Abstract
Background
Before the US Patient Protection and Affordable Care Act of 2010, there were documented insurance-based disparities in access to orthopaedic surgeons and care of orthopaedic conditions. While Massachusetts passed healthcare reform in 2007 with many similar provisions, it is unknown whether the disparities were present during the period of the law’s enactment.
Questions/purposes
We asked whether differences in rates of surgery between patients with novel government-subsidized healthcare plans and other forms of insurance, and between uninsured and insured patients, were similar after institution of the Massachusetts reform laws.
Methods
We identified 7577 patients diagnosed with upper extremity injuries between January 1, 2007 and October 1, 2010. From an institutional administrative database, we extracted demographics, insurance status, and plan of care. Insurance categories included government-subsidized healthcare plan (Commonwealth Care), private insurance, workers compensation, military-related (TriCare), Medicare, Medicaid (MassHealth), non-Commonwealth Care, and other insured and uninsured. After adjusting for age, gender, and diagnosis, we compared the proportions of patients who underwent elective surgery.
Results
Of 7577 patients, 1685 (22%) underwent elective upper extremity surgery. The adjusted rates of surgery were similar across most insurance categories, with higher rates in the workers compensation and TriCare categories compared with Commonwealth Care. Uninsured patients were as likely to undergo surgery as insured patients.
Conclusion
In a population with near-universal health insurance, a government-run health insurance exchange, and novel, government-subsidized, managed care plans, we found few insurance-based differences in rates of elective upper extremity orthopaedic surgery in a cohort of patients after healthcare reform.
Level of Evidence
Level IV, economic and decision analysis. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
With the recent passage of US Patient Protection and 13 Affordable Care Act of 2010 (PPACA) [24], policymakers and doctors are concerned whether and how the provisions in this act will affect the utilization and delivery of orthopaedic care. Speculations include, but are not limited to, an expansion of orthopaedic services, a reduction in the number of payer types, and further shifting of practices from private practice to hospital employee models [7]. Given the known insurance-based disparities in access, treatment, and outcomes in orthopaedics [2, 4, 11, 22, 26], portions of the new law are of particular interest, including the requirement to maintain minimal essential insurance coverage, the creation of government-run health insurance exchanges, and the creation of new partially subsidized healthcare plans [1, 21]. With millions of Americans likely to become insured, there likely will be increased demand for orthopaedic care, and it is unclear how this new demand, and incentives from novel healthcare plans, will affect practice.
One important potential effect of these laws is change in the rates of elective surgery. Before healthcare reform, rates of orthopaedic surgery reportedly varied according to health insurance status, with patients receiving workers compensation tending to have higher rates and patients who pay out-of-pocket (self-pay) tending to have lower rates [6, 10]. However, there have been no similar studies since the reform, and, as these insurance-based differences may represent disparities in care, it is important to identify whether they will persist after healthcare reform.
Enacted on January 1, 2007 in Massachusetts, “An Act Providing Access to Affordable, Quality, Accountable Health Care” led to several important changes, including a universal health insurance mandate, creation of the Commonwealth Connector (a government-sponsored health insurance exchange), and creation of Commonwealth Care (a state program offering partially subsidized managed care plans to residents who do not meet MassHealth [Medicaid in Massachusetts] eligibility requirements and earn less than 300% of the federal poverty guidelines) [3]. These laws reduced the state uninsured rate to 2.7% [20] and enrolled 160,000 state residents in Commonwealth Care programs [14]. A more recent federal law, the PPACA of 2010, contained several similar provisions, namely an individual requirement to maintain essential insurance coverage, a law enabling states to create health benefit exchanges, and a law enabling states “flexibility to establish basic health programs for low-income individuals not eligible for Medicaid” [24]. Given the similarities between the Massachusetts law and recent federal law, it is likely that certain practice trends in the period since the reform in Massachusetts foretell trends elsewhere in the nation.
We asked whether the differences in rates of surgery between Commonwealth Care and other forms of insurance, and between uninsured and insured patients were similar after institution of the Massachusetts reform.
