Abstract
In the EHDIC-SWB study, African-Americans are less likely to have depression than non-Hispanic whites. Religious service attendance is one possible explanation because studies have shown an inverse relationship between religious service attendance and depression. We examined the relationship between race, religious service attendance, and depression in 835 African-American and 573 non-Hispanic white adults aged 18 and older in the Exploring Health Disparities in Integrated Communities-Southwest Baltimore (EHDIC-SWB) study. Religious service attendance was measured according to participants’ response to “how often do you attend religious services?” Depression was measured using the Patient Health Questionnaire. African-Americans attended religious services more frequently than non-Hispanic whites, and had a lower percentage of depression (10.1% vs. 15.4%; p-value <0.05). After adjusting for the demographic variables and health-related characteristics, African-Americans displayed lower odds of having depression (OR = 0.68, 95% CI: 0.47–0.97) compared to non-Hispanic whites. However, when including religious service attendance in the model, we found race differences in depression (OR = 0.76, 95% CI: 0.52–1.11) were no longer significant. We concluded that among individuals living in a low-income, integrated urban environment, race disparities in depression were eliminated after accounting for race differences in religious service attendance. This suggests religious service attendance may serve as a protective factor against depression for African-Americans.
Keywords: Religious service attendance, Race, Depression
Background
Depression
Depression is a serious public health condition with a large societal burden that includes healthcare costs and years of potential life lost if it is not addressed and properly managed. In recent decades the USA has seen an increase in depression prevalence, but its impact is not uniformly distributed. The literature on race differences in depression prevalence is inconsistent. Governmental agencies such as the National Institute of Mental Health (NIMH) and some studies using nationally representative samples report that depression is less prevalent among African-Americans compared to non-Hispanic whites (hereafter referred to as whites).1–4 However, other studies show that African-Americans have a higher prevalence of depression and report greater impairment as a result.5–7 Further, the impact of depression on African-Americans may be more far reaching because they are more likely to be under diagnosed than whites and less likely than whites to seek mental health care because of potential stigma and historical mistreatment.8,9 To date most studies cite socioeconomic status,9 lack of social support, and inadequate coping mechanisms as reasons for a greater prevalence of depression among African-Americans.
The role of religion as a protective factor against depression and mental health among African-Americans has been hypothesized in studies that found that African-Americans were less likely to experience depression.10 Indeed, African-Americans have been found to be more religious than whites, but the impact of religiosity on race differences in depression is rarely empirically explored.10–14
Influence of Religious Service Attendance
Studies have shown that religiosity is associated with positive health outcomes such as less smoking, drinking, and lower blood pressure.15–17 Similar findings have reported an association between religious service attendance and lower odds of depression in African-American and white populations.18–20 Though there have been studies examining disparities in depression as well as studies examining the impact religious service attendance has on health behaviors and outcomes, little attention has been given to examining the impact of religious service attendance on depression when African-Americans and whites are living in the same environment and share similar socioeconomic status (SES). Among studies that find that African-Americans are more likely to experience depression, increased stress among African-Americans due to poverty and the environmental factors associated with lower SES such as crime or lack of agency of life circumstances are cited as potential reasons.13 The literature on religion has found that African-Americans may use religion or spirituality as a coping mechanism, particularly for stressors that may be particular to the African-American experience or poverty.11,13 By examining the association between race, depression, and religiosity among a population where African-Americans and whites share similar SES conditions, the possible race differences in stressors that are associated with depression due to differences in SES are likely mitigated.
In this study we explore one aspect of religiosity, the impact of religious service attendance on race differences in depression in African-Americans and whites who share similar contexts. We take into account that social and environmental factors may reveal important insights about the possible differences in health outcomes between African-American and white adults in the sample.21 The objective of this paper is to assess the role religious service attendance has on differences in depression among African-Americans and whites.
Methods
Population
EHDIC (Exploring Health Disparities in Integrated Communities) is an ongoing multi-site study of race disparities within communities where blacks and whites live together and where there are no race differences in SES, as measured by median income. The first EHDIC study site was in Southwest Baltimore, MD (EHDIC-SWB), a low-income urban area. Future EHDIC locations are planned.
