Abstract
Health promotion practice research conducted by or in partnership with community-based organizations (CBOs) serving Asian Americans, Native Hawaiians, and Pacific Islanders (AA and NHPI) can address health disparities. Few CBOs have the tools to integrate or initiate research into their programmatic agenda. The New York University (NYU) Center for the Study of Asian American Health (CSAAH) and the Asian & Pacific Islander American Health Forum (APIAHF) created a partnership with the goal to support CBO research infrastructure development by creating the Community Empowered Research Training (CERT) program.
Methods
A survey was conducted and discussions held with CBO leaders representing AA and NHPI communities to inform the development of the CERT program.
Results
The majority of participants are engaged in service-related research and reported interest in building their research capacity. CBOs may require help reframing how data can be collected and used to better inform programmatic activities and to address health disparities facing AA and NHPI communities.
Conclusions
CBOs possess both an interest in and access to local knowledge that can inform health priorities. Findings have been applied to the CERT program to build capacity to support community-initiated/driven research to address health disparities affecting AAs and NHPIs.
Keywords: Community health partnerships, community-based participatory research, health disparities, Asian Americans, Native Hawaiians, Pacific Islanders, research capacity building
Racial and ethnic minorities, including Asian American, Native Hawaiian, and Pacific Islander (AA and NHPI) populations, face significant health disparities. AA and NHPI communities are marked, however, by a considerable lack of health data and a tendency in the public health field to aggregate existing AA and NHPI data, further masking significant subgroup disparities.1,2 Few epidemiologic studies of AA and NHPI have been conducted, and even fewer have disaggregated data by subgroups for analysis. Thus, there is a weak body of evidence and knowledge to guide service planning and decision making in health services and policy development for AA and NHPI populations. A paradigm is needed that integrates the role and value of community involvement as a cornerstone to addressing health problems facing communities. Research conducted by or in partnership with communities is likely to be more meaningful and may lead to findings that can inform practice and have immediate impact on community health.
Community-based participatory research (CBPR)—the active and equal partnership of community stakeholders throughout the research process—has been identified as a promising strategy to address health disparities. It allows for the promotion of community relevant and culturally appropriate responses that can take into account the diversity within AA and NHPI subgroups.1,3–5 A key component of CBPR is building community capacity and promoting co-learning.6 If community-based organizations (CBOs) are to be involved as equal partners in the research process, they must be equipped with the language of research and requisite skills for engaging in the research discourse.7 An important tool for building research capacity is training and education. Ultimately, building research capacity will allow CBOs to better advocate for and improve the health of communities they serve.8
There exists, however, limited published information on research training programs for CBOs and none specific to AA and NHPI populations. Characteristically in CBPR projects, academic partners provide research training that is focused on a particular research method that will be utilized in the study, for example, collecting survey data, or conducting focus groups.9,10 Moreover, the literature does not include descriptions of the development and implementation of trainings, nor are the trainings themselves typically evaluated to assess satisfaction with the trainings, knowledge uptake, and skills development.
The training programs that have been reported in the literature tend to be resource and time intensive, requiring 3- to 12-month training commitments.7,11,12 Some examples include a year-long training program in Texas, which led participants through the conception, design, implementation, analysis, and dissemination of a project generated from a CBO’s program interests. Participating CBOs were recruited through a grant application process and were provided financial incentives plus availability of small research assistance funds.7 A formal evaluation was not conducted; thus, little information is presented on factors that contributed or impeded program outcomes. A training program on Long Island, New York,12 did conduct a formal evaluation that indicated an increase in participants’ research knowledge. The authors concluded, however, that the 15-week curriculum using an adapted masters-level public health training course led by faculty members may not be easily scaled up.
In sum, there exists a gap in the literature on the research training needs of CBOs and on evidence-based strategies to build their skills. There is also a lack of reporting on the use of a needs and resource assessment to inform the development of a training program curriculum, including identifying priority training topics and barriers and facilitators to effective knowledge transfer, including how and when the trainings should be implemented.
