Abstract
Objective
To compare associations of varus thrust and varus static alignment with pain in those with knee osteoarthritis (OA).
Method
This was a cross-sectional study of participants from a randomized controlled trial of vitamin D for knee OA. Participants were video recorded walking and scored for presence of varus thrust. Standard PA knee X-rays were measured for static alignment. Pain questions from the Western Ontario McMasters Osteoarthritis (WOMAC) questionnaire assessed symptoms.
We calculated means for total WOMAC pain by varus thrust and varus alignment (i.e. corrected anatomic alignment < 178°). We performed ordinal logistic regressions; outcomes: individual WOMAC pain questions; predictors: varus thrust and varus alignment.
Results
There were 82 participants, mean age 65.1 (±8.5), mean body mass index 30.2 (±5.4), and 60% female. Total WOMAC pain was 6.3 versus 3.9, p = 0.007 in those with versus without definite varus thrust. For varus alignment, total WOMAC pain was 5.2 versus 4.2, p = 0.30.
Odds ratios for pain with walking and standing were 5.5 (95%CI 2.0 – 15.1) and 6.0 (95%CI 2.2 – 16.2) in those with versus without definite varus thrust. There were no significant associations between varus alignment and individual WOMAC pain questions. Sensitivity analyses suggested a more stringent definition of varus might have been associated with walking and standing pain.
Conclusion
In those with knee OA, varus thrust and possibly varus static alignment, were associated with pain, specifically during weight-bearing activities. Treatment of varus thrust (e.g. via bracing or gait modification) may lead to improvement of symptoms.
Introduction
Osteoarthritis (OA) is a major public health problem as it is the most common form of arthritis occurring in 33% of people over the age of 601 and is a leading cause of disability among the elderly.2 This is particularly problematic because only limited therapies have been proven effective in reducing symptoms with the mainstay of treatment being NSAIDs, non-specific physical therapy interventions, local corticosteroid injections, and ultimately when these are ineffective, total joint replacements.3 The economic implication of OA is also substantial with direct costs attributable to the disease in the US exceeding $185 billion in 2007.4
In recent years, there is growing data to support that biomechanics are important in the pathophysiology of knee OA, with research showing that static and dynamic alignment are potent predictors of longitudinal progression.5–7 Static alignment, defined as the coronal plane assessment of the hip-knee-ankle angle, is an important determinant of load distribution within a knee.7 The load-bearing axis, a line drawn from the mid-femoral head to the mid-ankle, passes medial to the knee in a varus knee, which leads to increased forces across the medial compartment. Dynamic alignment is assessed during ambulation. Varus thrust is an easy to assess measure of dynamic alignment that has been defined as the first appearance of varus or abrupt worsening of existing varus while the limb is weight bearing during ambulation, with a return of the limb to a less varus alignment during the swing phase, or non-weight-bearing phase, of gait.5 This is a simple clinical assessment that does not require measurement using a sophisticated gait laboratory. Because knee pain in OA occurs predominantly with weight-bearing, it is reasonable to expect that dynamic findings may be more predictive of knee pain than static measures.
The WOMAC pain subscale is the sum of scores from 5 questions assessing knee symptoms, a validated instrument widely used in studies of knee osteoarthritis.8 However, there is growing evidence that the use of this summed score may not be appropriate. A publication studying the measurement properties of the WOMAC pain subscale suggests that the 5 WOMAC pain questions represent 2 separate domains where the questions asking about pain walking on a flat surface and on stairs represent one domain and the questions on night-time and sitting activities represent a second domain9. The standing question loaded on both factors. Therefore, summation of the 5 questions may not be the optimal method to evaluate knee OA symptoms. It has been proposed that perhaps only the items that display homogeneity should be summed or that each question be evaluated individually. Because varus thrust is a measure of dynamic alignment that becomes evident with ambulation, the pain questions that assessed pain during weight-bearing activities were of particular interest to us.
