Abstract
Objective
Owing to the shortcomings of clinical examination and radiographs, injury to the syndesmotic ligaments is often misdiagnosed. When there is no indication requiring that the fractured ankle be operated on, the syndesmosis is not tested intra-operatively, and rupture of this ligamentous complex may be missed. Subsequently the patient is not treated properly leading to chronic complaints such as instability, pain, and swelling. We evaluated three fracture classification methods and radiographic measurements with respect to syndesmotic injury.
Materials and methods
Prospectively the radiographs of 51 consecutive ankle fractures were classified according to Weber, AO-Müller, and Lauge-Hansen. Both the fracture type and additional measurements of the tibiofibular clear space (TFCS), tibiofibular overlap (TFO), medial clear space (MCS), and superior clear space (SCS) were used to assess syndesmotic injury. MRI, as standard of reference, was performed to evaluate the integrity of the distal tibiofibular syndesmosis. The sensitivity and specificity for detection of syndesmotic injury with radiography were compared to MRI.
Results
The Weber and AO-Müller fracture classification system, in combination with additional measurements, detected syndesmotic injury with a sensitivity of 47% and a specificity of 100%, and Lauge-Hansen with both a sensitivity and a specificity of 92%. TFCS and TFO did not correlate with syndesmotic injury, and a widened MCS did not correlate with deltoid ligament injury.
Conclusion
Syndesmotic injury as predicted by the Lauge-Hansen fracture classification correlated well with MRI findings. With MRI the extent of syndesmotic injury and therefore fracture stage can be assessed more accurately compared to radiographs.
Keywords: Radiograph, Magnetic resonance imaging, Ankle, Fracture, Syndesmosis
Introduction
Treatment of ankle fractures is determined by several factors such as patient age, soft tissue status, dislocation of the fracture, and integrity of the distal tibiofibular syndesmosis. As the major stabilizer of the distal tibiofibular joint, the ligamentous complex of the syndesmosis is critical in maintaining normal ankle function. The lateral malleolus of the fibula is firmly held in the fibular notch of the tibia, providing a tight elastic ankle mortise. There are four syndesmotic ligaments: the anterior distal tibiofibular ligament (ATIFL) and posterior distal tibiofibular ligament (PTIFL), which attach the anterior and posterior tibial and fibular tubercles, respectively, and the interosseous ligament (IOL), which is the thickened continuation of the interosseous membrane (IOM), and the transverse ligament extending between the malleolar fossa of the fibula and the dorsal rim of the distal tibia [1–4].
The classification of malleolar fractures constitutes the basis for treatment of acute ankle fractures. Three frequently used methods to describe ankle fractures are the Danis-Weber, AO-Müller, and Lauge-Hansen fracture classifications [5–7]. According to Weber and AO-Müller, a fracture is classified based on the level of the fibular fracture in relation to the syndesmotic ligaments. Lauge-Hansen describes the trauma mechanism of ankle fractures, based on the position of the foot at the time of injury and the direction in which the talus moves within the ankle mortise.
Additionally a number of radiographic parameters are used to evaluate the integrity of the syndesmotic and deltoid ligaments. Absence of tibiofibular overlap (TFO) at one side and a tibiofibular clear space (TFCS) larger than 6 mm may be an indication of syndesmotic injury [8–10]. A medial clear space (MCS) surpassing the tibial clear space (TCS) is indicative of deltoid injury, which regularly accompanies injury of the syndesmosis [10].
As it is difficult to assess injury to the syndesmosis on radiographs, the true incidence is a matter of speculation. Owing to the shortcomings of clinical examination and radiographs [2, 11], injury to the syndesmotic ligaments is often misdiagnosed. Subsequently the patient is not treated properly, leading to chronic complaints such as instability, pain, swelling, and early osteoarthritis [12, 13]. MR imaging enables identification of syndesmotic injuries that were not diagnosed at the initial radiographs and clinical examination [14–17].
The primary goal of this study was to correlate three common clinical fracture classification systems with MR findings, regarding injury of the syndesmosis in acute ankle fractures. Secondary goals were to determine the correlation between the radiographic measurements and fracture treatment in relation to syndesmotic injury.
Materials and methods
In a prospective study, between April 2004 and February 2007, 51 consecutive skeletally mature patients with an acute ankle fracture, who underwent radiographs as well as an MRI at the Erasmus University Medical Center in Rotterdam within 48 h of trauma, were included. Exclusion criteria were associated neurological or vascular injuries, fractures that were associated with a hindfoot or midfoot fracture, a former trauma of the ankle, contraindications for MRI, and an insufficient knowledge of the Dutch language. Informed consent was obtained, and the study was approved by the institutional review board.
Radiographs obtained at presentation included anteroposterior, lateral, and mortise views. The fractures on the radiographs were classified according to the Weber, AO-Müller, and Lauge-Hansen fracture classification systems [5–7]. Both the fracture type and additional measurements of the TFCS, TFO, and MCS/SCS ratio were used to assess possible syndesmotic injury on a radiograph (Fig. 1). The TFCS is the horizontal distance between the posterolateral border, the anterolateral border, or the incisura fibularis of the tibia and the medial border of the fibula. The TFO is the horizontal distance between the medial border of the fibula and the lateral border of the anterior tubercle and was measured at 1 cm above and parallel to the tibial plafond. The MCS is the widest distance between the medial border of the talus and the lateral border of the medial malleolus and was measured 0.5 cm beneath the talar dome, on a line parallel to the superior talar joint surface. The SCS was the vertical distance between the talar dome and the tibial plafond (Fig. 1) [8, 9, 18–22]. A TFCS larger than 6 mm, the absence of tibiofibular overlap (TFO < 0 mm), an MCS/SCS ratio larger than 1, or an MCS larger than 4 mm was considered deviated and indicative for possible syndesmotic injury. The radiographs were blinded for identity and evaluated by a radiologist with 11 years of experience in musculoskeletal radiology (J.H.). For the Weber and AO-Müller fracture classification, expected syndesmotic injury was determined by the fracture type in combination with the measurements. For the Lauge-Hansen fracture classification, expected syndesmotic injury was based on the trauma mechanism deduced from the radiographs.
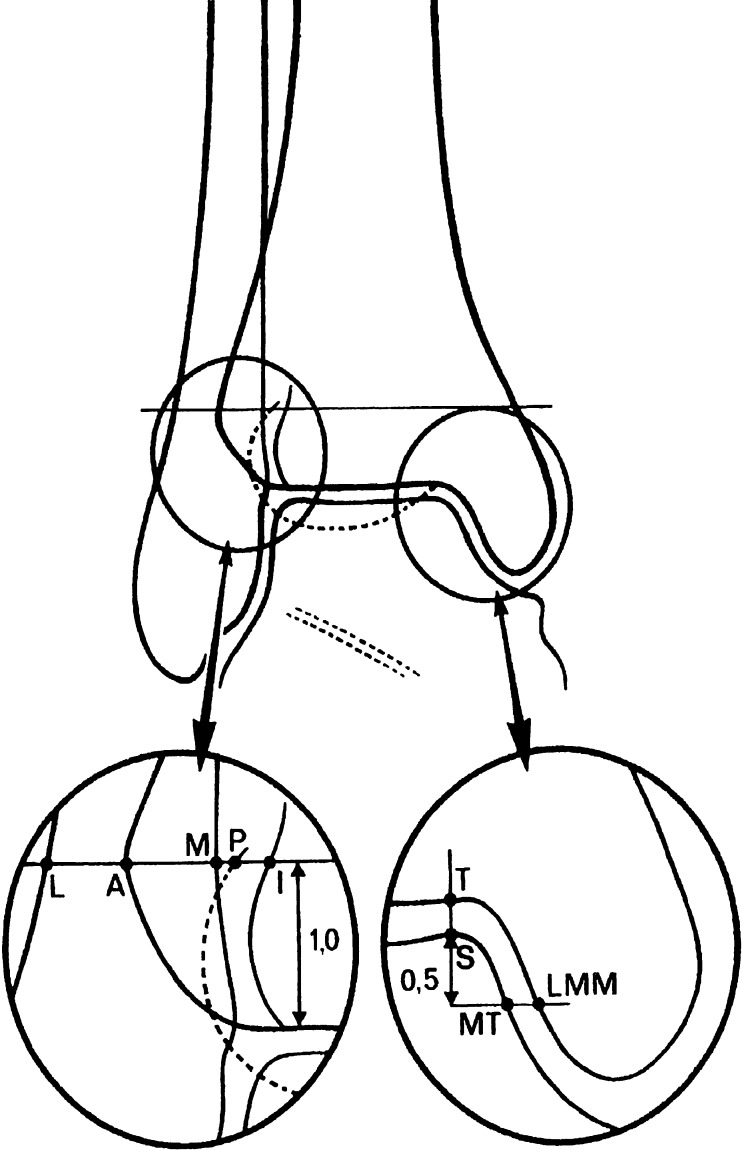
Fig. 1.