BACKGROUND
In 2009, the New York University (NYU) Center for the Study of Asian American Health (CSAAH), a National Institutes of Health National Institute on Minority Health and Health Disparities National Research Center of Excellence dedicated to reducing health disparities in the AA community, created a partnership (“the Partnership”) with the Asian & Pacific Islander American Health Forum (APIAHF), a national advocacy organization aimed at improving the health and well-being of AAs and NHPIs, and the Association of Asian Pacific Community Health Organizations (AAPCHO), a national association of community health centers dedicated to improving the health status and access to care of AAs and NHPIs. The Partnership was focused on developing strategies to further the conduct of health disparities research in AA and NHPI communities, including the enhancement of community’s ability to participate or initiate research and prevention/management activities.
Few CBOs have the tools to integrate or initiate research into their programmatic agenda. The Partnership’s goal is to support CBO research infrastructure development by creating a research capacity-building training program. To create a useful training program that can be integrated into a CBO’s organizational structure, the Partnership recognized the need to convene a national advisory committee and to conduct a needs and resource assessment to understand the challenges and facilitators to CBOs’ capacity to enact community-initiated and community-driven research. The purpose of this paper is to present the results of the mixed-method needs and resource assessment conducted to understand the capacity and research needs of CBOs who serve the AA and NHPI communities. We also discuss how this information was used to identify priorities and approaches for the development of a curriculum for the Community Empowered Research Training (CERT) program.
METHODS
Development of CERT
The CERT Program is being developed under the guidance of three university–community collaborative efforts. First, the NYU Health Promotion & Prevention Research Center’s Training Core, composed of community-based and academic experts in the field of training development and delivery, engages in monthly meetings to identify, review, refine, and approve training program components.
Second, the Partnership developed the National Advisory Committee on Research Development (NAC), a national committee composed of ten members representing community service organizations, advocacy organizations, and research institutions who have a broad range of community, policy, research, and evaluation expertise within the AA and NHPI health community, to advise on the development of the CERT program. The members of NAC were recruited through nominations of individuals with expertise within the AA and NHPI health community. The process consisted of a formal letter of nomination from a person familiar with the nominee’s career as well as self-nominations. Partnership directors reviewed nominations and formally invited individuals to serve a 2-year term on the Committee. NAC members participated in two face-to-face group discussions, and continue to provide guidance through monthly conference calls.
The first face-to-face group discussion was a 5-hour meeting that took place in June 2010. The meeting was co-facilitated by one APIAHF and one CSAAH staff member using a discussion guide and agenda that was co-created and finalized during two prior conference calls by the Partnership. The main purpose of the guide was to gain an exploratory understanding of how to build research capacity in AA and NHPI serving community groups, including needs, priorities, and strategies. The second half of the guide was to generate discussion and gain feedback and assessment on an initial draft of the needs and resource assessment tool. Suggestions for improvement and participant recruitment strategies were discussed and recorded. The second face-to-face group discussion was a 6-hour meeting that took place in November 2010. The meeting was again co-facilitated by one APIAHF and one CSAAH staff member and followed a discussion guide and agenda co-created by the Partnership during two prior conference calls. The purpose of this second discussion group was to present and discuss the results of the needs and resource assessment and identify principles and priority areas for the CERT curriculum. Consensus on priority topic areas for the CERT curriculum was recorded.
Last, the Community Advisory Board of the Community Engagement and Population Health Research Core of the NYU–HHC Clinical and Translational Science Institute reviewed project goals and helped to pilot the needs and resource assessment. The Community Engagement and Population Health Research Community Advisory Board consists of 19 community leaders representing a diverse cross-section of New York City’s racial and ethnic communities and integrating different perspectives from government, healthcare, social services, and CBOs. This approach to the development of CERT ensured full and equal involvement of the community congruent with the CBPR approach.