Patients and Methods
Using our institution’s orthopaedic department’s billing database, we identified all current procedural terminology (CPT) codes related to upper extremity procedures, excluding fractures, neoplasia, and infection, between December 1, 2009 and October 1, 2010. We identified all International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) codes associated with CPT codes occurring a minimum of 100 times. We then identified all new patients presenting with these ICD-9 codes as their primary diagnosis between January 1, 2007 and October 1, 2010 (n = 7577). For each individual, we recorded their age, sex, dates of service, ICD-9 codes, CPT codes, and insurance status at time of presentation. Institutional review board approval was obtained before the investigation.
During the study period, 1685 patients underwent surgery for an overall adjusted rate of surgery (AROS) of 22%. The AROS varied (p < 0.01) by primary diagnosis (Table 1), with carpal tunnel syndrome having the highest AROS (50%; 95% CI, 44%–55%) and contracture of palmar fascia having the lowest AROS (8%; 95% CI, 5%–16%).
Table 1.
Rates of surgery by orthopaedic diagnosis
| ICD-9 | Description | Total patients | Surgical patients | Percent who had surgery |
|---|---|---|---|---|
| 726.1 | Rotator cuff syndrome | 1678 | 248 | 14.8% |
| 729.5 | Shoulder pain | 880 | 103 | 11.7% |
| 354.0 | Carpal tunnel syndrome | 645 | 307 | 47.6% |
| 715.94 | Osteoarthritis hand | 587 | 120 | 20.4% |
| 727.05 | Hand/wrist tenosynovitis | 475 | 102 | 21.5% |
| 238.1 | Soft tissue mass | 432 | 121 | 28.0% |
| 727.41 | Ganglion of the wrist | 363 | 134 | 36.9% |
| 719.54 | Joint stiffness, hand | 355 | 48 | 13.5% |
| 719.43 | Forearm pain | 297 | 54 | 18.2% |
| 727.03 | Trigger finger (acquired) | 230 | 60 | 26.1% |
ICD = International Classification of Diseases.
We grouped patients into several categories according to insurance status, with a planned subgroup analysis (Fig. 1). The initial insurance categories were Commonwealth Care and non-Commonwealth Care. Then, we subcategorized patients in the non-Commonwealth Care category as either other insured or uninsured to enable a three-arm subgroup analysis. Finally, the other insured category was further divided into five subcategories: private insurance, workers compensation, TriCare (insurance for members of the US Armed Forces and their families), Medicare, and MassHealth (Medicaid for Massachusetts residents), which allowed for a seven-arm subgroup analysis. The private insurance category included 37 different insurance providers.
Fig. 1.
The flow chart shows how the subgroups were organized for analysis.
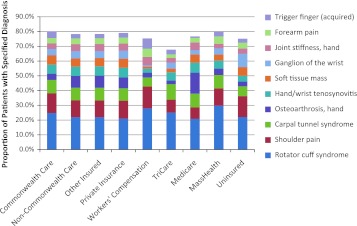
Of the patients in this cohort, 97% were insured (n = 7323) and 7% were enrolled in a Commonwealth Care plan (n = 500) (Table 2). By comparison, in 2009, 97% of the population in Massachusetts was insured [20], 2% was enrolled in a Commonwealth Care plan, 62% had employer-based or individual private insurance, 13% had Medicare, and 19% had MassHealth [15]. In 2010, the median age of the population in Massachusetts was 39.1 years and 51.6% of the population was female [27]. Logistic regression modeling was used to compare the likelihood of males undergoing surgery with the likelihood of females undergoing surgery while controlling for covariates, including diagnosis and insurance category. Females were 28% less likely (p < 0.001) than males to undergo surgery (odds ratio [OR], 1.28; 95% CI, 1.14–1.44). A chi-square analysis was used to compare the proportions of female patients in different insurance categories. There was no difference in the proportion of female patients in the Commonwealth Care category compared with the non-Commonwealth Care category (p = 0.09), or between Commonwealth Care, other insured, and uninsured (p = 0.12). In a seven-subgroup analysis, the proportion of female patients in each insurance category varied (Table 2, p < 0.001), with Medicare having the highest proportion of female patients (64%), and TriCare having the lowest (35%). Student’s t-test was used to compare the ages of the non-Commonwealth Care and Commonwealth Care cohorts. The non-Commonwealth Care cohort was older (p < 0.01) than the Commonwealth Care cohort. ANOVA was used to compare the ages of patients used in the three- and seven-arm subgroup analyses. The other insured cohort was older (p < 0.001) than the Commonwealth Care and uninsured cohorts. In the seven-category subgroup analysis, age differed (p < 0.001) across categories, with Medicare having the oldest population and TriCare having the youngest. The proportion of individual diagnoses in each insurance category varied across all insurance categories, with MassHealth having the highest proportion of patients with rotator cuff syndrome (30%), and TriCare having the highest proportion of patients with carpal tunnel syndrome (11%) (Fig. 2). Patient age did not predict the likelihood of undergoing surgery in any of the logistic regression models, and therefore is not considered to be associated with the rate of surgery.
