Abstract
Aims/Hypothesis
This study was aimed at assessing oxidative stress in LDL from obese patients with metabolic syndrome (MetS) compared with LDL from type 2 diabetic patients or control volunteers, and determining their effects on platelets.
Methods
The profiles of lipids, fatty acids and fatty acid oxidation products were determined in LDL isolated from plasma of MetS patients, type 2 diabetic patients and volunteers (n=10 per group). The effects of LDL isolated from these participants on platelet arachidonic acid signaling cascade and aggregation were investigated.
Results
Compared with LDL from control volunteers, LDL from obese MetS and type 2 diabetic patients contained lower cholesteryl esters, higher triacylglycerols and lower ethanolamine plasmalogens levels. Proportions of linoleic acid were decreased in phosphatidylcholine and cholesteryl esters in patients’ LDL. Among the markers of lipid peroxidation, oxidation products of linoleic acid (hydroxy-octadecadienoic acids) and malondialdehyde were increased by 59% and 2-fold, respectively in LDL from MetS patients and to the same extent in LDL from type 2 diabetic patients. LDL from MetS patients were as potent as LDL from type 2 diabetic patients in activating platelet arachidonic acid signaling cascade through increased phosphorylation of p38 MAPK and cytosolic phospholipase A2, and increased thromboxane B2 formation. LDL from patients with MetS and type 2 diabetes potentiated 3-fold and 3.5-fold respectively platelet aggregation whereas control LDL had no activating effects on platelets.
Conclusions/interpretation
MetS in obese patients, without or with diabetes, is associated with increased oxidative stress in LDL, which trigger platelet activation.
The protocol is registered in ClinicalTrials.gov as NCT00932087.
Keywords: Adult; Aged; Arachidonic Acid; metabolism; Biological Markers; blood; Blood Platelets; enzymology; metabolism; Diabetes Mellitus, Type 2; blood; complications; metabolism; Humans; Lipid Peroxidation; Lipids; blood; Lipoproteins, LDL; blood; chemistry; metabolism; Male; Metabolic Syndrome X; complications; Middle Aged; Obesity; blood; complications; metabolism; Oxidative Stress; Phospholipases A2, Secretory; blood; metabolism; Platelet Activation; Signal Transduction
Keywords: Lipid peroxidation, Fatty acids, LDL, Oxidized LDL, Platelets, Metabolic syndrome, Type 2 diabetes, Obesity
Introduction
There is strong evidence that type 2 diabetes is associated with increased oxidative stress [1] which may contribute to the elevated risk of atherothrombosis. Oxidatively modified LDL are implicated in the pathogenesis of atherosclerosis and could be present in plasma from type 2 diabetic patients. From one hand, autoantibodies to oxidized LDL were found to be increased in type 2 diabetic patients with macrovascular disease [2]. From the other hand, we recently showed that LDL from type 2 diabetic patients contained increased levels of lipid peroxides [3]. There is controversy on the occurrence of oxidative stress in patients with metabolic syndrome (MetS). Some studies showed higher levels of circulating oxidized LDL [4–6] and isoprostanes [7] in individuals with MetS. Other studies did not show any difference in oxidized LDL levels [8] or markers of oxidative damage (plasma F2-isoprostanes, HETE) [9] between MetS patients and healthy individuals. In addition, most studies focused on lipid peroxides issued from the non enzymatic peroxidation of arachidonic acid [7, 9] and paradoxically no data, to our knowledge, are available on circulating lipid peroxides issued from linoleic acid although it is the main polyunsaturated fatty acid (PUFA) in LDL. Considering that MetS increases the risk for the development of type 2 diabetes and cardiovascular diseases [10, 11], and that oxidative stress plays an important role in type 2 diabetes, it is important to determine whether oxidized LDL are already present in plasma from volunteers with a MetS.
Increased platelet activation occurs in type 2 diabetes [12] and MetS [13, 14] and may represent a key contributing factor in the process of atherosclerosis and its thrombotic complications. Oxidative stress has been identified as one of the factors closely associated with platelet hyperactivation in diabetes [12] and lipid hydroperoxides have been shown to stimulate platelet aggregation [15, 16]. Moreover, in vitro oxidized LDL [17, 18] and LDL from patients with type 1 [19] or type 2 diabetes [20] activate platelets via an increase of p38 MAPK phosphorylation and thromboxane B2 (TxB2) formation. To date, no data are available on the interaction between LDL from patients with MetS and platelets.
The objectives of the present study were 1) to measure different markers of oxidative stress in LDL from obese patients with MetS compared with LDL from type 2 diabetic patients or control volunteers and 2) to determine the effects of these LDL on platelets.
Methods
Patients and control volunteers
30 men (30–75-year-old) were recruited from the Department of Endocrinology and Metabolic Diseases (Hospices Civils de Lyon). Exclusion criteria were smoking, alcohol consumption > 2 alcohol units/day, vitamin supplementation and evidence of cardiovascular complications. Patients with a metabolic syndrome were selected according to the criteria of the American Heart Association (AHA) [21] and had to fulfill three or more of the following factors : waist circumference > 102 cm, triacylglycerols (TG) > 1.7 mmol/l, HDL cholesterol < 1 mmol/l, blood pressure > 130/85 mmHg and fasting plasma glucose > 5.6 mmol/l. Type 2 diabetic patients should present a percentage of HbA1C greater than 7% and an associated MetS. Patients treated by glitazone drugs were excluded and lipid-lowering drugs were suspended for at least 7 days before venipuncture. Control volunteers were in good health as assessed by medical history and had all above indices in the expected normal range. All volunteers gave written informed consent. The study protocol, registered in ClinicalTrials.gov as NCT00932087, was approved by the Local Ethics Committee (CCP Sud Est IV Hospices Civils de Lyon) and was in accordance with the principles of Helsinki declaration. With a statistical significance of P<0.05 and 90% power, a minimum of eight volunteers per group was required to detect a 50% difference in the concentration of MDA in LDL.
Blood collection
Venous blood was collected on EDTA. Plasma was immediately separated by centrifugation at 1,500g for 10 min. and was frozen at −80°C under nitrogen in the presence of 10 μmol/l butylhydroxytolune (BHT).
Plasma sPLA2 activity
Plasma secretory phospholipase A2 (sPLA2) activity was measured with a selective fluorescent substrate (Aterovax, Paris, France). Results are expressed in unit per ml of sample (U/ml), with one unit defined as the amount of sPLA2 enzyme which catalyses the release of one nmol of product in one min. The average intra-assay coefficient of variation (CV) for individual human plasma samples was 8.46% and the average inter-assay CV was 5.24%. The minimal detectable activity level was 10 U/ml.
LDL isolation
LDL (1.019–1.063 g/ml) were isolated from plasma by potassium bromide stepwise ultracentrifugation [22]. LDL preparations were extensively dialyzed against PBS containing 1 mmol/l EDTA. LDL used for their interactions with platelets were finally dialyzed against EDTA-free PBS. The concentration of proteins was estimated using a Bradford assay [23]. Enzymatic determinations of total cholesterol and TG were processed using commercial kits (Biomérieux, Marcy l’Etoile, France). Plasma high sensitive C-reactive protein (HS CRP) was measured by nephelometry. LDL particle diameters were determined by electrophoresis of plasma in non denaturating polyacrylamide gradient gels (Lara-Spiral SA, Couternon, France).