Needs and Resource Assessment
The needs and resource assessment was developed collaboratively with the Partnership and the NAC. The survey instrument was adapted from a needs assessment tool created by AAPCHO and the National Association of Community Health Centers. The on-line survey captured (1) organizational characteristics, such as agency type and size, (2) the extent to which agencies participate or are interested in engaging in research, such as type of research activities and number of years engaged in research activities, (3) research-related training, technical assistance, and resources needed, such as priority training topics and elements of effective trainings, and (4) agencies’ current level of infrastructure for research activities, such as policies and procedures, and hard infrastructure such as computers and meeting space. The survey was pilot tested with five leaders from CBOs and revised accordingly.
Sampling
Using snowball sampling, CBO partners of CSAAH, APIAHF, and the NAC were included in the sampling frame and further asked to recommend additional CBOs to participate in the survey. A survey sampling frame of 110 CBOs who serve a range of ethnic minority and other underserved communities across the United States was constructed (Table 1). The survey was also sent out through two community health list servers with large memberships of CBOs engaged in academic-based research, potentially representing an additional 150 organizations. In total, 50 surveys were completed from September 2010 to January 2011. An Institutional Review Board (IRB) protocol proposal submitted to NYU School of Medicine for Exempt Review was returned by the IRB Committee with the conclusion that the study did not qualify as human subjects research. The study team withdrew the Request for Exemption by request of the IRB.
Table 1.
Key Organizational Groups and Networks Included in the Needs and Resource Assessment Survey Sample
| Organization | Description |
|---|---|
| National Advisory Committee on Research Development (NAC) | A national committee composed of members representing community service organizations, advocacy organizations, and research institutions representing AA and NHPI communities |
| Health Through Action (HTA) Grantees of APIAHF | Health Through Action is a community investment initiative between the W. K. Kellogg Foundation and APIAHF to eliminate health inequities in AA and NHPI communities. |
| Pilot Grantees and Pilot Grant Applicants of the NYU B Free CEED | A national resource and expert center committed to eliminating hepatitis B disparities in Asian and Pacific Islander communities. B Free CEED provides pilot grants to build community capacity to engage in research and outreach to address hepatitis B-related health disparities. |
| Grantees and Community Partners of the Bronx Health REACH | A coalition formed to eliminate racial and ethnic disparities in health outcomes in diabetes and heart disease in African American and Latino communities in the southwest Bronx |
| Kellogg Community Health Scholars Program (KHSP) | A network of current and past post-doctoral fellows engaged in CBPR projects sponsored by KHSP, their program academic mentors, and community-based mentors. |
| Community Partners of the Community Engagement Core of the Johns Hopkins Institute for Clinical and Translational Research (ICTR) | A coalition of community leaders and CBO representatives who serve on the Community Research Advisory Council to advise the ICTR. |
| Coalition members of the Brooklyn Perinatal Network | A network aimed at addressing the high rate of infant mortality in the Brownsville section of Brooklyn and ensuring better maternal child health outcomes |
| Community Partners of the Mount Sinai Community IMPACT Diabetes Center | A multi-level, community-focused center aimed at improving diabetes-related health outcomes in primarily East Harlem and other communities predominantly populated with African Americans and Hispanics/Latinos |
| Community Advisory Board (CAB) members of the Community Engagement and Population Health Research (CEPHR) Core of the NYU-HHC Clinical and Translational Science Institute | The CAB provides direction and guidance to CEPHR program activities. The CAB includes representation from a diverse cross-section of New York City’s racial and ethnic communities and integrates different perspectives from government, healthcare, social services, and community leaders |
| National Community Committee (NCC) of the Health Promotion and Prevention Research Center (PRC) | The National Community Committee (NCC) is one of seven committees that help guide the PRC Program. The committee represents the people in communities that work with PRCs to do CBPR in chronic disease prevention and control |
Data Analysis
This paper presents findings on the 27 surveys representing CBOs that serve AA and NHPI communities. Descriptive data analysis was conducted on the survey findings using SAS 9.2 software (SAS, Inc., Cary, NC). Qualitative data from the two group discussions with the Partnership and NAC members are also presented. Detailed minutes were transcribed during the meetings and then reviewed for accuracy and amended as needed by the meeting participants. These meeting minutes were then reviewed and themes and concepts identified and coded.