The objective of this study was to evaluate the relationship of static alignment and varus thrust with pain in people with established knee OA. We hypothesized that there would be a relationship between varus thrust and pain, particularly with weight-bearing activities, but not between varus static alignment and pain.
Methods
Sample Selection
This was a cross-sectional study of a convenience sample selected from participants of a randomized controlled trial (RCT) of vitamin D for symptomatic radiographic knee OA (began 06/01/2005 and ended 09/30/2010) performed at Tufts Medical Center, Boston, MA. All study activities were approved by the Tufts Medical Center Institutional Review Board. Participants were required to have symptomatic radiographic tibiofemoral (TF) knee OA to be enrolled in the parent study RCT, meaning that participants had to have a Kellgren-Lawrence (KL) grade ≥ 2 and were required to have pain on most days of the month for at least a month in the last year in the same knee. The study was not restricted to participants with medial TF OA.
For this study, participants were recruited at the 2 year follow-up visit from the parent study RCT and were required to consent to the additional assessment of varus thrust using a video recording as described below. Investigators were blinded to the treatment allocation as well as to the pain assessment measures at the time of enrollment into this study. We excluded participants using any ambulatory assist device. There was a period of a few months where time during the parent study clinic visits was limited when no participants were recruited into this ancillary study.
Varus Thrust Assessments
Using a standard digital video camera (60 Hz), participants were video recorded walking 20 meters away from and towards a stationary camera at a self-selected speed at the parent study year 2 follow-up visit. Participants were evaluated within the clinic along an identical walking course and were asked to walk bare-footed.
We subjectively assessed for the presence of varus thrust, first appearance of varus or abrupt worsening of existing varus while the limb is weight bearing during ambulation, with a return of the limb to a less varus alignment during the swing phase, or non-weight-bearing phase, of gait. Blinded to the pain assessments, two rheumatologists trained to evaluate varus thrust (GHL & WFH) viewed the gait videos at separate reading sessions. Videos were evaluated for varus thrust as being definitely present, possibly present, or definitely absent. On average, these assessments were based on the first 5–6 strides taken while walking away from and the last 5–6 strides taken while walking towards the camera that could be easily viewed on each video recording. Any disagreements were adjudicated by consensus of both evaluators. The varus thrust score subsequently was dichotomized into two groups, hereforeward described as with definite varus thrust, only including those with the designation of varus thrust being definitely present, and without definite varus thrust which was comprised of those scored as having varus thrust possibly present and definitely absent.
X-rays
Posterior-Anterior (PA) semi-flexed radiographs of the study knee were taken at the parent study screening visit and at the year 2 follow-up visit, the same day on which the gait video recordings were obtained. Participants were asked to stand upright facing the anterior wall with their body weight distributed equally between the two legs. The great toes of both feet were verified to be in contact with the anterior wall. Both feet were fixed in 10° external rotation by positioning the feet on a foot map. Subsequently, the cassette holder was lowered so that the center of the film was located at the level of the participant’s TF joint line. The center line of the positioning frame was verified to be in the center of the cassette holder. Then the participant was asked to flex both knees until they touched the anterior wall of the frame, standardizing the extent of tibial flexion. With the great toes and knees still touching the anterior wall, both thighs were pressed directly against the wall, standardizing the extent of femoral flexion. The field of view was 14 × 17 inches for all radiographs. This was standardized by using a uniform cassette size for all knee radiographs and all radiographs were taken at a distance of 72 inches away from the joint of interest.
