Abstract
Campylobacter and Salmonella spp. prevalence and antimicrobial drug sensitivity were determined in northern elephant seals that had not entered the water and seals that were stranded on the California coast. Stranded seals had a higher prevalence of pathogenic bacteria, possibly from terrestrial sources, which were more likely to be resistant.
Keywords: Campylobacter; Enterobacteriaceae; Pinnipedia, Salmonella enterica, zoonosis, dispatch
A limited number of surveys have shown that pinnipeds (seals, sea lions, and walruses) can be infected with zoonotic enteric bacteria, including Salmonella and Campylobacter spp. and that some strains are resistant to antimicrobial drugs (1–3). Because both Salmonella and Campylobacter spp. are important zoonotic organisms, their presence in marine mammal feces raises concerns regarding risks to human health associated with exposure to coastal waters and marine mammals. Another concern is that these bacteria in marine mammals may reflect pollution of the California coast by feces from terrestrial sources, including sewage and runoff that contain domestic animal waste. To address these concerns, more detailed data on bacterial pathogen distribution along the California coast are needed.
Northern elephant seals (Mirounga angustirostris) are born on various California beaches and do not leave the beaches for several months after birth (4). Once the seals leave their natal beaches, they are at sea for most of their lives other than during breeding and the annual molt or if they are found "stranded" (if poor health or injury prevents them from leaving the shore) (5). We investigated the prevalence and antimicrobial drug sensitivity of Salmonella and Campylobacter spp. in northern elephant seals at different sites in California to ascertain the distribution of these bacteria in pinnipeds and determine their potential effect on marine mammal and human health.
The Study
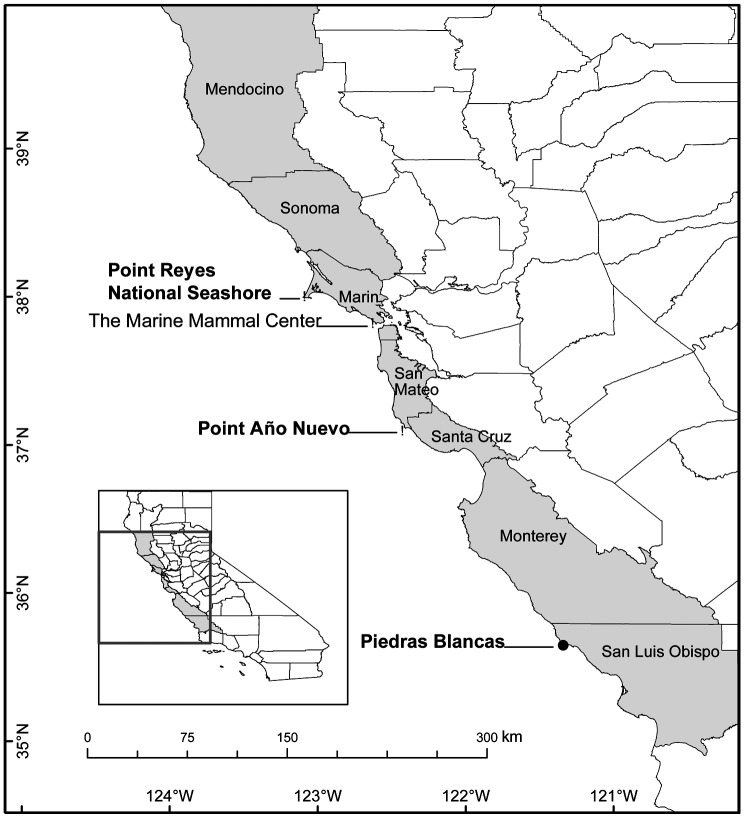
In February and March of 2003 and 2004, 165 northern elephant seals, which had been recently weaned and had never entered the water, were sampled on their natal beaches at 3 colonies in California (Figure). From February to July in 2003 and 2004, 195 juvenile northern elephant seals were found stranded live along the California coast, rescued, and brought to The Marine Mammal Center (TMMC), Sausalito, California, for rehabilitation. At TMMC, seals were physically restrained and examined, and rectal swabs with Cary-Blair transport medium (BD Diagnostics, Franklin Lakes, NJ, USA) were collected for bacterial culture. Animals were not treated until after sampling.