A schematic drawing of the ankle shows landmarks used for measurements of the different radiologic parameters. L Lateral border of the fibula, M medial border of the fibula, A anterior tibial tubercle, P posterior tibial tubercle, I floor of incisura fibularis, T tibial plafond, S superior point of medial talus, MT medial side of talus, LMM lateral side medial malleolus. AM is tibiofibular overlap (TFO). MI is tibiofibular clear space (TFCS). TS is superior clear space (SCS) and MTLMM is medial clear space (MCS). (Used with permission from A. Beumer, Clin. Orthop. Rel. Res 2004;423:227–234)
MRI was performed on a 1.5 T Gyroscan (Philips, Best, Netherlands) with a wrap-around ankle coil (E1 coil). The foot was kept in a fixed (neutral) position and stabilized with sandbags or a plaster. Dual TSE images (TR = 3,500–4,500 ms, TE = 11 ms, TE = 120 ms, echo train length = 14) were performed in three orthogonal planes, i.e. ,axial, coronal, and sagittal, and in an additional 45° oblique plane. The oblique image plane was defined in the coronal and sagittal views. In the coronal view, the 45° angle of the oblique plane was related to the tibial plafond and ran in a caudal-cranial and lateral-medial direction through the distal fibula. In the sagittal view, the direction of the oblique plane ran parallel to a line along the inferior border of the anterior and posterior tibia [23]. All series were performed with a 512 × 512 matrix. The field of view was 18–20 cm for coronal and sagittal imaging and 12–15 cm for axial and oblique imaging. The slice thickness of the images was 3.0 mm with an NSA of 2. For cartilage analysis, a sagittal T1 FFE (TE 20 ms, TR 7.8 ms, flip angle 25°), with an FOV of 15 cm, matrix 512 × 243, slice thickness of 3.0 mm with 1.5 mm overlap, and NSA = 2 was performed. A STIR, i.e., a short tau inversion recovery image (TR = 1,460 ms, TE = 15 ms, echo train length = 14), was performed in the coronal plane, with a field of view of 18–20 cm, a slice thickness of 4 mm (gap 0.4 mm) and a 256 × 256 matrix.
The MR images were independently analyzed by two radiologists with 11 and 31 years of musculoskeletal experience, respectively, and finally read in consensus (J.H., A.G.). They were blinded to the results of the radiographs. The majority of the patients were examined with MRI on the day of injury. Nineteen patients were treated with an open reduction with internal fixation (ORIF), of whom six underwent an MRI postoperatively. In all patients an MRI was obtained within 7 days after starting treatment, either plaster or surgery.
The presence of anterior or posterior syndesmotic injury was defined as follows: 0 = normal syndesmosis, i.e., normal ligament without bony avulsion; 1 = thickened syndesmosis, i.e., thickened ligament without bony avulsion; 2 = partially ruptured syndesmosis, i.e., partially ruptured ligament without bony avulsion; 3 = completely ruptured syndesmosis, i.e., ruptured ligament without a bony avulsion or an intact ligament with a bony avulsion. The anterior and posterior distal tibiofibular ligaments were evaluated in both the axial and oblique planes. A normal distal tibiofibular ligament consisted of multiple continuous thin fibers interspersed with normal high signal intensity fat on dual TSE-weighted images. In a thickened ligament the continuous fibers were thickened, not sharp, and the signal intensity of fat was intermediate on dual TSE-weighted images. A complete rupture was defined when the ligament was either discontinuous or invisible, or showed increased signal intensity with fluid in the ligament on T2-weighted TSE images. In a partially ruptured ligament, the discontinuity was not complete [14, 17, 23–25]. A tibial or fibular avulsion, both anteriorly and posteriorly, was evaluated as either present or absent. Posteriorly a fracture of the malleolus tertius, irrespective of its size, was defined as an avulsion. The interosseous and transverse ligaments were evaluated as follows: 0 = normal, 1 = thickened, 2 = partially ruptured, or 3 = completely ruptured.
The treatment plan, made by the surgeon, was based on the radiographs, without knowledge of MRI findings, and was denoted as follows: 0 = plaster, 1 = open reduction and internal fixation (ORIF) without setscrew, or 2 = ORIF with setscrew.
With MRI as gold standard, the sensitivity and specificity in assessing syndesmotic injury with the Weber, AO-Müller, and Lauge-Hansen fracture classifications were calculated. Correlation between the MCS-SCS ratio and deltoid ligament injury, as well as the correlation between the TFCS and TFO and syndesmotic injury were analyzed with the Mann-Whitney U test. All analyses were conducted using SPSS (version 15.0, SPSS, Chicago, IL, USA). A two-sided p-value < 0.05 was considered statistically significant.
Results
In total 51 patients were included with a mean age of 37 years and a range of 16–62 years; 28 were men and 23 were women. In 27 patients the injury involved the left and in 24 the right ankle. In six patients the MRI was performed postoperatively: within 2 days of the injury in five and after 7 days in one patient. The six patients who underwent an MRI after surgery received OSM consisting of a fibular plate with screws and/or screws in the medial malleolus. Presence of a plate and screws resulted in only minor local artifacts that did not prohibit the evaluation of the syndesmotic ligaments or deltoid ligaments. The other 45 patients underwent an MRI before treatment was started. Treatment consisted of a plaster in 32 patients, and ORIF with or without a setscrew in 6 and 13 patients, respectively.
Syndesmotic injury on MRI
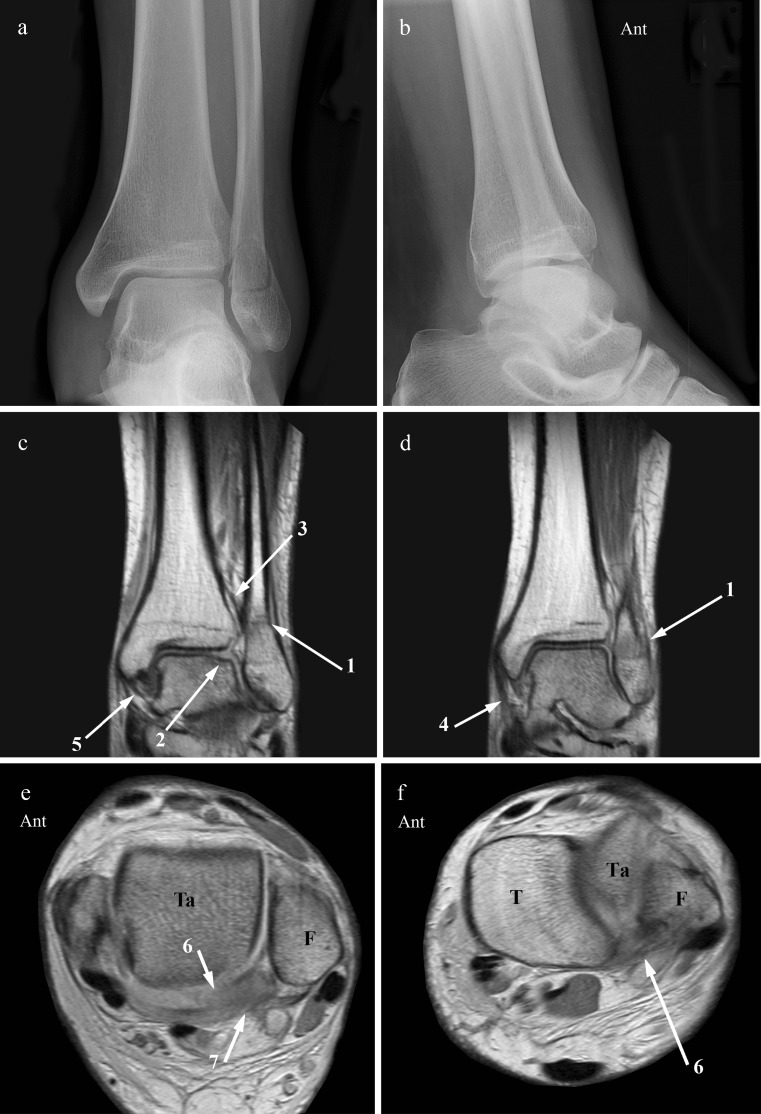
Syndesmotic injury consisted of either a rupture of the distal tibiofibular ligament or an intact tibiofibular ligament with a bony avulsion from either the tibia or fibula. Anteriorly, the distal tibiofibular ligament was ruptured in 27 patients and intact but associated with a fibular avulsion in 8 patients and with a tibial avulsion in 1. On the radiographs, however, only the tibial avulsion and three of eight fibular avulsion fractures were visible. Posteriorly, the distal tibiofibular ligament was ruptured in three patients. An intact ligament associated with an avulsion fracture occurred in 18 patients, but only at the tibia, and was defined as any size of posterior malleolus fracture. The posterior malleolus fracture was not visible on the radiographs in 6/18 patients, although it involved a large posteromedial fragment in 3. Injury of the posterior syndesmosis occurred only in combination with anterior injury (n = 21) (Fig. 2).