Fatty acid compositions of lipid classes
Following the addition of internal standards and extraction with ethanol:chloroform (1:2, v/v) in the presence of BHT (50 μmol/l), lipid classes were separated by thin-layer chromatography (TLC). Chloroform/methanol (80:8, v/v) was used to separate neutral lipids from phospholipids, and chloroform/methanol/water (63:27:4, by vol.) to separate phosphatidylcholines (PC), phosphatidylethanolamines (PE) and sphingomyelins. Neutral lipids were separated in TG and cholesteryl esters (CE) using hexane/diethylether/acetic acid (80:20:1, by vol.). The different spots were scrapped off, treated with trifluoride boron/methanol (1:1, v/v) for 90 min at 100°C. The derivatized fatty acid methyl esters and fatty dimethylacetals were extracted twice with isooctane and separated by gas chromatography using an HP 6890 gas chromatograph equipped with a SP 2380 capillary column (0.25μm, 30m × 0.25mm, Supelco, Bellefonte, PA, USA) and a flame ionization detector (FID). The respective concentrations of fatty acids, quantified according to the amount of appropriate internal standard, were used to calculate the concentrations of lipid classes.
Quantification of total monohydroxylated fatty acids
Following lipid extraction, dried extracts were hydrolyzed with 10 mol/l KOH for 20 min at 60°C [24]. Non esterified hydroxylated fatty acids and fatty acids were first separated on an Oasis Sep-Pak cartridge column (Waters, Milford, MA) [3]. Non esterified hydroxylated fatty acids were then separated by TLC with hexane/diethylether/acetic acid (60:40:1, by vol.), extracted with methanol, separated by reversed-phase HPLC (RP-HPLC) on X Bridge C18 column (3.5 μm, 4.6 × 150 mm, Waters, Milford, MA) using a gradient solvent of acetonitrile and water (pH 3) and detected at 235 nm (for details, see a profile presented as electronic supplementary material [ESM Fig. 1]).
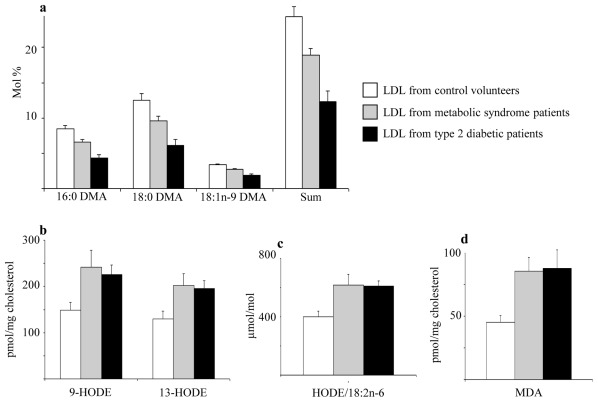
Fig. 1.
Indices of lipid peroxidation in LDL from control volunteers, obese patients with MetS or type 2 diabetes: fatty dimethylacetals (DMA) derived from PE plasmalogens (a), 9- and 13-HODE (b), HODE/18:2n-6 ratio (c) and MDA (d). Data are means ± SEM (n= 7 to 10 subjects per group). LDL from MetS patients vs LDL from control volunteers : significantly different (p < 0.05) for 16:0 DMA, 18:0 DMA, DMA sum, 9-HODE, 13-HODE, HODE/18:2 n-6 and (p < 0.01) for MDA. LDL from type 2 diabetic patients vs LDL from control volunteers : significantly different (p < 0.01) for 16:0 DMA, 18:0 DMA, 18:1 n-9 DMA, DMA sum and MDA ; significantly different (p < 0.05) for 9-HODE, 13-HODE and HODE/18:2 n-6. LDL from type 2 diabetic patients vs LDL from MetS patients : significantly different (p < 0.05) for 16:0 DMA, 18:0 DMA, 18:1 n-9 DMA and DMA sum. p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test. HODE, hydroxy-octadecadienoic acid; MDA, malondialdehyde; DMA, dimethylacetals; PE, phosphatidylethanolamine.
Malondialdehyde (MDA) determination
LDL samples were mixed with thiobarbituric acid (TBA) (10 mmol/l), acetic acid and BHT (5 mmol/l) and incubated at 95°C for 60 min [25]. The TBA-MDA adducts were extracted with ethyl acetate, separated onto a Nucleosil C18 column (5μm, 4.6 × 250 mm) and detected fluorimetrically (excitation 515 nm, emission 553 nm).
Vitamin E determination
LDL samples, containing tocol as an internal standard, were extracted twice with hexane (4 vol.) following the addition of ethanol (1 vol.) [20]. Tocopherol isomers were separated by RP-HPLC onto a Nucleosil C18 column (5μm, 4 × 150 mm) and detected fluorimetrically (excitation 295nm, emission 340nm).
Platelet isolation and incubation with LDL
Blood was collected at the blood bank from healthy volunteers who had not ingested any aspirin or other nonsteroidal antiinflammatory drugs in the previous 10 days. Platelets were isolated [26] and incubated in the presence or absence of LDL (1 mg/ml) for 2 h at 37°C.
Platelet p38 MAPK and cPLA2 activation
Following platelet lysis, proteins (30 μg) were denatured, electrophoresed in 12% Bis-Tris gels (Bio-Rad Laboratories, Marnes-la-Coquette, France) and transferred to nitrocellulose membranes. The membranes were incubated with either 1:5000 anti-p38 MAPK or antiphospho-p38 MAPK or anti-phospho-cytosolic phospholipase A2 (cPLA2) polyclonal antibodies (Cell Signaling Technologies, Beverly, MA), washed, and incubated with 1:10000 goat anti-rabbit horseradish peroxidase conjugate. p38 MAPK, phospho-p38 mitogen-activated protein kinase (MAPK) and phospho-cPLA2 were visualized by enhanced chemiluminescence, and bands were quantified by densitometry (Amersham Biosciences, Buckinghamshire, UK).
TxB2 measurement
Platelet TxB2 was quantified by competitive enzyme immunoassay (Amersham Biosciences, Buckinghamshire, UK).
Platelet aggregation
Aggregation was measured in isolated platelets in a Chrono-log dual-channel aggregometer (Coulter, Margency, France) according to the method of Born [27]. Platelet suspensions were pre-incubated for 5 min at 37°C in the presence or absence of LDL (0.1 mg/ml) and stimulated with subthreshold concentrations of collagen (75 ± 9 ng/ml) with continuous stirring at 1000 rpm. The subthreshold concentration of collagen was defined as the highest concentration of collagen that induced less than 15% increase in light transmission. The extent of platelet aggregation was expressed in terms of percentage of change in light transmission 4 min after the addition of collagen.
Statistical analysis
Results are expressed as the mean ± S.E.M. Comparisons between groups were performed using ANOVA followed by Fisher’s PLSD post hoc test. Correlation coefficients were determined using linear regression analysis.
