reverse: whether motivation partially mediated the relationship between knowledge and accuracy. We found that the first model was significant, Sobel = 2.11 (.22), p < .05, but not the second, Sobel = 1.4, ns. As depicted in Figure 4, motivation appears to increase decision accuracy by exerting some influence through knowledge. Although it is possible that mediation would be more evident in the older relative to younger group, we did not find support for this (within-age group Sobel tests were nonsignificant). Given our modest sample size, however, we caution against any firm conclusions regarding age differences in the mediational effects of knowledge on the motivation-accuracy relationship.
Figure 4.
Knowledge partially mediated the relationship between motivation and decision accuracy.
Discussion
The present study was undertaken to increase our understanding of how younger and older adults, who vary in knowledge, motivation, and dietary modification status, process NFPs to make accurate decisions regarding food healthfulness. Past research using eye tracking methodology has shown that individuals prefer to examine food label information that is central to their field of view and simple in content and format (Graham & Jeffery, 2011; van Herpen & van Trijp, 2011; Visschers et al., 2010). In the present study, we were interested in exploring how person factors interacted to impact how information is extracted (i.e., strategies) as well as how person factors and strategies impact decision accuracy.
Individuals Use Compensatory and Noncompensatory Strategies
The data show that individuals use both compensatory and noncompensatory strategies when deciding which of two NFPs is more healthful. These findings add to the literature surrounding NFP comprehension (Goldberg, Probart, & Zak, 1999a; Graham & Jeffery, 2011; Grunert et al., 2010; Levy & Fein, 1998; van Herpen & van Trijp, 2011) by showing that consumers use a variety of approaches (two at least) when evaluating food healthfulness based on NFPs, and further, that different decision making strategies are associated with different outcomes.
We found that the use of noncompensatory strategies, those that rely on making comparisons between single nutrients across labels, was driven by a motivation to avoid fat and junk food. Specifically, those with dietary modification goals increased their use of nutrient comparisons with increasing levels of motivation. We also found that none of these variables predicted compensatory strategies, those that entail evaluating different nutrient information within one label. However, a measure that considered both strategy types (i.e., strategy difference), showed a positive relationship between relatively more between- than within-NFP sequences and knowledge, again for those with dietary modifications. In none of these cases, however, did age reach significance, indicating age constancy in the use of the different strategies. Thus, younger and older adults appear to use quantitatively and qualitatively similar strategies when making healthfulness decisions based on NFPs.
However, we did find age differences in the effectiveness of noncompensatory decision making strategies. Specifically, relatively more between-NFP sequences (and fewer within-NFP sequences) was positively associated with decision accuracy of older adults. This finding adds to the literature on age differences in consumer decision making. Past research has shown that older adults preferred a noncompensatory decision making strategy when performing a mock car purchase task (Johnson, 1990). However, decision outcomes for that study were based on preferences and therefore linking strategies to accuracy was not possible. We suggest that when consumers compare several values back and forth across options, they may be constructing a mental model of the food that helps to track individual comparisons and determine which food is more healthful. It could be that more comparisons are required for older adults to arrive at a well-informed decision (Meyer, Russo, & Talbot, 1995).
We speculate that noncompensatory strategies may support more efficient decision making processes, at least for older adults. The number of food decisions that individuals make in a day exceeds 200 (Wansink & Sobal, 2007). One way to deal with this high information-processing load is to use effective strategies that enable individuals to assimilate large amounts of nutrition information on a food label, and in turn, increase the likelihood of using this information to make accurate healthfulness decisions. Moreover, decision strategies may support accurate decisions, in part, through their impact on mental model construction. Mental models are internal representations of aspects of the real world (e.g., objects, events, and processes) and include information regarding the structure and interrelationships among elements (Johnson-Laird, 1983). Mental models of specific foods may provide a coherent representation of the good and not-so-good nutrient qualities and in turn promote more accurate healthfulness decisions.
