Abstract
Context
The US Food and Drug Administration issued a black box warning for antidepressants and suicidal thoughts and behavior in children and young adults.
Objective
To determine the short-term safety of anti-depressants by standard assessments of suicidal thoughts and behavior in youth, adult, and geriatric populations and the mediating effect of changes in depressive symptoms.
Data Sources
All intent-to-treat person-level longitudinal data of major depressive disorder from 12 adult, 4 geriatric, and 4 youth randomized controlled trials of fluoxetine hydrochloride and 21 adult trials of venlafaxine hydrochloride.
Study Selection
All sponsor-conducted randomized controlled trials of fluoxetine and venlafaxine.
Data Extraction
The suicide items from the Children’s Depression Rating Scale–Revised and the Hamilton Depression Rating Scale as well as adverse event reports of suicide attempts and suicide during active treatment were analyzed in 9185 patients (fluoxetine: 2635 adults, 960 geriatric patients, 708 youths; venlafaxine: 2421 adults with immediate-release venlafaxine and 2461 adults with extended-release venlafaxine) for a total of 53 260 person-week observations.
Data Synthesis
Suicidal thoughts and behavior decreased over time for adult and geriatric patients randomized to fluoxetine or venlafaxine compared with placebo, but no differences were found for youths. In adults, reduction in suicide ideation and attempts occurred through a reduction in depressive symptoms. In all age groups, severity of depression improved with medication and was significantly related to suicide ideation or behavior.
Conclusions
Fluoxetine and venlafaxine decreased suicidal thoughts and behavior for adult and geriatric patients. This protective effect is mediated by decreases in depressive symptoms with treatment. For youths, no significant effects of treatment on suicidal thoughts and behavior were found, although depression responded to treatment. No evidence of increased suicide risk was observed in youths receiving active medication. To our knowledge, this is the first research synthesis of suicidal thoughts and behavior in depressed patients treated with antidepressants that examined the mediating role of depressive symptoms using complete longitudinal person-level data from a large set of published and unpublished studies.
In 2004, the US Food and Drug Administration (FDA) issued a black box warning for antidepressants and risk of suicide in children and adolescents. No actual suicides occurred in these trials with either antidepressant or placebo, so this concern was based primarily on suicide ideation and attempts.1 In 2006, the FDA extended the warning to young adults aged 18 to 25 years.2 The original warning was based on a meta-analysis of adverse event reports (AERs) of suicidal thoughts and behavior from 25 clinical randomized controlled trials (RCTs) conducted by the pharmaceutical companies in pursuit of approval of antidepressant medications. These trials were typically short term and limited to the newer antidepressant classes of selective serotonin reuptake inhibitors and serotoninnorepinephrine reuptake inhibitors. Results of the analysis revealed an overall odds ratio (OR) of 1.78 (95% CI, 1.14–2.77), indicating that the rate of suicidal thoughts and behavior from AERs was significantly higher in children randomized to active antidepressant treatment relative to placebo. The extension of the warning to young adults was based on a second meta-analysis of AERs in 372 RCTs in 99 839 adult patients. The FDA found a result that approached significance for young adults aged 18 to 24 years (OR=1.62; 95% CI, 0.97–2.71) and, in contrast, a significantly decreased risk in adults aged 25 to 64 years (OR=0.79; 95% CI, 0.64–0.98) and geriatric patients aged 65 years and older (OR=0.37; 95% CI, 0.18–0.76).
A similar analysis conducted by the FDA on prospectively measured suicidal thoughts and behavior in the youth studies failed to detect any evidence of increased risk of antidepressant treatment in these same studies.1 Their analysis focused on study end point and did not make use of the full longitudinal data that were available in these studies. No analysis of the prospective rating scale data was presented by the FDA for studies of adults.
To help determine what impact antidepressants have on the course of depression and suicidal thoughts and behavior in different age groups, we obtained complete longitudinal data for RCTs of fluoxetine hydrochloride conducted by Eli Lilly and Co, the Treatment for Adolescents With Depression Study of fluoxetine in children by the National Institute of Mental Health,3 and adult studies for venlafaxine hydrochloride conducted by Wyeth. These patient-level data allow us to do the following: (1) estimate rates of change in suicidal thoughts and behavior during the course of treatment; (2) study the relationship between depression severity and suicidal thoughts and behavior; and (3) determine the extent to which changes in depressive symptoms mediate the relationship between antidepressant treatment and suicidal thoughts and behavior. These analyses substantially expand the original analyses conducted by the FDA in children by including the complete longitudinal record for each patient and provide similar analyses for adult and geriatric populations, which were not previously reported by the FDA. This approach seeks to provide the clinician with a more accurate risk-benefit estimation for using antidepressants for major depressive disorder at all ages.
METHODS
STUDY DATA
A detailed description of the study data is available on request from the authors and will be available in a related publication.4
Our measures of suicide ideation and behavior were item 3 of the Hamilton Depression Rating Scale (HAM-D; used in adult and geriatric patients) and item 13 of the Childhood Depression Rating Scale–Revised (CDRS-R; used in children and adolescents). These measures were obtained on a weekly basis. The original response categories are provided in Table 1.
