Abstract
Introduction
Destructive spondyloarthropathy may occur in long-term hemodialysis patients, but focal amyloid deposits in the spine are rare. We present a case of upper cervical extradural amyloidoma with a history of long-term hemodialysis presenting with progressive and intractable radiculopathy.
Clinical presentation
We describe a 51-year-old female with a long-term history of hemodialysis treatment. She suffered progressive and intolerable right occipital headache. Neurological examination revealed right C2 radiculopathy. Magnetic resonance imaging (MRI) of the cervical spine showed a solid focal extradural mass lesion at the C2 level. She underwent subtotal resection of the extradural mass lesion and decompression of the right C2 nerve root by a posterior approach. Histological examination revealed amyloid deposits. The occipital headache immediately disappeared after surgery. Follow-up MRI 10 months after surgery demonstrated no recurrence of the extradural amyloidoma.
Conclusion
Development of an upper cervical extradural amyloidoma after long-term hemodialysis is extremely rare. Prompt evaluation of long-term hemodialysis patients suffering from progressive cervical pain should be recommended, and treatment is required if there are signs or symptoms of compression of a nerve root or the spinal cord.
Keywords: Amyloidoma, Cervical, Extradural, Hemodialysis, Radiculopathy
Introduction
Chronic kidney disease is becoming increasingly prevalent, but concurrently life expectancy is increasing. There has been considerable interest in hemodialysis-related disorders because of the increasing number of hemodialysis patients in developed countries [1, 2].
Hemodialysis-related amyloidosis is a unique type of amyloidosis affecting patients undergoing long-term hemodialysis. It involves deposition of amyloid fibrils containing β2-microglobulin in collagen tissue (particularly in the synovia of joints and tendons) and in subchondral bone [3, 4]. The most common manifestations are carpal tunnel syndrome and arthropathy of the shoulders, knees, hips, and axial skeleton [4].
Although destructive spondyloarthropathy (DSA) may occur in long-term hemodialysis patients, amyloid depositions are less common and have been reported only sporadically. In addition, focal masses of amyloid that are not diffusely deposited are rare [5]. We describe a rare case of an upper cervical extradural mass lesion, a hemodialysis-related amyloidoma, presenting with progressive and intractable radiculopathy.
Case report
We describe the case of a 51-year-old female with chronic renal insufficiency and a 29-year history of hemodialysis treatment. She suffered a progressive right occipital headache which over 3 months became intolerable.
She then visited our hospital. Neurological examination revealed radicular pain in the right C2 area with a positive Jackson’s test. Roentgenography and computed tomography of the cervical spine did not reveal a destructive bone lesion. However, magnetic resonance imaging (MRI) of the cervical spine showed a solid focal extradural mass lesion at the C2 level with predominantly low signal intensity on T2-weighted images (Fig. 1).
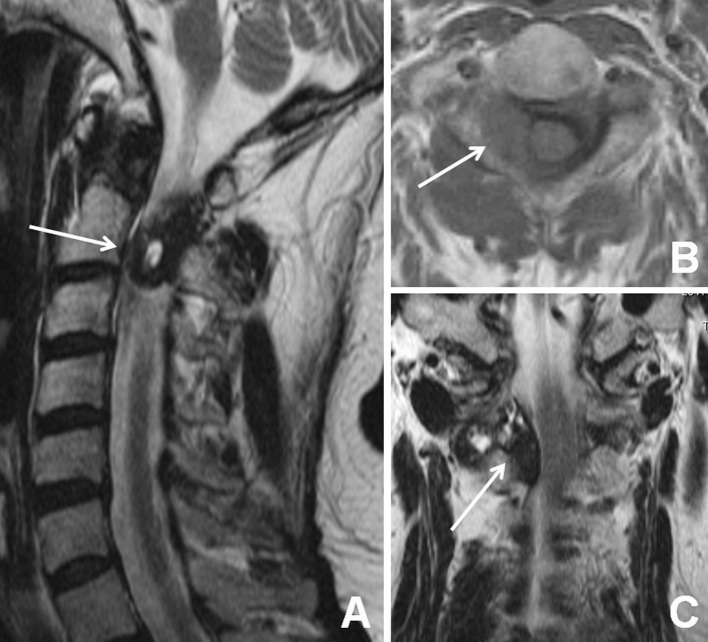
Fig. 1.
