Abstract
Previous research suggests that women who report dietary restraint tend to consume alcohol in greater quantities, however most studies use retrospective data collection, which are often unreliable, and no studies have accounted for this relationship with respect to potential changes in alcohol consumption across the menstrual cycle. Therefore, the present study investigated the relationship between prospectively monitored drinking patterns and dietary restraint across the menstrual cycle among females from the general population whose drinking level (7 – 20 drinks/week) places them at-risk for developing alcohol use disorders. Restrained eaters (RES; N = 51) and unrestrained eaters (UN-RES; N = 55), per the cognitive restraint scale scores from the Three-Factor Eating Questionnaire, provided prospective ratings measuring mood, alcohol consumption, and consequences of alcohol use across one full menstrual cycle. Dysphoric mood increased during the late luteal and menstrual phases in both groups. Although overall the RES group did not drink more than the UN-RES group, the RES group drank less than the UN-RES group during the follicular phase, suggesting that among RES women alcohol consumption may be modulated by hormonal fluctuations across the menstrual cycle. The differences between the present findings and previous research may be due to the cohorts sampled; the majority of previous studies sampled college students, where binge drinking and dietary restraint are more common, whereas this study sampled the general population. Future research should replicate prior studies in a college-aged population using the current design of prospective data collection for greater accuracy of self-reported alcohol consumption.
Keywords: women, “at-risk” drinking, dietary restraint, alcohol, menstrual cycle
1. Introduction1
Previous research in non-psychiatric populations have consistently found that women who show patterns of restrictive eating and/or tendencies towards dieting also show greater alcohol consumption (Bradstock et al., 1988; Bryant, Kiezebrink, King, & Blundell, 2010; Higgs & Eskenazi, 2007; Khaylis, Trockel, & Taylor, 2009; Krahn et al., 2005; Lavik, Clausen, & Pedersen, 1991; Stewart, Angelopoulos, Baker, & Boland, 2000; Xinaris & Boland, 1989). However, previous findings have been restricted by sampling only a subset of the female population (i.e., college women), retrospective data collection, which has been associated with underreporting of drinking behavior (Whitty & Jones, 1992), and not assessing the role of the menstrual cycle. In the general population, both an absence of menstrual cycle related changes in alcohol consumption (Charette, Tate, & Wilson, 1990; Freitag & Adesso, 1993; Holdstock & deWit, 2000; Nyberg, Wahlström, Backström, & Sundström-Poromaa, 2004; Terner & deWit, 2006) and increased alcohol consumption in the menstrual and luteal phases (Mello, Mendelson, & Lex, 1990; Pastor & Evans, 2003) have been found, suggesting that further research on the impact of the menstrual cycle on alcohol use is warranted.
The current study sought to investigate whether menstrual cycle-related changes in alcohol consumption are moderated by dietary restraint among women using a study design addressing previous methodological limitations. Therefore, changes in mood and alcohol consumption were assessed across the menstrual cycle between female restrained (RES) and unrestrained (UN-RES) eaters, who were also all “at-risk” drinkers, from the general population using prospective data collection. Based on previous research, we hypothesized that all women would increase alcohol consumption in the luteal and menstrual phases but there would be a greater increase in RES eaters than the UN-RES eaters.
2. Material and Methods
2.1 Participants
Women recruited from advertisements around the New York City area were told that the purpose of the study was to determine changes in mood, patterns of alcohol use and eating behavior across the menstrual cycle. Based on NIAAA (2010) guidelines, for women, “at-risk” drinking is defined as ≥ 7 drinks per week and binge drinking is defined as ≥ 4 drinks per day. Women who typically drank more than 20 drinks per week were excluded, similar to our previous studies (Evans & Levin, 2004, 2011; Pastor & Evans, 2003). No participant had an Axis I disorder within the last year. All women were normally cycling, not using hormonal contraceptives, and not pregnant (confirmed using a urine pregnancy test at screening). No one endorsed significant medical or psychiatric histories, moderate to severe premenstrual symptoms, or daily medication use. The Institutional Review Board at the New York State Psychiatric Institute approved this study. Participants signed informed consent and were financially compensated for their participation.