EHDIC-SWB is a cross-sectional face-to-face survey of the adult population (aged 18 and older) of two contiguous census tracts collected between June and September 2003. In addition to being economically homogenous, the study site was also racially balanced and well integrated, with almost equal proportions of black and white residents. In the two census tracts, the racial distribution was 51% black and 44% white, and the median income for the study area was $24,002, with no race difference. The census tracts were block listed to identify every occupied dwelling in the study area. During block listing, we identified 2,618 structures. Of those, 1,636 structures were determined to be occupied residential housing units (excluding commercial and vacant residential structures). After up to five attempts, contact was made with an eligible adult in 1,244 occupied residential housing units. Of that number, 65.8% were enrolled in the study, resulting in 1,489 study participants (41.9% of the 3,555 adults living in these two census tracts recorded in the 2000 Census). Because our survey had similar coverage across each census block group included the study area, the bias to geographic locale and its relationship with socioeconomic status should be minimal.21
Comparisons to the 2000 Census for the study area indicated that the EHDIC-SWB sample included a higher proportion of blacks and women, but was otherwise similar with respect to other demographic and socioeconomic indicators.21 For instance, our sample was 59.3% black and 44.4% male, whereas the 2000 Census data showed the population was 51% black and 49.7% male. Age distributions in our sample and 2000 Census data were similar with the median age (35–44 years) for both samples. The lack of race difference in median income in the census, $23,500 (black) vs. $24,100 (white), was replicated in EHDIC $23,400 (black) vs. $24,900 (white).
The survey was administered in person by a trained interviewer and consisted of a structured questionnaire, which included demographic and socioeconomic information, self-reported height and weight, self-reported health behaviors and chronic conditions, and three blood pressure (BP) measurements. The EHDIC study has been described in greater detail elsewhere.21 The Committee on Human Research at the Johns Hopkins Bloomberg School of Public Health approved the study. These analyses included 1,408 black and white respondents from the EHDIC-SWB sample.
Outcomes
Depression was evaluated using the Patient Health Questionnaire-9 (PHQ-9).22 The PHQ-9 is a nine-item scale adapted from the three-page self-administered questionnaire. The PHQ-9 uses a Likert-type scale with four possible responses (1 = not at all, 2 = several days, 3 = more than half the days, 4 = nearly every day). Answering “more than half the days” or “nearly every day” on four or more of the questions (including at least one of two questions: “little interest or pleasure in doing things” or “feeling down, depressed, or hopeless”) was classified as having depressive syndrome. Answering “more than half the days” or “nearly every day” on five or more of the questions (including at least one of two questions: “little interest or pleasure in doing things” or “feeling down, depressed, or hopeless”) was categorized as having major depression.
The PHQ-9’s construct validity and reliability was examined in a 2001 study conducted by Kroenke, Spitzer, and Wiliams, in which they concluded that evidence from two studies totaling 6,000 patients supported the validity and reliability of the PHQ-9. Furthermore, they argued, the “brevity coupled with its construct and criterion validity makes the PHQ-9 an attractive, dual-purpose instrument for making diagnoses and assessing severity of depressive disorders.”23 Participants in our study who were identified as having either depressive syndrome or major depression were combined to create one dichotomous depression variable that was used in the logistic regression models.
Main Independent Variables
Race was based on the participant’s self-identification as African-American or white (n = 1,408), which was 95% of the study population.
Religious service attendance was based on responses to the item, “how often do you go to religious services?” Responses include “never,” “once or twice a year,” “every month or so,” “once or twice a month,” “every week or more often,” and “more than once a week.” Religious service attendance was measured continuously.
Covariates
Other covariates included demographic variables and health-related characteristics. Demographic variables included: age, income, female sex, married or living as married, and highest education level completed. Both age and income were evaluated as continuous variables. Female sex was coded as a dichotomous variable. A binary variable was created to classify individuals who reported being married or living as married. Three binary variables measured a participant’s level of educational attainment (< 12 years of school, high school graduate/GED, and more than high school).
Health-related characteristics included: any chronic disease, obesity, self-rated health, drinking, and smoking status. Any chronic disease was ascertained by participants’ responding yes to having at least of the following: hypertension, heart disease or heart attack, cancer, stroke, diabetes, or breathing problems. Obesity was defined as self-reported body mass index of 30 or higher. A binary variable was created to identity those individuals who rated their health as fair or poor. Drinking and smoking status were both categorized into three groups: former, current, or never.