Results
Clinical characteristics of obese patients with MetS or diabetes and control volunteers
The clinical and metabolic characteristics of the volunteers are summarized in Table 1. Patients with MetS fulfilled the criteria of the AHA [21]. They were either overweight or obese, had abdominal obesity, mild hypertriglyceridemia with low HDL cholesterol and were hypertensive. 2/10 MetS patients were treated against hypertension whereas 4/10 type 2 diabetic patients took anti-hypertensive medications, which could explain why the mean systolic and diastolic blood pressures were higher in the MetS group compared to the type 2 diabetic group. In addition, MetS patients showed elevated fasting insulin concentrations and a tendency to increased HOMA index, suggesting insulin resistance. Levels of HS CRP, a circulating marker of systemic inflammation, were increased similarly in MetS and type 2 diabetic patients. Type 2 diabetic patients were poorly controlled and presented a metabolic syndrome. LDL cholesterol levels were lower in patients with MetS or type 2 diabetes compared with control volunteers while plasma TG levels were higher. Healthy control volunteers had all above indices in the expected normal range.
Table 1.
Clinical and metabolic characteristics of control volunteers and obese patients with MetS or type 2 diabetes.
| Control | Metabolic Syndrome | Type 2 diabetes | |
|---|---|---|---|
| n (sex) | 10 (M) | 10 (M) | 10 (M) |
| Age (years) | 50 ± 3 | 58 ± 2* | 57 ± 3 |
| BMI (kg/m2) | 24.3 ± 0.7 | 30.7 ± 1.4* | 30.8 ± 1.1** |
| Waist circumference (cm) | 92 ± 2 | 111 ± 3** | 116 ± 7** |
| Fasting glucose (mmol/l) | 5.5 ± 0.2 | 5.6 ± 0.1 | 9.0 ± 1.0**† |
| Fasting insulin (pmol/l) | 41.1 ± 6.9 | 68.4 ± 12.7* | 45.4 ± 12 |
| HOMA index | 1.54 ± 0.29 | 2.53 ± 0.52 | 2.75 ± 0.92 |
| CRP (mg/l) | 0.54 ± 0.12 | 3.61 ± 0.82* | 4.82 ± 1.52** |
| HbA1c (%) | 5.4 ± 0.1 | 5.7 ± 0.1 | 10.4 ± 0.9**† |
| HbA1c (mmol/mol) | 35.5 ± 0.6 | 38.5 ± 1.4 | 90.2 ± 9.8**† |
| Systolic blood pressure (mmHg) | 121 ± 3 | 144 ± 3** | 132 ± 6*† |
| Diastolic blood pressure (mmHg) | 78 ± 4 | 88 ± 5* | 77 ± 3 † |
| Total cholesterol (mmol/l) | 6.0 ± 0.4 | 5.2 ± 0.3 | 4.8 ± 0.4* |
| HDL-cholesterol (mmol/l) | 1.4 ± 0.1 | 1.1 ± 0.1** | 0.9 ± 0.1** |
| Total cholesterol/HDL-cholesterol | 4.5 ± 0.3 | 4.9 ± 0.3 | 5.3 ± 0.3* |
| LDL-cholesterol (mmol/l) | 4.1 ± 0.4 | 3.2 ± 0.2 | 2.7 ± 0.4** |
| VLDL-cholesterol (mmol/l) | 0.5 ± 0.1 | 0.8 ± 0.1** | 1.0 ± 0.1**† |
| Triacylglycerols (mmol/l) | 1.3 ± 0.1 | 2.2 ± 0.3** | 2.6 ± 0.2** |
| Antidiabetic treatment (%) | 0 | 0 | 80 |
| Antihypertensive treatment (%) | 0 | 20 | 40 |
| Hypolipidemic treatment (%) | 0 | 10 | 20 |
Data are means ± SEM (n= 8 to 10 subjects per group).
p <0.05 and
p < 0.01 vs LDL from control volunteers.
p <0.05 vs LDL from MetS patients.
p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test.
M, male; HOMA, HOmeostasis Model Assessment index calculated (fasting insulin × fasting glucose)/22.5; Hypolipidemic treatment was interrupted seven days before inclusion.
The sPLA2 activity was significantly increased in plasma from patients with MetS or type 2 diabetes (45.7 ± 4.3 and 51.9 ± 5.1U/ml, respectively) compared with plasma from healthy volunteers (34.4 ± 2.5 U/ml). sPLA2 activity showed positive correlations with waist circumference (r2 = 0.41, p < 0.001) and MDA concentrations in LDL (0.14, p < 0.05) and negative correlation with plasmalogen proportions (r2 = 0.15, p < 0.05).
Lipid and fatty acid compositions of LDL from obese patients with MetS or diabetes compared with LDL from control volunteers
As shown in Table 2, the concentrations of CE were lower in LDL from patients (−13% in MetS patients and −20% in type 2 diabetic patients) compared with LDL from control volunteers. By contrast, the concentrations of TG were higher in LDL from MetS (+50%) and type 2 diabetic patients (+72%). No differences in glycerophospholipid concentrations (both PC and PE) were observed between control and patients’ groups. LDL particle sizes were significantly lower in patients with MetS or type 2 diabetes compared with control volunteers. The fatty acid composition of CE and PC differed between patients and control volunteers (Table 3). The proportions of PUFA decreased in CE from MetS patients while saturated fatty acids (SFA) and monounsaturated fatty acids (MUFA) proportions increased. In particular, the proportion of linoleic acid (18:2 n-6), the main PUFA, decreased in CE and PC from MetS patients. Although palmitoleic acid (16:1 n-7) represents a minor fatty acid, its proportion increased by 70% in CE. Concerning LDL from type 2 diabetic patients, PUFA proportions decreased while those of SFA increased and MUFA were unchanged. In particular, the proportions of linoleic acid decreased while those of arachidonic acid (20:4 n-6) increased in CE and PC.
Table 2.
Lipid classes and particle size of LDL from control volunteers and obese patients with MetS or type 2 diabetes.
| Control | Metabolic Syndrome | Type 2 diabetes | |
|---|---|---|---|
| Cholesteryl esters (nmol/mg protein) | 2459 ± 118 | 2132 ± 61** | 1975 ± 88** |
| Phosphatidylcholines (nmol/mg protein) | 521 ± 17 | 477 ± 18 | 479 ± 21 |
| Phosphatidylethanolamines (nmol/mg prot.) | 17 ± 2 | 15 ± 1 | 18 ± 1 |
| Triacylglycerols (nmol/mg protein) | 140 ± 11 | 210 ± 19* | 241 ± 37** |
| LDL particle size (nm) | 25.1 ± 0.2 | 24.4 ± 0.2 * | 24.4 ± 0.1 * |
Data are means ± SEM (n=8 to 10 subjects per group).
p <0.05 and
p < 0.01 vs LDL from control volunteers.
p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test.
Table 3.