Fig. 2.
AP (a) and lateral (b) radiographs show an oblique fibula fracture (1), running from anteroinferior to posterosuperior, characteristic of a supination-external rotation injury. The medial malleolus (2) and posterior malleolus (3) are avulsed. AP (c) and lateral (d) radiographs after open reduction and internal fixation without a setscrew. The fracture of the posterior malleolus (3) is visible and not fixated. The fracture was classified as Weber type C, AO-Müller C2.3, Lauge-Hansen SE4. Coronal (e), 45° oblique (f, g), and axial proton-density-weighted (h) MR image. The coronal MRI shows the laterally dislocated talus, with a distal fibula fracture (1) and an avulsion fracture of the medial malleolus (2) attached to a thickened but intact superficial deltoid ligament (4). In f, the ATIFL (5) is ruptured, whereas the PTIFL (6) is intact and attached to an avulsion fracture of the posterolateral malleolus (3). In g, the ruptured interosseous ligament (7) is visible. In h, the fibula fracture (1) runs proximal to the interosseous membrane (8), which has a small tibial avulsion (9) up to this level. Ant Anterior, T tibia, F fibula
The interosseous ligament was injured in seven patients, and in six of seven patients showed intact fascicles with an avulsed periost from its tibial attachment. The interosseous ligament was ruptured in three patients in association with a ruptured anterior syndesmosis and in three patients with a ruptured anterior as well as posterior syndesmosis. In one patient it involved a ruptured interosseous ligament in combination with only a fracture of the medial malleolus. The transverse ligament was completely ruptured in one patient with only anterior syndesmotic injury (Fig. 3) and partially ruptured in another with both anterior and posterior syndesmotic injury.
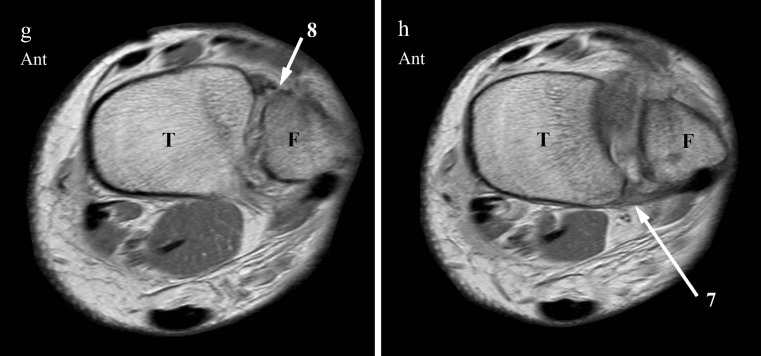
Fig. 3.
AP (a) and lateral (b) radiographs. Short distal fibula fracture (1) extending from just below to just above the level of the tibiotalar joint line. Measurements are normal. This fracture is classified as Weber type B, AO-Müller type B1.1, and Lauge-Hansen SE2. Coronal (c, d), axial (e) and 45° oblique (f, g, h) proton-density-weighted MR images. The coronal MRI (c, d) shows the fibula fracture (1), a posterolateral osteochondral lesion of the talar dome (2), a normal interosseous ligament (3), a thickened superficial (4), and a normal deep (5) deltoid ligament. On the axial (e) and oblique MR image (f), the transverse ligament (6) is ruptured. The PTIFL (7) appears to be ruptured in the axial plane (e) but is still continuous, although thickened, in the 45° oblique plane (h). The ATIFL (8) is ruptured (g). With the MRI findings, this would change the fracture into an AO-Müller type B1.2, but it would still be Lauge-Hansen SE2. Ant Anterior, Ta talus, T tibia, F fibula
The interosseous membrane (IOM) was intact in 39 patients, and its integrity could not be determined in 1. The IOM was injured in 11 patients, with a rupture in 4 and intact but attached to an avulsion of tibial periost in 7 patients. Both findings were interpreted as a rupture of the membrane. In 8 of 11 cases the rupture of the interosseous membrane was above the level of the fibula fracture and involved, in the majority, a supination-external rotation trauma (n = 7). In 3 of 11 cases with a ruptured membrane at or below the level of the fibula fracture, it involved a pronation-external-rotation trauma in 2.
Weber and AO-Müller fracture classification
Based on the Weber classification, 11 (21.6%) fractures were classified as type A, 23 (45.1%) as type B, and 11 (21.6%) as type C (Table 1). Six fractures (11.8%) could not be classified and involved either a solitary fracture of the medial malleolus with unknown status of the lateral collateral ligaments or a tibial avulsion fracture.
Table 1.