Table 1.
Suicide Risk Response Categories
| Score | Description |
|---|---|
| HAM-D item 3 | |
| 0 | Absent |
| 1 | Feels life is not worth living |
| 2 | Wishes he or she were dead or any thoughts of possible death to self |
| 3 | Suicide ideas or gestures |
| 4 | Attempts at suicide, any serious attempt |
| CDRS-R item 13 | |
| 1 | Understands the word suicide but does not apply term to self |
| 2 | Sharp denial of suicidal thoughts |
| 3 | Has thoughts about suicide, usually when angry |
| 4 | Between 3 and 5 |
| 5 | Has recurrent thoughts of suicide |
| 6 | Between 5 and 7 |
| 7 | Has made suicide attempt within the last month or is actively suicidal |
Abbreviations: HAM-D, Hamilton Depression Rating Scale; CDRS-R, Childhood Depression Rating Scale–Revised.
Our primary analyses used these as ordinal scales after collapsing the first 2 categories for the HAM-D and for the CDRS-R. These categories (feels life is not worth living [HAM-D] or sharp denial of suicidal thoughts [CDRS-R]) do not meet the threshold for suicide ideation (ie, passive thoughts about wanting to be dead or active thoughts about killing oneself)5 and have not been found to be predictive of later suicide in psychiatric out-patient clinic patients6 or nonfatal suicide attempts in RCTs.7 Descriptive analyses of suicide ideation and behavior were also provided. Suicide ideation and behavior were operationally defined as a HAM-D item 3 score greater than 2 (a score of 3 indicates suicide ideas or gestures) or a CDRS-R item 13 score greater than 2 (a score of 3 indicates that the patient has thoughts about suicide, usually when angry), based on the definitions in the article by Posner et al.5 For completeness, we augmented these measures with AERs of suicide attempts and suicide, which were available for the studies by Eli Lilly and Co and the Treatment for Adolescents With Depression Study. These AERs were coded as 7 for children and 4 for adults; timing was coded by date at onset. These collapsed ordinal scales are referred to later as suicide risk measures. For an overall measure of depressive symptoms, we summed all remaining HAM-D or CDRS-R items, excluding the item related to suicide to avoid bias in estimating the relationship between depression severity and suicide risk. This overall measure of depressive symptoms was used to assess the mediating effect of an antidepressant on suicide risk reduction.
STATISTICAL ANALYSIS
We first examined the observed distribution of suicide ideation or behavior as a function of time, treatment, and age group (Table 2). After 8 weeks the data were sparse and were therefore combined into a single category (≥9 weeks). The maximum length of follow-up was 130 days. The observed proportions were based on numbers of patients at risk in each condition. Unlike our companion study4 where we restricted analysis to the first 6 weeks of treatment so that all studies included all time points (ie, study and time are unconfounded), in this study we used all available data during active treatment so that we did not miss any adverse events. Second, we examined how antidepressant treatment affected suicide risk over time, using a 3-level mixed-effects ordinal logistic regression model in SuperMix.8 As in the companion article,4 we conducted an overall analysis of both drugs in adult and geriatric patients (ie, all trials using the HAM-D) followed by separate analyses for adult, geriatric, and youth trials of fluoxetine and adult trials of immediate-release and extended-release venlafaxine. These analyses accounted for exact days of assessment and controlled for individual-level covariates of age and sex. Random effects were included at both the patient and trial levels to account for the correlation of repeated measurements within patients and the correlation of patients within studies. Incomplete data were treated as missing at random in these analyses.9 To test the hypothesis that suicide risk is mediated by changes in depression severity, a second mixed-effects ordinal logistic regression model was used in which depression severity (HAM-D or CDRS-R total scores eliminating the suicide item) and the treatment×depression severity interactions were added to the model as time-varying covariates predicting suicide risk status. The interaction term allows the relationship between depression severity and suicide risk to be different for treated and control patients.10 We then conducted a mediational analysis to determine the extent to which reduction in the time-dependent depressive symptom score accounted for the effect of treatment on concurrent suicide risk. In addition, we fit a 3-level mixed-effects linear regression model to evaluate the effect of treatment on depression severity (HAM-D or CDRS-R scores independent of the suicide items) using all available data. The following are key requirements for a variable to be a mediator: (1) the putative mediator is affected by treatment; (2) the mediator is related to the outcome, either as a main effect or in interaction with treatment10; and (3) the mediator contribution reduces the effect of the treatment on suicide risk status. In the companion article,4 we have demonstrated that treatment is significantly related to the mediator (change in depression severity) for both drugs and all 3 age groups through 6 weeks; for these mediational analyses, we report effects on depression severity through 12 weeks. In this article, we test the hypothesis that the mediator (depression severity) is related to the outcome (suicide risk) and accounts for a significant proportion of the observed reduction in suicide ideation or behavior. The difference in rates of change (ie, slopes) in suicide risk between treated and control patients is measured by the treatment×time interaction. Comparison of models with and without the mediator effects allows us to determine the extent to which the effect of treatment on suicide risk is mediated by the effect of treatment on depression severity. Because these models are on a logit scale, a calibration of variances for these coefficients is necessary to compare them directly.11 The proportion of the mediation was then computed as 1 minus the ratio of the treatment×time interactions for the model with the mediator to the model without the mediator.11
Table 2.
