Abstract
Spinal epidural lipomatosis (SEL) is a rare but well-recognized condition. In general, the onset of its symptoms is insidious and the disease progresses slowly. We report two cases of rapid progression of SEL with no history of steroid intake in non-obese individuals after epidural steroid injection. These SEL patients developed neurologic symptoms after less than 5 months; these symptoms were confirmed to be due to SEL by serial MR images. After the debulking of the epidural fat, their symptoms improved.
Keywords: Spinal epidural lipomatosis, Epidural steroid injection
Introduction
Spinal epidural lipomatosis (SEL) is characterized by an excessive deposition of unencapsulated adipose tissue in the spinal canal. SEL has been implicated as a cause of back pain, radiculopathy, claudication, and paraparesis. SEL is a rare but well-recognized condition [1]. SEL is associated with exogenous steroid therapy, Cushing’s syndrome, and obesity [2–4]. In general, the onset of symptoms is steady, with a slow progression of neurologic findings. We introduce the cases of rapid progression of epidural lipomatosis.
Case 1
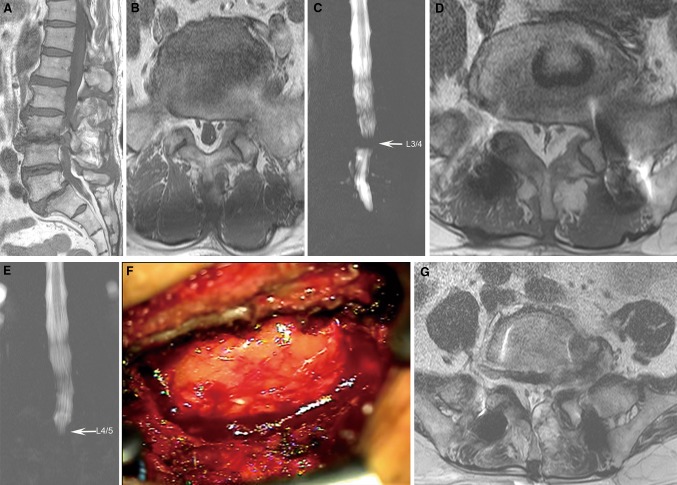
A 67-year-old man presented with back and left leg radiating pain. The patient had hypertension that was well controlled with an antihypertensive drug. His weight was 80 kg, and his height was 177 cm (Body mass index, BMI; 25.5 kg/m2). A plain X-ray showed isthmic spondylolisthesis at L5/S1. Magnetic resonance (MR) images showed an extruded disc at L3/4 and minimal epidural lipomatosis and a clear thecal sac in the lumbosacral spine (Fig. 1a, b). An MR myelogram revealed a complete block at L3/4 (Fig. 1c). He had undergone anterior lumbar interbody fusion (ALIF) at L5/S1 and bilateral removal of a herniated disc via laminectomy at L3/4. After surgery, his pain got disappeared. Five months after surgery, the patient complained of back pain, leg tightness in both legs and neurogenic claudication. MR images showed extensive epidural lipomatosis of the lumbosacral spine with significant constrictive compression of the thecal sac (Fig. 1d). An MR myelogram showed a complete block below L4/5 (Fig. 1e). After removal of lipomatosis (Fig. 1f) via laminectomy of L4/5 and L5/S1 (Fig. 1g), his symptoms improved. Histologic analysis revealed unencapsulated adipose tissue.