Main fatty acid compositions of cholesteryl esters and phosphatidylcholines in LDL from control volunteers and obese patients with MetS or type 2 diabetes.
| Fatty acid (mol%) | Control | Cholesteryl esters Metabolic syndrome | Type 2 diabetes | Control | Phosphatidylcholines Metabolic syndrome | Type 2 diabetes |
|---|---|---|---|---|---|---|
| 16:0 | 12.4 ± 0.4 | 13.5 ± 0.4* | 13.7 ± 0.3* | 33.5 ± 0.7 | 34.7 ± 0.4 | 34.3 ± 0.5 |
| 16:1n-7 | 2.5 ± 0.3 | 4.2 ± 0.3** | 2.8 ± 0.3 | 0.3 ± 0.1 | 0.5 ± 0.1 | 0.3 ± 0.1 |
| 16:1n-9 | 0.3 ± 0.1 | 0.4 ± 0.1 | 0.5 ± 0.1 | 0 | 0 | 0 |
| 18:0 | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 16.0 ± 0.5 | 15.8 ± 0.7 | 15.3 ± 0.7 |
| 18:1n-7 | 1.0 ± 0.2 | 0.7 ± 0.2 | 1.0 ± 0.2 | 1.3 ± 0.3 | 1.0 ± 0.2 | 1.2 ± 0.3 |
| 18:1n-9 | 20.6 ± 0.7 | 21.7 ± 0.7 | 22.1 ± 0.7 | 10.9 ± 0.5 | 10.9 ± 0.5 | 11.6 ± 0.3 |
| 18:2n-6 | 52.0 ± 1.2 | 46.7 ± 1.4** | 46.7 ± 1.1** | 21.8 ± 1.0 | 19.2 ± 0.7* | 19.6 ± 0.7* |
| 18:3n-3 | 0.4 ± 0.1 | 0.7 ± 0.0 | 0.5 ± 0.1 | 0 | 0 | 0 |
| 18:3n-6 | 0.8 ± 0.1 | 1.1 ± 0.1 | 0.8 ± 0.2 | 0 | 0 | 0 |
| 20:3n-6 | 0.8 ± 0.0 | 0.9 ± 0.1 | 0.9 ± 0.1 | 3.1 ± 0.2 | 3.7 ± 0.3* | 3.3 ± 0.2 |
| 20:4n-6 | 6.2 ± 0.4 | 7.0 ± 0.6 | 8.3 ± 0.5**† | 7.2 ± 0.6 | 8.8 ± 0.7 | 9.3 ± 0.5* |
| 20:5n-3 | 1.3 ± 0.2 | 1.3 ± 0.2 | 1.0 ± 0.2 | 1.1 ± 0.3 | 1.1 ± 0.1 | 0.9 ± 0.2 |
| 22:5n-3 | 0 | 0 | 0 | 0.4 ± 0.2 | 0.4 ± 0.2 | 0.4 ± 0.1 |
| 22:6n-3 | 0.7 ± 0.1 | 0.6 ± 0.1 | 0.6 ± 0.1 | 3.2 ± 0.4 | 2.6 ± 0.3 | 2.9 ± 0.2 |
| SFA | 13.5 ± 0.5 | 14.7 ± 0.4* | 14.7 ± 0.3* | 50.0 ± 0.9 | 50.9 ± 0.7 | 49.9 ± 0.6 |
| MUFA | 24.4 ± 0.8 | 27.1 ± 1.0* | 26.4 ± 0.5 | 12.9 ± 0.6 | 13.0 ± 0.6 | 13.4 ± 0.4 |
| PUFA | 62.1 ± 1.1 | 58.3 ± 1.2* | 59.0 ± 0.7* | 37.1 ± 0.9 | 36.1 ± 0.8 | 36.7 ± 0.5 |
Data are means ± SEM (n= 8 to 9 subjects per group).
p <0.05 and
p < 0.01 vs LDL from control volunteers.
p < 0.05 vs LDL from MetS patients.
p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test. SFA, saturated fatty acids; MUFA, monounsaturated fatty acids; PUFA, polyunsaturated fatty acids.
Special care was taken to measure ethanolamine plasmalogens (or alkenyl, acyl-glycerophosphoethanolamines). They are a glycerophospholipid subclass with a 16:0, 18:0 or 18:1 fatty chain attached at the sn-1 position via a vinyl ether bond, and are more susceptible to oxidation [28]. As shown in Fig. 1a, the proportions of 16:0 DMA (dimethyl acetal issued from the alkenyl residue) and 18:0 DMA were decreased by 22% and 23%, respectively in LDL from MetS patients compared with control LDL. In LDL from type 2 diabetic patients, 16:0, 18:0 and 18:1 DMA species were decreased by 47%, 50% and 42%, respectively. Altogether, the sum of DMA species, representative of plasmalogens, was decreased by 22% and 49%, respectively in LDL from patients with MetS or type 2 diabetes. Interestingly, ethanolamine plasmalogen proportions were negatively correlated with waist circumference (r2 = 0.22, p < 0.01).
Lipid peroxides and antioxidant contents of LDL from obese patients with MetS or diabetes compared with LDL from control volunteers
The concentrations of total (both free and esterified) hydroxylated fatty acids, the stable primary products of lipid peroxidation, were determined in LDL from patients and control groups. They mainly consisted of hydroxy-octadecadienoic acids (HODE) derived from linoleic acid and hydroxy-eicosatetraenoic acids (HETE) derived from arachidonic acid. 9-HODE and 13-HODE concentrations increased by 62 and 55% respectively in LDL from MetS patients and increased by 52 and 50% in LDL from type 2 diabetic patients (Fig. 1b). Additionally, the ratio of total HODE to linoleic acid increased by 54% and 52% respectively in LDL from MetS and type 2 diabetic patients (Fig. 1c). Among HETE, 8-, 11-, 12- and 15-HETE were detected in LDL from each volunteer. There were no significant differences in the concentrations of HETE between MetS patients and control volunteers (data not shown). Only 15-HETE isomer concentration was significantly increased by 82% in LDL from type 2 diabetic patients compared with LDL from control volunteers (50.8 ± 7.6 pmol/mg cholesterol vs 28.0 ± 4.3 pmol/mg cholesterol, p <0.05). The concentrations of MDA, issued from the degradation of fatty acid hydroperoxides, were significantly increased by 2-fold in patients with MetS or type 2 diabetes (Fig. 1d). The waist circumference was mildly correlated with TG and MDA levels in LDL (r2 = 0.13 and 0.25, respectively, p < 0.05) (see [ESM] Fig. 2a and b).
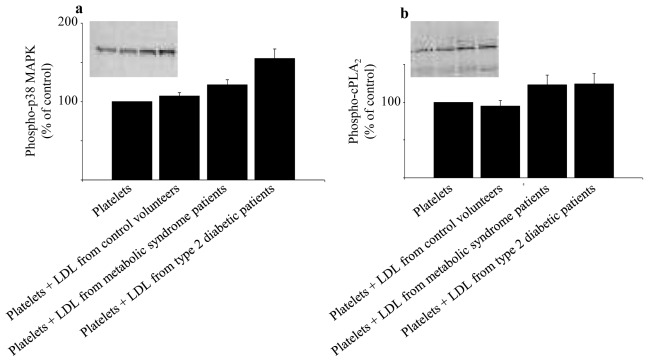
Fig. 2.