RESULTS
Survey Findings
Respondents represented a range of agencies in relation to size, geography, type of services provided, and years and extent of involvement in research (Table 2 and Figure 1). Given the sample targeted for the survey, it is not surprising that 89% (24/27) of respondents reported being currently engaged in research. The majority reported being involved in service-based or programmatic research and CBPR (Table 3). Respondents defined research as a broad array of activities to support their agency’s programmatic and policy agendas, for example, conducting needs assessments, program evaluations, and collecting data for policy advocacy.
Table 2.
Agency Information (N = 27)
| n (%) | |
|---|---|
| Agency type | |
| Community-based | 18 (66.7) |
| Health center | 8 (29.6) |
| Education center | 1 ( 3.7) |
| Number of employees | |
| <10 | 11 (40.7) |
| 10–50 | 10 (37.0) |
| >50 | 6 (22.2) |
| Personnel dedicated to research | |
| Yes | 16 (66.7) |
| Type of personnel involved in research (n = 16) | |
| Project coordinators | 13 (81.3) |
| Principal investigators | 10 (62.5) |
| Administrative support staff | 9 (56.3) |
| Project managers | 8 (50.0) |
| Community health workers | 8 (50.0) |
| Community organizers | 6 (37.5) |
| Research assistants | 5 (31.3) |
| Annual budget (U.S.$) | |
| <500,000 | 8 (29.6) |
| 500,000–2,000,000 | 8 (29.6) |
| 2,000,000–5,000,000 | 5 (18.5) |
| >5,000,000 | 6 (22.2) |
| Type of service provided | |
| Health/healthcare | 14 (51.9) |
| Policy/advocacy | 10 (37.0) |
| Social services | 10 (37.0) |
| Research | 8 (29.6) |
| Education | 7 (25.9) |
| Capacity building | 6 (22.2) |
Figure 1.
Geographical distribution of agencies surveyed.
Table 3.
Agency Responses to Select Research-Related Questions (n = 24)
| n (%) | |
|---|---|
| In what types of research is your agency currently involved? | |
| Service-based research (e.g., conducting a needs assessment to determine the need for a program or intervention). | 19 (79.2) |
| CBPR. | 16 (66.7) |
| Policy-related research. | 11 (45.8) |
| Health services research other than clinical trials (e.g., monitoring and evaluation of health services). | 9 (37.5) |
| Behavioral or sociological research (e.g., substance use among urban youth). | 8 (33.3) |
| Clinical trials (e.g., testing patient safety and efficacy of a new drug). | 2 ( 8.3) |
| To what extent is your agency currently involved in research? | |
| We conduct research in partnership with one or more institutions (e.g., with a faculty member at a university). | 24 (100.0) |
| We conduct research in partnership with one or more community groups. | 19 (79.2) |
| We conduct research on our own. | 17 (70.8) |
| We advise on research being conducted by others (e.g., serving on a study advisory committee). | 16 (66.7) |
| We endorse or support research being conducted by others (e.g., writing a letter of support for a study). | 13 (54.2) |
| We participate in research training being conducted by others (e.g., serving as a site for a multisite study). | 9 (37.5) |
| Overall, what percentage of your agency’s work has been involved in research? | |
| <10% | 4 (17.4) |
| 10%–25% | 12 (52.2) |
| 25%–50% | 6 (26.1) |
| 50%–75% | 1 ( 4.3) |
| >75% | 0 ( 0.0) |
| In the past 3 years, has your agency been the primary recipient of any research grants or funding (as opposed to a subcontractor)? | |
| Yes | 11 (47.8) |