2.2 Procedures
Based on an initial telephone interview, women who endorsed “at-risk” drinking were brought in for screening; participants were recruited to obtain both restrained and unrestrained eaters. During screening, all participants completed a number of questionnaires (see measures section). “At-risk” drinking was confirmed through a structured interview with the participant. Participants were assessed for current Axis I disorders, using the MINI International Neuropsychiatric Interview (Sheehan, Janavas, Knapp, Sheehan, & Baker, 1994) and substance abuse module of the Structured Clinical Interview for DSM-IV-TR (First, Spitzer, Gibbon, & Williams, 1994).
Eligible individuals were provided with modified Daily Ratings Form (DRFs; Pastor & Evans, 2003) to prospectively monitor their mood, alcohol consumption, and consequences of alcohol use across one full menstrual cycle. Participants were instructed to fill these forms out each morning for the previous day and to return them to the laboratory by mail each day using the addressed, stamped envelopes provided. Once all forms were received, participants came in for an exit interview to discuss their drinking behavior. Each participant was paid for her participation, received informational brochures on the effects of alcohol use, and offered treatment referrals if necessary.
2.3 Measures
The Beck-Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) and the State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970) assessed depression and anxiety, respectively. The Short Michigan Alcoholism Screening Test (SMAST; Selzer, Vinokur, & Van Rooijen, 1975) assessed the presence of alcohol-related problems, and the Quantity-Frequency-Variability Index (QFV; Cahalan, Cisin, & Crossley, 1985) assessed the frequency, type and quantity of alcohol use over the last month. The Alcohol Outcome Expectancy Questionnaire (AOEQ; Leigh & Stacy, 1993) assessed the positive and negative effects of alcohol consumption. The Premenstrual Assessment Form (Halbreich, Endicott, Schacht, & Nee, 1982) assessed premenstrual symptoms over the last three menstrual cycles. The Three Factor Eating Questionnaire (TFEQ; Stunkard & Messick, 1985) was used to classify each participant as either a restrained eater (RES group) or an unrestrained eater (UN-RES group) based on the median split of the cognitive restraint scale scores, a strategy successfully used in other studies (Kanarek, Ryu, & Przypek, 1995; Yeomans & Coughlan, 2009). The modified DRFs (see Endicott, Nee, Cohen, & Halbreich 1986; Pastor & Evans, 2003) were used to prospectively measure mood, alcohol consumption, consequences of drinking alcohol, and the onset and duration of menses.
2.4 Data Analysis
Analyses were based on the 106 women (55 UN-RES and 51 RES eaters) who completed the study. Chi-Square and t-tests compared demographic characteristics, depression, anxiety, SMAST scores, pattern of substance use, and menstrual cycle characteristics (e.g., onset of menses, cycle length) between the UN-RES and RES women.
The menstrual cycle was divided into three clearly defined phases: menstrual (days one to five of menses), follicular (days six to 10 after the onset of menses), and late luteal (five days prior to the onset of menses). Dependent measures of prospective alcohol consumption, based on information from the DRFs, included: 1) alcohol consumption during each of these three menstrual cycle phases (calculated as the number of drinks consumed): 2) number of drinking days; 3) number of days intoxicated, and 4) number of binge drinking episodes. Mood scores were calculated for these menstrual cycle phases by averaging the scores within each defined phase. Similarly, positive and negative consequences of drinking scores were calculated, but only on days alcohol was consumed. SPSS® software was used to conduct separate two-factor analyses of variance (ANOVA) with group (UN-RES and RES) as the between-subject factor and phase (menstrual, luteal, and follicular) as the within-subject factor for each dependent measure. Post hoc analysis using Tukey's HSD tests were used when warranted.
For all analyses, results were considered statistically significant at p ≤ 0.05.