Knowledge and Motivation
Past work has shown that motivation is related to knowledge which is related to NFP use and dietary intake (Fitzgerald et al., 2008). Other work has suggested that motivation to process nutrition information is positively associated with the amount of information accessed (Balasubramanian & Cole, 2002) and degree of conceptual integration (Miller et al., 2010) and that knowledge is related to understanding of food label information (Grunert et al., 2010) and knowledge acquisition (Miller, Gibson, et al., 2011). Moreover, past work has shown that health motivation may be more important than taste motivation in seeking difficult-to-locate nutrition information on a food label (Visschers et al., 2010). The present findings add to this literature by showing that, independently, knowledge and motivation were related to strategy use, but only among those with dietary modification goals. It is important to point out that those with dietary modification goals did not possess higher levels of either factor. Thus, it appears that these individuals utilized the knowledge and motivation that they did have, more effectively. Perhaps individuals who self-identify as having dietary restrictions have a deeper commitment to thoughtful food-related decision making, which is reflected in greater engagement in a healthfulness decision making task. We were somewhat surprised to find that stage of change and dietary modification goals were not more similar a) to each other and b) in their relationship to strategy use. Although both variables reflected greater engagement, they had multiplicative effects rather than independent effects. Moreover, both dietary modification goals and stage of change related to how adults used NFPs to make decisions whereas stage of change was also related to how well older adults, but not younger adults, used NFPs to make decisions.
There is some debate among researchers and clinicians regarding the role of knowledge in dietary choice. In essence, the larger question is: why do individuals eat unhealthy food when they know that these foods are unhealthy? We would argue that knowledge is necessary - but not sufficient - for accurate healthful decisions and healthy eating. It seems likely that motivation also plays a role. Data from the present study shed light on this issue in three ways. First, the data show that knowledge and motivation have independent effects on accuracy, as reflected by zero-order correlations, and that knowledge has a larger association with accuracy than does motivation. Both knowledge and motivation interact with dietary modification goals to impact strategy use. Thus, both factors play a role in how NFPs are processed. Second, the two factors grow in importance with age. We found that when knowledge and motivation were statistically controlled, age-related declines in accuracy were evident. These data suggest that both factors play a protective role in the ability to use NFPs to make healthful decisions. This finding is consistent with the migration hypotheses (Salthouse, 2003) suggesting that, as individuals age, they move into higher knowledge groups. These findings extend this pattern to include higher motivation groups as well as knowledge groups.
Finally, our study informs the literature on the relationship between knowledge and motivation. Mediational tests showed that motivation to avoid unhealthy foods (fat and junk food) impacts decision accuracy through prior knowledge of nutrition. This was true regardless of dietary modification goals and age. Cognitive researchers have suggested that knowledge remains inert unless is it activated in some way (Boekaerts, 1996; Bransford et al., 1999; Kintsch, 1998). It could be that motivation to eat healthful foods provides the spark that ignites the application of nutrition knowledge to food-related decision making.
NFP Comprehension and Aging
Roughly one half of consumers report reading a product’s label when purchasing a food for the first time (Choinière & Lando, 2008), regardless of age (Ollberding et al., 2010). One reason for low use could be challenges associated with understanding the information (Levy & Fein, 1998; Levy, Fein, & Schucker, 1992, 1996; Lewis & Yetley, 1992). Indeed, individuals in the present study were not always correct when evaluating two NFPs side by side. However, decision accuracy was comparable across age groups. This finding stands in contrast to past work showing age-related declines in NFP comprehension (Burton & Andrews, 1996; Levy et al., 1992). It is important to point out that our sample of older adults was high functioning. Older adults were in good health as reflected by a low number of chronic conditions and medications taken, and they had more years of education than younger adults. Thus, data from older adults in the present study represent aging under optimal conditions, a best case scenario. Indeed, the data showed that our older adults had sufficient levels of knowledge and motivation that offered some protection against age declines in accuracy. More work is needed to examine age differences relative to knowledge, motivation, and accuracy within a more diverse population.
Limitations
As noted above, one limitation of the present study is that the sample was high in cognitive functioning, well educated, and had good health. The sample size was also small. In a larger, more diverse sample, age declines in healthfulness accuracy may be evident and the roles of supportive factors may be greater. Although our findings offer a picture of decision making as it occurs under the best conditions, it is important to note that we may have underestimated the roles of age, dietary modification status, knowledge, and motivation. Moreover, the nature of the decision making task used in the present study may have encouraged an effortful approach to decision making that may be evident in only limited situations in the grocery store or restaurant (e.g., buying a food for the first time). More work is needed to determine how contextual factors (e.g., food environment, ethnicity, and acculturation) and other aspects of the food label (e.g., ingredient lists, health claims, brand information) impact decision making. For example, when brand information is present, we could find that individuals devote less effort to NFP comparisons than was observed in the present study. In addition, our study included a single question regarding dietary modification goals. More work is needed to determine whether there are meaningful subcategories of dietary modification status that differentially impact decision making processes. Research on strategies surrounding NFP use would also benefit from a more diverse set of decision making tasks. For example, the use of NFPs together with claims and pictures of various foods may offer another approach to understanding how nutrition information is processed on food labels (Houts, Doak, Doak, & Loscalzo, 2006).