Observed Suicidal Thoughts and Behavior Over Time
| Week | Fluoxetine Hydrochloride, No. (%)
|
Venlafaxine Hydrochloride, No. (%)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Youth
|
Adult
|
Geriatric
|
IR
|
ER
|
||||||
| Placebo | Treatment | Placebo | Treatment | Placebo | Treatment | Placebo | Treatment | Placebo | Treatment | |
| 0 | 315 (20.6) | 393 (18.8) | 1008 (5.4) | 1627 (4.7) | 470 (3.2) | 490 (2.7) | 919 (6.3) | 1502 (5.5) | 994 (1.6) | 1467 (1.7) |
| 1 | 114 (13.2) | 139 (14.4) | 883 (3.6) | 1364 (2.4) | 354 (2.5) | 368 (1.6) | 716 (4.9) | 1061 (2.5) | 871 (1.0) | 1276 (0.9) |
| 2 | 189 (14.8) | 253 (9.5) | 904 (4.5) | 1382 (2.1) | 393 (1.8) | 409 (1.7) | 719 (2.8) | 1096 (1.3) | 903 (1.0) | 1264 (0.6) |
| 3 | 148 (8.8) | 205 (8.8) | 731 (2.2) | 1261 (1.7) | 360 (2.2) | 370 (0.5) | 662 (1.7) | 1034 (1.2) | 819 (1.1) | 1145 (0.5) |
| 4 | 105 (14.3) | 139 (5.8) | 683 (2.2) | 1151 (1.1) | 364 (1.9) | 360 (1.4) | 641 (1.7) | 965 (0.4) | 807 (0.7) | 1182 (0.3) |
| 5 | 90 (15.6) | 96 (11.5) | 609 (1.3) | 1006 (0.7) | 313 (1.6) | 339 (2.1) | 196 (1.5) | 321 (0.9) | 199 (0.5) | 278 (1.8) |
| 6 | 167 (8.4) | 183 (10.9) | 529 (1.7) | 910 (1.2) | 309 (1.6) | 310 (0.6) | 397 (1.3) | 619 (1.0) | 614 (0.7) | 900 (0.6) |
| 7 | 78 (9.0) | 96 (14.6) | 335 (1.5) | 491 (0.4) | 160 (1.3) | 144 (2.8) | 196 (1.0) | 357 (1.1) | 169 (1.2) | 276 (0.7) |
| 8 | 50 (4.0) | 68 (8.8) | 297 (0.7) | 259 (1.2) | 53 (1.9) | 66 (1.5) | 117 (0) | 177 (0.6) | 448 (0.2) | 725 (0.6) |
| ≥9 | 81 (13.6) | 105 (4.8) | 396 (0) | 288 (0) | 108 (3.7) | 118 (0) | 57 (1.8) | 116 (0) | 300 (0.7) | 690 (0.6) |
Abbreviations: ER, extended release; IR, immediate release.
Results are reported as marginal maximum likelihood estimates (MMLEs), standard errors, and probability values (P values) of the treatment×time interaction, main effect of depression severity, and treatment×severity interaction. Estimates of marginal (population-averaged) ORs9 were then used to describe the percentage reduction in the probability of suicide risk following 8 weeks for treated vs control patients. We evaluated models with nonlinear time trends; however, the linear models provided the best overall fit.
There were relatively few suicide attempts and suicides (a total of 20 attempts and 2 suicides in 21 patients among 9185 patients across all age cohorts and drugs), allowing limited power to detect potential differences. Overall, a total of 16 suicide attempts were identified through the standardized CDRS-R or HAM-D measures. An additional 6 suicidal events were identified from AERs, 4 attempts and 2 suicides. These additional 6 AERs were coded using the Columbia Classification Algorithm of Suicide Assessment.5 Of the 2 suicides, one was by an adult receiving fluoxetine and the other was a geriatric patient receiving placebo. Of the 22 suicidal events, 9 were recorded at baseline (prior to initiation of treatment), 3 in week 1, 3 in week 2, 5 in week 3, 1 in week 4, and 1 in week 5.
RESULTS
The reported rates of suicide risk at baseline were 5% for adults, 3% for geriatric patients, and 20% for youths. In general, rates of suicide risk were reduced by 50% or more for both treated and control groups over time. Table 2 illustrates how suicide risk varies from baseline, where randomization produced virtually identical rates. For all ages and both drugs, rates of suicide risk among patients were not markedly different from those of control patients but were generally lower in treated patients than in control patients over time (starting from the second week). We note, however, that the simple observed proportions in Table 2 may be biased because they are restricted to patients with data at each week, and these patients may not be representative of all randomized patients, especially at later times. The mixed-effects model results described later (summarized in Table 3) make use of all available data for each subject in constructing the average time trends and therefore are unbiased in this respect.