Kellgren-Lawrence (KL) scores10 (0–4) were performed on the screening visit films. Static alignment measures were performed on the year 2 follow-up radiographs using a previously validated method.11 Anatomic alignment measures were modified to better reflect mechanical alignment subtracting a correction factor of 3.5 degrees for women and 6.4 degrees for men;11 those knees with a corrected anatomic alignment of < 178o were categorized as being varus aligned as similarly defined in other studies.12,13
Pain Assessments
The Western Ontario and McMasters University Index (WOMAC) pain questionnaire14 (Likert), a validated pain questionnaire to assess lower hip and knee pain in studies of osteoarthritis, was administered to evaluate the study knee at the year 2 follow-up visit, on the same day as the gait video recordings. The questionnaire consists of five questions, each with a potential score between 0 – 4, with 4 representing extreme pain. The weight-bearing questions included: pain on walking on a flat surface (question 1), pain on walking up and down stairs (question 2), and pain with standing upright (question 5). The non-weight bearing questions included: pain at night while in bed (question 3) and pain with sitting or lying down (question 4). The scores from all five questions were summed to give the total WOMAC pain scores.
Participant covariates
Date of birth was asked of the participants at the time of study entry and was used to ascertain their age. Sex was self-reported. Participants were weighed in kilograms (kgs) with their street clothes without their shoes utilizing Seca 770 Alpha scale. They were measured for height in meters (m) using a Holtain Stadiometer. Walk speed was ascertained by asking the participant to ambulate 20 meters at a self-selected speed on the same date that the gait video, x-ray, and WOMAC pain assessments were administered. The fastest of two trials was taken as the walk speed.
Statistical Methods
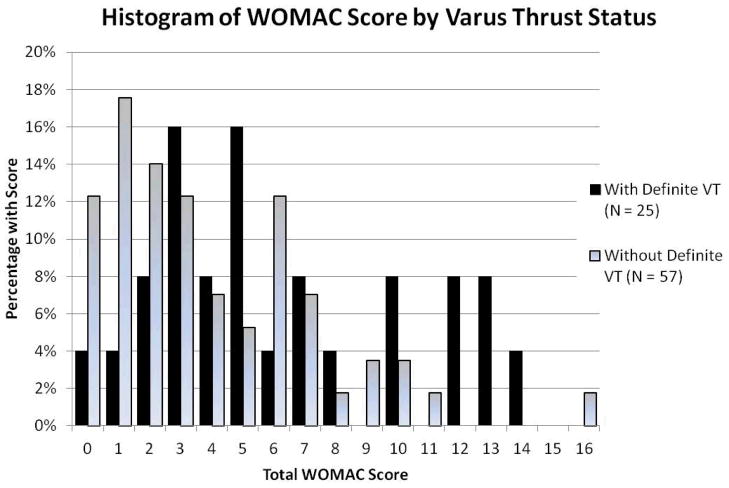
We only included the study knee identified for the parent randomized controlled trial that met the definition for symptomatic radiographic OA at baseline in the analyses. To compare the baseline demographic characteristics and radiographic OA scores of those with and without definite varus thrust, we used t-tests and chi-squared testing. We calculated means for the total WOMAC pain score grouped by with definite varus thrust versus without definite varus thrust, initially unadjusted, using t-testing to assess for statistical significance. We then calculated least squared means (LSMEANS) adjusting for age, sex, height, and weight and 20 meter walk speed. To show the distribution of the WOMAC pain score, we created a histogram of those with definite varus thrust versus without definite varus thrust.
We also performed ordinal logistic regressions with individual WOMAC pain questions as the outcomes and varus thrust as the predictor, subsequently adjusting for age, sex, height, and weight. Because few of the individual pain scores were very high, the pain scores of 2, 3 and 4 were collapsed into one level for the ordinal logistic regression models. The proportional odds assumption was checked for all models. If the test of assumptions for proportional odds test was statistically significant (e.g. meaning that the assumptions were not met) we did not present the results of those models. This is a conservative approach.15 We repeated the ordinal logistic regression using varus static alignment as the predictor. To address the possibility that the cutoff of 178 may not be optimal in the definition of varus static alignment, we performed a sensitivity analysis evaluating alternative cut offs between values of 171 – 180 degrees. All analyses were performed using SAS version 9.2.