Predicted syndesmotic injury based on three fracture classification systems and measurements on X-ray. Findings at MRI regarding the anterior (ATIFL) and posterior tibiofibular ligament (PTIFL), transverse ligament, interosseous membrane and ligament, deep and superficial deltoid ligament are presented, together with the type of treatment
| X-ray | MRI | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fracture classificationc | Measurementsd | Syndesmosis injurye | Syndesmose | |||||||||||||||||||||||
| No. | Age (years) | Sex | MRIa | Sideb | WE | AO | LH | TFCS | TFO | MCS | SCS | WE | AO | LH | Injuryf | ATIFLg | AvAnth | Injuryf | PTIFLg | AvPosh | IOLi | TRLi | IOMj | De ∆i | Su ∆i | ORk |
| 1 | 24 | M | 0 | R | C | C.2.3 | SE4 | 4.3 | 11.9 | 5.7 | 3.9 | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 2 | 0 | 3 | 1 | 1 | 1 |
| 2 | 48 | F | 0 | L | C | * | SE3 | 4.6 | 3.8 | 1.7 | 3.6 | 1 | 0 | 3 | 1 | 3 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| 3 | 33 | M | 0 | L | * | * | SE1-PE2 | 5.7 | 6.3 | 3.3 | 4.4 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 0 | 0 | 2 | 0 | 0 | 2 | 1 |
| 4 | 26 | M | 0 | R | B | B.1.1 | SE2 | 5.1 | 5.9 | 1.7 | 3.4 | 0 | 0 | 1 | 1 | 3 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 5 | 39 | M | 0 | L | B | B.1.2 | SE2 | 6.3 | 5.7 | 4.7 | 3.8 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 |
| 6 | 26 | M | 0 | R | B | B.1.2 | SE2 | 6.5 | 0.0 | 7.9 | 5.9 | 1 | 1 | 1 | 1 | 3 | 0 | 1 | 1 | 1 | 1 | 1 | * | 1 | 3 | 1 |
| 7 | 41 | F | 0 | L | C | C.1.2 | SE4 | 3.2 | 7.5 | 1.7 | 3.2 | 1 | 1 | 3 | 1 | 3 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| 8 | 58 | F | 0 | R | C | C.2.2 | SE4 | 3.6 | 4.4 | 3.4 | 5.3 | 1 | 1 | 3 | 1 | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| 9 | 48 | M | 0 | R | A | A.1.3 | SA1 | 3.4 | 7.1 | 2.3 | 3.3 | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 10 | 17 | F | 0 | L | * | * | PD2 | 4.4 | 5.6 | 2.8 | 2.8 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 11 | 57 | F | 0 | L | A | A.1.3 | SA1 | 3.3 | 5.3 | 2.1 | 3.1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| 12 | 22 | M | 0 | R | A | A.1.2 | SA1 | 4.9 | 8.0 | 1.9 | 2.7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| 13 | 41 | M | 0 | L | B | B.1.1 | SE2 | 2.8 | 7.6 | 2.1 | 2.9 | 0 | 0 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14 | 23 | M | 0 | L | B | * | SE3 | 4.5 | 3.2 | 1.3 | 3.1 | 1 | 0 | 3 | 1 | 3 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 3 | 3 | 1 |
| 15 | 48 | M | 0 | L | B | B.2.2 | SE4 | 5.7 | 9.8 | 3.1 | 2.9 | 1 | 1 | 3 | 1 | 3 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| 16 | 21 | M | 0 | R | C | C.2.3 | PE4 | 11.6 | 0.0 | * | * | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 0 | 1 | 4 | 1 | 3 | 1 | 0 | 2 |
| 17 | 51 | M | 0 | R | B | B.3.2 | SE4 | * | 0.0 | * | * | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| 18 | 41 | M | 0 | R | B | B.1.1 | SE2 | 4.0 | 12.8 | 3.8 | 4.6 | 0 | 0 | 1 | 1 | 3 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 |
| 19 | 58 | F | 0 | L | A | A.1.2 | SA1 | 4.4 | 3.7 | 1.7 | 2.4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20 | 58 | M | 0 | L | B | * | SE4 | 3.9 | 9.6 | 2.5 | 2.7 | 0 | 0 | 3 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 |
| 21 | 20 | F | 1 | R | B | B.2.1 | SE4 | 2.5 | 0.0 | 12.7 | 2.9 | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 | 3 | 1 |
| 22 | 18 | F | 0 | R | B | B.1.1 | SE2 | 6.0 | 2.6 | 2.7 | 2.9 | 0 | 0 | 1 | 1 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 |
| 23 | 55 | M | 0 | L | * | * | PA1-PE1 | 4.8 | 4.2 | 2.5 | 2.9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 |
| 24 | 25 | F | 0 | L | B | B.1.2 | SE2 | 5.1 | 6.0 | 3.8 | 3.0 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 1 | 0 |
| 25 | 53 | F | 0 | L | C | C.2.2 | PA3 | 9.8 | 0.0 | 2.5 | 2.9 | 1 | 1 | 3 | 1 | 0 | 2 | 1 | 3 | 0 | 1 | 1 | 0 | 0 | 1 | 2 |
| 26 | 62 | F | 0 | L | B | B.1.2 | SE2 | 4.1 | 10.4 | 2.3 | 2.2 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 27 | 33 | F | 0 | R | B | B.1.1 | SE2 | 4.6 | 3.3 | 3.1 | 3.4 | 0 | 0 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 28 | 52 | F | 1 | R | C | C.3.3 | PE4 | 7.7 | 0.0 | 3.5 | 5.0 | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 3 | 0 | 1 | 1 | 0 | 2 | 3 | 2 |
| 29 | 48 | M | 1 | L | B | * | SE3 | 6.9 | 3.0 | 4.6 | 5.0 | 1 | 1 | 3 | 1 | 1 | 2 | 0 | 1 | 0 | 4 | 1 | 1 | 2 | 2 | 0 |
| 30 | 29 | M | 0 | R | * | * | PA1 | 2.9 | 2.8 | 2.2 | 4.1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 0 |
| 31 | 58 | M | 1 | L | B | B.3.2 | SE4 | * | * | * | * | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 |
| 32 | 28 | F | 0 | R | A | A.1.2 | SA1 | 5.3 | 3.6 | 2.5 | 3.9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 33 | 27 | F | 0 | R | B | B.1.1 | SE2 | 4.0 | 3.2 | 3.3 | 3.1 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| 34 | 27 | M | 0 | L | B | B.3.3 | SE4 | 5.4 | 4.5 | 3.7 | 3.0 | 1 | 1 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| 35 | 56 | F | 0 | L | A | A.1.2 | SA1 | 3.8 | 6.9 | 2.4 | 2.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 36 | 56 | M | 0 | R | C | C.1.1 | SE2 | 2.5 | 9.4 | 2.7 | 4.3 | 1 | 1 | 1 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| 37 | 16 | F | 0 | L | A | A.2.2 | SA2 | 3.9 | 5.4 | 3.1 | 3.2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 38 | 18 | M | 0 | R | C | * | SE3 | 4.6 | 4.9 | 2.6 | 5.0 | 1 | 0 | 3 | 1 | 3 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 3 | 3 | 2 |
| 39 | 53 | F | 0 | L | B | B.1.1 | SE2 | 3.9 | 3.7 | 2.6 | 3.1 | 0 | 0 | 1 | 1 | 3 | 0 | 1 | 0 | 1 | 4 | 0 | 0 | 1 | 1 | 0 |
| 40 | 51 | F | 0 | R | B | B.1.1 | SE2 | 3.5 | 3.7 | 2.3 | 2.9 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| 41 | 56 | M | 1 | L | B | B.1.2 | SE2 | 0.8 | 3.1 | 7.8 | 2.6 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 1 | 0 | 4 | 0 | 1 | 1 | 2 | 1 |
| 42 | 27 | F | 0 | L | A | A.1.1 | SA1 | 5.1 | 0.6 | 2.3 | 3.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| 43 | 18 | M | 1 | R | C | C.1.3 | PE4 | 6.2 | 1.4 | 2.7 | 3.5 | 1 | 1 | 3 | 1 | 1 | 0 | 1 | 0 | 1 | 4 | 0 | 0 | 0 | 0 | 2 |
| 44 | 30 | F | 0 | L | * | * | PA1-PE1 | 5.0 | 4.4 | 2.1 | 3.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 45 | 27 | M | 0 | R | C | C3.3 | PE4 | 4.3 | 2.1 | 4.0 | 4.3 | 1 | 1 | 3 | 1 | 3 | 0 | 0 | 2 | 0 | 3 | 0 | 2 | 3 | 3 | 2 |
| 46 | 20 | M | 0 | R | A | A1.2 | SA1 | 5.1 | 6.2 | 2.9 | 4.8 | 0 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| 47 | 61 | F | 0 | L | B | B3.3 | PA3 | 3.0 | 4.5 | 2.1 | 3.0 | 0 | 0 | 3 | 1 | 3 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 48 | 36 | M | 0 | L | A | A1.2 | SA1 | 3.9 | 8.1 | 2.1 | 3.6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 49 | 17 | M | 0 | R | * | * | * | 4.1 | 1.4 | 2.5 | 2.8 | 0 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 50 | 22 | F | 0 | R | B | B.1.2 | SE2 | 7.1 | 0.0 | 2.3 | 2.4 | 1 | 1 | 1 | 1 | 3 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| 51 | 17 | M | 0 | L | A | A.1.3 | SA1 | 2.4 | 6.9 | 3.2 | 4.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
aMRI: 0 performed before treatment, 1 performed postoperatively
bSide of ankle fracture: R right, L left
cFracture classification: WE Weber, AO AO-Müller, LH Lauge Hansen
dX-ray measurements: TFCS tibiofibular clear space (normal value TFCS ≤ 6 mm), TFO tibiofibular overlap (normal value TFO > 0 mm), MCS medial clear space, SCS superior clear space (normal value MCS ≤ 4 mm or MCS/SCS ≤ 1)
eSyndesmosis injury based on X-ray and measurements for WE and AO: 0 no injury, 1 injury; for LH based on trauma mechanism deduced from X-ray: 0 no injury, 1 anterior injury, 2 posterior injury, 3 anterior and posterior injury
fSyndesmosis injury anterior or posterior on MRI (i.e., ruptured tibiofibular ligament or intact tibiofibular ligament with an avulsion fracture): 0 no injury, 1 injury
gATIFL and PTIFL: 0 normal tibiofibular ligament, 1 thickened tibiofibular ligament, 2 possibly ruptured tibiofibular ligament, 3 ruptured tibiofibular ligament
hAvulsion fracture anterior (AvAnt) or posterior (AvPos): 0 no avulsion, 1 tibial avulsion, 2 fibular avulsion
iInterosseous ligament (IOL), transverse ligament (TRL), deep deltoid ligament (De ∆), and superficial deltoid ligament (Su ∆): 0 normal, 1 thickened, 2 partially ruptured, 3 completely ruptured
jInterosseous membrane (IOM): 0 normal, 1 rupture of membrane higher than fibula fracture, 2 rupture of membrane at the same level as fibula fracture, 3 rupture of membrane lower than fibula fracture
kOperation (OR): 0 no ORIF, 1 ORIF without setscrew, 2 ORIF with setscrew
Based on the AO-Müller classification, 11 (21.6%) fractures were classified as type A, 20 (39.3%) as type B, and 9 (17.7%) as type C; see Table 1 for detailed subclassifications. In 11 (21.6%) patients, the fracture could not be described. In addition to the six fractures that also could not be classified according to Weber, these included five fibula fractures combined with either a fracture of the medial malleolus or the posterior malleolus.