Effects of LDL from control volunteers, obese patients with MetS or type 2 diabetes on the phosphorylation of p38 MAPK (a) and cPLA2 (b) in platelets. Platelets from blood donors were incubated for 2h at 37°C in the absence or presence of LDL (1 mg protein/ml) from either control volunteers, MetS patients or type 2 diabetic patients. Representative immunoblots and histograms of the normalized amount of phosphorylation of p38 MAPK and cPLA2 are shown. Data are means ± SEM (7 to 8 subjects per group). Platelets + LDL from MetS patients vs platelets incubated with buffer : significantly different (p < 0.05) for phospho-p38 MAPK and phospho-cPLA2. Platelets + LDL from type 2 diabetic patients vs platelets incubated with buffer : significantly different for phospho-p38 MAPK (p < 0.01) and phospho-cPLA2 (p < 0.05). Platelets + LDL from type 2 diabetic patients vs platelets + LDL from MetS patients : significantly different for phospho-p38 MAPK (p < 0.05). p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test. MAPK, mitogen activated protein kinase; cPLA2, cytosolic phospholipase A2.
The concentrations of vitamin E, the main liposoluble antioxidant, were determined in LDL. α-tocopherol concentrations did not differ between patients with MetS or type 2 diabetes (6.7 ± 0. 5 and 6.0 ± 0. 3 nmol/mg protein) vs control volunteers (5.9 ± 0. 3 nmol/mg protein). γ-tocopherol, representing 10% of α-tocopherol, was increased in LDL from MetS patients (0.9 ± 0.1 nmol/mg protein) compared with control LDL (0.6 ± 0.1 nmol/mg protein) but did not differ in LDL from type 2 diabetic patients (0.7 ± 0.1 nmol/mg protein).
Effects of LDL isolated from obese patients with MetS or diabetes, or control volunteers on platelet arachidonic acid signaling cascade
To determine the effects of LDL on platelet arachidonic acid cascade, platelets from healthy donors were incubated in the absence or presence of LDL from patients or control volunteers (1 mg/ml) for 2 hours at 37°C. Phosphorylated amounts of p38 MAPK and cPLA2, key enzymes involved in the release of arachidonic acid from membrane phospholipids, as well as concentrations of TxB2, the stable catabolite of the pro-aggregatory arachidonic acid metabolite thromboxane A2 (TxA2), were determined. As shown in Fig. 2, the addition of LDL from control volunteers to platelets had no effects on p38 MAPK and cPLA2 phosphorylations, compared with platelets alone. By contrast, the addition of LDL from patients with MetS or type 2 diabetes significantly increased p38 MAPK phosphorylation, by 21% and 55% respectively, and cPLA2 phosphorylation by 23 and 24%. Compared with control platelets, the incubation of platelets with LDL from patients with MetS or type 2 diabetes resulted in a 2-fold increased basal concentration of TxB2 whereas LDL from control volunteers had no effects (Fig. 3). Platelet TxB2 was negatively correlated with plasmalogen proportions (r2 = 0.44) and positively with HODE and MDA concentrations in LDL (r2 = 0.24 and 0.31, respectively, p < 0.01) (see [ESM] Fig. 2c and d).
Fig. 3.
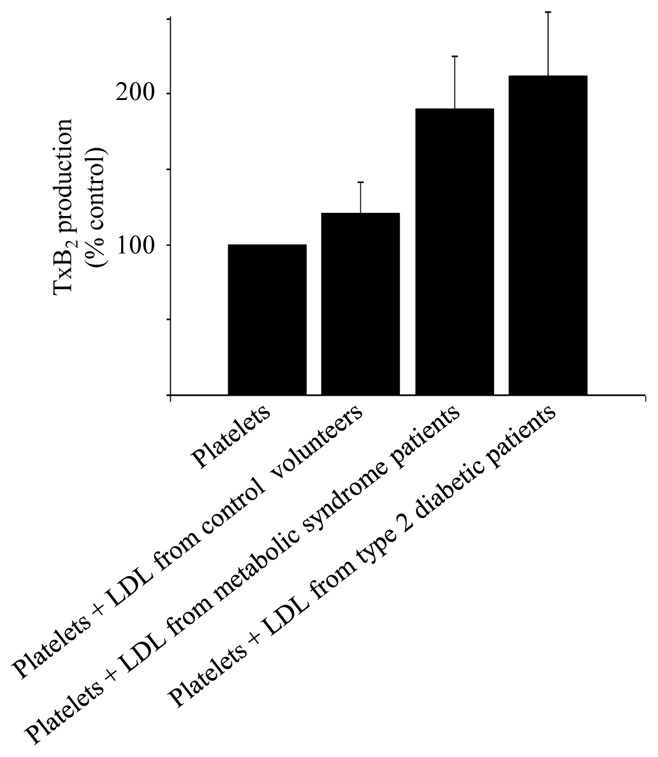
Effects of LDL from control volunteers, obese patients with MetS or type 2 diabetes on thromboxane B2 concentrations in unstimulated platelets. Platelets from blood donors were incubated for 2h at 37°C in the absence or presence of LDL (1 mg protein/ml) from either control subjects, MetS patients or type 2 diabetic patients. Data, expressed as percent of control, are means ± SEM (10 subjects per group). Thromboxane B2 concentrations in control unstimulated platelets were 187 ± 37 pmol/109 platelets. Platelets + LDL from type 2 diabetic patients vs platelets incubated with buffer, and Platelets + LDL from MetS patients vs platelets incubated with buffer : significantly different (p < 0.05). p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test.
Effect of LDL isolated from obese patients with MetS or diabetes, or control volunteers, on platelet aggregation
To determine the effect of LDL on platelet aggregation, platelets were preincubated for 5 min. with low concentrations of LDL (0.1 mg/ml) and then stimulated with sub-threshold concentrations of collagen for another 4 min. As shown in Fig. 4, there was no effect of LDL from control volunteers on collagen-induced platelet aggregation, compared with platelets incubated with buffer. By contrast, pre-incubation of platelets with LDL from MetS or type 2 diabetic patients resulted in a stimulation of platelet aggregation in response to subthreshold concentrations of collagen (+197% and +251%, respectively). Platelet aggregation was also potentiated by lower concentrations (50 μg/ml) of LDL from type 2 diabetic patients (data not shown).
Fig. 4.
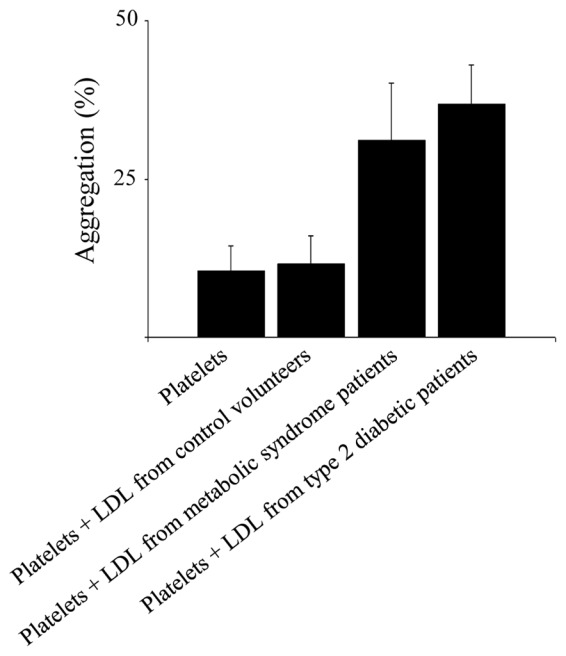
Effects of LDL from control subjects, obese patients with MetS or type 2 diabetes on the aggregation of platelets induced by collagen. Platelets from blood donors were preincubated for 5 min at 37°C in the absence or presence of LDL (0.1 mg protein/ml) from either control subjects, MetS patients or type 2 diabetic patients and stimulated with subthreshold concentrations of collagen (75 ± 9 ng/mL). Data, expressed as percent of aggregation, are means ± SEM of 5 subjects per group. Platelets + LDL from MetS patients vs platelets incubated with buffer : significantly different (p < 0.05). Platelets + LDL from type 2 diabetic patients vs platelets incubated with buffer : significantly different (p < 0.01). p values were obtained by ANOVA followed by Fisher’s PLSD post hoc test.