Results
In total, 82 participants had a mean age of 65.1 (±8.5), mean BMI of 30.2 (±5.4), mean height of 1.66 m (±0.09), mean weight of 83.5 kg (±17.1), 60% were female, 31% with definite varus thrust, 18% with possible varus thrust, and 51% with absent varus thrust. 39% of the varus thrust readings required adjudication.
Those with and without definite varus thrust were similar though the group with definite varus thrust had a greater severity of radiographic OA, were slightly heavier and a larger percentage were male (Table 1). Also 84% of those with definite varus thrust has varus static alignment while only 33% of those without varus thrust had varus alignment.
Table 1.
Demographic characteristics of those with and without definite varus thrust.
| With definite varus thrust (N = 25) | Without definite varus thrust (N = 57) | P values | |
|---|---|---|---|
| Age (years) | 63.2 (±8.5) | 62.9 (±8.6) | 0.90 |
| Height (meters) | 1.68 (±0.09) | 1.65 (±0.09) | 0.20 |
| Weight (kgs) | 88.9 (±17.2) | 81.2 (±16.7) | 0.06 |
| BMI (kg/m2) | 31.4 (±5.7) | 29.7 (±5.3) | 0.18 |
| Sex | 36% female | 70% female | 0.003 |
| KL 2 | 9 (36%) | 38 (67%) | |
| 3 | 7 (28%) | 12 (21%) | 0.016 |
| 4 | 9 (36%) | 7 (12%) | |
| Varus Static Alignment | 21 (84%) | 19 (33%) | <0.0001 |
Those with versus without definite varus thrust had a total WOMAC pain score of 6.3 versus 3.9, p = 0.007. When adjusting for age, sex, height, weight and walk speed, the difference in means was less pronounced and no longer significant, 5.7 versus 4.2, p = 0.09. This difference in total WOMAC pain score subgrouped by definite varus thrust status is highlighted also in the histogram depicted in figure 1. Those with varus static alignment versus without varus static alignment had a total WOMAC pain score of 5.2 versus 4.2, p = 0.30. After adjustment for the aforementioned covariates, the difference in total WOMAC pain score was further diminished to 4.8 versus 4.5, p = 0.68.
Figure 1.
Histogram of WOMAC pain score subgrouped by definite varus thrust status.
Table 2 shows the proportional odds ratio for each WOMAC individual pain question using definite varus thrust as the predictor. The proportional odds of having pain with walking and with standing up-right in those with definite varus thrust was more than or equal to 5 times that of those without definite varus thrust.
Table 2.
Proportional odds of pain in those with v. without definite varus thrust, using the individual WOMAC pain questions to define pain.
| Individual WOMAC pain questions | Frequency of people with levels of pain stratified by varus thrust status | Unadjusted Proportional Odds Ratio for Pain with v. without definite varus thrust | *Adjusted Proportional Odds Ratio for Pain with v. without definite varus thrust | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||||
| Weight-bearing Questions | Pain with walking | With definite varus thrust | 4 | 12 | 6 | 3 | 0 | 5.0 (1.9 – 12.8) | N/Aξ |
| Without definite varus thrust | 29 | 21 | 7 | 0 | 0 | ||||
| Pain standing upright | With definite varus thrust | 4 | 8 | 9 | 4 | 0 | 5.5 (2.2 – 13.9) | 4.1 (1.5 – 11.6) | |
| Without definite varus thrust | 31 | 16 | 8 | 2 | 0 | ||||
| Pain with stairs | With definite varus thrust | 2 | 11 | 4 | 7 | 1 | N/Aξ | 1.0 (0.4 – 3.0) | |
| Without definite varus thrust | 11 | 21 | 20 | 4 | 1 | ||||
|
| |||||||||
| Non-weight-bearing Questions | Pain at night in bed | With definite varus thrust | 11 | 6 | 7 | 1 | 0 | 2.0 (0.8 – 4.9) | 2.3 (0.8 – 6.8) |
| Without definite varus thrust | 35 | 12 | 8 | 1 | 1 | ||||
| Pain sitting or lying | With definite varus thrust | 11 | 10 | 3 | 1 | 0 | 1.5 (0.5 – 3.8) | 1.3 (0.4 – 3.7) | |
| Without definite varus thrust | 34 | 13 | 8 | 1 | 1 | ||||
Denotes adjustment for age, sex, height and weight.