Table 2.
Baseline demographic characteristics of study population by insurance type
| Patients | Commonwealth Care | Non-Commonwealth Care | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Other insured | Private insurance | Workers compensation | TriCare | Medicare | MassHealth | Uninsured | ||
| Total patients | 500 (7%) |
7077 (93%) |
6823 (90%) |
4671 (62%) |
215 (3%) |
124 (2%) |
1259 (17%) |
554 (7%) |
254 (3%) |
| Female patients | 313 (63%) |
4156 (59%) |
4014 (59%) |
2725 (58%) |
95 (44%) |
43 (35%) |
810 (64%) |
341 (62%) |
142 (56%) |
| Mean age (years) (± standard deviation) | 47.6 (± 11.7) |
52.3 (± 15.8) |
52.5 (± 15.8) |
49.2 (± 14.0) |
44.3 (± 11.3) |
37.1 (± 11.8) |
69.5 (± 12.4) |
49.9 (± 12.6) |
44.6 (± 12.9) |
Fig. 2.
The graph shows the proportions of patients with specified diagnosis by insurance type.
We defined the AROS as the number of patients who underwent surgery divided by the total number of patients in that cohort, after adjusting for sex, age, and diagnosis. We considered an effect size of 10% or greater difference in the AROS between the insurance groups to be clinically important. An a priori sample size calculation indicated a 10% difference in AROS between insurance categories with an α of 0.05 and a β of 0.20 (power = 0.80) could be achieved with 300 persons per insurance category. To adjust for age, sex, and diagnosis, we used a backward stepwise logistic regression model. In total, three schemes were modeled: a two-arm scheme (Commonwealth Care, non-Commonwealth Care), a three-arm scheme (Commonwealth Care, other insured, uninsured), and a seven-arm scheme (Commonwealth Care, private insurance, workers compensation, TriCare, Medicare, MassHealth, and uninsured). Then, we calculated ORs with 95% CI and estimated AROS using a two-tailed test.
The data required for analysis in this study regarding patient demographics, insurance status, diagnosis, and treatment, were available for all 7577 patients.
Results
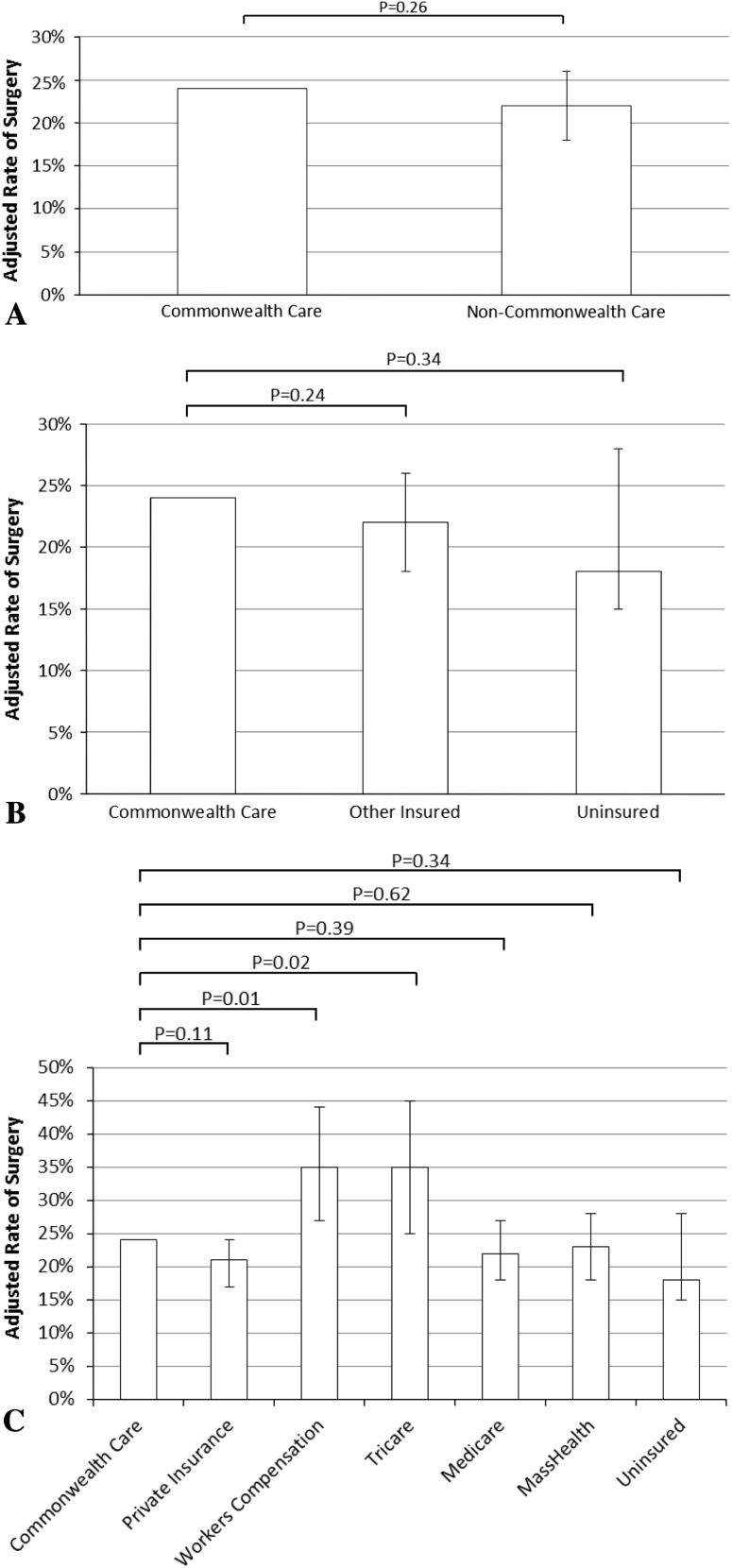