Conclusions
We found that the use of noncompensatory strategies (number of nutrient-to-nutrient comparisons between NFPs) increased with knowledge and motivation among those with dietary modifications goals. The data suggest that these individuals are more willing to apply their knowledge and motivation to a food-related decision making task. Among older adults, strategy and motivation were important moderators of decision accuracy after controlling for health variables. Moreover, after controlling for knowledge and motivation, age-related declines in accuracy were evident. Finally, across all individuals, knowledge mediated the relationship between motivation and accuracy, suggesting that motivation provides the impetus needed to apply what one knows to food decisions. Together, these data suggest that knowledge and motivation support more comparisons across choices, which in turn may enable more nutrient information to be assimilated and improve decision quality.
Highlights.
We examined how younger and older adults decided which of two NFPs was healthier.
Eye tracking was used to examine decision making strategies.
Dietary modification goals, knowledge, and motivation predicted strategy use.
The strategy-accuracy relationship depended on age and motivation.
Knowledge mediated the relationship between motivation and decision accuracy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lisa M. Soederberg Miller, Email: lmsmiller@ucdavis.edu, Department of Human and Community Development, University of California, Davis One Shields Avenue Davis, CA 95616; USA, Tel 530-752-3955 Fax 530-752-5660.
Diana L. Cassady, Email: dlcassady@phs.ucdavis.edu, Department of Public Health Sciences, One Shields Avenue, University of California, Davis Davis, CA 95616, Tel 530-754-5550 Fax 530-752-3118.
References
- Aikman SN, Crites SL. Structure of food attitudes: Replication of aikman, crites, and fabrigar (2006) Appetite. 2007;49(2):516–520. doi: 10.1016/j.appet.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Preventive Medicine. 2002;35(1):25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, Burke LE. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults. Circulation. 2010;122(4):406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian SK, Cole C. Consumers’ search and use of nutrition information: The challenge and promise of the nutrition labeling and education act. The Journal of Marketing. 2002;66(3):112–127. [Google Scholar]
- Bandura A. The primacy of self-regulation in health promotion. Applied Psychology: An International Review. 2005;54:245–254. [Google Scholar]
- Beydoun MA, Wang Y. Do nutrition knowledge and beliefs modify the association of socio-economic factors and diet quality among us adults? Preventive Medicine. 2008;46:145–153. doi: 10.1016/j.ypmed.2007.06.016. [DOI] [PubMed] [Google Scholar]
- Boekaerts M. Self-regulated learning at the junction of cognition and motivation. European Psychologist. 1996;1(2):100–112. [Google Scholar]
- Bransford JD, Brown AL, Cocking RR. How people learn: Brain, mind, experience, and school. Washington, DC: National Academy of Sciences; 1999. [Google Scholar]
- Burton S, Andrews JC. Age, product nutrition, and label format effects on consumer perceptions and product evaluations. Journal of Consumer Affairs. 1996;30:68–89. [Google Scholar]
- Burton S, Garretson JA, Velliquette AM. Implications of accurate usage of nutrition facts panel information for food product evaluations and purchase intentions. Journal of the Academy of Marketing Science. 1999;27(4):470–480. doi: 10.1177/0092070399274006. [DOI] [Google Scholar]
- Byrd-Bredbenner C, Kiefer L. The ability of elderly women to perform nutrition facts label tasks and judge nutrient content claims. Journal of Nutrition for the Elderly. 2000;20:29–46. [Google Scholar]
- Choinière CJ, Lando A. Health and diet survey. 2008. Retrieved May 2010, from Food and Drug Administration. [Google Scholar]
- Crites SL, Aikman SN. Impact of nutrition knowledge on food evaluations. European Journal of Clinical Nutrition. 2005;59:1194–1200. doi: 10.1038/sj.ejcn.1602231. [DOI] [PubMed] [Google Scholar]