Fig. 1.
a T1-weighted sagittal MR image showing an extruded disc at L3/4 and isthmic spondylolisthesis at L5/S1. b T1-weighted axial MR image showing minimal epidural lipomatosis at L5/S1. c MR myelogram showing a complete block at L3/4. d Five months after checking initial MR image, T1-weighted axial image showing extensive epidural fat encasing the thecal sac circumferentially with a Y-shaped configuration at L5/S1. e MR myelogram showing a complete block at L4/5. f Intraoperative photograph showing abundant fat tissue encasing the thecal sac. g Postoperative T2-weighted axial MR image showing well decompressed the thecal sac and the nerve root with minimal epidural hematoma
He had not experienced weight gain recently. He had taken non-steroidal anti-inflammatory drugs for his leg pain for several months and had been given two epidural steroid injections (triamcinolone, 40 mg) at L4/5 before the ALIF procedure 1 month prior. However, the patient had taken only anti-hypertensive medication after ALIF. We referred the patient to another university hospital for endocrinopathy. His hormone levels, including cortisol and thyroid hormones, were normal.
Case 2
A 64-year-old man presented with back pain after falling. The patient was only taking anti-hypertensive medication. His height and weight were 157 cm and 55.4 kg, respectively (BMI 22.5 kg/m2). His diagnosis was a compression fracture at T11 and L2. MR images and myelography also showed degenerative spondylolisthesis and spinal stenosis at L4-5 (Fig. 2a, b) and minimal lipomatosis in the lumbosacral spine (Fig. 2c). The mean T-score for the bone mineral density was −1.8. The patient underwent percutaneous vertebroplasty (PVP) at T11 and L2. Five months later, the patient visited our institute for severe back pain and claudication. The patient had an epidural steroid injection (triamcinolone, 40 mg) at L4–5 in another pain clinic 4 months prior to this visit. His height and weight were 155 cm and 54 kg, respectively. His basal hormone levels were normal. Recently, MR images showed a compression fracture of L3 and L5. Extensive lipomatosis encasing the thecal sac was found in the lumbosacral spine (Fig. 2d). MR myelography revealed cerebrospinal fluid (CSF) flow narrowing at L5/S1 (Fig. 2e). We simultaneously performed bilateral removal of the ligamentum flavum and the abundant fat tissue via unilateral laminectomy and PVP at L3 and L5. After surgery, the patient’s pain was greatly reduced (Fig. 2f).
Fig. 2.
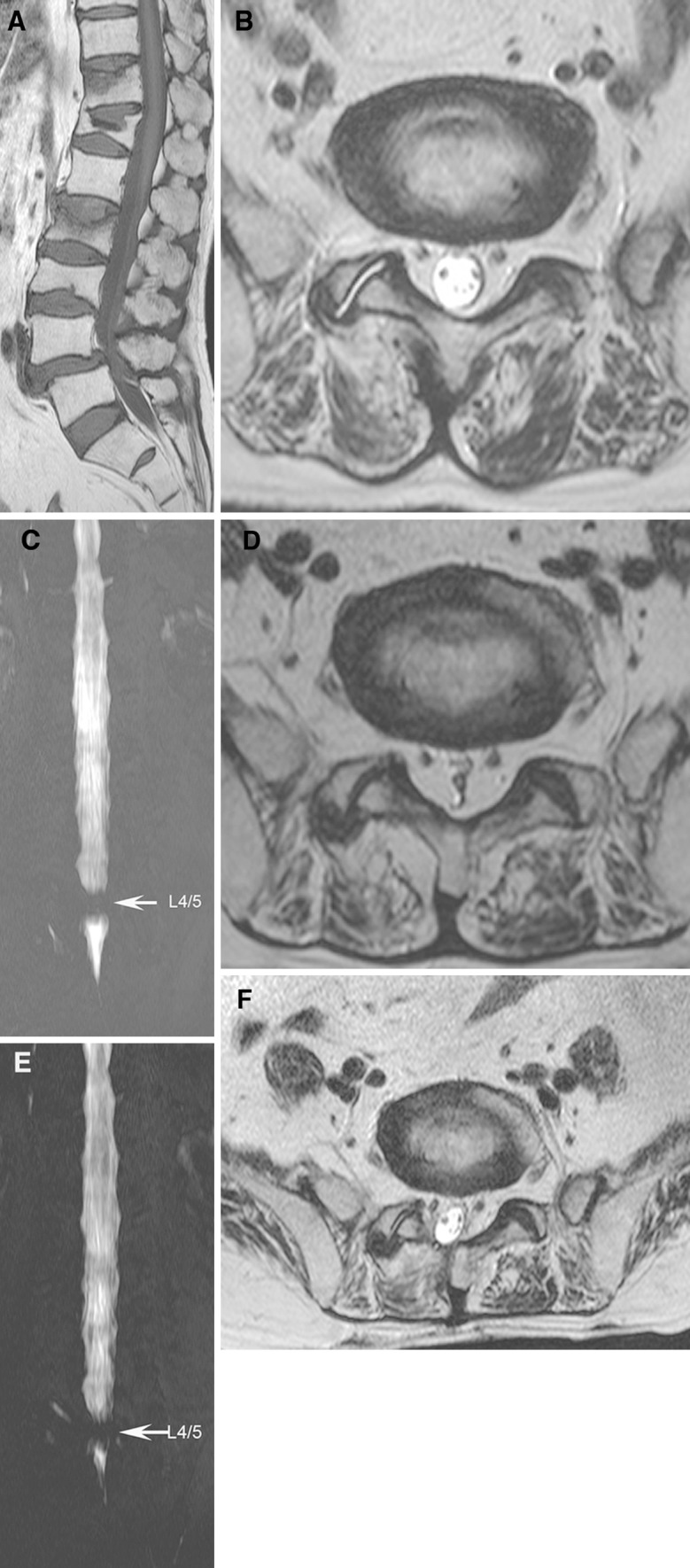
a T1-sagittal image showing acute compression fractures at T11 and L2 and degenerative spondylolisthesis at L4/5. b T2-weighted axial image showing minimal epidural lipomatosis at L5/S1. c MR myelogram showing a complete block at L4/5 and clear CSF flow at L5–S1. d Five months after checking initial MR image, T2-weighted axial image showing extensive epidural fat circumferentially compressing the thecal sac at L5/S1. e MR myelogram showing a complete block at L4–5 and constrictive narrowing at L5–S1. f Postoperative T2-weighted MR image showing well decompressed the thecal sac
Discussion