3. Results
Table 1 shows demographic characteristics for the UN-RES and RES groups. Overall, there were few differences between the two groups; the RES group reported significantly longer menstrual cycles (p = 0.05), fewer marijuana users (p = 0.02) and higher cognitive restraint (p < 0.0001) and disinhibition (p = 0.01) scores on the TFEQ than the UN-RES group. However, there were no differences between groups on retrospective self-reported weekly alcohol consumption; both groups drank an average of 13 drinks per week.
Table 1.
DEMOGRAPHICS
| UN-RES (N=56) | RES (N=51) | Sig. | |
|---|---|---|---|
| Demographicsa | |||
| Age (years) | 26.62 (5.20) | 26.98 (5.87) | N.S. |
| Racial/ethnic Composition (% White) | 52.73% | 56.86% | N.S. |
| Education (years) | 15.53 (3.72) | 15.49 (2.64) | N.S. |
| Body Mass Index (BMI) | 22.39 (3.65) | 22.83 (2.62) | N.S. |
| State Anxiety Inventory | 32.29 (8.45) | 33.55 (8.22) | N.S. |
| Trait Anxiety Inventory | 34.73 (8.13) | 35.24 (8.31) | N.S. |
| Beck Depression Inventory | 5.40 (4.28) | 5.41 (5.06) | N.S. |
| Short Michigan Alcohol Screening Test | 0.80 (1.08) | 0.75 (1.00) | N.S. |
| Age of Onset Menses (years) | 12.59 (1.46) | 12.60 (1.68) | N.S. |
| Menstrual Cycle Length | 28.65 (2.62) | 29.69 (2.91) | p=0.05 |
| Substance Use | |||
| Retrospective Mean Drinks Per Weeka | 12.97 (5.16) | 13.16 (5.30) | N.S. |
| Retrospective Range of Drinks Per Week | 4.00-28.00 | 3.00-22.00 | |
| % Caffeine Users | 82.14% | 92.16% | N.S. |
| % Marijuana Users | 51.79% | 29.41% | p=0.02 |
| % Cocaine Users | 12.50% | 3.92% | N.S. |
| % Cigarette Smokers | 39.29% | 33.33% | N.S. |
| Three Factor Eating Questionnaire (TFEQ)a | |||
| Cognitive Restraint Score | 4.23 (2.88) | 13.31 (2.60) | p<0.0001 |
| Disinhibition Score | 4.69 (2.56) | 6.22 (3.20) | p=0.01 |
| Hunger Score | 5.85 (2.54) | 5.41 (2.34) | N.S. |
Shown are means (standard deviations)
N.S. Not Significant
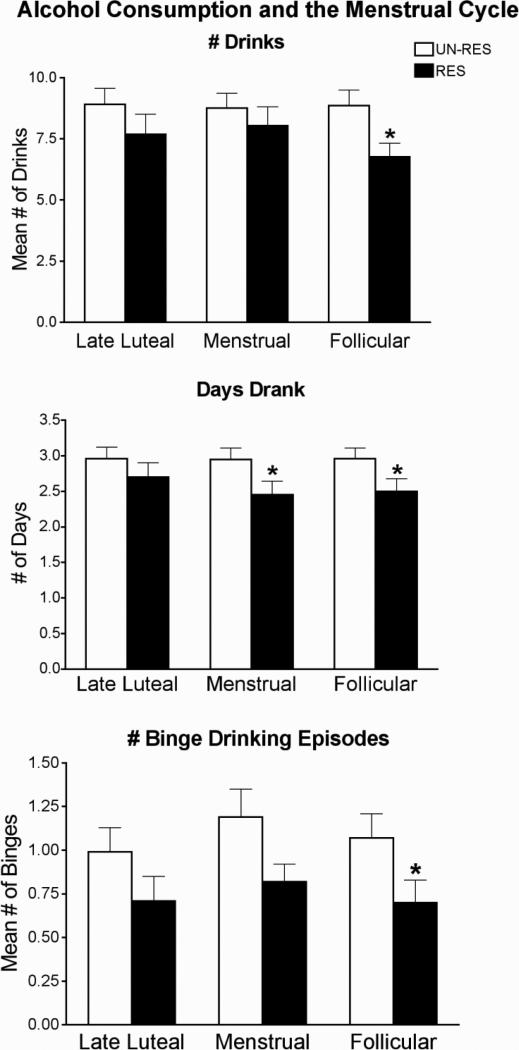
Based on the DRFs, dysphoric mood scores significantly increased in the late luteal and menstrual phases compared to the follicular phase [F (2/205) = 15.95, p < 0.0001] to the same extent in both groups. Figure 1 shows drinking patterns as a function of menstrual cycle phase and group. Based on the DRFs, there was a significant group effect with the RES group reporting significantly fewer drinks consumed [F (1/105) = 4.04; p = 0.05], drinking days [F (1/105) = 4.65; p = 0.03], number of binge drinking episodes [F (1/105 = 6.19; p = 0.01] and days intoxicated [F (1/105 = 3.85; p = 0.05], and greater negative consequences of drinking [F (1/105) = 4.31; p = 0.04] compared to the UN-RES