- Department of Agriculture, U. S. Nutrition insight. Vol. 29. Alexandria, VA: Center for Nutrition Policy and Promotion; 2004. Quality of diets of older americans. [Google Scholar]
- Ericsson KA, Kintsch W. Long-term working memory. Psychological Review. 1995;102(2):211–245. doi: 10.1037/0033-295x.102.2.211. [DOI] [PubMed] [Google Scholar]
- Fitzgerald N, Damio G, Segura-Pérez S, Pérez-Escamilla R. Nutrition knowledge, food label use, and food intake patterns among latinas with and without type 2 diabetes. Journal of the American Dietetic Association. 2008;108(6):960–967. doi: 10.1016/j.jada.2008.03.016. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the united states: A systematic review. JAMA. 2002;288(24):3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Fusillo AE, Beloian AM. Consumer nutrition knowledge and self reported food shopping behavior. Am J Public Health. 1977;67(9):846–850. doi: 10.2105/ajph.67.9.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golan E, Kuchler F, Krissoff B. Do food labels make a difference? Amber Waves, ERS, USDA. 2007;5:10–17. [Google Scholar]
- Goldberg JH, Probart CK, Zak RE. Visual search of food nutrition labels. Human Factors. 1999a;41:425–457. doi: 10.1518/001872099779611021. [DOI] [PubMed] [Google Scholar]
- Goldberg JH, Probart CK, Zak RE. Visual search of food nutrition labels. Human Factors: The Journal of the Human Factors and Ergonomics Society. 1999b;41(3):425–437. doi: 10.1518/001872099779611021. [DOI] [PubMed] [Google Scholar]
- Graham DJ, Jeffery RW. Location, location, location: Eye-tracking evidence that consumers preferentially view prominently positioned nutrition information. Journal of the American Dietetic Association. 2011;111(11):1704–1711. doi: 10.1016/j.jada.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunert K, Wills J. A review of european research on consumer response to nutrition information on food labels. Journal of Public Health. 2007;15(5):385–399. doi: 10.1007/s10389-007-0101-9. [DOI] [Google Scholar]
- Grunert KG, Wills JM, Fernández-Celemín L. Nutrition knowledge, and use and understanding of nutrition information on food labels among consumers in the uk. Appetite. 2010;55(2):177–189. doi: 10.1016/j.appet.2010.05.045. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Jensen HH, Batres-Marquez SP, Chen C. Sociodemographic, knowledge, and attitudinal factors related to meat consumption in the united states. Journal of the American Dietetic Association. 2005;105:1266–1274. doi: 10.1016/j.jada.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Guthrie JF, Derby BM, Levy AS. What people know and do not know about nutrition. In: Frazao E, editor. America’s eating habits: Changes and consequences. Washington, DC: USDA/ERS; 1999. pp. 243–280. [Google Scholar]
- Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychological Review. 2010;117(1):32–60. doi: 10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Education and Counseling. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Howlett E, Burton S, Kozup J. How modification of the nutrition facts panel influences consumers at risk for heart disease: The case of trans fat. [Article] Journal of Public Policy & Marketing. 2008;27:83–97. [Google Scholar]
- Jepson CC, Shelly Chronic issue-specific fear inhibits systematic processing of persuasive communications. Journal of Social Behavior & Personality. 1990;5(2):61–84. [Google Scholar]
- Johnson-Laird P. Mental models. Cambridge, MA: Harvard University Press; 1983. [Google Scholar]
- Johnson MM. Age differences in decision-making: A process methodology for examining strategic information processing. Journal of Gerontology: Psychological Sciences. 1990;45:P75–P78. doi: 10.1093/geronj/45.2.p75. [DOI] [PubMed] [Google Scholar]
- Kintsch W. Comprehension: A paradigm for cognition. New York: Cambridge University Press; 1998. [Google Scholar]
- Klohe-Lehman DM, Freeland-Graves J, Anderson ER, McDowell T, Clarke KK, Hanss-Nuss H, Milani TJ. Nutrition knowledge is associated with greater weight loss in obese and overweight low-income mothers. Journal of the American Dietetic Association. 2006;106(1):65–75. doi: 10.1016/j.jada.2005.09.047. [DOI] [PubMed] [Google Scholar]