Steroid-induced SEL was first diagnosed in a patient in 1975 by Lee et al. [5]. In SEL, overgrowth of adipose tissue in the epidural space causes compression of the spinal canal. Back pain is the most commonly reported symptom [6]. The symptoms usually depend on the level of canal compromise. SEL at the thoracic levels produces myelopathy, and SEL at the lumbar levels results in radiculopathy caused by direct mechanical compression and indirect vascular dysfunction [7]. According to the literature, SEL is associated with exogenous steroid intake, obesity, and Cushing’s syndrome [1]. A number of cases of idiopathic SEL have also been reported [8, 9]. SEL is the most frequently reported in patients on long-term steroid therapy or in patients with Cushing’s syndrome. Centripetal fat deposition associated with steroid use occurs in the trunk, neck, face, and midline structure. The pathogenesis of the excessive fat deposition associated with SEL still remains to be unclear. Feldman et al. [10] suggested that adipose tissue expresses glucocorticoid receptors. Thus, it is believed that steroids promote the hypertrophy of fat tissue that is normally present in the epidural space. The time interval of the progression of SEL is rarely reported. Serial MR images before and after development of SEL are not available for many SEL cases. Therefore, it is difficult to determine the time interval of progression. Clinically, in general, the onset of symptoms is gradual and the condition progresses slowly [6, 8]. For patients taking systemic steroid therapy, the time interval between the initiation of steroid use and the onset of neurologic deficit is an average of 19 months [11]. In obese individuals, the average symptom duration is about 20 months [12]. Both of the cases reported herein underwent epidural steroid injection without long-term intake of steroids. In the first case, the patient was given two epidural steroid injections before ALIF. Six months after the steroid injections, SEL progressed rapidly. In the second case, the patient was given one epidural steroid injection. Five months later, SEL progressed rapidly and was symptomatic. Roy-Camille et al [13]. reported first a SEL after lumbar epidural steroid injection. Then, four cases associated with epidural steroid injection have been reported [14–17]. We summarized five reported cases in Table 1. Kinds of steroid were triamcinolone acetonide and methylprednisolone acetate. Amounts of steroid and duration of the use varied considerably. Although MR images were not obtained before the epidural injection in all cases, the clinical and radiological data indicated that the progression of SEL was relatively rapid. Especially, two cases progressed rapidly similar to our cases. Four cases resulted in good outcome by decompressive surgery. Only one case treated conservatively. The pathogenesis of SEL associated with epidural steroid injection is unknown. Epidural steroid injection has potential systemic effects that suppress the hypothalamic–pituitary–adrenal axis, induce hypertension, elevate glucose level, and affect bone growth [18, 19]. Injected steroids in the epidural space penetrate into the blood stream and may promote fat deposition in the epidural space.