Discussion
The evidence for increased oxidative stress in MetS is still a matter of debate. In the present study, we provide several lines of evidence for increased oxidative stress in LDL from obese MetS patients, as assessed by different complementary indices of oxidative stress and special focus on oxidation products of linoleic acid, the most abundant PUFA in LDL. Higher concentrations of total HODE and lower proportions of linoleic acid in PC and CE were found in LDL from MetS patients compared with control LDL. Interestingly, HODE and linoleic acid levels were modified to the same extent in LDL from type 2 diabetic patients.
Conversely, there were no changes in total HETE concentrations in MetS patients, which is in agreement with a recent study showing no differences in the levels of oxidation products of arachidonic acid (total HETE and F2-isoprostanes) in individuals with features of MetS [9]. This suggests that oxidation products of linoleic acid could be better markers of lipid peroxidation than those of arachidonic acid. It should be mentioned that there was no dietary record in participants. Although we are not aware of any supplementation study reporting a concomitant decrease of linoleic acid and increase of arachidonic acid in plasma or LDL, we cannot exclude a potential effect of fat intake on plasma fatty acid composition.
The presence of an oxidative stress in LDL from MetS patients was confirmed with the decreased concentrations of plasmalogens in LDL from MetS patients (−22%) as well as in LDL from type 2 diabetic patients (−49%), compared with control LDL. This result indicates that plasmalogens may be targets and markers of ongoing oxidative stress and corroborates previous data showing a 20% decrease of plasmalogen PE in red blood cell membranes from hyperlipidemic patients [29]. In addition, we found that MDA, a commonly used overall marker of lipid peroxidation, described to correlate with total isoprostanes in plasma and tissues [30, 31], was increased to a similar extent in LDL from MetS and type 2 diabetic patients, in agreement with enhanced serum levels of TBARS in type 2 diabetic patients [32]. Although isoprostanes are recognized as reliable markers of oxidative stress in vivo, they derive exclusively from the free radical-induced peroxidation of arachidonic acid and their levels were either reported to be increased [9, 32] or unchanged [7] in patients with MetS. Altogether, the increase of several complementary indices of oxidative stress and especially of oxidized products of linoleic acid in LDL from MetS patients gives support to the hypothesis that the MetS is associated with higher levels of circulating oxidized LDL [4–6]. In addition, compared with control LDL, LDL from patients with MetS showed higher TG and lower CE levels as well as decreased particle size, suggesting a higher percentage of smaller and denser LDL particles. Therefore, our data corroborate that the MetS is associated with small and dense LDL particles [5, 33, 34], which are known to be more susceptible to oxidative modification [35].
Regarding the main antioxidant in LDL, we found similar concentrations of α-tocopherol in patients with MetS or type 2 diabetes and higher concentrations of γ-tocopherol in MetS patients. There have been discordant reports about vitamin E levels in patients with MetS or type 2 diabetes, showing either lower vitamin E concentrations in volunteers with a MetS that also consumed fewer fruits and vegetables [36] or no difference among volunteers with MetS or type 2 diabetes [37, 38]. Only one study to our knowledge reported slightly higher serum γ-tocopherol levels [38] and no changes of α-tocopherol among subjects with MetS. Our results obtained ex vivo suggest that tocopherols may have been spared by molecules (such as plasmalogens) serving as primary targets of free radicals during LDL oxidation [39].
It is worth noting that oxidative stress was enhanced to a similar extent in LDL from MetS patients as in LDL from type 2 diabetic patients, suggesting that factors associated with the MetS rather than poor glycemic control are key factors associated with oxidative modification of LDL. In agreement with this statement, our results show correlations between waist circumference and plasmalogens or MDA in LDL, suggesting an association between an excess of visceral fat and biochemical parameters associated with oxidative stress in LDL. It is also likely that obesity tightly associated with MetS may represent a major factor in the oxidative stress evidenced in LDL from obese MetS patients.
Besides, our results show that the activity of sPLA2 is correlated with plasmalogens and MDA in LDL, suggesting that this enzyme catalyzes the hydrolysis of oxidized phospholipids in LDL [40]. The correlation between the activity of sPLA2 and the waist circumference is in line with the association of sPLA2 with MetS [41].
Regarding the functionality of LDL from patients with MetS, we show for the first time that LDL from MetS patients activate platelets and prime collagen-induced platelet aggregation. The activation occurs through an increased phosphorylation of p38 MAPK, the stress kinase responsible for the phosphorylation of cytosolic phospholipase A2 [42], the key enzyme involved in the release of arachidonic acid from membrane phospholipids [43]. It resulted in an increased formation of TxA2, as assessed by the increased concentration of the stable catabolite, TxB2. We confirm that LDL isolated from type 2 diabetic patients activate platelets through the arachidonic acid cascade [20] and give new evidence for a priming effect of LDL on platelet aggregation, whereas LDL from control volunteers have no activating effects. Regarding the molecules in patients’ LDL responsible for platelet activation, our data suggest the implication of lipid peroxides. LDL from patients with either obese MetS or type 2 diabetic patients showed similar increased levels of lipid peroxides and activated platelets to the same extent. In addition, correlation analyses show that platelet TxB2 concentration is related to the concentrations of HODE and MDA in LDL, suggesting that lipid peroxides could underlie the activating effects of LDL on platelets and that glycation is not necessarily required. It is also important to take into account obesity in future studies to identify the mechanism by which oxidized LDL activate platelets.
Besides, our results obtained ex vivo strengthen the implication of fatty acid peroxides in platelet activation as previously demonstrated in in vitro studies [15, 44]. We have indeed shown that fatty acid hydroperoxides, precursors of HETE and HODE, potentiated platelet aggregation and activated platelets via the arachidonic acid signaling cascade [16]. More recently, the Podrez group showed that oxidized choline glycerophospholipids induce platelet aggregation via CD36 [45].
Altogether, our results support that 1) oxidative stress is increased in LDL from obese MetS patients, with or without type 2 diabetes and that 2) in vivo oxidatively modified LDL from MetS patients activate control platelets to the same extent than LDL from type 2 diabetic patients. Considering that MetS often precedes the occurrence of diabetes [46], and that cardiovascular complications occur frequently at the onset of type 2 diabetes, our data support the hypothesis that oxidative stress in metabolic syndrome is an early promoter of prematured atherothombosis [47]. The identification of specific targets of oxidative stress in MetS such as linoleic acid-containing lipids might provide opportunities to selectively slow down some peculiar lipid peroxidation process in LDL at the stage of the MetS and to prevent associated platelet hyperactivation.
Acknowledgments
This study was supported by INSERM and ANR grant (ANR-05-COD-D019-01). RC was funded by the French Ministry of Education and Research. CC is supported by the CNRS. The authors gratefully thank Pr. Ziad Mallat and Aterovax (Paris, France) for the analysis of sPLA2 activity.