Statistical Analysis
The mean and proportional differences between racial categories for the demographic and health-related characteristics were evaluated using Student’s t for continuous variables and chi-square tests for categorical variables. The odds of depression were specified using step-wise multiple logistic regression models to determine the influence of each group of variables on the association between race and depression. In each model we add a set of covariates to the previous model grouped as follows: model 1—age-adjusted only, model 2—demographic variables and health-related characteristics, and model 3—religious service attendance. All tests were two-sided, and p-values < 0.05 were considered significant. Statistical analysis was performed using Stata 11 (Stata Corp, College Station, TX, USA).
Results
Table 1 displays the demographic and health-related characteristics of the EHDIC-SWB participants by race. African-Americans, on average, were younger and had lower incomes than whites, but were more likely to be a high school graduate or GED recipient, and less likely to be married. Health-related characteristics show that fewer African-Americans reported poor or fair health compared to whites, while more African-Americans reported being current drinkers or never smoking. African-Americans demonstrated higher rates of religious service attendance. This is particularly evident in those who reported attending once or twice a month or more frequently compared to whites. African-Americans also exhibited a lower percentage of people who never attended religious services and a lower percentage of depression than whites.
Table 1.
Distribution of demographic and health-related characteristics of the EHDIC-SWB participants by race
| Variable | Non-Hispanic whites (n = 573) | African-Americans (n = 835) |
|---|---|---|
| Age (years), mean ± SD | 42.6 ± 16.2 | 37.5 ± 13.3* |
| Female (%) | 56.9 | 54.4 |
| Married/living as married (%) | 24.1 | 14.1* |
| Education (%) | ||
| Less than HS graduate | 47.5 | 35.4* |
| HS diploma/GED | 34.2 | 45.1* |
| Education beyond HS | 18.3 | 19.5 |
| Income (dollars), mean ± SD | 24,816.76 ± 23,414.73 | 23,471.20 ± 32,485.74* |
| Any chronic disease (%) | 54.6 | 42.6* |
| Obesity (%) | 29.9 | 32.1 |
| Poor/fair health (%) | 37.4 | 28.2* |
| Drinking status (%) | ||
| Never drink | 16.6 | 20.5 |
| Former drinker | 40.4 | 31.1* |
| Current drinker | 43.0 | 48.4* |
| Smoking status (%) | ||
| Never smoke | 15.5 | 22.6* |
| Former smoker | 10.5 | 6.6* |
| Current smoker | 74.0 | 70.8 |
| Religious service attendance (%) | ||
| Never | 47.9 | 24.0* |
| Once or twice a year | 19.3 | 19.3 |
| Every month or so | 6.5 | 8.6 |
| Once or twice a month | 8.3 | 17.7* |
| Every week or more often | 13.4 | 20.3* |
| More than once a week | 4.6 | 10.1* |
| Depression | 15.4 | 10.1* |
Any chronic disease is based on participant report of being diagnosed with at least one of the following: hypertension, heart disease or heart attack, cancer, stroke, diabetes or sugar diabetes, or breathing problems such as asthma or emphysema
*p < 0.05
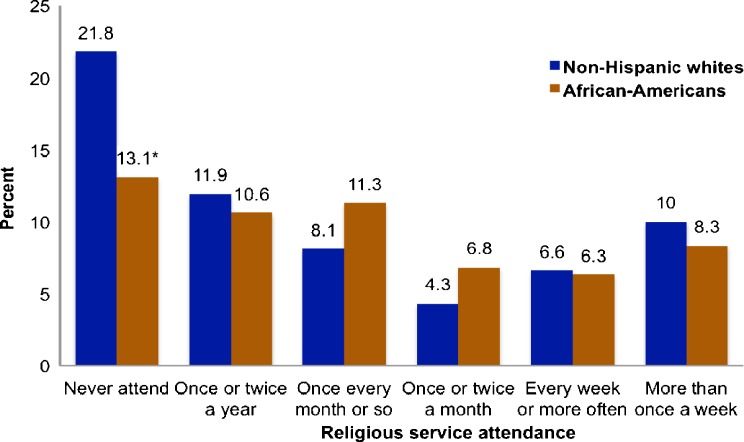
Figure 1 displays the distribution of depression by religious service attendance and race. Among those who never attended religious services, fewer African-Americans reported depression (13.1% v. 21.8%; p < 0.05) compared to whites. There were no race differences in depression in any other religious service attendance group.