Table 1.
Summary of reported spinal epidural lipomatosis after epidural steroid injection
| Case no | Author | Age/sex | Level | Steroid | Total of dosage of steroid (mg) | Duration of steroid use | Imaging | Interval of imaging | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Roy-Cammille et al. | 64/F | T10–L2 | Methylprednisolone acetate | 4,120 | Unknown | Myelography after steroid use | a | Laminectomy T10–L2 | Improved |
| 2 | Tok et al. | 45/M | L4–5 | Triamcinolone acetonide | 40 | 3 months | MRI before and after steroid use | 3 months | Laminotomy L1–4, Laminectomy L5, PLF | Improved |
| 3 | Sandberg et al. | 68/M | L2–3 | Triamcinolone acetonide | 240 | 3 months | MRI before and after steroid use | 6 months | Laminectomy L2–5 | CR |
| 4 | McCullen et al. | 61/F | L4–5–S1 | Methylprednisolone acetate | 1,200 | 4 years | MRI before and after steroid use | 4 years | Conservative | CR |
| 5 | Kim et al. | 59/F | L3–S1 | Triamcinolone acetonide | 760 | 3 years | MRI after steroid use | – | Laminectomy L3–S1 | CR |
CR Complete recovery
aThe authors did not check radiologic image before epidural steroid injection
Conclusion
These cases of the SEL caused by epidural steroid injection progressed exceptionally rapid and compromised neural structures.
Acknowledgments
This study was supported by a grant from the Wooridul Spine Foundation.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Fogel GR, Cunningham PY, 3rd, Esses SI. Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine J. 2005;5:202–211. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 2.Chapman PH, Martuza RL, Poletti CE, Karchmer AW. Symptomatic spinal epidural lipomatosis associated with Cushing’s syndrome. Neurosurgery. 1981;8:724–727. doi: 10.1227/00006123-198106000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Guegan Y, Fardoun R, Launois B, Pecker J. Spinal cord compression by extradural fat after prolonged corticosteroid therapy. J Neurosurg. 1982;56:267–269. doi: 10.3171/jns.1982.56.2.0267. [DOI] [PubMed] [Google Scholar]
- 4.Maillot F, Mulleman D, Mammou S, Goupille P, Valat JP. Is epidural lipomatosis associated with abnormality of body fat distribution? A case report. Eur Spine J. 2006;15:105–108. doi: 10.1007/s00586-005-0955-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee M, Lekias J, Gubbay SS, Hurst PE. Spinal cord compression by extradural fat after renal transplantation. Med J Aust. 1975;1:201–203. doi: 10.5694/j.1326-5377.1975.tb111328.x. [DOI] [PubMed] [Google Scholar]
- 6.Fassett DR, Schmidt MH (2004) Spinal epidural lipomatosis: a review of its causes and recommendations for treatment. Neurosurg Focus 16:E11. pii160411 [PubMed]
- 7.Al-Khawaja D, Seex K, Eslick GD (2008) Spinal epidural lipomatosis—a brief review. J Clin Neurosci 15:1323–1326. doi:10.1016/j.jocn.2008.03.001 [DOI] [PubMed]