Table 3.
Marginal Maximum Likelihood Estimates, Standard Errors, and P Values for Each Cohort and Effect
| Statistic | Overall | Fluoxetine Hydrochloride
|
Venlafaxine Hydrochloride
|
|||
|---|---|---|---|---|---|---|
| Youth | Adult | Geriatric | IR | ER | ||
| Treatment on Suicide Risk | ||||||
| MMLE | −0.2091 | 0.0809 | −0.1689 | −0.1479 | −0.3777 | −0.1501 |
| SE | 0.0289 | 0.0595 | 0.0644 | 0.0688 | 0.0650 | 0.0565 |
| P value | <.001 | .17 | .009 | .03 | <.001 | .008 |
|
| ||||||
| Treatment on Depressive Symptoms at 12 wk | ||||||
| MMLE | −4.0337 | −3.8976 | −4.2882 | −2.7224 | −5.0358 | −3.5658 |
| SE | 0.2730 | 1.5238 | 0.5645 | 0.8308 | 0.5032 | 0.4402 |
| P value | <.001 | .01 | <.001 | .001 | <.001 | <.001 |
|
| ||||||
| Depressive Symptoms on Suicide Risk | ||||||
| MMLE | 0.3070 | 0.1261 | 0.3091 | 0.2963 | 0.3219 | 0.2923 |
| SE | 0.0094 | 0.0116 | 0.0206 | 0.0289 | 0.0168 | 0.0156 |
| P value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
|
| ||||||
| Treatment×Depressive Symptoms Interaction on Suicide Risk | ||||||
| MMLE | 0.0159 | −0.0046 | 0.0342 | 0.0417 | 0.0056 | 0.0106 |
| SE | 0.0127 | 0.0141 | 0.0283 | 0.0417 | 0.0221 | 0.0211 |
| P value | .21 | .74 | .23 | .32 | .80 | .62 |
|
| ||||||
| Treatment on Suicide Risk Adjusted for Depressive Symptoms | ||||||
| MMLE | −0.0620 | 0.1293 | 0.0192 | −0.1501 | −0.1672 | 0.0088 |
| SE | 0.0314 | 0.0662 | 0.0674 | 0.0788 | 0.0631 | 0.0515 |
| P value | .048 | .05 | .78 | .06 | .008 | .86 |
Abbreviations: ER, extended release; IR, immediate release; MMLE, marginal maximum likelihood estimate.
OVERALL ANALYSIS OF ADULT AND GERIATRIC PATIENTS
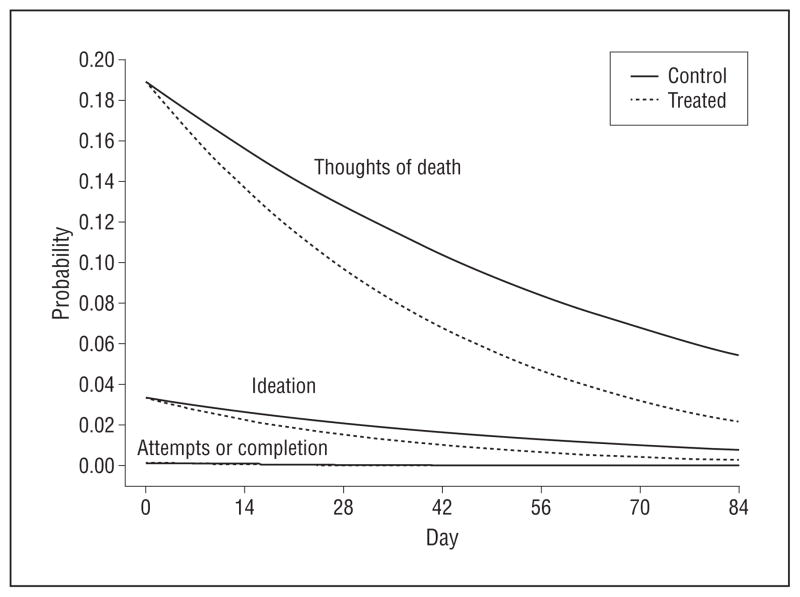
We found a statistically significant difference in the reduction in suicide risk over time between treated patients and those receiving placebo (MMLE=−0.2091; SE=0.0289; P<.001) (Figure 1). Thus, treated patients had a greater reduction in suicide risk over time relative to control patients receiving placebo. The rate of change was 58% faster in treated patients relative to control patients, which results in an estimated 78.9% decrease in the probability of suicidal risk for control patients after 8 weeks of study participation and a 90.5% decrease for treated patients. Figure 1 displays the estimated probabilities for each of the 3 ordinal response categories in treated and control patients and reveals that most suicidal events (19% at baseline) were of low severity (thoughts of death), followed by ideation with a baseline rate of 3% and suicide attempts or completion at 0.1% at baseline. The beneficial effect of treatment on the probability of suicide risk is apparent approximately 2 weeks following treatment initiation.
Figure 1.