Figure.
Location of The Marine Mammal Center (TMMC), rescue range of TMMC (shaded), and northern elephant seal rookeries (Point Reyes National Seashore, Point Año Nuevo, Piedras Blancas) where seals were sampled along the California coastline.
Salmonella enterica was isolated, identified with standard procedures (6), and stored at –80°C in Microbank bead vials (Pro-Lab Diagnostics, Austin, TX, USA) until it was tested for antimicrobial drug susceptibility. Salmonella isolates were sent to the National Veterinary Services Laboratory (Ames, IA, USA) for serotyping. Antimicrobial drug susceptibility was performed with broth microdilution according to the Sensititre user manual and National Committee for Clinical Laboratory Standards (NCCLS) guidelines (7) for amikacin, amoxicillin-clavulanic acid, ampicillin, cefazolin, ceftiofur, ceftizoxime, chloramphenicol, enrofloxacin, gentamicin, tetracycline, ticarcillin-clavulanic acid, and trimethoprim-sulfamethoxazole. Campylobacter spp. were selected by using Campy-CVA agar (Hardy Diagnostics, Santa Maria, CA, USA) that was incubated under microaerophilic conditions at 37°C for 48 to 96 h, identified by using standard procedures (8), and stored at –80°C in Microbank bead vials until they were tested for antimicrobial drug susceptibility. Campylobacter isolates were tested for susceptibility to ciprofloxacin, doxycycline, erythromycin, and gentamicin according to previously described techniques (9,10). Odds ratios were compared among the different bacteria and seal populations by using mixed- or fixed-effects logistic regression, with geographic location as the random effect and seal rookery as the fixed effect (11). A forward-stepping algorithm was used, and terms with p<0.05, based on the Wald statistic, were included in the final model.
Salmonella spp. were isolated from 3 (1.8%) of 165 natal-site elephant seals and 72 (36.9%) of 195 stranded seals. Stranded seals were 41× more likely to test positive for Salmonella spp. than natal-site seals (odds ratio [OR] 40.9, p<0.001, 95% confidence interval [CI] 7.7–218). All 3 Salmonella isolates from the natal-site seals were serotype Typhimurium and were sensitive to all antimicrobial drugs tested (Table 1). Eighty-three Salmonella isolates of 5 different serotypes, Newport, Saint Paul, Montevideo, Typhimurium, and Reading, were collected from 72 stranded seals; Newport was the most common serotype. Eleven stranded seals were positive for 2 different serotypes. Only 4 Salmonella Newport isolates from stranded seals were resistant to antimicrobial drugs; 3 isolates were resistant to ampicillin, with intermediate resistance to ticarcillin-clavulanic acid, and 1 isolate was resistant to amoxicillin–clavulanic acid and cefazolin.
Table 1. Serotypes and antimicrobial drug resistance* of Salmonella spp. isolated from natal-beach and stranded northern elephant seals, California, 2003–2004.
| Serotype | No. resistant isolates/total (%) |
|
|---|---|---|
| Natal-beach seals | Stranded seals | |
| Newport | 0/0 | 4/42 (9.5) |
| Saint Paul | 0/0 | 0/17 |
| Montevideo | 0/0 | 0/15 |
| Typhimurium | 0/3 | 0/2 |
| Reading | 0/0 | 0/7 |
| All serotypes | 0/3 | 4/83 (4.8) |
*Intermediately resistant or resistant to >1 antimicrobial drugs.
On the basis of biochemical analysis, Campylobacter jejuni, C. lari, and an unknown Campylobacter sp. were isolated from both groups of elephant seals (Table 2). C. jejuni was the most common Campylobacter species isolated, followed by C. lari and the unknown Campylobacter sp. (Table 2). One natal-site seal and 8 stranded seals were infected with 2 Campylobacter spp. Stranded seals were 6.0× more likely to test positive for Campylobacter spp. than natal-site seals (OR 5.97, p<0.001, 95% CI 4.2–8.4). Stranded seals were 4.3× more likely to be positive for C. jejuni (OR 4.33, p<0.001, 95% CI 1.8–10.6), 7.2× more likely to be positive for C. lari (OR 7.2, p<0.001, 95% CI 2.4–21.4), and 22× more likely to be positive for the unknown Campylobacter sp. (OR 21.9, p = 0.003, 95% CI 2.9–164) than natal-site seals. Ciprofloxacin was the only antimicrobial drug to which isolates were resistant (intermediate or complete); resistance was detected in both groups of seals but was more common in stranded seals (Table 2).
