Abstract
Gout is a common metabolic disease characterized by the development of arthritis and nephropathy related to the deposition of monosodium urate crystals within the joints, periarticular tissues, skin and kidneys. Tophus formation seen around the spinal column is very rare, while occurrences of spinal gout tophus without systemic gout disease are much more unique. In our study, we report a spinal gout case that presented with right sciatica without previous history of systemic gout disease.
Keywords: Gout tophus, Radiculopathy, Spinal column, Management
Introduction
Gout is a common metabolic disease characterized by the development of arthritis and nephropathy related to deposits of monosodium urate (MSU) crystals within the joints, periarticular tissues, skin and kidneys [4, 9, 13]. Nodules formed by the accumulation of MSU crystals in the soft tissue are called tophi. Histopathological confirmation of the tophus provides the definitive diagnosis of gout [9, 13, 14]. Tophi are most commonly seen in locations where blood circulation and temperature are low, such as the helix of the ear and the first metatarsophalangeal joint [2, 9, 13]. The occurrence of gout tophus in the spine has been reported in a limited number of cases [13, 14].
In this study, we report a rare case that presented with pain in the lower back and right leg with no previous history of gout. Lumbar magnetic resonance imaging (MRI) showed a spinal mass lesion that had been excised successfully. Histopathological examination revealed the surprising diagnosis of gout tophus.
Case report
A 77-year-old female patient was admitted to our clinic with the chief complaint of severe low back pain radiating to her right leg for 5 months. Pain had increased gradually and became very severe over the last month in spite of the multiple medical therapies given. She had no systemic diseases other than hypertension. Her gait was antalgic with restricted and painful low back movements. Neurological examination revealed a positive Laseque’s test and hypoesthesia on the right L5 dermatome. Lumbar MRI showed a mass lesion approximately 3 × 2 cm extending from the superior-anterior of the L5 vertebral body to the pedicle that markedly constricted the right neural foramen and compressed the right L5 neural radix. Marked degenerative hypertrophy was also noted in the facet articulations (Fig. 1a, b). MRI images gave rise to the suspicion of malignancy. Bone erosion that markedly constricted the spinal canal in the level of the right L5 neural foramen with a soft tissue component was observed on the lumbar computed tomography (CT) images (Fig. 2). No primary or metastatic tumors were found in the whole body examinations. Bone scintigraphy showed sclerotic areas and increased activity in the vertebras. Since the patient had very severe sciatica, surgical excision of the mass lesion compressing the right L5 root was planned for both diagnostic and treatment purposes. Mass lesion involving the facet articulations and the pedicle was excised. Widespread calcification and numerous crystal structures, rhomboidal and needle shaped, giving negative birefringence under polarized light within the calcification areas were observed on the histopathological examination, and the mass lesion was defined as gout tophus (Fig. 3a, b, c). The leg pain improved postoperatively (Fig. 4a, b). In the biochemical tests, it was seen that the uric acid level was high (7.2 mg/dl), a hypouricemic diet was recommended, and cholchicine treatment (0.5 mg/dl, twice a day) was initiated.
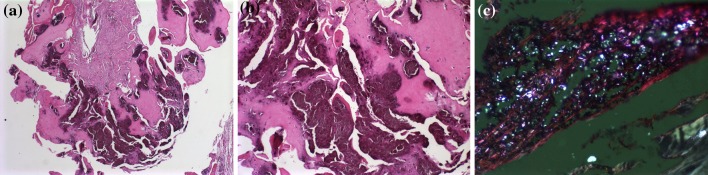
Fig. 1.
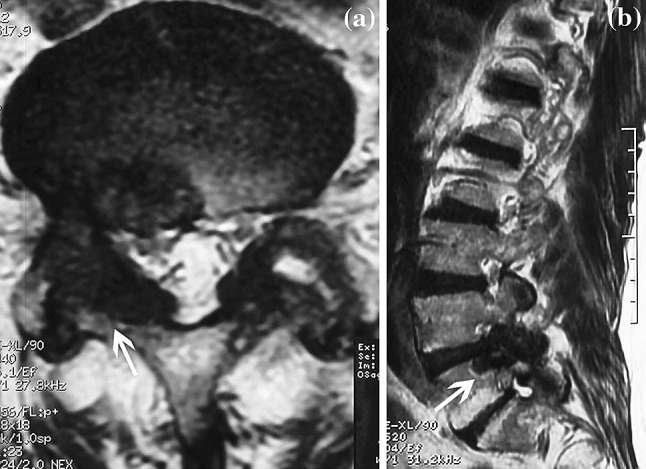
a, b T2-weighted axial and sagittal images show extradural lesions with severe dural sac and right root compression by the gout tophaceous deposits
Fig. 2.