Figure 1.
Distribution of depression by religious service attendance and race.
Table 2 shows the association between race and depression. When adjusting for age in model 1, African-Americans exhibited lower odds of depression relative to whites (OR = 0.62, 95% CI = 0.45–0.85). After adjusting for demographic variables and health-related characteristics in model 2, African-Americans continued to display lower odds of depression compared to whites (OR = 0.68, 95% CI = 0.47–0.97). However, when including religious service attendance in the model, race differences in depression were no longer significant (OR = 0.76, 95% CI = 0.52–1.11).
Table 2.
The association between race and depression in the EHDIC-SWB study
| Independent variable | Model 1 (n = 1,405) | Model 2 (n = 1,375) | Model 3 (n = 1,363) |
|---|---|---|---|
| African-American | 0.62 (0.45–0.85) | 0.68 (0.47–0.97) | 0.76 (0.52–1.11) |
| Age | 1.00 (1.00–1.02) | 1.00 (0.98–1.00) | 1.00 (0.98–1.01) |
| Female | 1.46 (1.01–2.10) | 1.53 (1.06–2.21) | |
| Married/living as married | 0.92 (0.57–1.47) | 0.88 (0.54–1.43) | |
| Education level | |||
| Less than HS graduate | 1.00 | 1.00 | |
| HS graduate/GED | 0.79 (0.54–1.16) | 0.82 (0.56–1.22) | |
| More than HS graduate/GED | 0.75 (0.43–1.33) | 0.79 (0.44–1.42) | |
| Income | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | |
| Any chronic disease | 1.49 (1.00–2.20) | 1.51 (1.01–2.25) | |
| Poor/fair health | 3.22 (2.22–4.66) | 3.08 (2.11–4.48) | |
| Obese | 0.96 (0.66–1.39) | 1.00 (0.68–1.46) | |
| Drinking status | |||
| Never drink | 1.00 | 1.00 | |
| Former drinker | 1.16 (0.68–2.00) | 1.13 (0.66–1.95) | |
| Current drinker | 1.14 (0.65–2.00) | 1.07 (0.60–1.89) | |
| Smoking status | |||
| Never smoke | 1.00 | 1.00 | |
| Former smoker | 0.80 (0.34–1.84) | 0.72 (0.30–1.72) | |
| Current smoker | 1.68 (0.93–3.03) | 1.61 (0.89–2.92) | |
| Religious service attendance | 0.87 (0.78–0.98) |
Any chronic disease is based on participant report of being diagnosed with at least one of the following: hypertension, heart disease or heart attack, cancer, stroke, diabetes or sugar diabetes, or breathing problems such as asthma or emphysema
Discussion
We examined the association between race, depression, and religious service attendance in a low-income urban, integrated community. In EHDIC-SWB, whites have a higher rate of depression than African-Americans, while African-Americans have greater religious service attendance. Using multiple logistic regression models, we found that religious service attendance explained the race differences in depression in EHDIC-SWB.
Studies show that African-Americans attend religious services more frequently than whites.24,25 Similarly, sociologists and other scholars whose research falls under African-American studies have explored the role of black churches in the social as well as spiritual lives of African-Americans.26,27 In EHDIC-SWB, African-Americans attend religious services more frequently than whites, which is consistent with what literature suggests about religious service attendance among African-Americans.