The authors thank all participants, the nursing staff at Hospices Civils de Lyon for expert blood drawing assistance and Martine Broyer for particle size data analysis.
CC, RC, ML and PM conceived and designed the study. CCA, MM and PM recruited the patients. RC and AS acquired data. All authors interpreted data. CC wrote the manuscript and RC, ML and PM revised the manuscript. All authors approved the final version of the manuscript.
Abbreviations
- BHT
butylhydroxytoluene
- CE
cholesteryl esters
- cPLA2
cytosolic phospholipase A2
- DMA
dimethylacetal
- HDL
high-density lipoproteins
- HETE
hydroxy-eicosatetraenoic acid
- HODE
hydroxy-octadecadienoic acid
- HS CRP
high sensitivity C-reactive protein
- MAPK
mitogen-activated protein kinase
- MetS
metabolic syndrome
- MDA
malondialdehyde
- MUFA
monounsaturated fatty acids
- PC
phosphatidylcholine
- PE
phosphatidylethanolamine
- PL
phospholipids
- PUFA
polyunsaturated fatty acids
- SFA
saturated fatty acids
- sPLA2
secretory phospholipase A2
- TBA
thiobarbituric acid
- TBARS
thiobarbituric acid reactive species
- TG
triacylglycerols
- TLC
thin-layer chromatography
- TxA2
thromboxane A2
- TxB2
thromboxane B2
Footnotes
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
References
- 1.Stephens JW, Khanolkar MP, Bain SC. The biological relevance and measurement of plasma markers of oxidative stress in diabetes and cardiovascular disease. Atherosclerosis. 2009;202:321–329. doi: 10.1016/j.atherosclerosis.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Hsu RM, Devaraj S, Jialal I. Autoantibodies to oxidized low-density lipoprotein in patients with type 2 diabetes mellitus. Clin Chim Acta. 2002;317:145–150. doi: 10.1016/s0009-8981(01)00767-7. [DOI] [PubMed] [Google Scholar]
- 3.Colas R, Pruneta-Deloche V, Guichardant M, et al. Increased lipid peroxidation in LDL from type-2 diabetic patients. Lipids. 2010;45:723–731. doi: 10.1007/s11745-010-3453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holvoet P, Kritchevsky SB, Tracy RP, et al. The metabolic syndrome, circulating oxidized LDL, and risk of myocardial infarction in well-functioning elderly people in the health, aging, and body composition cohort. Diabetes. 2004;53:1068–1073. doi: 10.2337/diabetes.53.4.1068. [DOI] [PubMed] [Google Scholar]
- 5.Sigurdardottir V, Fagerberg B, Hulthe J. Circulating oxidized low-density lipoprotein (LDL) is associated with risk factors of the metabolic syndrome and LDL size in clinically healthy 58-year-old men (AIR study) J Intern Med. 2002;252:440–447. doi: 10.1046/j.1365-2796.2002.01054.x. [DOI] [PubMed] [Google Scholar]
- 6.Park SH, Kim JY, Lee JH, Park HY. Elevated oxidized low-density lipoprotein concentrations in postmenopausal women with the metabolic syndrome. Clin Chim Acta. 2011;412:435–440. doi: 10.1016/j.cca.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 7.Hansel B, Giral P, Nobecourt E, et al. Metabolic syndrome is associated with elevated oxidative stress and dysfunctional dense high-density lipoprotein particles displaying impaired antioxidative activity. J Clin Endocrinol Metab. 2004;89:4963–4971. doi: 10.1210/jc.2004-0305. [DOI] [PubMed] [Google Scholar]
- 8.Sjogren P, Basu S, Rosell M, et al. Measures of oxidized low-density lipoprotein and oxidative stress are not related and not elevated in otherwise healthy men with the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2005;25:2580–2586. doi: 10.1161/01.ATV.0000190675.08857.3d. [DOI] [PubMed] [Google Scholar]
- 9.Seet RC, Lee CY, Lim EC, et al. Markers of oxidative damage are not elevated in otherwise healthy individuals with the metabolic syndrome. Diabetes Care. 2010;33:1140–1142. doi: 10.2337/dc09-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 11.Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 12.Vericel E, Januel C, Carreras M, Moulin P, Lagarde M. Diabetic patients without vascular complications display enhanced basal platelet activation and decreased antioxidant status. Diabetes. 2004;53:1046–1051. doi: 10.2337/diabetes.53.4.1046. [DOI] [PubMed] [Google Scholar]
- 13.Vaduganathan M, Alviar CL, Arikan ME, et al. Platelet reactivity and response to aspirin in subjects with the metabolic syndrome. Am Heart J. 2008;156:1002 e1001–1002 e1007. doi: 10.1016/j.ahj.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Vaidya D, Yanek LR, Faraday N, Moy TF, Becker LC, Becker DM. Native platelet aggregation and response to aspirin in persons with the metabolic syndrome and its components. Metab Syndr Relat Disord. 2009;7:289–296. doi: 10.1089/met.2008.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calzada C, Vericel E, Mitel B, Coulon L, Lagarde M. 12(S)-Hydroperoxy-eicosatetraenoic acid increases arachidonic acid availability in collagen-primed platelets. J Lipid Res. 2001;42:1467–1473. [PubMed] [Google Scholar]
- 16.Coulon L, Calzada C, Moulin P, Vericel E, Lagarde M. Activation of p38 mitogen-activated protein kinase/cytosolic phospholipase A2 cascade in hydroperoxide-stressed platelets. Free Radic Biol Med. 2003;35:616–625. doi: 10.1016/s0891-5849(03)00386-1. [DOI] [PubMed] [Google Scholar]
- 17.Akkerman JW. From low-density lipoprotein to platelet activation. Int J Biochem Cell Biol. 2008;40:2374–2378. doi: 10.1016/j.biocel.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Ferretti G, Rabini RA, Bacchetti T, et al. Glycated low density lipoproteins modify platelet properties: a compositional and functional study. J Clin Endocrinol Metab. 2002;87:2180–2184. doi: 10.1210/jcem.87.5.8466. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe J, Wohltmann HJ, Klein RL, Colwell JA, Lopes-Virella MF. Enhancement of platelet aggregation by low-density lipoproteins from IDDM patients. Diabetes. 1988;37:1652–1657. doi: 10.2337/diab.37.12.1652. [DOI] [PubMed] [Google Scholar]
- 20.Calzada C, Coulon L, Halimi D, et al. In vitro glycoxidized low-density lipoproteins and low-density lipoproteins isolated from type 2 diabetic patients activate platelets via p38 mitogen-activated protein kinase. J Clin Endocrinol Metab. 2007;92:1961–1964. doi: 10.1210/jc.2006-2045. [DOI] [PubMed] [Google Scholar]
- 21.Grundy SM, Hansen B, Smith SC, Jr, Cleeman JI, Kahn RA. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation. 2004;109:551–556. doi: 10.1161/01.CIR.0000112379.88385.67. [DOI] [PubMed] [Google Scholar]