Using this definition of pain, the assumptions of proportional odds was not met; therefore, we did not report the proportional odds using this definition of pain.
Table 3 reports the proportional odds ratio for the individual WOMAC pain questions using varus corrected anatomic alignment as the predictor. Pain was not more likely in those with varus alignment compared to those without varus alignment using any of the 5 individual questions in either unadjusted or adjusted analyses.
Table 3.
Proportional odds of pain in those with v. without varus corrected anatomic alignment (varus was defined as a corrected anatomic angle < 178°), using the individual WOMAC pain questions to define pain.
| Individual WOMAC pain questions | Frequency of people with levels of pain stratified by varus static alignment | Unadjusted Proportional Odds Ratio for Pain with v. without varus static alignment | * Adjusted Proportional Odds Ratio for Pain with v. without varus static alignment | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||||
| Weight-bearing Questions | Pain with walking | Varus | 13 | 19 | 5 | 3 | 0 | 1.6 (0.7 – 3.5) | N/Aξ |
| No Varus | 20 | 14 | 8 | 0 | 0 | ||||
| Pain standing upright | Varus | 14 | 12 | 10 | 4 | 0 | 1.9 (0.8 – 4.3) | 1.5 (0.6 – 3.8) | |
| No Varus | 21 | 12 | 7 | 2 | 0 | ||||
| Pain with stairs | Varus | 5 | 18 | 9 | 6 | 2 | 1.0 (0.4 – 2.2) | 0.8 (0.3 – 2.1) | |
| No Varus | 8 | 14 | 15 | 5 | 0 | ||||
|
| |||||||||
| Non-weight-bearing Questions | Pain at night in bed | Varus | 23 | 7 | 7 | 2 | 1 | 1.0 (0.4 – 2.4) | 1.2 (0.5 – 3.3) |
| No Varus | 23 | 11 | 8 | 0 | 0 | ||||
| Pain sitting or lying | Varus | 24 | 10 | 4 | 1 | 1 | 0.7 (0.3 – 1.6) | 0.6 (0.2 – 1.6) | |
| No Varus | 21 | 13 | 7 | 1 | 0 | ||||
Denotes adjustment for age, sex, height, weight, and walk speed.
Using this definition of pain, the assumptions of proportional odds was not met; therefore, we did not report the proportional odds using this definition of pain.
In order to address the possibility that this choice of 178 degrees as a cutoff to define varus static alignment was appropriate, we performed a sensitivity analysis by modifying the cutoff used for the definition of varus alignment from 171 – 180. Using any of these definitions, the means for the summed WOMAC score were never statistically significantly different in those with and without varus alignment. For the individual WOMAC questions, the only analyses that were intermittently significant were those unadjusted analyses evaluating pain with walking and standing and adjusted analyses evaluating pain with sitting or lying down, presented in Table 4.
Table 4.
Sensitivity analysis showing the results for proportional odds of pain in those with v. without varus corrected anatomic alignment using different cutoff points for varus alignment. Bolded results highlight the statistically significant results.