- Kristal AR, Levy L, Patterson RE, Li SS, White E. Trends in food label use associated with new nutrition labeling regulations. Am J Public Health. 1998;88(8):1212–1215. doi: 10.2105/ajph.88.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Mora PA. Is there a science of the processes underlying health and illness behaviors? A comment on maes and karoly. Applied Psychology: An International Review. 2005;54:255–266. [Google Scholar]
- Levy AS, Fein SB. Consumers’ ability to perform tasks using nutrition labels. Journal of Nutrition Education and Behavior. 1998;30:210–217. [Google Scholar]
- Levy AS, Fein SB, Schucker RE. More effective nutrition label formats are not necessarily preferred. Journal of the American Dietetic Association. 1992;92:1230–1234. [PubMed] [Google Scholar]
- Levy AS, Fein SB, Schucker RE. Performance characteristics of seven nutrition label formats. Journal of Public Policy & Marketing. 1996;15:1–15. [Google Scholar]
- Lewis CJ, Yetley EA. Focus group sessions on formats of nutrition labels. Journal of the American Dietetic Association. 1992;92:62–66. [PubMed] [Google Scholar]
- Lin CJ, Lee J, Yen ST. Do dietary intakes affect search for nutrient information on food labels? Social Science & Medicine. 2004;59:1955–1967. doi: 10.1016/j.socscimed.2004.02.030. [DOI] [PubMed] [Google Scholar]
- Meyer BJF, Russo C, Talbot A. Discourse comprehension and problem solving: Decisions about the treatment of breast cancer by women across the life span. Psychology and Aging. 1995;10:84–103. doi: 10.1037//0882-7974.10.1.84. [DOI] [PubMed] [Google Scholar]
- Mhurchu CN, Gorton D. Nutrition labels and claims in new zealand and australia: A review of use and understanding. Australian and New Zealand Journal of Public Health. 2007;31(2):105–112. doi: 10.1111/j.1753-6405.2007.00026.x. [DOI] [PubMed] [Google Scholar]
- Miller CK, Headings A, Peyrot M, Nagaraja H. A behavioural intervention incorporating specific glycaemic index goals improves dietary quality, weight control and glycaemic control in adults with type 2 diabetes. Public Health Nutrition. 2011;14(07):1303–1311. doi: 10.1017/S1368980011000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS. Age differences in the effects of domain knowledge on reading efficiency. Psychology and Aging. 2009;24(1):63–74. doi: 10.1037/a0014586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS, Gibson TN, Applegate EA. Predictors of nutrition information comprehension in adulthood. Patient Education and Counseling. 2010;80(1):107–112. doi: 10.1016/j.pec.2009.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS, Gibson TN, Applegate EA, de Dios J. Mechanisms underlying comprehension of health information in adulthood: The roles of prior knowledge and working memory capacity. Journal of Health Psychology. 2011;16(5):794–806. doi: 10.1177/1359105310392090. [DOI] [PubMed] [Google Scholar]
- Moorman C. A quasi experiment to assess the consumer and informational determinants of nutrition information processing activities: The case of the nutrition labeling and education act. Journal of Public Policy & Marketing. 1996;15(1):28–44. [Google Scholar]
- Morrow DG, Weiner M, Young J, Steinley D, Deer MM, Murray MD. Improving medication knowledge among older adults with heart failure: A patient-centered approach to instruction design. Gerontologist. 2005;45(4):545–552. doi: 10.1093/geront/45.4.545. [DOI] [PubMed] [Google Scholar]
- Nebeling L, Yaroch AL, Seymour JD, Kimmons J. Still not enough: Can we achieve our goals for americans to eat more fruits and vegetables in the future? American Journal of Preventive Medicine. 2007;32(4):354–355. doi: 10.1016/j.amepre.2006.12.018. [DOI] [PubMed] [Google Scholar]
- Neilsen Company. [Accessed 2-8-12];Battle of the bulge and nutrition labels: Healthy eating trends around the world. 2012 from: http://www.nielsen.com/content/corporate/us/en/insights/reports-downloads/2012/healthy-eating-trends-around-the-world.html.