Despite the high numbers engaged in some type of research activity, 96% (26/27) of respondents indicated that they were interested in developing their research capacity. Findings indicate that agencies’ main motivations for building their research capacity include to inform policy and to build up, evaluate, and sustain programs (Table 4). Almost 67% (16/24) of CBOs dedicate 25% or less of their agency’s work on research. Fewer than half (47.8%, 11/24) have been the primary recipient of research grants. Almost 67% (16/24) of CBOs reported having staff who were dedicated to carrying out research activities. The majority of CBOs (88%) indicated having had past collaborations with external researchers. When asked what made these collaborations successful, the top three responses included: (1) the partnership helped to build organizational capacity, (2) the partnership was characterized by trust, and (3) the partnership served a useful function. On the other hand, the top three challenges of collaborations with external researchers included the following: (1) the researchers did not understand the CBO’s priorities, (2) the researchers did not understand the community, and (3) the partnership took up more staff time than it was worth. When queried about the top three barriers to participating in research, CBO respondents listed: (1) the need for external funding, (2) the need to align research-related activities with the organizational mission / the lack of research-related funding opportunities for CBOs, and (3) a lack of dedicated staff time to conduct or participate in research.
Table 4.
What Are Your Agency’s Main Motivations for Wanting to Develop Its Ability to Conduct Research and/or Partner With Academic Investigators? (n = 26)
| n (%) | |
|---|---|
| To use data for policy | 24 (92.3) |
| To bring in additional resources | 24 (92.3) |
| To develop programs | 22 (84.6) |
| To evaluate the effectiveness of programs | 22 (84.6) |
| To advance the field of community health | 21 (80.8) |
| To monitor productivity | 15 (57.7) |
| To support staff | 15 (57.7) |
Qualitative Findings
The ten NAC members, representing leadership of national CBOs and community health centers serving AA and NHPI communities, were brought together for two face-to-face discussions. These discussions highlighted several important themes that have informed the overall goal of the CERT program and guided the needs and resource assessment that was conducted. Participants in the first group discussion voiced concern over the lack of AA and NHPI data and confirmed the vital role that CBOs can play in filling the knowledge gap. It was noted that CBOs collect rich data on the communities they serve and that the overall goal of the project should be to help CBOs to reframe how the data can be collected and used to better inform their own programmatic activities and to address larger health disparities facing the AA and NHPI communities they serve.
Discussants pointed out, however, that not all CBOs are interested in conducting research or building their research capacity because of their service focus. Instead, there was agreement that, at this stage, our time would be better spent on identifying and targeting CBOs interested in conducting research. Furthermore, a distinction was made between research-ready organizations—an organization that with minimal training and technical assistance may be ready to engage in research or a research partnership—and organizations that are not research ready. The group consensus was that given limited resources, for these organizations, it may not be realistic to build their in-house capacity for research. Instead, time would be better spent providing them with a foundation of knowledge, an overview of the value of data and research, and the tools and resources to negotiate equitable partnerships with research entities. Discussants also pointed out that AA and NHPI serving CBOs often face additional challenges in part because of the heterogeneity of AA and NHPI populations. This heterogeneity in languages, cultures, and approaches to health result in few pan-Asian CBOs and instead a greater number of smaller issue-specific CBOs serving culturally and linguistically distinct subpopulations. The result is greater competition for limited resources and perhaps a greater reluctance on the part of AA and NHPI serving CBOs to include research activities along with their service focus.