In 33 patients with normal measurements on radiographs, MRI showed absence of syndesmotic injury in 13 cases, consisting of 9 patients with a Weber type A and 4 patients with an unclassifiable fracture (Table 2). In the remaining 20 patients with normal measurements, anterior syndesmotic injury was present in 9 (Fig. 4), and both anterior and posterior syndesmotic injury in 11 patients. Syndesmotic injury was defined as either a rupture of the tibiofibular ligament or an intact tibiofibular ligament attached to an avulsion fracture. The measurements were normal in 2 patients with a Weber type A, or AO-Müller A1.2 and A1.3 fracture, with only anterior syndesmotic injury, and in 10 patients with a Weber type B (3 with only anterior and 7 with anterior and posterior injury), or 7 with a AO-Müller B1.1 fracture (3 with only anterior and 4 with anterior and posterior injury) and 1 AO-Müller B3.3 fracture (anterior and posterior injury). The measurements were also normal in six patients with a Weber type C fracture, with only anterior syndesmotic injury present in three and both anterior and posterior injury in another three cases, and in four patients with an AO-Müller type C fracture, three with anterior and one with both anterior and posterior injury. Two fractures that could not be classified by Weber and six that could not be classified by AO-Müller also showed syndesmotic injury.
Table 2.
Predicted syndesmotic injury (n) in acute ankle fractures, classified on radiographs according to Weber and AO-Müller and additional measurements, compared with syndesmotic injury on MRI
| Webera | Syndesmotic injury (MRI)b | AO-Müllera | Syndesmotic injury (MRI)b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 3 | 0 | 1 | 3 | ||||
| A | 0 | 9 | 2 | 0 | 44A | 0 | 9 | 2 | 0 |
| 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | ||
| B | 0 | 0 | 3 | 7 | 44B | 0 | 0 | 3 | 5 |
| 1 | 0 | 8 | 5 | 1 | 0 | 7 | 5 | ||
| C | 0 | 0 | 3 | 3 | 44C | 0 | 0 | 3 | 1 |
| 1 | 0 | 0 | 5 | 1 | 0 | 0 | 5 | ||
| nc | 0 | 4 | 1 | 1 | nc | 0 | 4 | 1 | 5 |
| 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | ||
aAssociated measurements on radiographs: 0 normal, 1 deviated
bSyndesmotic injury on MRI: 0 no injury, 1 anterior syndesmotic injury, 3 anterior and posterior syndesmotic injury
Fig. 4.
AP (a) and lateral (b) radiographs show a distal fibula fracture (1). Measurements are normal. The coronal proton-density-weighted MR image (c) also shows the fibula fracture (1). The axial proton-density-weighted MR image (d) is just below the level of the fibula fracture and demonstrates the rupture of the ATIFL (2). The fascicles of the PTIFL (3) are a little thickened but intact. This is a Weber type B, AO-Müller type B1.1, Lauge-Hansen SE2 fracture with normal measurements but with anterior syndesmotic injury. Ant Anterior, T tibia, F fibula
In 18 patients with deviating measurements, syndesmotic injury was present in all of them, with only anterior syndesmotic injury in 8 and both anterior and posterior injury in 10 patients. These included 13 patients with a Weber type B fracture, and 12 patients with AO-Müller type B fracture (at least B1.2) and 1 unclassifiable fracture, with only anterior syndesmotic in 8 and both anterior and posterior syndesmotic injury in 5 patients. The measurements deviated in five patients with a Weber or AO-Müller type C fracture with both anterior and posterior syndesmotic injury.
With MRI as gold standard, both the Weber and AO-Müller classification in association with the additional measurements detected injury of the anterior and posterior syndesmosis with a sensitivity of 47% (95%CI: 31–64%) and a specificity of 100% (95%CI: 75–100%). No correlation was found between the TFCS and TFO and the presence of syndesmotic injury (p = 0.152 and p = 0.682, respectively). With an MCS/SCS ratio > 1 or MCS > 4 mm, no correlation could be demonstrated with a rupture of the superficial or deep deltoid ligament (p = 1.00).
Lauge-Hansen fracture classification
Based on the Lauge-Hansen classification, 28 (54.8%) fractures were classified as supination external rotation (SE), 4 (7.8%) as pronation external rotation (PE), 11 (21.6%) as supination adduction (SA), 3 (5.9%) as pronation adduction (PA), and 1 (2.0%) as pronation dorsiflexion (PD); see Table 1 for detailed subclassifications. In four (7.8%) patients the fracture could not be classified. These involved either a solitary fracture of the medial malleolus with unknown status of the collateral ligaments or a tibial avulsion fracture.
In 15 patients without expected syndesmotic injury on the radiographs, MRI showed anterior syndesmotic injury in 3 patients (1 SA1 and 1 unclassifiable fracture) (Table 3). In 36 patients with expected syndesmotic injury on the radiographs, MR showed 1 patient without injury (PD2 fracture). Compared to MRI, Lauge-Hansen underestimated syndesmotic injury in 9 patients and overestimated in 5 (Table 3).
Table 3.
Predicted syndesmotic injury (n) as expected by Lauge-Hansen on the radiographs (Synd-X) compared with syndesmotic injury on MRI (Synd-MR)
| Lauge-Hansen | Synd-MR | ||
|---|---|---|---|
| Synd-X | 0 | 1 | 3 |
| 0 | 12 | 3 | 0 |
| 1 | 1 | 10 | 6 |
| 3 | 0 | 4 | 15 |
0 No injury, 1 anterior syndesmotic injury, 3 anterior and posterior syndesmotic injury
With MRI as gold standard, the Lauge-Hansen classification detected injury of the anterior and posterior syndesmosis with a sensitivity of 92% (95%CI: 79–98%), and a specificity of 92% (95%CI: 64–99.8%).
Treatment
Treatment was based on radiographs and perioperative findings, but without knowledge of MRI findings. In 19 patients the fracture was treated with an open reduction and internal fixation (ORIF), and in 6 of them the syndesmosis was fixed with a setscrew (Table 4). ORIFs with a setscrew included one patient with a rupture of the anterior syndesmosis associated with a rupture of the interosseous ligament, three patients with a rupture of both the anterior as well as posterior syndesmosis, and two patients with a rupture of both the anterior as well as posterior syndesmosis in association with a rupture of the interosseous ligament. All were Weber type C fractures or PE4 (n = 4), PA3 (n = 1), or SE3 (n = 1). The syndesmosis was fixed with a setscrew in four patients with an intact and in two patients with a ruptured interosseous membrane. In 0% (0/10) of Weber type B fractures and 86% (6/7) of Weber type C fractures treated with ORIF, a setscrew was required.