| Static alignment Cut off (degrees) | Unadjusted Proportional Odds Ratio for Walking Pain with v. without varus static alignment | Unadjusted Proportional Odds Ratio for Standing Pain with v. without varus static alignment | *Adjusted Proportional Odds Ratio for Sitting or Lying Pain with v. without varus static alignment |
|---|---|---|---|
| 180 | 1.8 (0.8 – 4.2) | 2.6 (1.1 – 6.2) | 0.5 (0.2 – 1.4) |
| 179 | 1.3 (0.6 – 3.1) | 2.0 (0.9 – 4.7) | 0.4 (0.1 – 1.1) |
| 177 | 1.7 (0.7 – 3.8) | 1.9 (0.8 – 4.2) | 0.5 (0.2 – 1.5) |
| 176 | 1.7 (0.7 – 3.8) | 1.8 (0.8 – 4.2) | 0.5 (0.2 – 1.5) |
| 175 | 2.3 (1.0 – 5.4) | 2.4 (1.0 – 5.7) | 0.2 (0.1 – 0.7) |
| 174 | 2.9 (1.2 – 7.3) | 2.7 (1.1 – 6.6) | 0.2 (0.1 – 0.8) |
| 173 | NA | 2.4 (1.0 – 5.9) | 0.2 (0.1 – 0.8) |
| 172 | NA | 2.8 (1.1 – 7.2) | 0.3 (0.1 – 1.0) |
| 171 | NA | 2.1 (0.7 – 6.0) | 0.2 (0.04 – 1.0) |
NA = not applicable because did not meet assumptions for ordinal logistic regression.
Denotes adjustment for age, sex, height, weight, and walk speed.
Discussion
To our knowledge, our study is the first to show that in those with symptomatic knee OA, the presence of varus thrust, a measure of dynamic alignment known to be a predictor of structural progression,5,16 was associated with greater overall knee pain, specifically during weight-bearing activities. We have also illustrated that varus static alignment, also a known predictor of structural progression,7 was possibly associated with weight-bearing pain in the same study though with a much smaller effect estimate.
Of those with definite varus thrust in this study, 84% had varus static alignment while only 33% of those without definite varus thrust had varus static alignment. Although definite varus thrust and varus static alignment are clearly closely related, they do not represent the exact same construct. Varus thrust is a measure of dynamic alignment visualized during gait while varus static alignment is measured on a still radiograph. While both have been previously shown to be potent predictors of structural progression,5,7,16 highlighting the importance of biomechanics in knee OA pathophysiology; in our cross-sectional study, we found that varus thrust was more convincingly associated with pain compared with varus static alignment. Understanding the differences among those who have varus alignment who do and do not have varus thrust may provide important insights into sources of pain in knee OA. Intuitively, it is not surprising that a dynamic alignment measure would be predictive of symptoms in knee OA whereas the equivalent static alignment measure would be less so. Perhaps it is those who have greater laxity in the joint who have varus thrust which can be best measured during gait. It could also be that varus thrust is a surrogate measure of the external adduction moment, another measure of dynamic alignment which has been associated with excessive loading upon the medial compartment. Chang et al showed in a sample of 64 participants that those with varus thrust had a higher external adduction moment than those without varus thrust.5 Further, there was a recent study showing that those with an elevated external adduction moment had a higher prevalence of medial compartment bone marrow lesions visualized on MRI,17 a feature that has also been associated with knee pain.18–21
Although the definition of varus static alignment used in this study was similar to ones used in prior epidemiologic studies,12,13 in order to address the possibility that other definitions could have been more appropriate, we performed a sensitivity analysis by modifying the cutoff used for the definition of varus alignment from 171 – 180. Using any of these definitions, the summed WOMAC score subgrouped by varus alignment was not statistically significant. For the individual WOMAC questions, the unadjusted analyses evaluating pain with walking and standing showed statistical significance in the direction we expected (table 4). With modification of the static alignment definition, some of the unadjusted weight-bearing analyses showed a significant association of varus alignment with pain. Surprisingly, the point estimates for the association of varus alignment with pain using the non-weight-bearing question of “pain with sitting or lying” were less than 1, suggesting that varus alignment was protective of pain with sitting or lying. An interpretation of these findings could be that the cutoff of 178 is more appropriate since this unexpected result is not evident with this definition. Alternatively, a lower cutoff definition could be more appropriate and static alignment is associated with pain with standing but that there is some reason why participants are simultaneously less likely to develop pain with sitting or lying down. In any case, the relationship between varus static alignment and pain is substantially weaker than that of varus thrust when using a variety of cutoff definitions for varus static alignment.