Probabilities of suicide risk in adult and geriatric fluoxetine hydrochloride and venlafaxine hydrochloride studies. Solid lines indicate estimated probabilities for control patients receiving placebo; dashed lines, estimated probabilities for treated patients; thoughts of death curves, “wishes he or she were dead or any thoughts of possible death to self” or worse; ideation curves, “suicide ideas or gestures” or worse; and attempts or completion curves, “suicide attempts or suicides.”
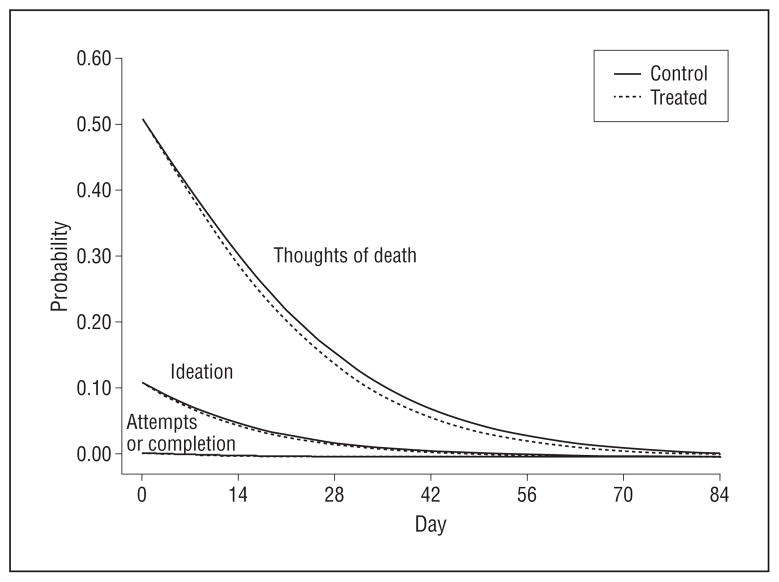
The mediation model of all adult and geriatric patients revealed the following. First, there was a significant overall faster reduction in depressive symptoms (excluding suicidal thoughts and behavior) over time for treated patients vs control patients (treatment difference at 12 weeks: MMLE=−4.0337; SE=0.2730; P<.001), as we found in the companion study.4 This estimate indicates an average estimated difference in depression severity of 4.03 HAM-D units between treated and control patients at 12 weeks. Second, we found a statistically significant main effect of depression severity on contemporaneous suicide risk (MMLE=0.3070; SE=0.0094; P<.001), indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was similar for treated and control patients (MMLE=0.0159; SE=0.0127; P=.21). Following adjustment for depression severity (Figure 2), the treatment×time interaction was still statistically significant (MMLE=−0.0620; SE=0.0314; P=.048); however, it was dramatically reduced from the model that did not adjust for depression severity. The percentage of the overall treatment effect attributable to mediation was 77%. This finding reveals that most of the beneficial effect of antidepressant treatment on suicide risk is mediated through the effect of antidepressant treatment on depression severity.
Figure 2.
Probabilities of suicide risk adjusting for depression severity in adult and geriatric fluoxetine hydrochloride and venlafaxine hydrochloride studies. Solid lines indicate estimated probabilities for control patients; dashed lines, estimated probabilities for treated patients; thoughts of death curves, “wishes he or she were dead or any thoughts of possible death to self” or worse; ideation curves, “suicide ideas or gestures” or worse; and attempts or completion curves, “suicide attempts or suicides.”
To interpret these findings in terms of population-averaged effects, we transformed these individual-level effect parameters for models into population rates of suicide ideation or attempts over time, adjusted for the mediator. Figure 2 illustrates this mediational effect by plotting the marginal probability of suicide risk for each threshold in treated and control patients, adjusting for depression severity. In terms of depression severity, we have selected a hypothetical patient who begins the trial severely depressed (HAM-D total score=30) and improves at a rapid rate of 0.35 HAM-D units per day through 12 weeks. In contrast to the clear intervention differences in Figure 1, Figure 2 reveals that there is essentially no difference in suicide risk attributable to treatment once the effect of depression severity is controlled, illustrating the previous mediational analysis result.
ADULT FLUOXETINE STUDIES
A statistically significant treatment×time interaction was found in adult fluoxetine studies (MMLE=−0.1689; SE=0.0644; P=.009), indicating that treated patients had a significantly greater reduction in suicide risk over time relative to control patients receiving placebo. The rate of change was 57% faster in treated patients relative to control patients, resulting in an 83.0% decrease in the probability of suicide risk for control patients after 8 weeks of study participation and a 91.6% decrease for treated patients. Fluoxetine produced a faster decline in depressive symptoms over time compared with placebo (treatment difference at 12 weeks: MMLE = −4.2882; SE=0.5645; P<.001). The mediation model revealed a statistically significant main effect of depression severity (MMLE=0.3091; SE=0.0206; P<.001), indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was the same for treated and control patients (MMLE=0.0342; SE=0.0283; P=.23). Following adjustment for depression severity, the difference in rates of change in suicide risk between treated and control patients was not statistically significant (MMLE=0.0192; SE=0.0674; P=.78). The percentage of the overall treatment effect attributable to mediation was 82%. This finding reveals that the beneficial effect of fluoxetine treatment on suicide risk in adults is mediated through the effect of antidepressant treatment on depression severity.