Table 4.
Fracture treatment (n) in relation to syndesmotic injury on MRI. Treatment consisted of plaster or open reduction and internal fixation (ORIF) with or without setscrew.
| Fracture treatment | Syndesmotic injury | ||
|---|---|---|---|
| 0 | 1 | 3 | |
| Plaster | 12 | 13 | 7 |
| ORIF, no setscrew | 1 | 3 | 9 |
| ORIF, with setscrew | 0 | 1 | 5 |
Syndesmotic injury on MRI: 0 no injury, 1 anterior syndesmotic injury, 3 anterior and posterior syndesmotic injury
Discussion
Our study population consisted of 51 consecutive patients with an acute ankle fracture. The fracture distribution conformed to other studies with reported fracture types of LH type SE (42–72%), PE (7–22%), SA (6–20%), and PA (5–21%) [26].
Anterior or posterior syndesmotic injury was defined as a rupture of the tibiofibular ligament or as an intact tibiofibular ligament attached to an avulsion fracture. With MRI as gold standard, both the Weber and AO-Müller classifications, in association with the additional measurements, detected injury of the anterior and posterior syndesmosis with a sensitivity of 47% and a specificity of 100%. LH detected syndesmotic injury with both a sensitivity and a specificity of 92%. To compare the sensitivity and specificity of the three fracture classification systems, no distinction was made with regard to the extent of syndesmotic injury, as with Weber and AO-Müller it is not possible to differentiate between anterior and posterior syndesmotic injury. With LH however, syndesmotic injury can be evaluated in more detail. In 14 cases we found a discrepancy between syndesmotic injury as predicted by LH and findings at MRI. LH under- and overestimated syndesmotic injury in 9 and 5 patients, respectively.
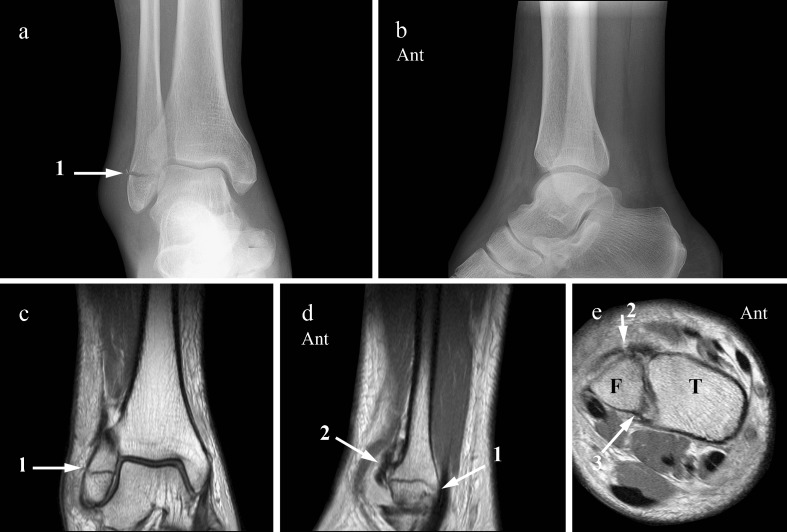
Underestimation involved three cases in which LH missed a rupture of the anterior syndesmosis. On radiographs, a transverse fibular fracture below the level of the tibiotalar joint space was present, suggesting a supination adduction type 1 (SA1) fracture. MRI showed, in addition to the transverse fibular fracture, injury of the anterior syndesmosis (Fig. 5). This is therefore not compatible with the general statement that the syndesmosis is not involved in supination-adduction injury, which is by definition an infrasyndesmotic injury. Gardner et al. also found 1 case, in a series of 59 patients, with a supination-adduction trauma in which the anterior tibiofibular ligament was ruptured [27]. As the ATIFL runs approximately in a 45° oblique plane from the anterior tibial tubercle to the anterior fibular tubercle and just crosses the anterolateral talar corner, its fibular insertion point lies a little below the level of the tibiotalar joint space [24, 28]. A fibula fracture at this level could therefore result in injury of the ATIFL. This finding could affect treatment outcome, as in the presence of syndesmotic injury a non-weightbearing cast would be the preferred treatment. In case of anterior syndesmotic injury, early weightbearing could result in an elongated healed ATIFL leading to complaints of chronic instability or even early osteoarthritis.
Fig. 5.
AP (a) and lateral (b) radiographs. A transverse fibular malleolar fracture (1) below the level of the tibiotalar joint space is visible. No fracture is visible at the medial or posterior malleolus. Measurements are normal. The fracture was classified as Weber A, AO-Müller A1.3, Lauge-Hansen SA1. Coronal (c), sagittal (d), and axial (e) proton-density-weighted MR image. The transverse fibula fracture (1) is visible on the coronal and sagittal MR image. The lower border of the ruptured ATIFL (2) lies just across the fibula fracture as can be seen on the sagittal MR image (d). In the 45° oblique image (e) the ATIFL (2) is thickened and avulsed from the fibula. The PTIFL (3) is intact. Ant Anterior, T tibia, F fibula
In six other cases of underestimated syndesmotic injury, LH predicted only anterior syndesmotic injury, whereas MRI showed also posterior injury. Anterior syndesmotic injury consisted of a ruptured ATFIL in four and an anterior fibular avulsion fracture in two patients. Posterior syndesmotic injury involved five patients with an intact PTIFL attached to an avulsed fragment of the posterior malleolus, which was not visible on the radiographs, and one patient with a ruptured posterior tibiofibular ligament (Fig. 6). In two patients the superficial deltoid ligament was partially or completely ruptured. With these findings on MRI, the fracture would change from SE2 into SE3 in three cases, from SE2 into SE4 in two cases, and from unclassifiable SE1/PE1 into PA2 in one case. For therapeutic management it is important to know whether a fracture is stable or unstable. An unstable fracture should be treated with an open reduction and internal fixation (ORIF) and, if necessary, syndesmotic stability should be regained with a setscrew. In two patients with an underestimated SE4 fracture, ORIF was performed without fixation of the syndesmosis with a setscrew, although on MRI the superficial ligament was partially or completely ruptured, and the deep deltoid ligament was intact in both. The measurements deviated only in one case. It is likely that the deep deltoid ligament prevents a lateral shift of the talus when the fibula is pulled laterally with the hook test [29], whereas the superficial deltoid ligament gives restraint to a valgus position of the talus.
Fig. 6.
AP (a) and lateral (b) radiographs show a distal fibula fracture (1) at the level of the syndesmosis, running obliquely from anteroinferior to posterosuperior, characteristic of a supination-external rotation trauma. Measurements are normal. This fracture is classified as Weber type B, AO-Müller type B1.1, and Lauge-Hansen SE2. Coronal (c) and 45° oblique (d) proton-density-weighted MR images demonstrate the fibula fracture (1), and a normal deep (2) and superficial (3) deltoid ligament. The ATIFL is ruptured (4), whereas the intact PTIFL (5) is attached to an avulsion fracture of the posterolateral malleolus (6). This is therefore a Weber type B fracture with normal measurements but with anterior as well as posterior syndesmotic injury. According to Lauge-Hansen, this is an SE3 fracture
Overestimation of syndesmotic injury occurred in five cases. In one case with a pronation-dorsiflexion type 2 injury (PD2), the radiographs showed a transverse fracture of the medial malleolus and a fracture of the anterior rim of the distal tibia, which was interpreted as a possible Chaput-Tillaux fracture, implying anterior syndesmotic injury. On MRI the fracture of the medial malleolus was well visualized. The intact multifascicular ATIFL was attached to a normal tubercle of Chaput that was adjacent to a comminute impression fracture of the anterior tibial rim.