We found no differences between the AROS of the Commonwealth Care and non-Commonwealth Care categories (Fig. 3A). In the three-arm subgroup analysis, there were no differences between the AROS of the Commonwealth Care, other insured, and uninsured categories (Fig. 3B). In the seven-arm subgroup analysis, there were no differences between the AROS of the Commonwealth Care, private insurance, Medicare, MassHealth, and uninsured categories (Fig. 3C). The workers compensation and TriCare categories had higher AROS compared with the Commonwealth Care, with calculated differences in AROS of 11% (95% CI, 3%–20%) between Commonwealth Care and workers compensation, and 11% (95% CI, 1%–21%) between Commonwealth Care and TriCare categories (Fig. 3C)
Fig. 3A–C.
(A) No difference is seen between the adjusted rate of surgery (AROS) of the Commonwealth Care and non-Commonwealth Care groups. (B) There is no difference between the AROS of Commonwealth Care, Other Insured, and Uninsured group. (C) The AROS of the workers compensation and TriCare groups were higher than that of the Commonwealth Care group, but the AROS of the Private Insurance, Medicare, MassHealth, and Uninsured groups, were not different than that of the Commonwealth Care group.
Discussion
Enacted in 2010, the PPACA aimed to address several problems with the current healthcare system. Several of the law’s provisions, namely the minimum essential coverage mandate, the creation of state-run healthcare exchanges, and novel government-subsidized healthcare plans, were similar to those that have been in place in Massachusetts for several years [3, 24]. Given these similarities, it is plausible that practice patterns seen in Massachusetts since health reform was enacted may predict practice changes in other states. We sought to determine whether patients with Commonwealth Care, a novel government-subsidized healthcare plan, received surgery at rates similar to those for patients with other forms of insurance, and whether patients remaining uninsured despite the universal minimum essential coverage mandate received surgery at rates similar to those for patients with insurance.
