Abstract
Objective
Lumbosacral transitional vertebrae (LSTV) are relatively common skeletal anomalies with a debated role in low back pain. There are few documented cases of conservative care being used to address LSTV-associated symptomatology. The current report discusses chiropractic management of 2 patients with unilateral sacralization.
Clinical Features
Two patients with LSTV involving unilateral sacralization of L5, a Castellvi type IIIa variant, presented with back pain to a chiropractic clinic. Each case presented with symptomatology similar to piriformis syndrome.
Intervention and Outcome
Manual therapy, including spinal manipulation soft tissue therapies and exercise/stretching, was used to address the presenting symptoms. Approximately 2 weeks after initial treatment, the first patient subjectively reported a 70% improvement in symptoms, with lumbar extension increased to full in active range of motion at the lumbar spine but with continued tenderness and hypertonicity at the left piriformis and gluteus medius. After 4 weeks of treatment, the second patient reported improvement in pain and perceived mobility, although prolonged standing remained an aggravating factor. Although both showed improvement, neither case resulted in complete resolution of symptoms.
Conclusion
The presenting cases demonstrated partial resolution of symptoms after chiropractic management. It is proposed that sacralization is a possible cause of back pain in these cases.
Key indexing terms: Lumbar vertebrae, Lumbosacral region, Congenital abnormalities
Introduction
Congenital variations involving malformed vertebrae take various forms. Lumbosacral transitional vertebrae (LSTV) are relatively common,1-6 with prevalence ranging anywhere from less than 1% of the population to more than 20%.2,4-6 The exact role of transitional vertebrae in low back pain is unknown, with some studies suggesting that transitional vertebrae increase the likelihood of, and are therefore reliable predictors of, low back pain,3,7-9 whereas others suggest that there is no greater prevalence of low back pain in those patients with transitional vertebrae when compared with the population at large.5,10,11
Incomplete LSTV variants that create partial or unilateral transitional elements can occur, but are less common.12 A review of the literature suggests that LSTV anomalies occur in approximately 7% of the population,12 although there are few documented cases.10,12-14 One case report15 describes a case of partial transitional lumbosacral vertebrae presenting as a Castellvi16 type IIb variant, where an accessory articulation was formed bilaterally between the elongated transverse processes (TVPs) of L5 and the sacrum, although links between congenital variations and back pain are not clear. Unilateral sacralization, termed by Castellvi as type IIIa variants, has been documented in the literature.10,12,13,17 However, no case reports have been reported to date that describe chiropractic care of patients with these anomalies. The purpose of this case report is to describe chiropractic care of 2 patients with unilateral sacralization.
Case reports
Consent for publication of clinical information was provided by the patients, providing that anonymity was maintained.
Case 1
A 51-year-old healthy female patient presented with left-sided low back pain (numeric pain scale, 6-7/10) of 8 years' duration. The pain was described as a constant dull ache in the lumbosacral and gluteal regions; sharp pains were noted in the left lumbar spine with certain movements. No radiation of pain to the leg was reported. Rising from a seated position and prolonged standing (ie, at work) were cited as aggravating factors; topical anti-inflammatory medication was cited as the only significant relieving factor.
Before presenting for chiropractic treatment, the patient was seen by her family physician, who had ordered lumbar spine radiographs. The radiographic report revealed the skeletal anomaly, and the patient was subsequently referred for a magnetic resonance imaging investigation to rule out nerve entrapment and/or disk involvement. Plain films of the lumbar spine showed mild L5/S1 facet arthrosis and an enlarged left TVP on the L5 vertebral body fused to the sacrum. Magnetic resonance imaging of the lumbar spine showed disk desiccation at L3/4 and L4/5, with disk bulges at L2/3, L3/4, and L4/5. Degenerative changes were noted throughout these levels. Hypertrophy of the ligamentum flavum was noted, resulting in mild but not significant narrowing of the spinal canal.