ADULT IMMEDIATE-RELEASE VENLAFAXINE STUDIES
A statistically significant treatment×time interaction was found in adult immediate-release venlafaxine studies (MMLE=−0.3777; SE=0.0650; P<.001), indicating that treated patients had a significantly greater reduction in suicide risk over time relative to control patients receiving placebo. The rate of change was 82% faster in treated patients relative to control patients, resulting in an 81.0% decrease in the probability of suicidal thoughts or behavior for control patients after 8 weeks of study participation and a 93.5% decrease for treated patients. Immediate-release venlafaxine produced a faster decline in depressive symptoms over time than did placebo (treatment difference at 12 weeks: MMLE=−5.0358; SE=0.5032; P<.001). The mediation model revealed a statistically significant main effect of depression severity (MMLE=0.3219; SE=0.0168; P<.001), indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was the same for treated and control patients (MMLE=0.0056; SE=0.0221; P=.80). Following adjustment for depression severity, the treatment×time interaction remained statistically significant (MMLE=−0.1672; SE=0.0631; P=.008); however, the magnitude was substantially reduced. The percentage of the overall treatment effect attributable to mediation was 81%. This finding reveals that most of the beneficial effect of immediate-release venlafaxine treatment on suicide risk in adults is mediated through the effect of antidepressant treatment on depression severity.
ADULT EXTENDED-RELEASE VENLAFAXINE STUDIES
A statistically significant treatment×time interaction was found in adult extended-release venlafaxine studies (MMLE=−0.1501; SE=0.0565; P=.008), indicating that treated patients had a significantly greater reduction in suicide risk over time relative to control patients receiving placebo. The rate of change was 37% faster in treated patients relative to control patients, resulting in a 77.1% decrease in the probability of suicide risk for control patients after 8 weeks of study participation and an 88.7% decrease for treated patients. Patients receiving extended-release venlafaxine experienced a faster decline in depressive symptoms (treatment difference at 12 weeks: MMLE=−3.5658; SE=0.4402; P<.001) relative to control patients. The mediation model revealed a statistically significant main effect of depression severity (MMLE=0.2923; SE=0.0156; P<.001), indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was the same for treated and control patients (MMLE=0.0106; SE=0.0211; P=.62). Following adjustment for depression severity, the treatment×time interaction was no longer statistically significant (MMLE=0.0088; SE=0.0515; P=.86). The percentage of the overall treatment effect attributable to mediation was 83%. This finding reveals that the beneficial effect of extended-release venlafaxine treatment on suicide risk in adults is mediated through the effect of antidepressant treatment on depression severity.
GERIATRIC FLUOXETINE STUDIES
A statistically significant treatment×time interaction was found in geriatric fluoxetine studies (MMLE=−0.1479; SE=0.0688; P=.03), indicating that treated patients had a significantly greater reduction in suicide risk over time relative to control patients receiving placebo. The rate of change was 66% faster in treated patients relative to control patients, resulting in a 69.0% decrease in the probability of suicide risk for control patients after 8 weeks of study participation and an 84.0% decrease for treated patients. Geriatric patients receiving fluoxetine decreased their depressive symptoms more quickly than did patients receiving placebo (treatment difference at 12 weeks: MMLE=−2.7224; SE=0.8308; P=.001). The mediation model revealed a statistically significant main effect of depression severity (MMLE=0.2963; SE=0.0289; P<.001), indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was the same for treated and control patients (MMLE=0.0417; SE=0.0417; P=.32). Following adjustment for depression severity, the treatment×time interaction was no longer statistically significant (MMLE=−0.1501; SE=0.0788; P=.06). The percentage of the overall treatment effect attributable to mediation was 57%. This finding reveals that slightly more than half of the beneficial effect of fluoxetine treatment relative to placebo on suicide risk in geriatric patients is mediated through the effect of antidepressant treatment on depression severity (ie, partial mediation).
YOUTH FLUOXETINE STUDIES
The treatment×time interaction was not statistically significant in youth fluoxetine studies (MMLE=0.0809; SE=0.0595; P=.17), indicating that we could find no difference between treated and control patients in terms of suicide risk. The marginal ORs indicated a 61.3% decrease in the probability of suicidal thoughts or behavior for control patients after 8 weeks of study participation and a 50.3% decrease for treated patients. Youth patients receiving fluoxetine decreased their depressive symptoms more quickly than patients receiving placebo (treatment difference at 12 weeks: MMLE=−3.8976; SE=1.5238; P=.01). A statistically significant main effect of depression severity (MMLE=0.1261; SE=0.0116; P<.001) on suicide risk was found, indicating that depression severity is positively associated with suicide risk. The treatment×depression severity interaction was not statistically significant, indicating that the relationship between depression severity and suicide risk was the same for treated and control patients (MMLE = −0.0046; SE=0.0141; P=.74). Despite a strong association between depression severity and suicide risk in youths, treatment with fluoxetine was not found to be related to suicide risk when compared with placebo.