- 22.Havel RJ, Eder HA, Bragdon JH. The distribution and chemical composition of ultracentrifugally separated lipoproteins in human serum. J Clin Invest. 1955;34:1345–1353. doi: 10.1172/JCI103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1006/abio.1976.9999. [DOI] [PubMed] [Google Scholar]
- 24.Browne RW, Armstrong D. HPLC analysis of lipid-derived polyunsaturated fatty acid peroxidation products in oxidatively modified human plasma. Clin Chem. 2000;46:829–836. [PubMed] [Google Scholar]
- 25.Therasse J, Lemonnier F. Determination of plasma lipoperoxides by high-performance liquid chromatography. J Chromatogr. 1987;413:237–241. doi: 10.1016/0378-4347(87)80232-3. [DOI] [PubMed] [Google Scholar]
- 26.Lagarde M, Bryon PA, Guichardant M, Dechavanne M. A simple and efficient method for platelet isolation from their plasma. Thromb Res. 1980;17:581–588. doi: 10.1016/0049-3848(80)90098-5. [DOI] [PubMed] [Google Scholar]
- 27.Born GV. Aggregation of blood platelets by adenosine diphosphate and its reversal. Nature. 1962;194:927–929. doi: 10.1038/194927b0. [DOI] [PubMed] [Google Scholar]
- 28.Engelmann B, Brautigam C, Thiery J. Plasmalogen phospholipids as potential protectors against lipid peroxidation of low density lipoproteins. Biochem Biophys Res Commun. 1994;204:1235–1242. doi: 10.1006/bbrc.1994.2595. [DOI] [PubMed] [Google Scholar]
- 29.Engelmann B, Schonthier UM, Richter WO, Duhm J. Changes of membrane phospholipid composition of human erythrocytes in hyperlipidemias. II. Increases in distinct molecular species of phosphatidylethanolamine and phosphatidylcholine containing arachidonic acid. Biochim Biophys Acta. 1992;1165:38–44. doi: 10.1016/0005-2760(92)90073-5. [DOI] [PubMed] [Google Scholar]
- 30.Dreissigacker U, Suchy MT, Maassen N, Tsikas D. Human plasma concentrations of malondialdehyde (MDA) and the F2-isoprostane 15(S)-8-iso-PGF(2alpha) may be markedly compromised by hemolysis: evidence by GC-MS/MS and potential analytical and biological ramifications. Clin Biochem. 43:159–167. doi: 10.1016/j.clinbiochem.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Walsh SW, Vaughan JE, Wang Y, Roberts LJ., 2nd Placental isoprostane is significantly increased in preeclampsia. FASEB J. 2000;14:1289–1296. doi: 10.1096/fj.14.10.1289. [DOI] [PubMed] [Google Scholar]
- 32.Griesmacher A, Kindhauser M, Andert SE, et al. Enhanced serum levels of thiobarbituric-acid-reactive substances in diabetes mellitus. Am J Med. 1995;98:469–475. doi: 10.1016/s0002-9343(99)80347-7. [DOI] [PubMed] [Google Scholar]
- 33.Garin MC, Kalix B, Morabia A, James RW. Small, dense lipoprotein particles and reduced paraoxonase-1 in patients with the metabolic syndrome. J Clin Endocrinol Metab. 2005;90:2264–2269. doi: 10.1210/jc.2004-1295. [DOI] [PubMed] [Google Scholar]
- 34.Gentile M, Panico S, Jossa F, et al. Small dense LDL particles and metabolic syndrome in a sample of middle-aged women. Findings from Progetto Atena. Clin Chim Acta. 2008;388:179–183. doi: 10.1016/j.cca.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 35.Tribble DL, Holl LG, Wood PD, Krauss RM. Variations in oxidative susceptibility among six low density lipoprotein subfractions of differing density and particle size. Atherosclerosis. 1992;93:189–199. doi: 10.1016/0021-9150(92)90255-f. [DOI] [PubMed] [Google Scholar]
- 36.Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations: findings from the Third National Health and Nutrition Examination Survey. Diabetes. 2003;52:2346–2352. doi: 10.2337/diabetes.52.9.2346. [DOI] [PubMed] [Google Scholar]
- 37.Feillet-Coudray C, Rock E, Coudray C, et al. Lipid peroxidation and antioxidant status in experimental diabetes. Clin Chim Acta. 1999;284:31–43. doi: 10.1016/s0009-8981(99)00046-7. [DOI] [PubMed] [Google Scholar]
- 38.Ford ES. Intake and circulating concentrations of antioxidants in metabolic syndrome. Curr Atheroscler Rep. 2006;8:448–452. doi: 10.1007/s11883-006-0018-8. [DOI] [PubMed] [Google Scholar]
- 39.Hahnel D, Beyer K, Engelmann B. Inhibition of peroxyl radical-mediated lipid oxidation by plasmalogen phospholipids and alpha-tocopherol. Free Radic Biol Med. 1999;27:1087–1094. doi: 10.1016/s0891-5849(99)00142-2. [DOI] [PubMed] [Google Scholar]
- 40.Mallat Z, Lambeau G, Tedgui A. Lipoprotein-associated and secreted phospholipases A in cardiovascular disease: roles as biological effectors and biomarkers. Circulation. 2010;122:2183–2200. doi: 10.1161/CIRCULATIONAHA.110.936393. [DOI] [PubMed] [Google Scholar]
- 41.Mattsson N, Magnussen CG, Ronnemaa T, et al. Metabolic syndrome and carotid intima-media thickness in young adults: roles of apolipoprotein B, apolipoprotein A-I, C-reactive protein, and secretory phospholipase A2: the cardiovascular risk in young Finns study. Arterioscler Thromb Vasc Biol. 2010;30:1861–1866. doi: 10.1161/ATVBAHA.110.204669. [DOI] [PubMed] [Google Scholar]
- 42.Borsch-Haubold AG, Kramer RM, Watson SP. Phosphorylation and activation of cytosolic phospholipase A2 by 38-kDa mitogen-activated protein kinase in collagen-stimulated human platelets. Eur J Biochem. 1997;245:751–759. doi: 10.1111/j.1432-1033.1997.t01-1-00751.x. [DOI] [PubMed] [Google Scholar]
- 43.Kramer RM, Sharp JD. Structure, function and regulation of Ca2+-sensitive cytosolic phospholipase A2 (cPLA2) FEBS Lett. 1997;410:49–53. doi: 10.1016/s0014-5793(97)00322-0. [DOI] [PubMed] [Google Scholar]
- 44.Calzada C, Vericel E, Lagarde M. Low concentrations of lipid hydroperoxides prime human platelet aggregation specifically via cyclo-oxygenase activation. Biochem J. 1997;325 ( Pt 2):495–500. doi: 10.1042/bj3250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Podrez EA, Byzova TV, Febbraio M, et al. Platelet CD36 links hyperlipidemia, oxidant stress and a prothrombotic phenotype. Nat Med. 2007;13:1086–1095. doi: 10.1038/nm1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sattar N, Gaw A, Scherbakova O, et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003;108:414–419. doi: 10.1161/01.CIR.0000080897.52664.94. [DOI] [PubMed] [Google Scholar]
- 47.Wiernsperger NF. Oxidative stress as a therapeutic target in diabetes: revisiting the controversy. Diabetes Metab. 2003;29:579–585. doi: 10.1016/s1262-3636(07)70072-1. [DOI] [PubMed] [Google Scholar]