In four other cases of overestimation, injury of both the anterior and posterior syndesmosis was expected on the radiographs, but MRI showed only anterior injury. In one case with a suspected SE4 trauma, based on a fibula fracture, a suspected medial malleolus avulsion fracture and posterior syndesmotic injury inferred from the type of trauma mechanism, MRI showed neither posterior nor medial injury, resulting in down staging of the fracture into SE2. In two cases, a supination external rotation type 3 and 4 trauma was based on an obliquely running fibula fracture, from anteroinferior to posterosuperior, associated with either a suspected posterior malleolus avulsion fracture or an avulsion fracture of the medial malleolus. MRI, however, showed in both cases no posterior malleolus fracture or ruptured posterior tibiofibular ligament but did show either a medial malleolus avulsion fracture or a possibly ruptured deltoid ligament. Both experimentally and clinically, an SE4 injury can exist without damage to the posterior tibiofibular ligament [30, 31]. The absence of posterior injury suggests these fractures could also be a pronation external rotation injury type 3 (PE3). In that case, however, the direction of the fibula fracture line should be from anterosuperior to posteroinferior, and usually the level of the fracture is above the syndesmosis, which was not the case in these two patients. In a study with cadavers, Haraguchi et al. showed that a pronation external rotation trauma could result in a fibula fracture at the level of the syndesmosis with a fracture line running from anterosuperior to posteroinferior [32]. They also noted that medial injury occurred after the fracture of the fibula and posterior injury was absent in four of eight cadavers. This means that a PE3 or SE4 type of fracture cannot always be distinguished on radiographs or MRI only. The clinical relevance of this distinction is based on the stability of the tibiotalar and tibiofibular joint. As with PE fractures, the level of the fibula fracture is above the syndesmosis and could be accompanied by a rupture of the interosseous membrane, this fracture type would benefit from a setscrew, whereas fibula fractures within 3.0–4.5 cm of the tibiotalar joint do not need a setscrew [33].
The fourth case of overestimated syndesmotic injury involved a pronation-external rotation type 4 trauma (PE4, i.e., Maisonneuve fracture), based on a proximal fibula fracture, an avulsed medial malleolus, and possible fracture of the posterior malleolus. Although MRI showed an intact posterior malleolus, the posterior tibiofibular ligament was thickened and attached to a slip of avulsed tibial periosteum from the posterior malleolus, suggesting at least some kind of posterior traumatic stress. Therefore, based on these findings the fracture should be classified as PE3.
On radiographs, injury of the distal tibiofibular syndesmosis can be predicted based on the type of fracture. According to Weber the more proximal the fibula fracture, the greater the risk of a disrupted syndesmosis and ankle instability. A rupture of the syndesmotic ligaments is assumed in all type C and in 50% of type B fractures [5]. In the AO-Müller classification, syndesmotic injury is expected in all fractures with at least a type B1.2 fracture. However it is not possible to predict which of the Weber type B or AO-Müller type B1.1 fractures will have injury of the syndesmotic ligaments, and for that reason radiographic measurements can be used to deduce syndesmotic injury. In our study the Weber and AO-Müller fracture classification showed a low sensitivity of 47% for prediction of syndesmotic injury. In contrast to literature in which 50% of Weber type B fractures are expected to have syndesmotic injury, our study showed syndesmotic injury in all patients, either anterior (48%) or both anterior and posterior (52%). Measurements, however, were normal in 64% with only anterior and in 67% with both anterior and posterior syndesmotic injury. In all Weber type C fractures, syndesmotic injury was present, as expected, although the measurements were normal in 55%. Nielson et al. showed that the tibiofibular clear space (TFCS) and tibiofibular overlap (TFO) did not correlate with anterior and posterior tibiofibular ligament injuries [34]. According to Beumer et al. there is no optimal radiographic parameter to assess the integrity of the syndesmosis. Absence of tibiofibular overlap at one side may be an indication of syndesmotic injury, and a medial clear space surpassing the tibial clear space is indicative of deltoid injury [22]. As a secondary question in this study, we looked at the additional value of the measurements and also concluded that the TFCS and TFO did not correlate with syndesmotic injury and neither did a widened medial clear space correlate with deltoid ligament injury [35]. A possible explanation for normal measurements in the presence of syndesmotic injury could be the spontaneous reduction of the tibiofibular diastasis after the acute injury. But whenever measurements deviated, syndesmotic injury was always present, whereas normal measurements did not exclude syndesmotic injury.
Syndesmotic stability occurs in the coronal, sagittal, rotational, and axial planes, but only the coronal and rotational plane instabilities are routinely addressed clinically [36]. Coronal plane stability is tested intraoperatively with the hook test by pulling laterally on the fibula with a bone hook. Lateral movement of the fibula or widening of the mortise on the AP radiograph suggests the need for a setscrew. Van den Bekerom reported a sensitivity of 39% and specificity of 96% of the hook test with a cut-off of the height of the fibula fracture of 4.5 cm [37]. Rotational plane instability can be tested with an intraoperative fluoroscopic external rotation stress test and is based on radiographic tibiofibular clear space measurements. With intraoperative fluoroscopy Jenkinson et al. detected syndesmotic instability in 37% of ankle fractures [38]. Xenos et al. evaluated syndesmotic instability with the external rotation stress test by assessing posterior movement of the fibula on lateral radiographs [39], suggesting instability of the syndesmosis in a sagittal plane. These studies show that syndesmotic instability can occur in different planes and depends on which of the osseoligamentous structures are disrupted and therefore play a role in the discussion of which ankle fractures need to be stabilized with a setscrew. Therefore if the surgeon knows preoperatively which syndesmotic ligaments are injured, application and interpretation of available intraoperative tests could be optimized and result in a better evaluation of syndesmotic instability and aid in the decision of whether or not to use a setscrew.
Our study showed several shortcomings. It was not possible to perform an MRI preoperatively in all patients, but the presence of a plate and screws did not influence image quality, and the syndesmotic ligaments could still be well evaluated. The presence of a setscrew could influence the observer with regard to the extent of syndesmotic injury. This occurred only in two cases in which both anterior and posterior syndesmotic injuries were obviously present, and a bias therefore not likely. We did not perform a standardized preoperative stress test, nor was the intra-operatively used stress test performed in a standardized way, but this conforms to the daily routine in our clinic. This study was a radiographic analysis without clinical or long-term follow-up.
Overall we can conclude that, in this study, the sensitivity for detecting syndesmotic injury with the Weber and AO-Müller fracture classification in combination with additional measurements is low, and much higher with the Lauge-Hansen fracture classification. We showed that syndesmotic injury was present in all Weber type B fractures, although measurements were normal in 65%. Remarkably, none of the Weber type B fractures treated with ORIF required a setscrew, although both anterior and posterior syndesmotic injury was present. MRI showed that posterior syndesmotic injury only occurred in association with anterior syndesmotic injury, and in 80% consisted of an intact posterior tibiofibular ligament attached to an avulsion fracture of the posterior malleolus, which was not visible on the radiographs in 33%. Anterior avulsion fractures were only visible on the radiographs in 50%. Although Lauge-Hansen is the best available fracture classification for predicting syndesmotic injury, MRI can be of additional value in determining its exact extent, as until now when referring to syndesmotic injury the exact extent of osseoligamentous involvement has not been defined.
Conclusion
Lauge-Hansen is the best fracture classification to predict syndesmotic injury with both a sensitivity and a specificity of 92%. The Weber and AO-Müller fracture classification system detected syndesmotic injury with a sensitivity of 47% and a specificity of 100%. In this study, 100% of Weber type B fractures showed a rupture of the syndesmosis, in contrast to 50% reported in literature. On radiographs, underestimation of anterior and posterior syndesmotic injury is partly due to missed fibular or tibial avulsion fractures in 50 and 67%, respectively. Posterior syndesmotic injury occurred only in association with anterior syndesmotic injury and in 86% consisted of a posterior malleolus fracture. TFCS and TFO did not correlate with syndesmotic injury, nor did a widened MCS correlate with deltoid ligament injury. In 12% of patients, ORIF with a setscrew was performed, but not only in unstable fractures.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Contributor Information
J. J. Hermans, Phone: +31-24-3614011, Email: jjhermans@gmail.com
N. Wentink, Email: noortje_wentink@hotmail.com
A. Beumer, Email: achbeumer@hotmail.com
W. C. J. Hop, Email: w.hop@erasmusmc.nl
M. P. Heijboer, Email: m.heijboer@erasmusmc.nl
A. F. C. M. Moonen, Email: sjorsmoonen@hotmail.com
A. Z. Ginai, Email: a.ginai@erasmusmc.nl
References
- 1.Bartonicek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25(5–6):379–386. doi: 10.1007/s00276-003-0156-4. [DOI] [PubMed] [Google Scholar]
- 2.Kelikian H, Kelikian S. Disorders of the ankle. London: W.B. Saunders Company; 1985. [Google Scholar]
- 3.Kapandji IA. Funktionelle Anatomie der Gelenke. Schematisierte und kommentierte Zeichnungen zur menslichen Biomechanik. Stuttgart: Ferdinand Enke; 1985. 148–65.