- Neuhouser ML, Kristal AR, Patterson RE. Use of food nutrition labels is associated with lower fat intake. Journal of the American Dietetic Association. 1999;99:45–50. 53. doi: 10.1016/S0002-8223(99)00013-9. [DOI] [PubMed] [Google Scholar]
- Ollberding NJ, Wolf RL, Contento I. Food label use and its relation to dietary intake among us adults. Journal of the American Dietetic Association. 2010;110(8):1233–1237. doi: 10.1016/j.jada.2010.05.007. [DOI] [PubMed] [Google Scholar]
- Park DC, Scharz N, editors. Cognitive aging: A primer. Philadelphia: Psychology Press; 2000. [Google Scholar]
- Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. American Journal of Preventive Medicine. 2004;27(5):385–390. doi: 10.1016/j.amepre.2004.08.001. [DOI] [PubMed] [Google Scholar]
- Popkin BM, Zizza C, Siega-Riz AM. Who is leading the change? Us dietary quality comparison between 1965 and 1996. American Journal of Preventative Medicine. 2003;25:1–8. doi: 10.1016/s0749-3797(03)00099-0. [DOI] [PubMed] [Google Scholar]
- Posner BM, Jette AM, Smith KW, Miller DR. Nutrition and health risks in the elderly: The nutrition screening initiative. Am J Public Health. 1993;83(7):972–978. doi: 10.2105/ajph.83.7.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RE, Mainous AG, Diaz VA, Matheson EM, Everett CJ. Use of the nutrition facts label in chronic disease management: Results from the national health and nutrition examination survey. Journal of the American Dietetic Association. 2010;110(4):628–632. doi: 10.1016/j.jada.2009.12.015. [DOI] [PubMed] [Google Scholar]
- Post RE, Mainous AG, III, Diaz VA, Matheson EM, Everett CJ. Use of the nutrition facts label in chronic disease management: Results from the national health and nutrition examination survey. Journal of the American Dietetic Association. 2010;110(4):628–632. doi: 10.1016/j.jada.2009.12.015. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of psychotherapy integration. New York: Oxford University Press; 2005. pp. 147–171. [Google Scholar]
- Salthouse T. Interrelations of aging, knowledge, and cognitive performance. In: Staudinger UM, Lindenberger U, editors. Understanding human development: Dialogues with lifespan psychology. Dordrecht, Netherlands: Kluwer; 2003. pp. 265–287. [Google Scholar]
- Salthouse TA. Theoretical perspectives on cognitive aging. Hillsdale: Erlbaum; 1991. [Google Scholar]
- Salthouse TA, Babcock RL. Decomposing adult age differences in working memory. Developmental Psychology. 1991;27(5):763–776. [Google Scholar]
- Sharkey N, Sharkey A. What is the point of facilitation? The loci of knowledge-based facilitation in sentence processing. Journal of Memory and Language. 1987;26(3):255–276. [Google Scholar]
- Stine EAL, Hindman J. Age differences in reading time allocation for propositionally dense sentences. Aging and Cognition. 1994;1(1):1–12. [Google Scholar]
- Teisl MF, Levy AS. Does nutrition labeling lead to healthier eating? Journal of Food Distribution Research. 1997;28:19–26. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health. Washington, DC: 2000. [Google Scholar]
- van Herpen E, van Trijp HCM. Front-of-pack nutrition labels. Their effect on attention and choices when consumers have varying goals and time constraints. Appetite. 2011;57(1):148–160. doi: 10.1016/j.appet.2011.04.011. [DOI] [PubMed] [Google Scholar]
- van Trijp HCM, van der Lans IA. Consumer perceptions of nutrition and health claims. Appetite. 2007;48(3):305–324. doi: 10.1016/j.appet.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Variyam JN. Do nutrition labels improve dietary outcomes? Health Economics. 2008;17(6):695–708. doi: 10.1002/hec.1287. [DOI] [PubMed] [Google Scholar]
- Variyam JN, Golan E. New health information is reshaping food choices. Food Review. 2002;25(1):13–18. [Google Scholar]
- Visschers VH, Hess R, Siegrist M. Health motivation and product design determine consumers’ visual attention to nutrition information on food products. Public Health Nutrition. 2010;13(07):1099–1106. doi: 10.1017/S1368980009993235. [DOI] [PubMed] [Google Scholar]
- Wansink B, Sobal J. Mindless eating. Environment and Behavior. 2007;39(1):106–123. doi: 10.1177/0013916506295573. [DOI] [Google Scholar]
- Wardle J, Parmenter K, Waller J. Nutrition knowledge and food intake. Appetite. 2000;34(3):269–275. doi: 10.1006/appe.1999.0311. [DOI] [PubMed] [Google Scholar]
- Wills JM, Schmidt DB, Pillo-Blocka F, Cairns G. Exploring global consumer attitudes toward nutrition information on food labels. Nutrition Reviews. 2009;67(s1):S102–S106. doi: 10.1111/j.1753-4887.2009.00170.x. [DOI] [PubMed] [Google Scholar]
- Worsley A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pacific Journal of Clinical Nutrition. 2002;11(s3):S579–S585. doi: 10.1046/j.1440-6047.11.supp3.7.x. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Schultz R. Health-engagement control strategies and 2-year changes in older adults’ physical health. Psychological Sciences. 2008;19:537–548. doi: 10.1111/j.1467-9280.2008.02120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]