Informing the CERT Curriculum
Survey Findings
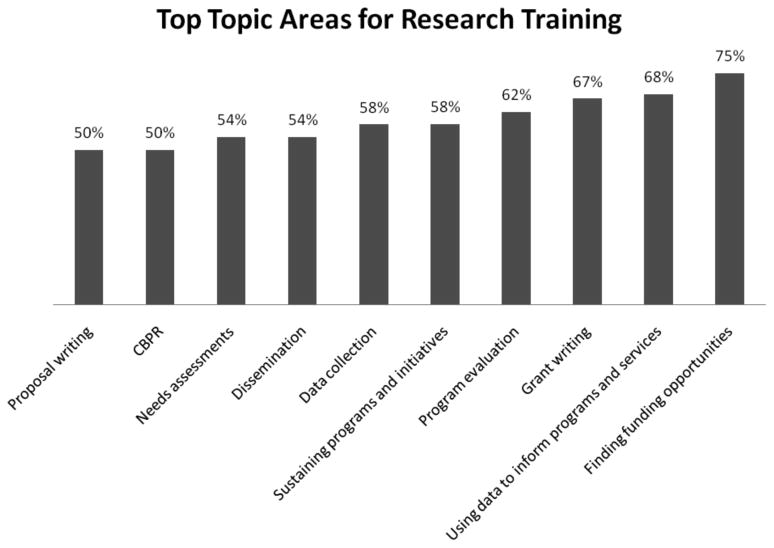
The survey also included questions to directly inform the curriculum and format of the CERT program. For example, survey respondents were queried on priority research training topics. Top responses included finding and capitalizing on funding opportunities, grant writing, using data to inform programs and services, and planning and conducting program evaluations. There was less interest in disseminating and reporting of research and evaluation findings, using information from the published public health literature, or data-related activities including data collection methods or data analysis (Figure 2). The majority of respondents noted that senior leadership and management should attend such training programs: 81.5% indicated that staff at the program director or managerial level, and 44.4% answered at the executive director level (Table 5). Findings from the group discussions also underscored the need to target the participation of the CBO’s executive director in order to secure buy-in and support for organizational-level change, as well as to mitigate the loss of research skills owing to staff turnover, which is common among CBOs. The majority of survey respondents indicated that a 2- to 3-day intensive program was favored over a multiweek seminar training program. Respondents also expressed a preference for in-person training that takes places in a classroom setting rather than a webinar or toolkit (Table 5).
Figure 2.
Agency priority areas for research training.
Table 5.
Agency Responses to Inform CERT Program (n = 27)
| n (%) | |
|---|---|
| Which level of staff member would you be willing to send to a research training program? | |
| Program director/manager | 22 (81.5) |
| Associate/coordinator | 16 (59.3) |
| Executive director | 12 (44.4) |
| Assistant | 8 (29.6) |
| Director | 8 (29.6) |
| Intern | 7 (25.9) |
| CEO/president | 2 ( 7.4) |
| Not willing to send any staff member | 1 ( 3.7) |
| How much of your time, or a staff member’s time, would you be willing to dedicate to a research-training program? | |
| One full day per week, over several months | 4 (16.0) |
| One full day every 2 weeks, over several months | 2 ( 8.0) |
| One full day per month, over several months | 7 (28.0) |
| Two or 3 full-day intensive | 10 (40.0) |
| One-week intensive | 2 ( 8.0) |
| How effective do you think the following methods of training would be in achieving your learning goals? (Very effective) | |
| Workshops/classroom setting | 20 (80.0) |
| Webinar | 7 (28.0) |
| Toolkit/resource material | 7 (28.0) |
Finally, in response to an open-ended question for additional thoughts regarding engaging CBOs in research, three main themes emerged: (1) the importance of a training program that understands the tensions between the programmatic priorities of an agency and research activities, (2) the importance of a training program that builds the capacity of agencies to carry out relevant research activities to inform the agencies’ programmatic and policy agendas, and (3) the importance of bidirectional capacity building, to ensure that academic institutions understand community concerns related to research and how to foster equitable partnerships with community.
Qualitative Findings
Findings from the group discussions provided support for including learning methods that employ adult learning theories into the training approach. Adult learning theory holds that adults learn best through experience (discovery), reflection, and abstract conceptualization.13,14 Therefore, the training curriculum will be grounded in participants’ experiences. Discussions provided support for creating a training program co-facilitated by CBO leaders and that represented community, academic, foundation, and government perspectives. Discussants also stressed the importance of sharing community experience through the use of case studies and to highlight not only successes but also lessons learned.