COMMENT
Results of the first analysis of all longitudinal suicidal event data across published and unpublished placebo-controlled RCTs of fluoxetine (adult, youth, and geriatric patients) and venlafaxine (adults) revealed that there was no evidence of increased suicide risk with treatment. Except for youths, the level of suicide risk for most subjects in these trials was low, and for all groups there was a major reduction in risk over time. Most events were suicidal ideation. We found that for adults treated with fluoxetine, extended-release venlafaxine, or immediate-release venlafaxine and geriatric patients treated with fluoxetine, treatment resulted in significant decreases relative to placebo in suicide risk measures over time. No statistically significant differences were found for fluoxetine in youths. Suicide risk was strongly related to severity of depression, and changes over time in suicide risk closely mirrored those of depression severity changes over this same period in both youths and adults. Other studies have reported that the rate of suicidal behavior in major depressive disorder is much higher during episodes than between episodes.12 For all adult trials, depression severity mediated the effect of antidepressant medication on suicide risk. Mediation accounted for approximately 80% of the overall treatment effect in adults, but less (57%) for geriatric patients. For youths, depression severity was strongly related to suicide risk and depression responded to treatment, but no effect of treatment on suicide risk was found.
These results clarify the relationship between suicidal thoughts and behavior and antidepressant treatment, particularly in adult and geriatric patients, because they suggest that adult and geriatric patients whose symptoms do not diminish remain at higher suicide risk. Variation in response to antidepressant treatment is substantial; in one trial, it was estimated that more than half of adults were nonresponsive to placebo and 30% were nonresponsive to a selective serotonin reuptake inhibitor.13 The STAR*D results indicate that a sizable proportion of those who are nonresponsive to a first antidepressant can improve under an alternative medication.14 Our findings emphasize the need to successfully treat episodes of major depressive disorder to lower the suicide risk. Our results for adult and geriatric patients, which show statistically significant beneficial effects of antidepressant treatment on suicide risk, largely agree with the FDA findings and further demonstrate the mediating role of depressive symptom change. With respect to youths, we did not replicate the FDA’s finding of increased risk with antidepressant treatment. However, the FDA found that fluoxetine was the only antidepressant that was effective for depression. Our results apply to fluoxetine and it remains to be determined whether the findings generalize to other antidepressants. Newer, improved prospective measures of suicidal ideation and behavior now exist,5 are now mandated by the FDA, and should be analyzed as done here.
This study avoided the problem of publications being biased in favor of positive clinical trials by examining all industry trials of fluoxetine and venlafaxine but nevertheless did not have enough statistical power to analyze suicidal ideation and actual suicidal behavior separately. Suicidal ideation rates and the ratios to suicides and suicide attempts are higher in youths compared with adults, making ideation a potentially weaker indicator of risk of behavior in youths.15
The mediation analyses show the importance of antidepressant response in mediating the benefit of antidepressants for suicide risk in adult and geriatric patients. It is important to note that these analyses could be done only by combining individual patient-level data in the same analysis. The methods we have used here, nonlinear mixed-effects regression models and mediation analysis, are applied to answer complex hypotheses with individual-level data that are synthesized across multiple trials. These methods of person-level meta-analysis or integrative data analysis16 are superior to standard meta-analysis,17 which cannot adjust adequately for different time frames, different ways of handling missing data, and different analytical choices for mediation analysis. A second critically important aspect of these studies is that they all have random assignment and blinded assessment. In all trials, these procedures balanced suicidal thought and behavior incidence at baseline between treated and control patients and assured equivalent assessment procedures. Randomization brings about balance in both observable and unobservable potential confounders, whereas no such guarantee is available for observational data.
A limitation of these studies is that they rely on a single ordinal clinician rating of suicidal thoughts and behavior, supplemented by AERs of suicide attempts or suicides. For youths, the FDA analyses that relied on suicide-related AERs in the clinical records alone found statistically significant increased risk of suicidal thoughts and behavior for those treated with antidepressants compared with placebo, whereas we did not find this effect in our analysis of the systematically collected CDRS-R suicide item that was augmented with the AERs of suicidal behavior. There is debate in the literature on how best to examine mediation in nonlinear longitudinal models. In particular, the proportion of reduction in effect due to mediation, which we used in this article, is known to be unstable when the treatment effect is small.11 For adults, the large treatment effects and depressive symptom effects on suicide risk mitigate this concern, but the percentage reduction for geriatric patients has more uncertainty.
Unanswered questions remain. While the findings of mediation are clear for adults in 3 sets of trials and geriatric patients in 1 set of trials, we did not find a statistically significant effect of treatment on suicide in youths, despite a large overall reduction in depressive symptoms. We do not yet know why some youths whose depressive symptoms are reduced continue to have suicidal ideation and behavior. Perhaps other psychopathology plays a more important role in suicidal behavior and ideation such as aggressive impulsive traits in youths.18 Thus, even if antidepressants reduce depressive symptoms overall in youths, it is possible that a subset may retain some level of risk for suicidal ideation or attempts. The overall rate, however, was not significantly greater than that found for youths randomized to placebo. It was the finding of an increased rate of ideation and attempts using AERs that formed the entire basis for the FDA black box warning, and notably, we do not find such a signal using data that draw on both AERs and prospective systematic ratings of suicidal ideation and behavior.