- 4.Lutz W. Zur Struktur der unteren Tibiofibularverbindung und der Membrana interossea cruris. Anat Entwickl Gesch. 1942;111:315–321. doi: 10.1007/BF00538090. [DOI] [Google Scholar]
- 5.Weber BG. Die Verletzungen des oberen Sprunggelenkes. Zweite, überarbeitete und ergänzte Auflage. Vienna: Hans Huber Bern Stuttgart; 1972.
- 6.Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60(5):957–985. doi: 10.1001/archsurg.1950.01250010980011. [DOI] [PubMed] [Google Scholar]
- 7.Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Berlin: Springer-Verlag; 1990. [Google Scholar]
- 8.Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10(3):156–160. doi: 10.1177/107110078901000308. [DOI] [PubMed] [Google Scholar]
- 9.Pneumaticos SG, Noble PC, Chatziioannou SN, Trevino SG. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int. 2002;23(2):107–111. doi: 10.1177/107110070202300205. [DOI] [PubMed] [Google Scholar]
- 10.Beumer A. Chronic instability of the anterior syndesmosis of the ankle: biomechanical, kinematical, radiological and clinical aspects. Rotterdam: Erasmus University Rotterdam; 2007. [Google Scholar]
- 11.Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77(6):847–856. doi: 10.2106/00004623-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10(6):325–330. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 13.Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294–298. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- 14.Vogl TJ, Hochmuth K, Diebold T, Lubrich J, Hofmann R, Stockle U, et al. Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol. 1997;32(7):401–409. doi: 10.1097/00004424-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182(1):131–136. doi: 10.2214/ajr.182.1.1820131. [DOI] [PubMed] [Google Scholar]
- 16.Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85(3):324–329. doi: 10.1302/0301-620X.85B3.13174. [DOI] [PubMed] [Google Scholar]
- 17.Oae K, Takao M, Naito K, Uchio Y, Kono T, Ishida J, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227(1):155–161. doi: 10.1148/radiol.2271011865. [DOI] [PubMed] [Google Scholar]
- 18.Pettrone FA, Gail M, Pee D, Fitzpatrick T, Van Herpe LB. Quantitative criteria for prediction of the results after displaced fracture of the ankle. J Bone Joint Surg Am. 1983;65(5):667–677. [PubMed] [Google Scholar]
- 19.Sclafani SJ. Ligamentous injury of the lower tibiofibular syndesmosis: radiographic evidence. Radiology. 1985;156(1):21–27. doi: 10.1148/radiology.156.1.4001407. [DOI] [PubMed] [Google Scholar]
- 20.Ebraheim NA, Lu J, Yang H, Rollins J. The fibular incisure of the tibia on CT scan: a cadaver study. Foot Ankle Int. 1998;19(5):318–321. doi: 10.1177/107110079801900509. [DOI] [PubMed] [Google Scholar]
- 21.Joy G, Patzakis MJ, Harvey JP., Jr Precise evaluation of the reduction of severe ankle fractures. J Bone Joint Surg Am. 1974;56(5):979–993. [PubMed] [Google Scholar]
- 22.Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004(423):227–34. [DOI] [PubMed]
- 23.Hermans JJ, Ginai AZ, Wentink N, Hop WC, Beumer A. The additional value of an oblique image plane for MRI of the anterior and posterior distal tibiofibular syndesmosis. Skeletal Radiol. 2011;40(1):75–83. [DOI] [PMC free article] [PubMed]
- 24.Hermans JJ, Beumer A, De Jong AW, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010;217(6):633–45. [DOI] [PMC free article] [PubMed]
- 25.Kim S, Huh YM, Song HT, Lee SA, Lee JW, Lee JE, et al. Chronic tibiofibular syndesmosis injury of ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology. 2007;242(1):225–235. doi: 10.1148/radiol.2421051369. [DOI] [PubMed] [Google Scholar]
- 26.Lindsjo U. Classification of ankle fractures: the Lauge-Hansen or AO system? Clin Orthop Relat Res. 1985;199:12–16. [PubMed] [Google Scholar]
- 27.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma. 2006;20(4):267–272. doi: 10.1097/00005131-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Boonthathip M, Chen L, Trudell DJ, Resnick DL. Tibiofibular syndesmotic ligaments: MR arthrography in cadavers with anatomic correlation. Radiology. 2010;254(3):827–836. doi: 10.1148/radiol.09090624. [DOI] [PubMed] [Google Scholar]
- 29.Snedden MH, Shea JP. Diastasis with low distal fibula fractures: an anatomic rationale. Clin Orthop Relat Res. 2001;382:197–205. doi: 10.1097/00003086-200101000-00027. [DOI] [PubMed] [Google Scholar]
- 30.Michelson J, Solocoff D, Waldman B, Kendell K, Ahn U. Ankle fractures. The Lauge-Hansen classification revisited. Clin Orthop Relat Res. 1997;345:198–205. doi: 10.1097/00003086-199712000-00029. [DOI] [PubMed] [Google Scholar]
- 31.Yde J, Kristensen KD. Ankle fractures. Supination-eversion fractures stage II. Primary and late results of operative and non-operative treatment. Acta Orthop Scand. 1980;51(4):695–702. doi: 10.3109/17453678008990863. [DOI] [PubMed] [Google Scholar]
- 32.Haraguchi N, Armiger RS. A new interpretation of the mechanism of ankle fracture. J Bone Joint Surg Am. 2009;91(4):821–829. doi: 10.2106/JBJS.G.01288. [DOI] [PubMed] [Google Scholar]
- 33.Boden SD, Labropoulos PA, McCowin P, Lestini WF, Hurwitz SR. Mechanical considerations for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am. 1989;71(10):1548–1555. [PubMed] [Google Scholar]
- 34.Nielson JH, Gardner MJ, Peterson MG, Sallis JG, Potter HG, Helfet DL, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;436:216–221. doi: 10.1097/01.blo.0000161090.86162.19. [DOI] [PubMed] [Google Scholar]
- 35.Koval KJ, Egol KA, Cheung Y, Goodwin DW, Spratt KF. Does a positive ankle stress test indicate the need for operative treatment after lateral malleolus fracture? A preliminary report. J Orthop Trauma. 2007;21(7):449–455. doi: 10.1097/BOT.0b013e31812eed25. [DOI] [PubMed] [Google Scholar]
- 36.Candal-Couto JJ, Burrow D, Bromage S, Briggs PJ. Instability of the tibio-fibular syndesmosis: have we been pulling in the wrong direction? Injury. 2004;35(8):814–818. doi: 10.1016/j.injury.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 37.van den Bekerom MP, Haverkamp D, Kerkhoffs GM, van Dijk CN. Syndesmotic stabilization in pronation external rotation ankle fractures. Clin Orthop Relat Res. 2010;468(4):991–5. [DOI] [PMC free article] [PubMed]
- 38.Jenkinson RJ, Sanders DW, Macleod MD, Domonkos A, Lydestadt J. Intraoperative diagnosis of syndesmosis injuries in external rotation ankle fractures. J Orthop Trauma. 2005;19(9):604–609. doi: 10.1097/01.bot.0000177114.13263.12. [DOI] [PubMed] [Google Scholar]
- 39.Grath GB. Widening of the ankle mortise. A clinical and experimental study. Acta Chir Scand Suppl. 1960;263(Suppl):1–88. [PubMed] [Google Scholar]