- 8.Akhaddar A, Ennouali H, Gazzaz M, Naama O, Elmostarchid B, Boucetta M (2008) Idiopathic spinal epidural lipomatosis without obesity: a case with relapsing and remitting course. Spinal Cord 46:243–244. doi:10.1038/sj.sc.3102099 [DOI] [PubMed]
- 9.Lopez-Gonzalez A, Resurreccion Giner M (2008) Idiopathic spinal epidural lipomatosis: urgent decompression in an atypical case. Eur Spine J 17(Suppl 2):S225–227. doi:10.1007/s00586-007-0465-0 [DOI] [PMC free article] [PubMed]
- 10.Feldman D, Loose D. Glucocorticoid receptors in adipose tissue. Endocrinology. 1977;100:398–405. doi: 10.1210/endo-100-2-398. [DOI] [PubMed] [Google Scholar]
- 11.Russell NA, Belanger G, Benoit BG, Latter DN, Finestone DL, Armstrong GW. Spinal epidural lipomatosis: a complication of glucocorticoid therapy. Can J Neurol Sci. 1984;11:383–386. doi: 10.1017/s0317167100045765. [DOI] [PubMed] [Google Scholar]
- 12.Pouchot J, Si-Hassen C, Damade R, Bayeux MC, Mathieu A, Vinceneux P. Cauda equina compression by epidural lipomatosis in obesity. Effectiveness of weight reduction. J Rheumatol. 1995;22:1771–1775. [PubMed] [Google Scholar]
- 13.Roy-Camille R, Mazel C, Husson JL, Saillant G (1991) Symptomatic spinal epidural lipomatosis induced by a long-term steroid treatment. Review of the literature and report of two additional cases. Spine (Phila Pa 1976) 16:1365–1371 [DOI] [PubMed]
- 14.Kim HS, Han IH, Lee JH, Choi BK. Symptomatic spinal epidural lipomatosis induced by repeated epidural steroid injections. Korean J Spine. 2009;6:218–220. [Google Scholar]
- 15.McCullen GM, Spurling GR, Webster JS. Epidural lipomatosis complicating lumbar steroid injections. J Spinal Disord. 1999;12:526–529. doi: 10.1097/00002517-199912000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Sandberg DI, Lavyne MH. Symptomatic spinal epidural lipomatosis after local epidural corticosteroid injections: case report. Neurosurgery. 1999;45:162–165. doi: 10.1097/00006123-199907000-00037. [DOI] [PubMed] [Google Scholar]
- 17.Tok CH, Kaur S, Gangi A (2011) Symptomatic spinal epidural lipomatosis after a single local epidural steroid injection. Cardiovasc Intervent Radiol. doi:10.1007/s00270-010-9982-z [DOI] [PubMed]
- 18.Emkey RD, Lindsay R, Lyssy J, Weisberg JS, Dempster DW, Shen V. The systemic effect of intraarticular administration of corticosteroid on markers of bone formation and bone resorption in patients with rheumatoid arthritis. Arthritis Rheum. 1996;39:277–282. doi: 10.1002/art.1780390215. [DOI] [PubMed] [Google Scholar]
- 19.Younes M, Neffati F, Touzi M, Hassen-Zrour S, Fendri Y, Bejia I, Ben Amor A, Bergaoui N, Najjar MF. Systemic effects of epidural and intra-articular glucocorticoid injections in diabetic and non-diabetic patients. Joint Bone Spine. 2007;74:472–476. doi: 10.1016/j.jbspin.2006.10.009. [DOI] [PubMed] [Google Scholar]