Postural examination revealed a mild “reversed S” scoliotic curve in the thoracolumbar spine, with left lateral tipping of the iliac crests. Lumbar spine range of motion was measured using a manual goniometer to be full in flexion and 22° in extension. Left lateral flexion was limited to 10°; right lateral flexion and rotation were otherwise normal. Orthopedic testing of the lumbar spine revealed a bilateral straight leg raise of 80°, with no leg pain reported. Results of Braggard and Ely tests were negative bilaterally for diskogenic pain. Thomas test result was negative bilaterally; Patrick-FABER, sacroiliac compression, and Yeoman test results were positive for sacroiliac joint irritation on the left. Neurological examination revealed deficits in deep tendon reflexes (1+) and strength (4/5) at L4 on the left; sensation was normal. Motion palpation revealed fixations in the lower lumbar spine and L5/S1 bilaterally although more pronounced on the left, with tender points noted in the left piriformis, gluteus medius, and erector spinae musculature. Palpation of the left piriformis muscle elicited referral of pain to the posterior left thigh. As no imaging was available at assessment, a preliminary diagnosis of piriformis syndrome was made; and treatment, including spinal manipulative therapy (SMT), myofascial release therapy (MRT) and trigger point therapy (TPT), was begun at a frequency of 3 treatments per week.
Diversified technique SMT was used during treatment, with the midlumbar spine and the sacroiliac junction providing the most consistent release (cavitation) during side-posture adjusting. Myofascial release therapy was directed to the left-sided gluteus medius and piriformis muscles. Myofascial release therapy was performed with the patient in side-lying position; for the gluteus medius muscle, treatment involved pressure applied to the gluteus medius (to the patient's tolerance) while the hip and knee were manually flexed by the practitioner, with the hip slightly adducted. Myofascial release therapy to the piriformis muscle involved this same side-lying posture and knee-to-chest movement, this time with pressure applied to the piriformis muscle and external hip rotation added to the manual movement at the point where 90° of both hip and knee flexion had been reached. In each case, 3 to 4 sets of 4 repetitions each were performed. Finally, TPT involved sustained pressure (to the patient's tolerance) to the muscle in question, either gluteus medius or piriformis, while the patient was in a prone lying position. Pressure was held for approximately 10 seconds or until the patient reported feeling a decrease in any pain associated with the pressure.
The treatment was tolerated well, although left-sided SMT did not result in an audible cavitation. Approximately 2 weeks after assessment, the patient subjectively reported a 70% improvement in her symptoms, with lumbar extension increased to full in active range of motion at the lumbar spine but with continued tenderness and hypertonicity at the left piriformis and gluteus medius. Proprioceptive neuromuscular facilitation stretching of the piriformis was introduced to the treatment and was tolerated well but did not result in significant improvements in piriformis range of motion during MRT. Treatment continued for 6 weeks, with the patient noting general improvements in range of motion and day-to-day pain levels, although nighttime pain related to prolonged held positions continued to be a limiting factor. Treatment frequency was decreased gradually, and the patient was seen for continued treatment once every 1 to 2 months. At the last treatment, pain levels were reported to be stable; but a general, nagging pain and tightness remained at the left piriformis muscle. Sleep was reportedly improved, with waking at night continuing to be problematic, although the patient reported greater ease in returning to sleep.
Case 2
A 62-year-old healthy female patient presented with left-sided low back pain (numeric pain scale, 8/10) of 2 years' duration. The pain was described as a constant “throbbing,” localized to the left-sided low back, in the gluteal and piriformis region. Radiation to the left lower leg in an L4/5 dermatomal pattern was reported as an accompanying symptom. Prolonged sitting, standing, or lying on the affected side was cited as an aggravating factor; no reliable relieving factors were cited. The patient reported a long history of low back pain, with her most recent episode following a fall at home.
Before the patient presented for chiropractic treatment, a computerized tomography (CT) scan of the lumbar spine was ordered by the patient's family physician as part of the initial investigations into the cause(s) of the chief concern. The patient provided copies of the report and the CT scan. The CT of the lumbar spine showed the left TVP of L5 fused to the sacral ala with a small (1.0 mm) joint space created between the TVP and the ilium. The anterior view revealed an enlarged left ilium, with the iliac crest to superior acetabular border distance measured at 8 mm greater on the left vs the right (Figs 1 and 2).
Fig 1.