Table 2. Prevalence and antimicrobial resistance* of Campylobacter spp. isolated from natal-beach and stranded northern elephant seals, California, 2003–2004.
| Species | Natal-beach |
Stranded† |
||
|---|---|---|---|---|
| Positive seals/total (%)‡ | Resistant isolates/total (%) | Positive seals/total (%)‡ | Resistant isolates/total (%) | |
| Campylobacter jejuni | 17/165 (10.3) | 0/16§ | 54/194 (27.8) | 2/54 (3.7) |
| C. lari | 5/165 (3.0) | 2/5 (40.0) | 26/194 (13.4) | 8/23§ (34.8) |
| Unknown Campylobacter sp. | 1/165 (0.6) | 0/1 | 23/194 (11.9) | 12/20§ (60.0) |
| All Campylobacter spp. | 22/165 (13.3) | 94/194 (48.5) | ||
*Intermediately resistant or resistant to >1 antimicrobial drugs.
†The presence of Campylobacter spp. was not determined for 1 stranded seal because other bacteria overgrew on the plate.
‡Number of seals positive can be fewer than total number of Campylobacter isolates because multiple Campylobacter spp. were isolated from some seals.
§Not all isolates were tested for susceptibility because of contamination or lack of growth after freezing.
Conclusions
Prevalence of Salmonella and Campylobacter spp. was higher in juvenile northern elephant seals that became stranded along the coast of central California than in seals on their natal beaches that had never entered the water. A potential explanation for this difference is that stranded seals may have harbored bacteria but were not shedding them while they were in good health on their natal beaches. Infections with some pathogenic bacteria may be asymptomatic, but animals may intermittently shed bacteria, especially if stressed (12,13). Stress and malnutrition can suppress immunity, which makes an individual animal more susceptible to infection and prolongs existing infection (14). Another possible explanation for the higher prevalence in stranded seals is that stranded animals are more susceptible to infection, because of stress or malnutrition, by pathogens in the environment from terrestrial sources, such as contaminated freshwater and sewage outfall. The fact that isolates from stranded seals tend to be resistant supports this possibility.
The cause of the higher prevalence of pathogenic bacteria in stranded juvenile northern elephant seals should be determined, especially if animals are infected by pathogenic bacteria from terrestrial sources contaminating the marine environment. Coastal freshwater runoff is associated with a high risk for infection of southern sea otters (Enhydra lutris nereis) with Toxoplasma gondii in California and might also be a risk factor for infection of elephant seals with pathogenic fecal bacteria (15). Further studies to identify environmental risk factors for infection of elephant seals with Campylobacter and Salmonella spp. and genetic fingerprinting of these isolates may help determine the sources of these bacteria.
Acknowledgments
We thank Michelle Caudle, Denise Greig, Barbara Byrne, Pat Morris, Brian Hatfield, Rich Walker, Dan Costa, Sarah Allen, Brent Stewart, staff of the University of California Reserve System, the rangers of Año Nuevo State Reserve, and staff of the Point Reyes National Seashore.
This project was supported by the Wildlife Health Center, University of California, Davis; the Prescott Marine Mammal Rescue Assistance Grant Program; and the West Coast Center for Oceans and Human Health (WCCOHH) as part of the National Oceanic and Atmospheric Administration Oceans and Human Health Initiative, WCCOHH publication no. 4. WCCOHH is part of the National Marine Fisheries Service's Northwest Fisheries Science Center, Seattle, Washington. Samples were collected under MMPA permits numbers 87-1593-01, 373-1575, and 486-1506.
Biography
Dr Stoddard is a research fellow at TMMC, Golden Gate National Recreation Area, Sausalito, California. Her research interests are marine mammals as indicators of fecal bacterial contamination in the marine environment, including pathogenic bacteria and antimicrobial drug–resistant commensal bacteria such as Escherichia coli.