Initial magnetic resonance images of the patient. a Right paramedian sagittal T2-weighted image of the cervical spine. A low signal intensity mass lesion with a hyperintense signal at the center can be observed in the spinal canal at the C1–2 level (arrow). b Axial T1-weighted image of the cervical spine at the C2 level. A mass lesion of homogenous low signal intensity can be observed in the right extradural space (arrow). c Coronal T2-weighted image of the cervical spine. A “dumbbell-shaped” extradural mass lesion of mixed signal intensity can be observed in the right C1–2 intervertebral space with compression of the spinal cord (arrow)
She underwent hemilaminectomies on the right side of the C1 and C2 laminae, subtotal resection of the extradural mass lesion, and decompression of the right C2 nerve root using a posterior approach. Intraoperative findings were a mass lesion covered by a reactive membrane. The latter was hypovascularized waxy tissue without a relationship with a yellow ligament at the C2–3 level or the posterior atlantoaxial membrane (Fig. 2). Histological examination revealed amyloid deposits (Fig. 3). The occipital headache immediately disappeared after surgery. A soft neck collar was applied after surgery. She was discharged from the hospital without neurological manifestations on the 14th postoperative day. Follow-up MRI 10 months after surgery demonstrated no recurrence of the extradural amyloidoma (Fig. 4).
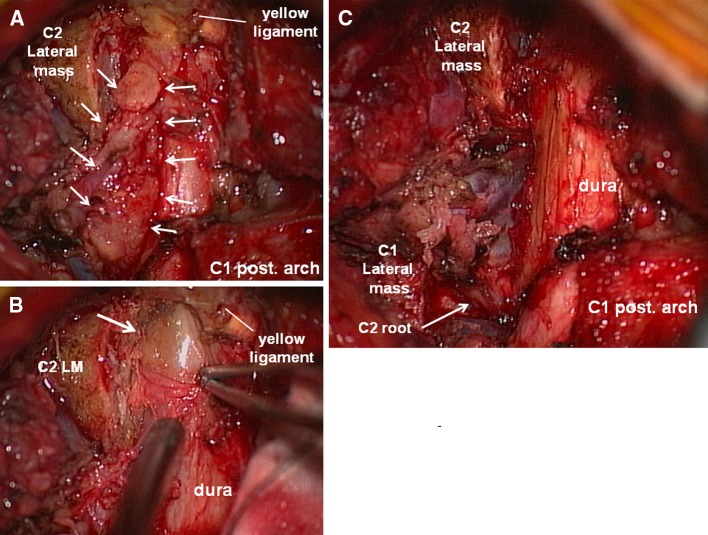
Fig. 2.
Intraoperative photographs of the patient. a Microscopic view after C1 and C2 hemilaminectomy on the right side. A waxy mass can be observed in the extradural space that extends laterally through the C1–2 intervertebral space (arrow). b A photograph after partial resection of the yellow ligament at the C2–3 level. A yellowish mass within the reactive outer membrane can be observed in the subligamentous extradural space without attachment to the yellow ligament. c Final microscopic view after resection of the mass lesion. The dural sac and right C2 nerve root (arrow) are decompressed and the ventral venous plexus can be observed
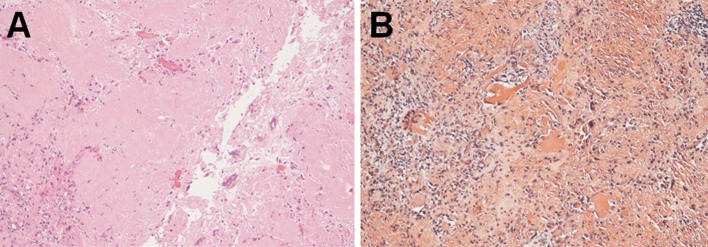
Fig. 3.
Photomicrographs of a surgical specimen. a Histological finding with hematoxylin and eosin staining shows extracellular tissue composed of amorphous and eosinophilic material. b Amyloid fibrils are densely enhanced with direct fast scarlet staining
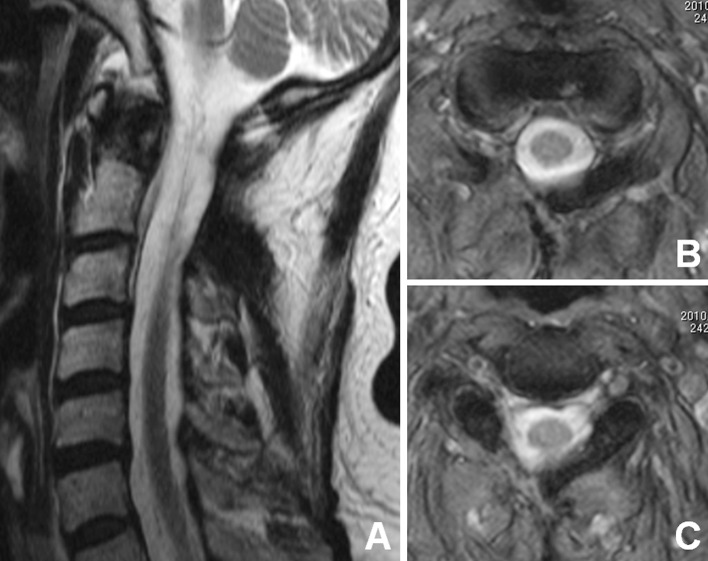
Fig. 4.