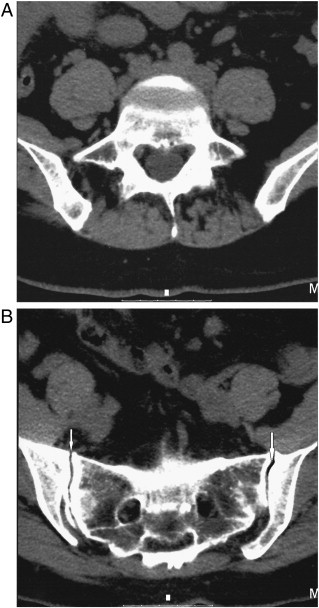
A, Computed tomographic scan of fifth lumbar vertebra. Vertebral body shape is well maintained. B, Computed tomographic scan of the sacroiliac joints. Sacroiliac joint space is well preserved (white arrows).
Fig 2.
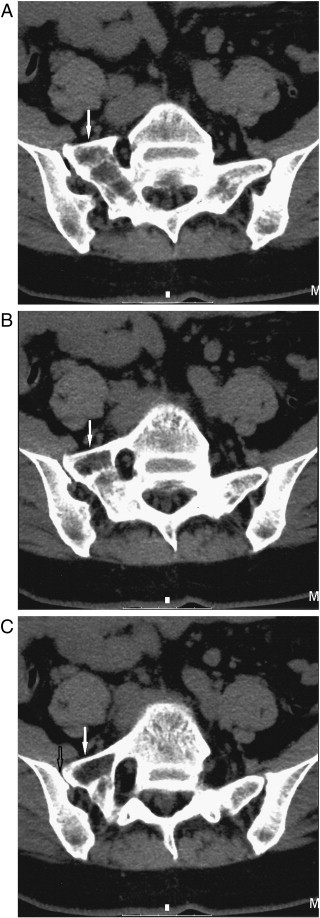
A and B, Sequential CT scan images of lumbosacral junction, from cephalad aspect (A) to caudal (C). Note malformation of left TVP of L5 (white arrows). C, Articulation between the malformed left TVP of L5 and the left ilium is visible (black arrow). TVP ilial articulation measures approximately 1.0 mm.
Postural examination revealed a mild decrease in the lordosis of the lumbar spine in both seated and standing postures. Lumbar spine range of motion was full, with pain at the end range of flexion. Orthopedic testing of the lumbar spine revealed a bilateral straight leg raise of 60° but with no leg pain reported. Results of Braggard and Ely tests were negative bilaterally for diskogenic pain. Thomas test, sacroiliac compression, and Yeoman test results were negative bilaterally; Patrick-FABER test result was positive for sacroiliac joint irritation on the left, with pain localized to the left piriformis muscle. Result of the neurological examination was unremarkable. Motion palpation revealed fixations in the lumbar spine and L5/S1 bilaterally, with tender points noted bilaterally in the erector spinae musculature at L4/5/S1. Referral of pain to the left posterior knee was noted on palpation of the left piriformis muscle. A preliminary diagnosis of left-sided piriformis syndrome was made; and a treatment plan, including SMT, MRT, and TPT 3 times per week, was proposed.
As with the patient in case 1, diversified, side-posture SMT was used, with the thoracolumbar junction (adjusted using supine-lying, anterior adjustments), midlumbar spine, and sacroiliac joints being the areas receiving treatment. Myofascial release and TPT to the gluteus medius and piriformis muscles were performed as described in the preceding case.
The patient was seen once weekly for 4 weeks, with MRT treatment tolerated well, although the initial plan for treatment 3 times per week was not possible because of scheduling. In general, the piriformis muscle responded well to manual therapies, demonstrating immediate improvements in range of motion associated with MRT maneuvers, although these changes were not long-lasting. Spinal mobilizations were tolerated well but were limited by decreased lumbosacral mobility; no audible release (cavitation) was noted at the lumbosacral junction with SMT.
After 4 weeks of treatment, the patient was forced to discontinue further treatment because of limited extended health care benefits. At discharge, a mild subjective improvement in pain level and perceived mobility was noted by the patient, although prolonged standing remained the most substantial aggravating factor. On palpation, a general decrease in muscle hypertonicity in the piriformis muscle was noted, as was slightly improved mobility in the lumbar spine.