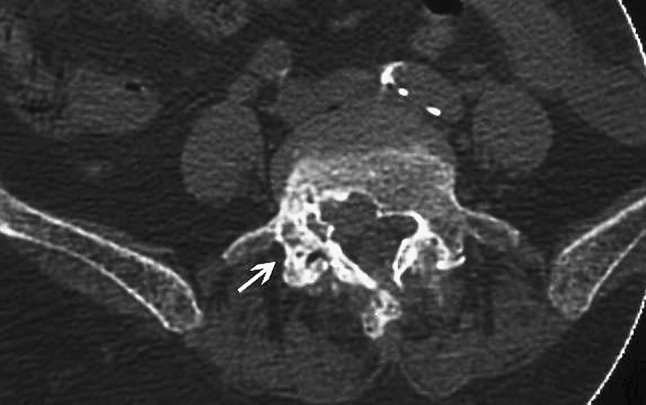
Axial CT shows bone erosions with calcifications over the right L4–5 facet joint and surrounding soft tissue masses
Fig. 3.
a Histologic preparation of the tissue, which shows a deposit of calcium pyrophosphate dihydrate on the soft tissue (H&E ×40). b There was a cartilaginous matrix associated with the lesion (H&E ×200). c Photomicrograph of a deposit of calcium pyrophosphate dihydrate during disease. The rhomboid-shaped crystals were examined using polarized light with red plate. The crystals are bluish white (weak positive birefringence) (×400)
Fig. 4.
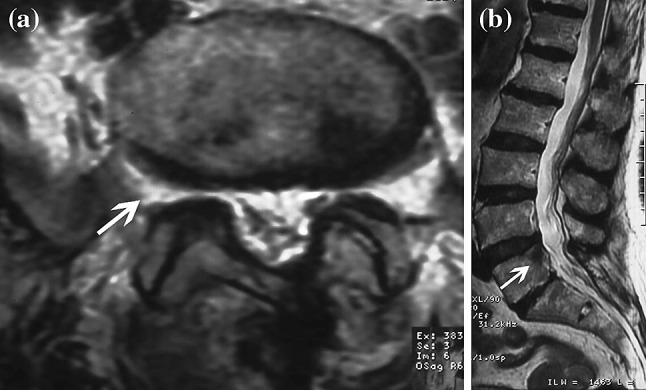
a, b Postoperative MR images
Discussion
High levels of uric acid can cause accumulation of MSU crystals in the periarticular tissues, synovial membrane, subchondral bone and the articular cartilage in the long term. This formation of soft tissue masses is called tophus [4, 9, 10]. While tophus of the spinal column is rare, the occurrence of spinal gout tophus without systemic gout disease, as in our case, is even rarer [8, 14].
Although etiopathogenesis of the crystal accumulation in the axial skeleton is not known completely, it has been reported that factors like degenerative disease of the spine, necrosis of the tissues or previous injuries can trigger the process [1, 4, 8]. The reason for the peripheral joints being involved more commonly in gout is considered to be related to the decrease of the solubility of the crystals in places with lower temperature and formation of tophi in the avascular tissues [8–10]. In addition, lower blood pH causes a decrease in the binding plasma proteins and trauma causes an increase in the precipitation of urate crystals, both of which cause the tophus formation to increase [5, 8, 10, 13]. There were degenerative changes in our case, consistent with her age, and it was thought that this could contribute to the formation of spinal tophus. Crystal deposition is generally seen in the vertebral bodies in the spine, pedicles, lamina, ligamentum flavum, interapophyseal cartilage, intervertebral disc and epidural space [1, 10, 15]. In our case also, there were vertebral body, pedicle and neural foramen involvements. Kelly et al. [7] have reported that all the sections of the spine are equally involved in gout patients. While the most frequent involvement in the cases reported in the literature is the lumbar region, especially L4–5 region, furthermore thoracic and cervical region involvements are also seen [1, 4, 10]. Lumbar region involvement was present in our case. A relation was found in the most recent studies between the tophus and the erosion in the facet articulation [9, 11, 13]. Chang suggested that tophaceous accumulation started from the facet articulations and then spread to the ligamentum flavum [8]. This assumption is consistent with the lower pH values, which can accelerate the depositing of crystals, seen in facet articulations [2, 10, 13, 15]. The period for the formation of tophi following the first episode of the acute gout arthritis is on average 10 years. Tophi are seen in approximately 50% of 10-year cases [1, 3, 9, 10]. Our case is interesting because of her presentation with spinal involvement without peripheral gout arthritis.