group. Specifically, post-hoc analyses showed that the RES group reported significantly fewer drinks consumed (p = 0.02), significantly fewer binge drinking episodes (p = 0.05), and a trend in greater negative consequences of drinking (p = 0.06) in the follicular phase than the UN-RES group, with no group differences in these measures during the luteal or menstrual phases (p's > 0.05). Further, the RES group drank on significantly fewer days during the menstrual (p = 0.04) and follicular (p = 0.05) phases, but not the luteal phase (p > 0.05), than the UN-RES group. There were no other significant differences in scores on other self-reports (all p's > 0.05).
Figure 1.
Alcohol consumption as a function of menstrual cycle phase and group. Data points show means and vertical bars show 1 S.E.M. * indicates a significant difference between UN-RES and RES eaters at p<0.05.
4. Discussion
The present study investigated the link between restrictive eating and prospective drinking behavior in female “at-risk” drinkers. In support of our hypotheses, our results showed that dysphoric mood significantly increased in the late luteal and menstrual phases compared to the follicular phase, as shown previously (Gonda et al., 2008; Pastor & Evans, 2003; Reed, Levin, & Evans, 2008). In contrast to a previous study where lower dietary restraint was associated with fewer premenstrual symptoms retrospectively (Bowen & Grunberg, 1990), mood changes across the menstrual cycle were similar in the RES and UN-RES groups in the current study, most likely due to the use of prospective data collection in our study.
RES women did not drink more than UN-RES women, also contrary to our hypotheses and previous findings (Bradstock et al., 1988; Higgs & Eskenazi, 2007; Krahn, Kurth, Gomberg, & Drewnowski, 2005; Lavik, Clausen, & Pedersen, 1991; Stewart, Angelopoulos, Baker, & Boland, 2000; Xinaris & Boland, 1989). The differences between the present findings and previous research may be due to the cohorts sampled and the use of prospective, rather than self-reports. Further, there was no overall menstrual cycle effect on drinking levels among women, although this was consistent with previous findings (Charette Tate, & Wilson, 1990; Freitag & Adesso, 1993; Holdstock & deWit, 2000). However, RES women drank less than the UN-RES women during the follicular phase suggesting that RES women may be less restrained in their drinking during the luteal phase, when dysphoric mood is greater, than the follicular phase, similar to previous hypotheses (Price, DiMarzio, & Eckert, 1987; McLeod, Foster, Hoehn-Saric, Svikis, & Hipsley, 1994; Svikis et al., 2006).