Footnotes
Suggested citation for this article: Stoddard RA, Gulland FMD, Atwill ER, Lawrence J, Jang S, Conrad PA. Salmonella and Campylobacter spp. in northern elephant seals, California. Emerg Infect Dis [serial on the Internet]. 2005 Dec [date cited]. http://dx.doi.org/10.3201/eid1112.050752
References
- 1.Smith WA, Mazet JA, Hirsh DC. Salmonella in California wildlife species: prevalence in rehabilitation centers and characterization of isolates. J Zoo Wildl Med. 2002;33:228–35. [DOI] [PubMed] [Google Scholar]
- 2.Foster G, Holmes B, Steigerwalt AG, Lawson PA, Thorne P, Byrer DE, et al. Campylobacter insulaenigrae sp. nov., isolated from marine mammals. Int J Syst Evol Microbiol. 2004;54:2369–73. 10.1099/ijs.0.63147-0 [DOI] [PubMed] [Google Scholar]
- 3.Johnson SP, Nolan S, Gulland FM. Antimicrobial susceptibility of bacteria isolated from pinnipeds stranded in central and northern California. J Zoo Wildl Med. 1998;29:288–94. [PubMed] [Google Scholar]
- 4.Le Boeuf BJ, Laws RM. Elephant seals: an introduction to the genus. In: Le Boeuf BJ, Laws RM, editors. Elephant seals: population ecology, behavior, and physiology. Berkeley (CA): University of California Press; 1994. p. 1–26. [Google Scholar]
- 5.Wilkinson DM. Report to assistant administrator for fisheries: program review of the Marine Mammal Strandings Networks. Silver Springs (MD): US Department of Commerce, National Marine Fisheries Services; 1991. [Google Scholar]
- 6.Bopp CA, Brenner FW, Fields PI, Wells JG, Strockbine NA. Escherichia, Shigella, and Salmonella. In: Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, editors. Manual of clinical microbiology. Washington: ASM Press; 2003. p. 654–71. [Google Scholar]
- 7.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals, approved standards; NCCLS document M31-A2. Wayne (PA): The Committee; 2002. [Google Scholar]
- 8.Nachamkin I. Campylobacter and Arcobacter. In: Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, editors. Manual of clinical microbiology. Washington: ASM Press; 2003. p. 902–14. [Google Scholar]
- 9.McDermott PF, Bodeis SM, Aarestrup FM, Brown S, Traczewski M, Fedorka-Cray P, et al. Development of a standardized susceptibility test for Campylobacter with quality-control ranges for ciprofloxacin, doxycycline, erythromycin, gentamicin, and meropenem. Microb Drug Resist. 2004;10:124–31. 10.1089/1076629041310064 [DOI] [PubMed] [Google Scholar]
- 10.National Committee for Clinical Laboratory Standards. MIC testing supplemental tables; NCCLS document M100-S13 (M7). Wayne (PA): The Committee; 2003. [Google Scholar]
- 11.StataCorp. Stata cross-sectional time series, reference manual: release. College Station (TX): StataCorp; 2003. p. 32–140. [Google Scholar]
- 12.Clegg FG, Chiejina SN, Duncan AL, Kay RN, Wray C. Outbreaks of Salmonella Newport infection in dairy herds and their relationship to management and contamination of the environment. Vet Rec. 1983;112:580–4. 10.1136/vr.112.25.580 [DOI] [PubMed] [Google Scholar]
- 13.Jones K, Howard S, Wallace JS. Intermittent shedding of thermophilic campylobacters by sheep at pasture. J Appl Microbiol. 1999;86:531–6. 10.1046/j.1365-2672.1999.00702.x [DOI] [PubMed] [Google Scholar]
- 14.Amati L, Cirimele D, Pugliese V, Covelli V, Resta F, Jirillo E. Nutrition and immunity: laboratory and clinical aspects. Curr Pharm Des. 2003;9:1924–31. 10.2174/1381612033454252 [DOI] [PubMed] [Google Scholar]
- 15.Miller MA, Gardner IA, Kreuder C, Paradies DM, Worcester KR, Jessup DA, et al. Coastal freshwater runoff is a risk factor for Toxoplasma gondii infection of southern sea otters (Enhydra lutris nereis). Int J Parasitol. 2002;32:997–1006. 10.1016/S0020-7519(02)00069-3 [DOI] [PubMed] [Google Scholar]