Magnetic resonance images of the patient 10 months after surgery. Right paramedian sagittal T2-weighted image of the cervical spine (a) shows disappearance of the mass lesion. Axial T2-weighted images at the C2 level (b, c) show decompression of the spinal cord
Discussion
Hemodialysis-related spondyloarthropathy has been divided into three types: destructive spondyloarthropathy, amyloid deposition in spinal ligaments, and pseudotumor of the craniocervical junction. DSA, first proposed by Kuntz et al. [6], is destructive peridiscal arthritis. It may involve a soft-tissue mass containing deposition of amyloid or crystals. Amyloid deposition in spinal ligaments was first reported in regard to extradural amyloid deposits by Allain et al. [7] in 1988. Thickening of the ligamentum flavum with an inflammatory reaction was observed at the same time, and both the deposits and the ligament demonstrated amyloid deposition by immunostaining with anti-β2-microglobulin [8]. Retro-odontoid pseudotumors have been observed in hemodialysis patients for over 10 years by systematic MRI with a incidence of 20–30%, and are often neurologically asymptomatic [9].
Amyloid deposits are potentially observed in DSA and amyloid deposition in spinal ligaments. These amyloid deposits are, in general, diffuse in distribution. Conversely, cervical focal amyloidoma is unusual in hemodialysis-related amyloidosis [5]. Hemodialysis-related amyloidoma in the lateral mass of atlas and dens of axis was reported by Oruckaptan et al. [10] in 2009. In a case report by Vignes et al. [5] of hemodialysis-related cervical extradural amyloidoma at C3 (which was close to our case with respect to localization but not identical), the yellowish pseudotumor was very firm, highly vascularized, and very strongly attached to a thick ligamentum flavum. Different to the present case, the hypovascularized amyloidoma was covered with a reactive membrane in the extradural space and not attached strongly to the yellow ligament at C2–3 level. In general, at the atlantoaxial level, there are posterior atlantoaxial membranes between the C1 posterior arch and C2 lamina alternative to the yellow ligaments at the level below. Intraoperative findings in the present case also demonstrated that the deposit was not related to the posterior atlantoaxial membrane. Furthermore, no relationship was confirmed between the deposits and the right atlantoaxial facet joint. The course of deposition in the present case was unpredictable.
The mechanism of development of amyloidosis is still controversial [5]. Ito et al. [11] reported that amyloid deposits were densely distributed at the enthesis of capsular fibers to the bone and in annular tears in the intervertebral disks. Even if amyloid fibrils deposit in the extradural loose connective space, the reason why deposition at the level occurs focally with laterality is unclear. Focal cervical amyloidoma must be considered in the differential diagnosis of a cervical mass lesion, particularly in long-term hemodialysis patients.
The best treatment of hemodialysis-related amyloidosis is renal transfusion [12], recently there have been considerable interest in β2-microglobulin adsorption column [13]. Because the clinical presentation was mostly caused by a mass effect to the spinal root or spinal cord [3, 4, 7, 14–16], medical therapy is limited to symptomatic approaches to lessen pain and inflammation in joints [3]. Therefore, prompt evaluation of long-term hemodialysis patients suffering from cervical pain should be emphasized so that they can be referred for surgical evaluation.