The primary strength of this study was the prospective reporting of alcohol consumption compared to previous studies that relied on retrospective self-reports (Higgs & Eskenazi, 2007; Krahn, Kurth, Gomberg, & Drewnowski, 2005; Lavik Clausen, & Pedersen, 1991; Stewart, Angelopoulos, Baker, & Boland, 2000), allowing for a more accurate assessment of drinking behavior. Additionally, these individuals were sampled from the general population, leading to a broader understanding of alcohol consumption patterns amongst women. However, this could also be considered a limitation; the significant findings associating restrictive eating patterns and binge drinking episodes found in previous studies may be unique to college and adolescent-aged women where these issues are more relevant (Higgs & Eskenazi, 2007; Khaylis, Trockel, & Taylor, 2009; Krahn, Kurth, Gomberg, & Drewnowski, 2005; Lavik Clausen, & Pedersen, 1991; Stewart, Angelopoulos, Baker, & Boland, 2000). Lastly, this is the first study to take into account menstrual cycle effects, shown to influence the effects of other drugs of abuse (Justice & de Wit, 1999; Sofuoglu, Dudish-Poulsen, Nelson, Pentel, & Hatsukami, 1999; Evans, Haney, & Foltin, 2002), on drinking patterns among restrained eaters. Although we were unable to confirm menstrual cycle phases with hormone levels, the robust self-reported mood changes observed across the menstrual cycle in both groups strongly suggest that we appropriately identified the correct phases of the menstrual cycle in the current study.
5. Conclusions
In summary, these findings suggest that among women in the general population who drink at an “at-risk” level, dietary restraint is not indicative of greater alcohol consumption and may actually be a protective factor, particularly during the follicular phase of the menstrual cycle when dysphoric mood is lower. Therefore, the phenomenon of restrained eating and binge drinking among women may be restricted to the college atmosphere, where irregular eating and drinking patterns are more prevalent and potentially problematic (Kelly-Weeder, 2010; Khaylis, Trockel, & Taylor, 2009). Future research should confirm the findings of previous studies in college populations using prospective data collection to better determine the interaction of drinking, eating, and mood patterns, and how this may affect the risk of developing greater alcohol-related problems.
Highlights.
Restrained eaters consumed less alcohol during the follicular phase
Dysphoric mood increased during the late luteal and menstrual phases
Prospective data collection was advantageous for greater self-report accuracy
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations:
UN-RES – unrestrained eaters
RES- restrained eaters
References
- Beck AT, Steer RA, Brown GK. BDI-II Beck Depression Inventory Manual. 2nd ed. The Psychological Corp Harcourt Brace and Company; San Antonio, TX: 1996. [Google Scholar]
- Bowen DJ, Grunberg NE. Variations in food preference and consumption across the menstrual cycle. Physiology and Behavior. 1990;47(2):287–291. doi: 10.1016/0031-9384(90)90144-s. [DOI] [PubMed] [Google Scholar]
- Bradstock K, Forman MR, Binkin NJ, Gentry EM, Hogelin GC, Williamson DF, Trowbridge FL. Alcohol use and health behavior lifestyles among U.S. women: The behavioral risk factor surveys. Addictive Behaviors. 1988;13(1):61–71. doi: 10.1016/0306-4603(88)90026-3. [DOI] [PubMed] [Google Scholar]
- Bryant EJ, Kiezebrink K, King NA, Blundell JE. Interaction between disinhibition and restraint: Implications for body weight and eating disturbance. Eating and Weight Disorders. 2010;15(1-2):e43–51. doi: 10.1007/BF03325279. [DOI] [PubMed] [Google Scholar]
- Cahalan D, Cisin IH, Crossley HM. Quantity-frequency-variability index. In: Lettieri DJ, Nelson JE, Sayers MA, editors. NIAAA Treatment Handbook Series. Vol. 2. NIAAA; Rockville, MD: 1985. pp. 78–81. [Google Scholar]
- Charette L, Tate DL, Wilson A. Alcohol consumption and menstrual distress in women at higher and lower risk for alcoholism. Alcoholism: Clinical and Experimental Research. 1990;14(2):152–157. doi: 10.1111/j.1530-0277.1990.tb00462.x. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Cohen J, Halbreich U. Premenstrual changes: Patterns and correlates of daily ratings. Journal of Affective Disorders. 1986;10(2):127–135. doi: 10.1016/0165-0327(86)90035-2. [DOI] [PubMed] [Google Scholar]