Discussion
Lumbosacral transitional vertebrae occur at a prevalence of up to 20.8%,1-6 with LSTV anomalies such as unilateral sacralization occurring in up to 7.4% of the population.12 The correlation between such anomalies and low back pain, however, remains in question.7-9,11 The majority of the reported cases that require intervention are treated surgically,10,13,14,18-20 with little evidence available in the literature regarding conservative treatment of patients with such anomalies.21 This report summarizes 2 patients with unilateral sacralization who were treated with manual therapies.
In 1984, Castellvi et al17 proposed a system of categorization for LSTV. They proposed 4 specific types of LSTV variants, including those with (a) enlargement of the TVPs of L5, to a maximum width of 19 mm (Castellvi type Ia [unilateral] or Ib [bilateral]); (b) incomplete lumbarization/sacralization with enlarged TVPs that have diarthrodial joints between itself and the sacrum (type IIa [unilateral] or IIb [bilateral]); (c) lumbarization/sacralization with complete osseous fusion of the TVPs to the sacrum (type IIIa [unilateral] or IIIb [bilateral]); and (d) a combination of unilateral type II transition with a type III on the contralateral side (type IV). The variant in the cases discussed in this report is type IIIa.
The possible association between LSTV and low back pain remains a debated subject. Some have argued that altered biomechanics of weight transmission across the L5-S1 articulation result because LSTV are associated with altered morphology at the joint.22-27 These altered biomechanics are hypothesized to cause biomechanical compensations, which may partially explain the ipsilateral muscle hypertonicity noted in the current cases and by Brenner.21 Other investigators8 have suggested that LSTV increase the severity of the clinical picture, regardless of the causal relationship between LSTV and low back pain. Still others dismiss the association between LSTV and low back pain altogether.11
The majority of the literature on this subject is presented as case studies,10,13,14,18-21 the majority of which describe resolution of symptoms (low back pain, radicular symptoms) following surgical resection of the enlarged TVP and/or diskectomy.10,13,14,18-20 In addition, Weber and Ernestus19 described cases of 2 patients with unilateral LSTV who were treated with selective nerve blocks, which were successful in eliminating radicular symptoms and low back pain. Very little literature regarding conservative care for patients with LSTV is available, though. One recent report discusses the conservative treatment of a patient with a Castellvi type IIa variant, which differs from the current case, as that case involves an accessory articulation formed between the TVP and the sacral ala.21 In that case, symptoms presented as low back pain with radicular symptoms; and radiographs revealed the skeletal anomaly. The patient's symptoms resolved following a combination of manual therapies, stretching, and exercise.
In the cases discussed herein, pain presented in a similar fashion, initially as piriformis pain with referral, with imaging revealing the lumbosacral malformation. In each case, the skeletal anomaly limited ipsilateral flexion and coincided with ipsilateral muscular symptomatology. These findings seem to echo the arguments of Mahato,22-27 who suggested that the biomechanical alterations brought on by the skeletal anomaly could contribute to the symptomatology. Conservative treatment directed at the involved muscle group in these cases resulted in decreases in symptom frequency and intensity, although it did not result in complete resolution in either case. The key question, then, is this: does the skeletal anomaly play any type of role in the lumbosacral muscular symptomatology?
The majority of cases summarized in previous case studies involved radicular symptoms as the primary symptom.10,13,14,18-20 In the cases discussed here, only one presented with radicular symptoms, which closely mimicked the radicular symptoms often noted clinically in piriformis syndrome.28,29 Improvement in radicular symptomatology was not achieved with manual therapies in this case (no. 2), although extenuating circumstances resulted in treatment being discontinued after only 4 treatments. Whether continued treatment would have resulted in decreased radicular symptoms is unknown. In case 1, improvements in pain levels and mobility were noted following a course of manual treatment. If, as Mahato22-27 suggests, the decreased mobility at the L5/S1 junction resulted in biomechanical changes and altered weight distribution at this level, it is possible that these biomechanical changes increased the stress on the muscles in the region of the sacroiliac and lumbosacral junctions on the affected side, which resulted in the observed presentation. If that is the case, there is a possible role for conservative care in patients with this type of anomaly, not to relieve pressure on an impinged nerve but instead to address muscular alterations in the lumbopelvic musculature. Although the presence of ipsilateral muscle hypertonicity associated with skeletal anomaly and resolution of symptoms with conservative care suggests an association between Castellvi LSTV variants and low back pain, there are not enough data to draw a definitive conclusion. More work in this area is required.