The act of attending a religious service in itself is not an adequate explanation for lower depression among African-Americans in the EHDIC-SWB study. In order to understand why religious service attendance is associated with lower odds of depression, it is important to explore what is being taken from religious service attendance. Frequently attending religious services is associated with greater social support, and frequent attendance suggests that the religious organization may serve as an important social body within an individual’s life. In particular and historically, African-American congregations sponsor more social service programs and provide more health information and crisis intervention than white congregations.28–30
In EHDIC-SWB, the additional health-promoting benefits of increased church attendance among African-Americans explained increased depression prevalence among whites. The mental health benefits of frequent church attendance could be direct such as the experience of being a part of an entity or church family. Those who belong to not only religious organizations, but the most involved religious organizations, sometimes experience better mental health outcomes, including lower odds of depression and lower rates of suicide.31 Furthermore, the increased social support experienced by frequent attendees may be associated with lower odds of depression as well. The design of the EHDIC study provides a unique opportunity to explore differences in depression among whites and blacks after controlling for social context. While we explore the association between depression and religious service attendance, we were not able to account for other variables that are associated with depression such as work-related stress or terminal illness. As previously mentioned, latent variables associated with regular church attendance are likely to be associated with better health and lower odds of depression; however, a limitation of this study is that only frequency of attendance was measured. In spite of this, several studies have demonstrated the positive association between health and religiosity using only religious service attendance as a measure of religiosity.32–34 Because the study was conducted in a low-income urban context, the generalizability of the results is limited to such communities. It is also not known if our results would differ in a higher-income or non-urban environment. Further, examining the relationship between depression and religious service attendance in other racial ethnic groups living under similar social and environmental conditions would be an avenue for additional research. The data presented in this paper is cross-sectional, and therefore a causal inference cannot be made. It is believed, however, that this study will contribute to better understanding how religious service attendance and ideally the inclusion of other religiosity and spirituality dimensions impact differences in depression between whites and African-Americans. The implications of these findings are important to future research on other unaddressed effects of religion, as well as to intervention activities that may facilitate culturally relevant mental health screening and treatment and positive well-being, particularly in the lives of those who espouse a religious orientation.
Acknowledgments
This research was supported by grant# P60MD000214-01 from the National Center on Minority Health and Health Disparities (NCMHD) of the National Institutes of Health (NIH), a grant from Pfizer, Inc., and grant# 5U50MN325127 from the Centers for Disease Control.
References
- 1.Blazer D, Kessler R, McGonagle K, Swartz M. The pravlence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 2.Kessler R, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 3.Kessler R, McGonagle K, Zhao S, et al. Lifetime and 12-month prevalence of comorbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 4.Weissman M, Bruce M, Leaf P, Florio L, Holzer C. Affective disorders. In: Robins L, editor. Pschiatric Disorders in America. New York, NY: Free Press; 1991. pp. 53–80. [Google Scholar]
- 5.Ostrove JM, Feldman P, Adler NE. Relations among socioeconomic status indicators and health for African-Americans and whites. J Health Psychol. 1999;4(4):451–463. doi: 10.1177/135910539900400401. [DOI] [PubMed] [Google Scholar]
- 6.Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. J Gerontol Ser B Psychol Sci Soc Sci. 2005;60(2):S93–S101. doi: 10.1093/geronb/60.2.S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 8.Probst J, Laditka S, Moore C, Harun N, Powell M. Race and ethnicity differences in reporting of depressive symptoms. Adm. Policy Ment. Health Ment Health Serv Res. 2007;34(6):519–529. doi: 10.1007/s10488-007-0136-9. [DOI] [PubMed] [Google Scholar]