It was seen from the literature review that the majority of the gout patients with spinal involvement were in their fifth to seventh decades, and there was male predominance [5, 8, 10]. Spinal gout can cause axial pain as well as various neurologic findings such as radiculopathy, neurogenic claudication, cauda equine syndrome and myelopathy [1, 4, 6, 9]. In addition, patients can be asymptomatic in the early stages and where the hyperuricemia is under control and can only be diagnosed on autopsy [1, 8, 15]. The presence of the erosive lesion in the mechanical sense can cause spinal pain [6, 7, 10]. Patients with gout tophi in the lumbar region generally present with acute or subacute forms of radiculopathy or claudication [1, 7, 8]. With these characteristics, it can be confused with lumbar discopathy, spinal stenosis or degenerative spondylosis [9, 11, 13]. In addition, the hypermetabolic activity in the spine can resemble infections or neoplastic etiologies [7, 10, 15]. In our case also, the gout tophus in the lumbar region had created lower back pain. Spinal gout has varying radiographic characteristics including degenerative spondylosis, discovertebral erosions, bone destruction causing joint subluxation, spinal deformity, spontaneous fusion and pathologic fractures [4, 10, 11, 13]. Plain X-rays of the spine have rather low sensitivity to the diagnosis of spinal gout [9, 11, 15]. Spinal gout can be confused with degenerative spondylosis, pyogenic spondylosis and tuberculous spondylitis. Disc spaces are generally preserved in tuberculous spondylitis [11, 13, 15]. The diagnosis of spinal gout disease is rather difficult [7, 9, 10]. As much as 30% of the patients with acute gout attacks have serum uric acid levels within normal limits [11–13]. In the literature review, serum uric acid levels of gout patients with spinal involvement are generally high. Spinal gout can have a clinical presentation including lower back pain, fever and high levels of CRP with or without neurologic deficits, and can mimic spinal infections or calcium pyrophosphate dihydrate accumulation disease [4, 5, 7, 13]. Furthermore, gout tophus in the spine can be confused with primary bone tumors, metastases, infective granulomas or extramedullary hematopoiesis, both with clinical findings and radiographic appearance. The basic radiological difference between spinal gout and these diseases is the clear-cut erosive changes [5, 6, 12]. MRI and computerized tomography (CT) are the most specific imaging methods in the differential diagnosis of spinal gout. Classical CT findings of gout are as follows: lobular juxta-articular mass with decreased density as compared to the surrounding muscular tissue, intraarticular and juxta-articular bony erosions with sclerotic borders and normal bone density [12, 13, 15]. MRI with gadolinium is important in the diagnostic approach because while uric acid crystals give medium-hypointense images in T1-weighted sections, they vary in the T2-weighted sections, being mostly hypointense. Homogeneous contrast retention is observed in both sections [6, 12, 15]. Our case also had similar imaging characteristics.
Histopathologic examination of the tophus is required for the definitive diagnosis of spinal gout. Tophus is observed under polarized light microscope as fibrous tissue with gray extracellular material surrounded by histiocytes and leukocytes with polymorphic nuclei. Crystals have needle shapes displaying negative double refraction under polarized light microscope [5, 7, 9, 10]. A diagnosis of our patient without systemic involvement was made also with the histopathologic examination of the tophus that was removed with surgery. Early diagnosis is rather important for spinal gout, since medical treatment started in a timely manner can prevent the need for spinal surgery [2, 4, 7]. Nonsteroid anti-inflammatory agents, intravenous colchicine, systemic or intraarticular corticosteroid treatment and adrenocorticotropic hormones are the first-step drugs to be used in acute attacks [3, 5, 9]. Allopurinol must be used to solve the tophaceous deposit in the periods following the acute attack [2, 3, 13]. Furthermore, uricosuric drugs like probenecid and sulfinpyrazone can be used to decrease the blood uric acid level [2, 3, 9]. In patients with neurologic deficits, beginning pharmacologic treatment is generally required following surgical decompression [3, 4, 11].