- Evans SM, Haney M, Foltin RW. The effects of smoked cocaine during the follicular and luteal phases of the menstrual cycle in women. Psychopharmacology. 2002;159(4):397–406. doi: 10.1007/s00213-001-0944-7. [DOI] [PubMed] [Google Scholar]
- Evans SM, Levin FR. Response to alcohol in women: Role of the menstrual cycle and a family history of alcoholism. Drug and Alcohol Dependence. 2011;114(1):18–30. doi: 10.1016/j.drugalcdep.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SM, Levin FR. Differential response to alcohol in light and moderate female social drinkers. Behavioral Pharmacology. 2004;15(3):167–181. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview For DSM-IV axis I disorders, patient edition (SCID-I/P, version 2.0) Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- Freitag WJ, Adesso VJ. Mood effects of alcohol and expectancies across the menstrual cycle. Alcohol. 1993;10:291–298. doi: 10.1016/0741-8329(93)90008-c. [DOI] [PubMed] [Google Scholar]
- Gonda X, Telek T, Juhasz G, Lazary J, Vargha A, Bagdy G. Patterns of mood changes throughout the reproductive cycle in healthy women without premenstrual dysphoric disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2008;32:1782–1788. doi: 10.1016/j.pnpbp.2008.07.016. [DOI] [PubMed] [Google Scholar]
- Halbreich U, Endicott J, Schacht S, Nee J. The diversity of premenstrual changes as reflected in the Premenstrual Assessment Form. Acta Psychiatrica Scandinavica. 1982;65(1):46–65. doi: 10.1111/j.1600-0447.1982.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Higgs S, Eskenazi T. Dietary restraint and disinhibition are associated with Increased alcohol use behaviours and thoughts in young women social drinkers. Eating Behaviors. 2007;8:236–243. doi: 10.1016/j.eatbeh.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Holdstock L, deWit H. Effects of ethanol at four phases of the menstrual cycle. Psychopharmacology. 2000;150(4):374–382. doi: 10.1007/s002130000461. [DOI] [PubMed] [Google Scholar]
- Justice AH, de Wit H. Acute of d-amphetamine during the follicular and luteal phases of the menstrual cycle in women. Psychopharmacology. 1999;145(1):67–75. doi: 10.1007/s002130051033. [DOI] [PubMed] [Google Scholar]
- Kanarek RB, Ryu M, Przypek J. Preferences for foods with varying levels of salt and fat differ as a function of dietary restraint and exercise but not menstrual cycle. Physiological Behavior. 1995;57(5):821–826. doi: 10.1016/0031-9384(94)00341-2. [DOI] [PubMed] [Google Scholar]
- Kelly-Weeder S. Binge drinking and disordered eating in college students. Journal of the American Academy of Nurse Practitioners. 2010;23(1):33–41. doi: 10.1111/j.1745-7599.2010.00568.x. [DOI] [PubMed] [Google Scholar]
- Khaylis A, Trockel M, Taylor CB. Binge drinking in women at risk for developing eating disorders. International Journal of Eating Disorders. 2009;42(2):409–414. doi: 10.1002/eat.20644. [DOI] [PubMed] [Google Scholar]
- Krahn DD, Kurth CL, Gomberg E, Drewnowski A. Pathological dieting and alcohol use in college women- a continuum of behaviors. Eating Behaviors. 2005;6:43–52. doi: 10.1016/j.eatbeh.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Lavik NJ, Clausen SE, Pedersen W. Eating behaviour, drug use, psychopathology and parental bonding in adolescents in Norway. Acta Psychiatrica Scandinavica. 1991;84(4):387–390. doi: 10.1111/j.1600-0447.1991.tb03164.x. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Stacy AW. Alcohol outcome expectancies: Scale construction and predictive utility in higher order confirmatory models. Psychological Assessment. 1993;5(2):216–229. [Google Scholar]
- McLeod DR, Foster GV, Hoehn-Saric R, Svikis DS, Hipsley PA. Family history of alcoholism in women with generalized anxiety disorder who have premenstrual syndrome: patient reports of premenstrual alcohol consumption and symptoms of anxiety. Alcoholism, Clinical and Experimental Research. 1994;18(3):664–670. doi: 10.1111/j.1530-0277.1994.tb00928.x. [DOI] [PubMed] [Google Scholar]
- Mello NK, Mendelson JH, Lex BW. Alcohol use and premenstrual symptoms in social drinkers. Psychopharmacology. 1990;101(4):448–455. doi: 10.1007/BF02244221. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism [July 8, 2011];Rethinking drinking: Alcohol and your health. 2010 NIH Publication No. 10-3770, from http://rethinkingdrinking.niaaa.nih.gov/default.asp.