DISCUSSION
The majority of CBO survey respondents reported currently being engaged in research. This was expected given the survey sample was derived from CBOs who have a relationship with organizations engaged in community health research. Ninety-six percent, however, reported an interest in developing their ability to conduct research. Overall, research was reported as a means to sustain programmatic services and organizational staff. CBO respondents reportedly were less interested in receiving training or technical assistance on using available evidence-based health information or on disseminating research and evaluation findings; however, one of the top three motivators for wanting to develop research capacity was to advance the field of community health.
In general, the qualitative data from the group discussions validated survey findings. Findings supported the role that external researchers can play in providing research support and the need to provide tools and resources for CBOs to support equitable partnerships and to foster co-learning. Findings also highlighted the importance of developing a training model that is relevant to CBOs and that helps to reframe the role of research to align with their organizational mission. Furthermore, the group discussions illuminated important contextual factors specific to AA and NHPI serving CBOs. For example, because of the heterogeneity of AA and NHPI communities, who represent myriad culturally and linguistically distinct populations, AA and NHPI serving CBOs may be even more fragmented than other CBOs serving ethnic minority communities. For this reason, there is likely to be a greater range between CBOs that are not research ready and CBOS that are research ready. Therefore, research training programs aimed at building the research capacity of AA and NHPI serving CBOs will need to target trainings to the different levels of research readiness.
Findings suggest that the development of training programs should be targeted to higher level personnel, and that in-person, short-duration programs would be the most effective and accessible to CBOs. To engage CBO interest, findings also suggest that sessions on identifying and capitalizing on funding opportunities, grant writing, and using data to inform programs and policies should be prioritized in the curriculum. Importantly, findings also stressed the importance of a training program co-developed and implemented with CBO leadership.
Limitations
The survey was sent to more than 260 CBOs through a snowball sampling frame. The organizations that completed the survey may represent CBOs already participating in and interested in research activities, thus presenting a self-selection bias. Furthermore, the small sample size (N = 27) precludes the study team from assessing differences based on key characteristics of the organization, such as size of organization, geography, mission, and so on. Because the survey was completed by a convenience sample of organizational leaders from mostly research-ready CBOs, the findings may be unique to organizational leaders who are interested in research or building research capacity and may not be representative of CBOs overall. The use of a mixed-methods approach allowed us to collect information that provided context to the survey findings.
Future work should strive to capture a larger sample of diverse CBOs, specifically those not already engaged in research activities in order to more fully understand how to target training programs to non–research-ready groups. Attempts should also be made to capture a larger sample size in order to analyze differences in organizational characteristics. In addition, future surveys should capture specific ethnic group data in order to better understand if there are unique capacity building needs for CBOs serving specific ethnic subpopulations.
CONCLUSION
In our study, CBOs serving AA and NHPI communities were found to be engaged in local, service-related research. These CBOs possess both an interest and access to rich, local knowledge that can inform health disparity priorities. There is a need for evidence-based training to build the research capacity of CBOs. The CERT program can encourage CBOs to engage in community-initiated and driven research that will ultimately create a pool of trained community members poised to address the health disparities within their communities.
Acknowledgments
The NYU CSAAH is a National Institutes of Health National Institute for Minority Health and Health Disparities Research Center of Excellence (COE) dedicated to reducing health disparities in the AA community. The APIAHF is a national advocacy organization aimed at improving the health and well-being of AAs and NHPIs. AAPCHO is a national association of community health centers dedicated to improving the health status and access to care of AAs and NHPIs.
The authors acknowledge the contributions of our local partners and individuals who are engaged in this collaborative effort: Charles B. Wang Community Health Center (Shao- Chee Sim, Art Cusack, Sylvia Wong), and the NYU Steinhardt School of Culture, Education and Human Development’s Public Health Program (Yumary Ruiz).