Conclusion
Hemodialysis-related extradural amyloidomas are extremely rare. However, they should be considered in the differential diagnosis of spinal mass lesion, particularly in long-term hemodialysis patients. Prompt evaluation of long-term hemodialysis patients suffering from progressive cervical pain should be recommended. Treatment is required if there are signs or symptoms of compression of nerve roots or the spinal cord.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Jassal SV, Trpeski L, Zhu N, Fenton S, Hemmelgarn B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ. 2007;177:1033–1038. doi: 10.1503/cmaj.061765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Genestier S, Meyer N, Chantrel F, Alenabi F, Brignon P, Maaz M, Muller S, Faller B. Prognostic survival factors in elderly renal failure patients treated with peritoneal dialysis: a nine-year retrospective study. Perit Dial Int. 2010;30:218–226. doi: 10.3747/pdi.2009.00043. [DOI] [PubMed] [Google Scholar]
- 3.Danesh FR, Klinkmann J, Yokoo H, Ivanovich P. Fatal cervical spondyloarthropathy in a hemodialysis patient with systemic deposition of beta2-microglobulin amyloid. Am J Kidney Dis. 1999;33:563–566. doi: 10.1016/S0272-6386(99)70195-2. [DOI] [PubMed] [Google Scholar]
- 4.Moslavac S, Dzidic I, Kejla Z, Tomas D. Hemodialysis-associated amyloidosis with cervical spinal cord compression and incomplete tetraplegia: a case report. Spinal Cord. 2007;45:799–801. doi: 10.1038/sj.sc.3102112. [DOI] [PubMed] [Google Scholar]
- 5.Vignes JR, Eimer S, Dupuy R, Donois E, Liguoro D. Beta(2)-microglobulin amyloidosis caused spinal cord compression in a long-term haemodialysis patient. Spinal Cord. 2007;45:322–326. doi: 10.1038/sj.sc.3101969. [DOI] [PubMed] [Google Scholar]
- 6.Kuntz D, Naveau B, Bardin T, Drueke T, Treves R, Dryll A. Destructive spondylarthropathy in hemodialyzed patients. A new syndrome. Arthritis Rheum. 1984;27:369–375. doi: 10.1002/art.1780270402. [DOI] [PubMed] [Google Scholar]
- 7.Allain TJ, Stevens PE, Bridges LR, Phillips ME. Dialysis myelopathy: quadriparesis due to extradural amyloid of beta 2 microglobulin origin. Br Med J (Clin Res Ed) 1988;296:752–753. doi: 10.1136/bmj.296.6624.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nokura K, Koga H, Yamamoto H, Kimura A, Tamai H, Yazaki S, Suzuki N, Miyazaki S, Niwa T. Dialysis-related spinal canal stenosis: a clinicopathological study on amyloid deposition and its AGE modification. J Neurol Sci. 2000;178:114–123. doi: 10.1016/S0022-510X(00)00377-4. [DOI] [PubMed] [Google Scholar]
- 9.Rousselin B, Helenon O, Zingraff J, Delons S, Drueke T, Bardin T, Moreau JF. Pseudotumor of the craniocervical junction during long-term hemodialysis. Arthritis Rheum. 1990;33:1567–1573. doi: 10.1002/art.1780331015. [DOI] [PubMed] [Google Scholar]
- 10.Oruckaptan H, Karli Oguz K, Isikay I, Ruacan S. Amyloidoma of the temporal bone and upper cervical spine; presentation of a rare clinical entity with a brief literature review. Turk Neurosurg. 2009;19:159–162. [PubMed] [Google Scholar]
- 11.Ito M, Abumi K, Takeda N, Satoh S, Hasegawa K, Kaneda K. Pathologic features of spinal disorders in patients treated with long-term hemodialysis. Spine (Phila Pa 1976) 1998;23:2127–2133. doi: 10.1097/00007632-199810010-00018. [DOI] [PubMed] [Google Scholar]
- 12.Jadoul M, Drueke T, Zingraff J, Strihou C. Does dialysis-related amyloidosis regress after transplantation? Nephrol Dial Transplant. 1997;12:655–657. doi: 10.1093/ndt/12.4.655. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto Y, Hirawa N, Yamaguchi S, Ogawa N, Takeda H, Shibuya K, Kawahara K, Kojima H, Dobashi Y, Fujita M, Azusima K, Miyazaki N, Kobayashi M, Kobayashi C, Fujiwara A, Yuto J, Saka S, Yatsu K, Toya Y, Yasuda G, Ohnishi T, Umemura S. Long-term efficacy and safety of the small-sized beta2-microglobulin adsorption column for dialysis-related amyloidosis. Ther Apher Dial. 2011;15:466–474. doi: 10.1111/j.1744-9987.2011.00937.x. [DOI] [PubMed] [Google Scholar]
- 14.Davidson GS, Montanera WJ, Fleming JF, Gentili F. Amyloid destructive spondyloarthropathy causing cord compression: related to chronic renal failure and dialysis. Neurosurgery. 1993;33:519–522. doi: 10.1227/00006123-199309000-00026. [DOI] [PubMed] [Google Scholar]
- 15.Hsu CW, Wu MS, Leu ML. Dialysis-related cervical amyloidoma presenting with quadriplegia. Ren Fail. 2001;23:135–138. doi: 10.1081/JDI-100001293. [DOI] [PubMed] [Google Scholar]
- 16.Abumi K, Ito M, Kaneda K. Surgical treatment of cervical destructive spondyloarthropathy (DSA) Spine (Phila Pa 1976) 2000;25:2899–2905. doi: 10.1097/00007632-200011150-00011. [DOI] [PubMed] [Google Scholar]