Limitations
This report, while adding to the base of knowledge regarding this particular LSTV, has several limitations. Firstly, although case reports add to the body of knowledge on a subject and provide the impetus for further investigation, they offer preliminary information. The lack of a proper control and of pooled objective measures is a major limitation of case studies; thus, they cannot show causation. Secondly, the association between low back pain and LSTV remains in question. These factors combine to make it difficult to draw firm conclusions from the presented information. A possible avenue for further exploration could be to determine the prevalence of LSTV in patients with lumbosacral muscular symptoms and/or radiculopathy. This would help to determine the connection between LSTV and low back pain.
Conclusion
This report discusses 2 cases of Castellvi type IIIa lumbosacral malformations. Each case presented with piriformis-like symptomatology. Although the role of conservative care in Castellvi-type malformations is in question, this case adds to the current evidence in support of the use of conservative care in this type of presentation. With more research and future case reports, an acknowledged role for manual therapies may be proven to be valid.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Lu X., Hou C., Yuan W., Zhang Z., Chen A. Complete traumatic anterior dislocation of the lumbosacral joint: a case report. Spine (Phila Pa 1976) 2009;34(14):E488–E492. doi: 10.1097/BRS.0b013e3181a8cdad. [DOI] [PubMed] [Google Scholar]
- 2.Lee C.H., Park C.M., Kim K.A., Hong S.M., Seol H.Y., Kim B.H. Identification and prediction of transitional vertebrae on imaging studies: anatomical significance of paraspinal structures. Clin Anat. 2007;20(8):905–914. doi: 10.1002/ca.20540. [DOI] [PubMed] [Google Scholar]
- 3.Steinberg E.L., Luger E., Arbel R., Menachem A., Dekel S. A comparative roentgenographic analysis of the lumbar spine in male army recruits with and without lower back pain. Clin Radiol. 2003;58(12):985–989. doi: 10.1016/s0009-9260(03)00296-4. [DOI] [PubMed] [Google Scholar]
- 4.Kim N.H., Suk K.S. The role of transitional vertebrae in spondylolysis and spondylolytic spondylolisthesis. Bull Hosp Jt Dis. 1997;56(3):161–166. [PubMed] [Google Scholar]
- 5.Leboeuf C., Kimber D., White K. Prevalence of spondylolisthesis, transitional anomalies and low intercrestal line in a chiropractic patient population. J Manipulative Physiol Ther. 1989;12(3):200–204. [PubMed] [Google Scholar]
- 6.Magora A., Shwartz A. Relation between the low back pain syndrome and x-ray findings. 2. Transitional vertebra (mainly sacralization) Scand J Rehabil Med. 1978;10(3):135–145. [PubMed] [Google Scholar]
- 7.Dai L. Lumbosacral transitional vertebrae and low back pain. Bull Hosp Jt Dis. 1999;58(4):191–193. [PubMed] [Google Scholar]
- 8.Taskaynatan M.A., Izci Y., Ozgul A., Hazneci B., Dursun H., Kalyon T.A. Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine (Phila Pa 1976) 2005;30(8):E210–E213. doi: 10.1097/01.brs.0000158950.84470.2a. [DOI] [PubMed] [Google Scholar]
- 9.Bron J.L., van Royen B.J., Wuisman P.I. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007;73(6):687–695. [PubMed] [Google Scholar]
- 10.De Bernardi E. A rare finding in the lumbar column (unilateral dysmorphia of the lumbar transverse apophysis with sacral characteristics of the IV without sacralization of the V) Radiol Med. 1950;36(4):307–311. [PubMed] [Google Scholar]
- 11.Peterson C.K., Bolton J., Hsu W., Wood A. A cross-sectional study comparing pain and disability levels in patients with low back pain with and without transitional lumbosacral vertebrae. J Manipulative Physiol Ther. 2005;28(8):570–574. doi: 10.1016/j.jmpt.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Kamanli A., Genc H. Radiological abnormalities of the lumbosacral spine in young male individuals. J Back Musculo Rehab. 2002;16:91–94. doi: 10.3233/bmr-2002-162-307. [DOI] [PubMed] [Google Scholar]