Notably, the severity of radiographic knee OA was greater in those with definite varus thrust as compared with those without definite varus thrust. We did not enter KL score as a potential covariate in our adjusted model expecting that varus thrust could be a mediator in the relationship between higher KL scores being associated with knee pain. However, because there is a possibility that varus thrust may be associated with pain independently of KL score, we did perform additional analyses adding KL score to the unadjusted logistic regression models and found that varus thrust was still significantly associated with the sum of the WOMAC pain questions in addition to the individual standing and walking pain questions. These findings support that varus thrust is associated with knee pain independent of the fact that this finding is associated with more severe radiographic evidence of OA.
Although there is some doubt regarding the measurement properties of the summed WOMAC pain subscale, it is still the current OARSI recommended22 and FDA accepted outcome measure for assessment of symptoms in knee OA clinical trials. In our study, we evaluated pain by using the sum of the WOMAC pain questions and also the individual WOMAC pain questions. Doing both allowed for better characterization of the heterogenous pain that occurs in knee OA.
Varus thrust is a clinical assessment of dynamic loading that can be performed inexpensively. In our study, we used a standard video camera to record participants ambulating at a self-selected speed 20 meters away from and then towards the camera. With the adjudication of the measure between two rheumatologists who were blinded to pain assessments we did find that this measure was strongly related to the summed WOMAC pain assessment and specifically, weight-bearing pain, namely pain with walking on a flat surface and pain with standing. Because we did have a substantial number of knees that required adjudication of this reading (39%), we performed a sensitivity analysis where we restricted the analyses to only those knees that did not require adjudication. In this analysis, the results were similar with the exception that the total WOMAC pain in those with definite varus thrust versus without varus thrust (5.2 v. 3.9) was no longer statistically significant, p = 0.20, likely reflecting a loss of power with the lower number of observations though the direction of the relationship was still similar. However, the unadjusted odds ratios for the individual pain questions remained unchanged with the walking and standing analyses being statistically significant, suggesting that the association between varus thrust and pain is real.
There are limitations to our study, with an important one being that we have a relatively small sample size. It will be important to replicate our findings in a larger cohort of participants. Also, this is a cross-sectional study, limiting our ability to draw conclusions regarding whether varus thrust causes pain. Longitudinal studies will be needed to test this hypothesis. Another important limitation is that we used PA semi-flexed films, available in the parent study, to assess a corrected anatomic alignment as opposed to the accepted gold standard of using long-limb films to measure mechanical alignment as our measure of static alignment. Anatomic alignment is a valid and useful biomechanical parameter, but results could differ using true mechanical alignment.11 Therefore, there is still the possibility that static alignment assessed via mechanical alignment could be more strongly associated with knee OA pain.
Nonetheless, our study has found that there is a strong association between varus thrust and pain in those with knee OA, particularly with weight-bearing activities. This finding is not replicated when evaluating for an association of varus static alignment with pain though there was a suggestion of this possibility in our sensitivity analyses using a more stringent definition of varus alignment. The potential clinical implications of the findings of this study include that perhaps those with varus thrust are a special phenotype of OA who will selectively respond to customized biomechanical modifications. For instance, treatment of varus thrust with bracing or gait retraining may provide symptomatic relief for the group of people with this particular finding. Because varus thrust has been demonstrated to be associated with structural progression in other studies,5,23 biomechanical intervention to improve symptoms may also provide structural benefits. Therefore identification of a particular phenotype of the disease, specifically those with varus thrust, may bring us one step closer to finding an effective symptom and structure modifying treatment for knee OA.