- 9.Walsemann KM, Gee GC, Geronimus AT. Ethnic differences in trajectories of depressive symptoms: disadvantage in family background, high school experiences, and adult characteristics. J Health Soc Behav. 2009;50(1):82–98. doi: 10.1177/002214650905000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferraro KF, Koch JR. Religion and health among black and white adults: examining social support and consolation. J Sci Study Relig. 1994;33(4):362–375. doi: 10.2307/1386495. [DOI] [Google Scholar]
- 11.Chatters L, Taylor R, Jackson JS, Lincoln KD. Religious coping among African Americans, Caribbean blacks, and non-Hispanic whites. J Community Psychol. 2008;36(3):371–386. doi: 10.1002/jcop.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levin JS, Taylor R, Chatters LM. Race and gender differences in religiosity among older adults: findings from four national surveys. J Gerontol. 1994;49(3):S137–S145. doi: 10.1093/geronj/49.3.s137. [DOI] [PubMed] [Google Scholar]
- 13.Pargament KL. The Psychology of Religion and Coping: Theory, Research, and Practice. New YorkYork, NY: Guilford; 1997. [Google Scholar]
- 14.Taylor R, Chatters L, Jackson JS. Correlates of spirituality among African Americans and Caribbean blacks in the United States: findings from the National Survey of American Life. J Black Psychol. 2009;35(3):317–342. doi: 10.1177/0095798408329947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bell C, Bowie J, Thorpe R. The interrelationship between hypertension and blood pressure, attendance at religious services, and race/ethnicity. J Relig Health. 2010:1–13. [DOI] [PMC free article] [PubMed]
- 16.Gillum R, Dupree N. Religiousness, health, and health behavior in public-use data of the National Center for Health Statistics. J Relig Health. 2007;46(1):155–165. doi: 10.1007/s10943-006-9083-0. [DOI] [Google Scholar]
- 17.Hill TD, Burdette AM, Ellison CG, Musick MA. Religious attendance and the health behaviors of Texas adults. Prev Med. 2006;42(4):309–312. doi: 10.1016/j.ypmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Baetz M, Griffin R, Bowen R, Koenig HG, Marcoux E. The association between spiritual and religious involvement and depressive symptoms in a Canadian population. J Nerv Ment Dis. 2004;192(12):818–822. doi: 10.1097/01.nmd.0000146735.73827.85. [DOI] [PubMed] [Google Scholar]
- 19.Ellison CG, Flannelly KJ. Religious involvement and risk of major depression in a prospective nationwide study of African American adults. J Nerv Ment Dis. 2009;197(8):568–573 510.1097/NMD.1090b1013e3181b1008f1045. [DOI] [PubMed]
- 20.Olphen J, Schulz A, Israel B, et al. Religious involvement, social support, and health among African-American women on the east side of Detroit. J Gen Intern Med. 2003;18(7):549–557. doi: 10.1046/j.1525-1497.2003.21031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.LaVeist T, Thorpe R, Bowen-Reid T, et al. Exploring health disparities in integrated communities: overview of the EHDIC study. J Urban Health. 2008;85(1):11–21. doi: 10.1007/s11524-007-9226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JBW. Group at PHQPCS. Validation and utility of a self-report version of PRIME-MD. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunt LL, Hunt MO. Race, region, and religious involvement: a comparative study of whites and African Americans. Soc Forces. 2001;80(2):605–631. doi: 10.1353/sof.2001.0098. [DOI] [Google Scholar]
- 25.Taylor RJ, Chatters LM, Jayakody R, Levin JS. Black and white differences in religious participation: a multisample comparison. J Sci Study Relig. 1996;35(4):403–410. doi: 10.2307/1386415. [DOI] [Google Scholar]
- 26.Taylor RJ, Chatters ALM. Religious life of black Americans. In: Jackson JS, editor. Life in Black America. Newbury Park, CA: Sage; 1991. pp. 105–123. [Google Scholar]
- 27.Lincoln CE, Mamiya LH. The Black Church in the African American Experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- 28.Ellison CG. Religion, health, and well-being among African Americans. Afr Am Res Perspect. 1998;4:65–84. [Google Scholar]
- 29.Ortega ST, Crutchfield RD, Rushing WA. Race differences in elderly personal well-being. Res Aging. 1983;5(1):101–118. doi: 10.1177/0164027583005001006. [DOI] [Google Scholar]
- 30.Taylor RJ, Chatters LM. Church members as a source of informal social support. Rev Relig Res. 1988;30(2):193–203. doi: 10.2307/3511355. [DOI] [Google Scholar]
- 31.Pescosolido B, Georgianna S. Durkheim, suicide, and religion: towards a network theory of suicide. Am Sociol Rev. 1989;54(1):33–48. doi: 10.2307/2095660. [DOI] [PubMed] [Google Scholar]
- 32.Gillum RF, Ingram DD. Frequency of attendance at religious services, hypertension, and blood pressure: the third national health and nutrition examination survey. Psychosom Med. 2006;68(3):382–385. doi: 10.1097/01.psy.0000221253.90559.dd. [DOI] [PubMed] [Google Scholar]
- 33.Graham TW, Kaplan BH, Cornoni-Huntley JC, James SA, Becker C, Hames CG, et al. Freqeuncy of church attendance and blood pressure elevation. J Behav Med. 1978;1(1):37–43. doi: 10.1007/BF00846585. [DOI] [PubMed] [Google Scholar]
- 34.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87(6):957–961. doi: 10.2105/AJPH.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]