A limitation of RCTs for studying suicide risk is that suicidal patients are often excluded from such studies. While this may be true, we note that the rate of suicidal thoughts and behavior were highest at baseline, and 9 of the 20 suicide attempts occurred prior to treatment initiation (ie, were rated as being present at baseline).
In summary, we found that treatment with fluoxetine and venlafaxine decreased suicide risk in adult and geriatric patients and that the effect of treatment on depression severity appears to be the mechanism whereby antidepressants lower suicide risk in adult and geriatric patients. We found no evidence that fluoxetine increased risk of suicidal thoughts or behavior in youths.
Acknowledgments
Funding/Support: This work was supported by grants MH062185 (Dr Mann), R56 MH078580 (Drs Gibbons and Brown), MH8012201 (Drs Gibbons and Brown), and MH040859 (Dr Brown) from the National Institute of Mental Health and grant 1U18HS016973 from the Agency for Healthcare Research and Quality (Dr Gibbons).
Footnotes
Author Contributions: Dr Gibbons had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional Contributions: Data were supplied by the National Institute of Mental Health (Treatment for Adolescents With Depression Study), Wyeth, and Eli Lilly and Co.
Financial Disclosure: Dr Gibbons has served as an expert witness for the US Department of Justice, Wyeth, and Pfizer Pharmaceuticals in cases related to antidepressants and anticonvulsants and suicide. Dr Brown directed a suicide prevention program at the University of South Florida that received funding from JDS Pharmaceuticals. Dr Mann has received research support from GlaxoSmithKline and Novartis.
References
- 1.Hammad TA. [Accessed December 15, 2010];Review and evaluation of clinical data. http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf.
- 2.US Food and Drug Administration. [Accessed December 15, 2010];Clinical review: relationship between antidepressant drugs and suicidality in adults. http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdf.
- 3.March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J Treatment for Adolescents With Depression Study (TADS) Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 4.Gibbons RD, Hur K, Brown CH, Davis JM, Mann JJ. Who benefits from antidepressants? synthesis of 6-week patient-level outcomes from double-blind placebo controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry. doi: 10.1001/archgenpsychiatry.2011.2044. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown GK, Steer RA, Henriques GR, Beck AT. The internal struggle between the wish to die and the wish to live: a risk factor for suicide. Am J Psychiatry. 2005;162(10):1977–1979. doi: 10.1176/appi.ajp.162.10.1977. [DOI] [PubMed] [Google Scholar]
- 7.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedeker D, Gibbons RD, Du Toit SHC, Patterson D. SuperMix: A Program for Mixed-Effects Regression Models. Chicago, IL: Scientific Software International; 2008. [Google Scholar]
- 9.Siddique J, Brown CH, Hedeker D, Duan N, Gibbons RD, Miranda J, Lavori PW. Missing data in longitudinal trials, part B: analytic issues. Psychiatr Ann. 2008;38(12):793–801. doi: 10.3928/00485713-20081201-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraemer HC, Gibbons RD. Why does the randomized clinical trial methodology so often mislead clinical decision making? focus on moderators and mediators of treatment. Psychiatr Ann. 2009;39(7):736–745. doi: 10.3928/00485713-20090625-06. [DOI] [Google Scholar]
- 11.MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint effect in logistic and probit regression. Clin Trials. 2007;4(5):499–513. doi: 10.1177/1740774507083434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161(8):1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 13.Muthén B, Brown HC. Estimating drug effects in the presence of placebo response: causal inference using growth mixture modeling. Stat Med. 2009;28(27):3363–3385. doi: 10.1002/sim.3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007;164(2):201–204. doi: 10.1176/ajp.2007.164.2.201. [DOI] [PubMed] [Google Scholar]
- 15.Mann JJ, Emslie G, Baldessarini RJ, Beardslee W, Fawcett JA, Goodwin FK, Leon AC, Meltzer HY, Ryan ND, Shaffer D, Wagner KD. ACNP Task Force report on SSRIs and suicidal behavior in youth. Neuropsychopharmacology. 2006;31 (3):473–492. doi: 10.1038/sj.npp.1300958. [DOI] [PubMed] [Google Scholar]
- 16.Curran PJ, Hussong AM. Integrative data analysis: the simultaneous analysis of multiple data sets. Psychol Methods. 2009;14(2):81–100. doi: 10.1037/a0015914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, Vigna-Taglianti F, Howe G, Masyn K, Wang W, Muthén B, Stephens P, Grey S, Perrino T Prevention Science and Methodology Group. Methods for synthesizing findings on moderation effects across multiple randomized trials [published online March 1, 2011] Prev Sci. doi: 10.1007/s11121-011-0207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar JO, Mann JJ. Familial pathways to early-onset suicide attempt: risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry. 2002;59(9):801–807. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]