In conclusion, spinal gout tophus can be confused with different diagnoses, because it forms an epidural mass lesion with lower back symptoms. It is possible to reach an accurate diagnosis with an anamnesis taken carefully, imaging methods and a histopathologic examination of the biopsy specimen. Improvement in symptoms is generally obtained with surgical decompression and proper medical treatment. Spinal gout tophus must be kept in mind for patients presenting with radicular lower back pain, as with the case presented here, even when there is no systemic gout disease.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Beier CP, Hartmann A, Woertgen C, Brawanski A, Rothoerl RD. A large, erosive intraspinal and paravertebral gout tophus. Case report. J Neurosurg Spine. 2005;3:485–487. doi: 10.3171/spi.2005.3.6.0485. [DOI] [PubMed] [Google Scholar]
- 2.Chang IC. Surgical versus pharmacologic treatment of intraspinal gout. Clin Orthop Relat Res. 2005;433:106–110. doi: 10.1097/01.blo.0000151456.52270.39. [DOI] [PubMed] [Google Scholar]
- 3.Dhote R, Roux FX, Bachmeyer C, Tudoret L, Daumas-Duport C, Christoforov B. Extradural spinal tophaceous gout: evolution with medical treatment. Clin Exp Rheumatol. 1997;15:421–423. [PubMed] [Google Scholar]
- 4.Draganescu M, Leventhal LJ. Spinal gout: case report and review of the literature. J Clin Rheumatol. 2004;10:74–79. doi: 10.1097/01.rhu.0000120898.82192.f4. [DOI] [PubMed] [Google Scholar]
- 5.Fontenot A, Harris P, Macasa A, Menon Y, Quinet R. An initial presentation of polyarticular gout with spinal involvement. J Clin Rheumatol. 2008;14:188–189. doi: 10.1097/RHU.0b013e318177a6b2. [DOI] [PubMed] [Google Scholar]
- 6.Hsu CY, Shih TT, Huang KM, Chen PQ, Sheu JJ, Li YW. Tophaceous gout of the spine: MR imaging features. Clin Radiol. 2002;57:919–925. doi: 10.1053/crad.2001.1001. [DOI] [PubMed] [Google Scholar]
- 7.Kelly J, Lim C, Kamel M, Keohane C, O’Sullivan M. Topacheous gout as a rare cause of spinal stenosis in the lumbar region. Case report. J Neurosurg Spine. 2005;2:215–217. doi: 10.3171/spi.2005.2.2.0215. [DOI] [PubMed] [Google Scholar]
- 8.King JC, Nicholas C. Gouty arthropathy of the lumbar spine: a case report and review of the literature. Spine. 1997;22:2309–2312. doi: 10.1097/00007632-199710010-00023. [DOI] [PubMed] [Google Scholar]
- 9.Lam HY, Cheung KY, Law SW, Fung KY. Crystal arthropathy of the lumbar spine: a report of 4 cases. J Orthop Surg (Hong Kong) 2007;15:94–101. doi: 10.1177/230949900701500122. [DOI] [PubMed] [Google Scholar]
- 10.Mahmud T, Basu D, Dyson PH. Crystal arthropathy of the lumbar spine. J Bone Joint Surg Br. 2005;87:513–517. doi: 10.1302/0301-620X.87B4.15555. [DOI] [PubMed] [Google Scholar]
- 11.Nakajima A, Kato Y, Yamanaka H, Ito T, Kamatani N. Spinal tophaceous gout mimicking a spinal tumor. J Rheumatol. 2004;31:1459–1460. [PubMed] [Google Scholar]
- 12.Popovich T, Carpenter JS, Rai AT, Carson LV, Williams HJ, Marano GD. Spinal cord compression by tophaceous gout with fluorodeoxyglucose-positron-emission tomographic/MR fusion imaging. Am J Neuroradiol. 2006;27:1201–1203. [PMC free article] [PubMed] [Google Scholar]
- 13.Suk KS, Kim KT, Lee SH, Park SW, Park YK. Tophaceous gout of the lumbar spine mimicking pyogenic discitis. Spine J. 2007;7:94–99. doi: 10.1016/j.spinee.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Varga J, Giampaolo C, Goldenberg DL. Tophaceous gout of the spine in a patient with no peripheral tophi: case report and review of the literature. Arthritis Rheum. 1985;28:1312–1315. doi: 10.1002/art.1780281118. [DOI] [PubMed] [Google Scholar]
- 15.Yen PS, Lin JF, Chen SY, Lin SZ. Tophaceous gout of the lumbar spine mimicking infectious spondylodiscitis and epidural abscess: MR imaging findings. J Clin Neurosci. 2005;12:44–46. doi: 10.1016/j.jocn.2004.03.020. [DOI] [PubMed] [Google Scholar]