Acknowledgments
Dr. Lo was supported by the American College of Rheumatology/Research and Education Foundation and the Arthritis Foundation through the Arthritis Investigator Award. The Randomized Controlled Trial of Vitamin D for Knee OA is supported by NIH/NIAMS (NIAMS R01 AR051361 and NIH M01 RR 00054). This work was supported in part by the Houston VA HSR&D Center of Excellence (HFP90-020).
Footnotes
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–8. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 2.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–99. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 4.Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA. Insurer and out-of-pocket costs of osteoarthritis in the US: Evidence from national survey data. Arthritis Rheum. 2009;60:3546–53. doi: 10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- 5.Chang A, Hayes K, Dunlop D, et al. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 2004;50:3897–903. doi: 10.1002/art.20657. [DOI] [PubMed] [Google Scholar]
- 6.Sharma L, Song J, Dunlop D, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940–5. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama. 2001;286:188–95. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 8.Bellamy N, Kean WF, Buchanan WW, Gerecz-Simon E, Campbell J. Double blind randomized controlled trial of sodium meclofenamate (Meclomen) and diclofenac sodium (Voltaren): post validation reapplication of the WOMAC Osteoarthritis Index. J Rheumatol. 1992;19:153–9. [PubMed] [Google Scholar]
- 9.Stratford PW, Kennedy DM, Woodhouse LJ, Spadoni GF. Measurement properties of the WOMAC LK 3.1 pain scale. Osteoarthritis Cartilage. 2007;15:266–72. doi: 10.1016/j.joca.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Kellgren JH, Lawrence JS. The epidemiology of chronic rheumatism: atlas of standard radiographs. Oxford, UK: Blackwell Scientific; 1962. [Google Scholar]
- 11.Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52:1730–5. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]
- 12.Englund M, Guermazi A, Roemer FW, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60:831–9. doi: 10.1002/art.24383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neogi T, Nevitt M, Niu J, et al. Subchondral bone attrition may be a reflection of compartment-specific mechanical load: the MOST Study. Ann Rheum Dis. 2010 doi: 10.1136/ard.2009.110114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 15.Gameroff M. Using the Proportional Odds Model for Health-Related Outcomes: Why, When, and How with Various SAS R Procedures. SAS Users Group International Conference (SUGI); 2011 April 9–13, 2011; Philadelphia. 2011. [Google Scholar]
- 16.Chang A, Hochberg M, Song J, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk for knee osteoarthritis. Arthritis Rheum. 2010 doi: 10.1002/art.27377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennell KL, Creaby MW, Wrigley TV, et al. Bone marrow lesions are related to dynamic knee loading in medial knee osteoarthritis. Ann Rheum Dis. 2010 doi: 10.1136/ard.2009.118182. [DOI] [PubMed] [Google Scholar]
- 18.Felson DT, Chaisson CE, Hill CL, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–9. doi: 10.7326/0003-4819-134-7-200104030-00007. [DOI] [PubMed] [Google Scholar]
- 19.Felson DT, Niu J, Guermazi A, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 20.Torres L, Dunlop DD, Peterfy C, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006;14:1033–40. doi: 10.1016/j.joca.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 21.Lo GH, McAlindon TE, Niu J, et al. Bone marrow lesions and joint effusion are strongly and independently associated with weight-bearing pain in knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2009;17:1562–9. doi: 10.1016/j.joca.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman R, Brandt KD, Hochberg MC, Moskowitz R. Design and conduct of clinical trials in patients with osteoarthritis: recomendations from a task force of the Osteoarthritis Research Society. Osteoarthritis and Cartilage. 1996;4:217–43. doi: 10.1016/s1063-4584(05)80101-3. [DOI] [PubMed] [Google Scholar]
- 23.Chang A, Hochberg M, Song J, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk of developing knee osteoarthritis. Arthritis Rheum. 2010;62:1403–11. doi: 10.1002/art.27377. [DOI] [PMC free article] [PubMed] [Google Scholar]