The authors thank all the members of the NAC who provided guidance and input on the development and recruitment for the capacity building needs assessment project for APIAHF and CSAAH: Peter Cheng, Marianne Chung, Zeenat Hasan, Linda Lee, Fahina Tavake-Pasi, Therese Rodriguez, Marguerite Ro, Shao-Chee Sim, Hardayal Singh, Alek Sripipatana, and Rosy Chang Weir. We also thank Laura Wyatt (CSAAH) for her assistance with the data analysis, Corina Chung and Lloyd Asato (APIAHF) for their project coordination and support, Rhodora Ursua (CSAAH) for her review of the manuscript, and Rebecca Park (CSAAH) for coordination and submission. Last, the authors acknowledge the leadership of the APIAHF and CSAAH in supporting this effort: Kathy Lim Ko (APIAHF) and Mariano Rey (CSAAH).
The authors acknowledge the National Institutes of Health, the Centers for Disease Control and Prevention, and the Health Through Action Program, via support from the W.K. Kellogg Foundation. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, the CDC, and the W.K. Kellogg Foundation.
References
- 1.Ro MJ, Yee AK. Out of the shadows: Asian Americans, Native Hawaiians, and Pacific Islanders. Am J Public Health. 2010 May;100:776–8. doi: 10.2105/AJPH.2010.192229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: Historical challenges and potential solutions. J Health Care Poor Underserved. 2010 Nov;21:1354–81. doi: 10.1353/hpu.2010.0939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Israel BA, Shulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improved public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 4.Minkler M, Wallerstein N, editors. community-based participatory research for health. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- 5.Butterfoss F. Process evaluation for community participation. Annu Rev Public Health. 2006;27:323–40. doi: 10.1146/annurev.publhealth.27.021405.102207. [DOI] [PubMed] [Google Scholar]
- 6.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006 Jul;7:312–23. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 7.May M, Law J. CBPR as community health intervention: Institutionalizing CBPR within community based organizations. Prog Community Health Partnersh. 2008 Summer;2:145–55. doi: 10.1353/cpr.0.0019. [DOI] [PubMed] [Google Scholar]
- 8.Wallerstein N. What is the evidence on effectiveness of empowerment to improve health? Copenhagen: WHO Regional Office for Europe; Health Evidence Network report [2006 Feb; cited 2011 Feb 15]. Available from: http://www.euro.who.int/Document/E88086.pdf. [Google Scholar]
- 9.Tumiel-Berhalter LM, McLaughlin-Diaz V, Vena J, Crespo CJ. Building community research capacity: Process evaluation of community training and education in a community-based participatory research program serving a predominately Puerto Rican community. Prog Community Health Partnersh. 2007 Spring;1:89–97. doi: 10.1353/cpr.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loh P, Sugerman-Brozan J, Wiggins S, Noiles D, Archibald C. From asthma to AirBeat: Community-driven monitoring of fine particles and black carbon in Roxbury, Massachusetts. Environ Health Perspect. 2002 Apr;110( Suppl 2):297–301. doi: 10.1289/ehp.02110s2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Masuda JR, Creighton G, Nixon S, Frankish J. Building capacity for community-based participatory research for health disparities in Canada: The case of “partnerships in community health research”. Health Promot Pract. 2010;12:280–92. doi: 10.1177/1524839909355520. [DOI] [PubMed] [Google Scholar]
- 12.Goodman MS, Dias JJ, Stafford JD. Increasing research literacy in minority communities: CARES Fellows Training Program. J Empir Res Hum Res Ethics. 2010 Dec;5(4):33–41. doi: 10.1525/jer.2010.5.4.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knowles MS. The modern practice of adult education: From pedagogy to andragogy. Rev. Chicago: Follett Publishing Company; 1980. [Google Scholar]
- 14.Knowles MS. The adult learner: A neglected species. 3. Houston: Gulf Publishing Company; 1984. [Google Scholar]