- Nyberg S, Wahlström G, Backström T, Sundström-Poromaa I. Altered sensitivity to alcohol in the late luteal phase among patients with premenstrual dysphoric disorder. Psychoneuroendocrinology. 2004;29(6):767–777. doi: 10.1016/S0306-4530(03)00121-5. [DOI] [PubMed] [Google Scholar]
- Pastor AD, Evans SM. Alcohol outcome expectancies and risk for alcohol use problems in women with and without a family history of alcoholism. Drug and Alcohol Dependence. 2003;70(2):201–214. doi: 10.1016/s0376-8716(03)00007-3. [DOI] [PubMed] [Google Scholar]
- Price WA, DiMarzio LR, Eckert JL. Correlation between PMS and alcoholism among women. Ohio Medicine. 1987;83(3):201–202. [PubMed] [Google Scholar]
- Reed SC, Levin FR, Evans SM. Changes in mood, cognitive performance and appetite in the late luteal and follicular phases of the menstrual cycle in women with and without PMDD (premenstrual dysphoric disorder). Hormone Behavior. 2008;54(1):185–193. doi: 10.1016/j.yhbeh.2008.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer ML, Vinokur A, Van Rooijen L. A self-administered version of the short Michigan Alcoholism Screening Test (SMAST). Journal of Studies on Alcohol. 1975;36(1):117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- Sheehan D, Janavs E, Knapp M, Sheehan R, Baker KH. Mini International Neuropsychiatric Interview, (MINI), Version 4.4. University of South Florida Institute for Research in Psychiatry; Tampa, FL: 1994. [Google Scholar]
- Sofuoglu M, Dudish-Poulsen S, Nelson D, Pentel PR, Hatsukami DK. Sex and menstrual cycle differences in the subjective effects from smoked cocaine in humans. Experimental and Clinical Psychopharmacology. 1999;7(3):274–283. doi: 10.1037//1064-1297.7.3.274. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory (”Self-Evaluation Questionnaire”) Consulting Psychologists Press; Palo Alto, CA: 1970. [Google Scholar]
- Stewart SH, Angelopoulos M, Baker JM, Boland FJ. Relations between dietary restraint and patterns of alcohol use in young adult women. Psychology of Addictive Behaviors. 2000;14(1):77–82. doi: 10.1037//0893-164x.14.1.77. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Svikis DS, Miles DR, Haug NA, Perry B, Hoehn-Saric R, McLeod D. Premenstrual symptomatology, alcohol consumption, and family history of alcoholism in women with premenstrual syndrome. Journal of Studies on Alcohol. 2006;67(6):833–836. doi: 10.15288/jsa.2006.67.833. [DOI] [PubMed] [Google Scholar]
- Terner JD, de Wit H. Menstrual cycle phase and responses to drugs of abuse in humans. Drug and Alcohol Dependence. 2006;84(1):1–13. doi: 10.1016/j.drugalcdep.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Whitty C, Jones RJ. A comparison of prospective and retrospective diary methods of assessing alcohol use among university undergraduates. Journal of Public Health. 1992;14(3):264–270. [PubMed] [Google Scholar]
- Xinaris S, Boland FJ. Disordered eating in relation to tobacco use, alcohol consumption, self-control, and sex-role ideology. International Journal of Eating Disorders. 1989;9(4):425–433. [Google Scholar]
- Yeomans MR, Coughlan E. Mood-induced eating. Interactive effects of restraint and tendency to overeat. Appetite. 2009;52(2):290–298. doi: 10.1016/j.appet.2008.10.006. [DOI] [PubMed] [Google Scholar]