- 13.Arseni C., Maretsis M. Paralyzing sciatica caused by unilateral sacralization. Presentation of a case. Neurol Psihiatr Neurochir. 1969;14(2):97–100. [PubMed] [Google Scholar]
- 14.Malawski S., Milecki M. Results of treatment of unilateral sacralization of transverse process of the fifth lumbar vertebrae. Chir Narzadow Ruchu Ortop Pol. 1998;63(5):487–494. [PubMed] [Google Scholar]
- 15.Muir JM. Partial lumbosacral transitional vertebrae: a case report of bilateral lumbosacral accessory articulation. J Chiropractic Med (in press). [DOI] [PMC free article] [PubMed]
- 16.Hsieh C.Y., Vanderford J.D., Moreau S.R., Prong T. Lumbosacral transitional segments: classification, prevalence, and effect on disk height. J Manipulative Physiol Ther. 2000;23(7):483–489. doi: 10.1067/mmt.2000.108817. [DOI] [PubMed] [Google Scholar]
- 17.Castellvi A.E., Goldstein L.A., Chan D.P. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9(5):493–495. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Miyoshi Y., Yasuhara T., Date I. Posterior decompression of far-out foraminal stenosis caused by a lumbosacral transitional vertebra—case report. Neurol Med Chir (Tokyo) 2011;51(2):153–156. doi: 10.2176/nmc.51.153. [DOI] [PubMed] [Google Scholar]
- 19.Weber J., Ernestus R.I. Transitional lumbosacral segment with unilateral transverse process anomaly (Castellvi type 2A) resulting in extraforaminal impingement of the spinal nerve: a pathoanatomical study of four specimens and report of two clinical cases. Neurosurg Rev. 2010;34(2):143–150. doi: 10.1007/s10143-010-0300-7. [DOI] [PubMed] [Google Scholar]
- 20.Abe E., Sato K., Shimada Y., Okada K., Yan K., Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976) 1997;22(7):823–826. doi: 10.1097/00007632-199704010-00023. [DOI] [PubMed] [Google Scholar]
- 21.Brenner A.K. Use of lumbosacral region manipulation and therapeutic exercises for a patient with a lumbosacral transitional vertebra and low back pain. J Orthop Sports Phys Ther. 2005;35(6):368–376. doi: 10.2519/jospt.2005.35.6.368. [DOI] [PubMed] [Google Scholar]
- 22.Mahato N.K. Facet dimensions, orientation, and symmetry at L5-S1 junction in lumbosacral transitional States. Spine (Phila Pa 1976) 2011;36(9):E569–E573. doi: 10.1097/BRS.0b013e3181f6ecb2. [DOI] [PubMed] [Google Scholar]
- 23.Mahato N.K. Morphological traits in sacra associated with complete and partial lumbarization of first sacral segment. Spine J. 2010;10(10):910–915. doi: 10.1016/j.spinee.2010.07.392. [DOI] [PubMed] [Google Scholar]
- 24.Mahato N.K. Morphometric analysis and identification of characteristic features in sacra bearing accessory articulations with L5 vertebrae. Spine J. 2010;10(7):616–621. doi: 10.1016/j.spinee.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Mahato N.K. Complete sacralization of L5 vertebrae: traits, dimensions, and load bearing in the involved sacra. Spine J. 2010;10(7):610–615. doi: 10.1016/j.spinee.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Mahato N.K. Association of rudimentary sacral zygapophyseal facets and accessory and ligamentous articulations: implications for load transmission at the L5-S1 junction. Clin Anat. 2010;23(6):707–711. doi: 10.1002/ca.21009. [DOI] [PubMed] [Google Scholar]
- 27.Mahato N.K. Variable positions of the sacral auricular surface: classification and importance. Neurosurg Focus. 2010;28(3):E12. doi: 10.3171/2009.12.FOCUS09265. [DOI] [PubMed] [Google Scholar]
- 28.Hopayian K., Song F., Riera R., Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010;19(12):2095–2109. doi: 10.1007/s00586-010-1504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirschner J.S., Foye P.M., Cole J.L. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009;40(1):10–18. doi: 10.1002/mus.21318. [DOI] [PubMed] [Google Scholar]