This study had certain limitations. First, the study was performed at a single, academic, orthopaedic practice; however, the participating physicians were not salaried and not compensated using relative value units (RVU). Physician compensation was enumerated relative to collections. The results of this study may have limited applicability to nonacademic settings or in smaller communities, and multicenter analysis of this issue would be edifying. Despite this limitation, as a single-institution study, it avoided potentially confounding, site-specific variables, and selection of the entire cohort seen with the specified diagnoses rather than a subgroup served to minimize selection bias. Second, we had small samples of workers compensation, Tricare, and uninsured subgroups in the seven-arm analysis. The small sample size increased the probability of making a Type II error (failing to reject the null hypothesis that there were no differences in the rates of surgery between Commonwealth Care and the above-mentioned subgroups) above the commonly accepted standard of 0.20. Although performing subgroup analysis reduced statistical power, we believed such an analysis should not be avoided, as studies have shown insurance-based differences in operative rates were subtle and may have been masked by the method of insurance stratification [10]. Future studies of larger cohorts may address this issue. Third, administrative billing data were limited by their inability to control for confounders. The implication was that there may be an unknown element that was unaccounted for by our methods. However, our regression model adjusted for the potential confounders of sex and primary diagnosis.
There has been some research regarding the rates of orthopaedic surgery according to insurance status. Brinker et al. [6] evaluated rates of surgery from a single group of 40 orthopaedic surgeons in private practice working in private, nonprofit, and academic hospitals, in a large metropolitan area between 1999 and 2004. They found higher rates of surgery among patients with workers compensation compared with other payer types, but similar rates of surgery among the other payer types, including self-paying patients. Gundle et al. [10] evaluated surgical rates after meniscal tear at one orthopaedic practice from 2003 to 2006. They found higher rates of surgery among patients with workers compensation compared with private insurance, and lower rates of surgery among self-pay patients compared with those with private insurance. To our knowledge, there have been no studies of patients since healthcare reform has been initiated. We found that in a population seen at an academic orthopaedic practice between 2007 and 2010, the rates of elective upper extremity surgery were similar between Commonwealth Care and most other forms of insurance, with higher rates of elective surgery in workers compensation and TriCare categories compared with Commonwealth Care, and no difference between rates of surgery between the uninsured and most categories of insured patients.
Studies comparing the workers compensation population with other populations have identified several psychosocial factors that influence treatment and outcome [5, 23]. We did not account for these factors, and future studies may benefit from such consideration.
The absence of a difference in the rate of surgery between the uninsured and most categories of insured patients differed from the findings of Brinker et al. [6] and Gundle et al. [10]. Although it was unclear what exactly accounted for this difference, it was possible our uninsured cohort included patients who received services from a Massachusetts program called Free Care Services, or Health Safety Net. This benefit provided remuneration for facility fees, but distributed no monies toward professional services. In this way, this population remained unaffected by the healthcare mandate, but may have been able to have surgery at the same rate as insured patients. For these patients, physician participation and availability constituted their only barrier to surgical treatment. In other states, where support for institutional cost is not available, a higher disparity may exist. Additionally, we classified patients who elected to pay out of pocket for their care as uninsured. As a result, this subset may have contributed to the absence of a difference between groups.
Insurance status is a major factor influencing healthcare in the United States. In the Institute of Medicine report “Care without Coverage, Too Little, Too Late” [8], they found working-age, uninsured Americans received delayed or insufficient care, had more severe disease, and had higher mortality rates compared with insured patients [8]. Since this report, other studies in various specialties have emerged with similar findings [19, 25]. In orthopaedics, insurance status also was associated with differential access, treatment, and outcomes. In 2006, Skaggs et al. [26] reported in a nationwide study of 250 orthopaedic practices that pediatric patients with Medicaid had limited access to obtaining outpatient appointments in approximately 40% of practices, and were unable to obtain an outpatient appointment in approximately 20% of practices. Alosh et al. [2] found Medicare patients were more likely, and Medicaid patients less likely, to undergo cervical spine surgery than patients with private insurance. Hinman and Bozic [11] found patients with Medicaid had worse preoperative and postoperative outcomes after THA. We added to the existing literature by showing that cohorts after the healthcare reform had few insurance-based differences in rates of surgery at a metropolitan academic center.
The healthcare reform efforts in Massachusetts could be predictive of national healthcare reform; however caution must be taken in extrapolating trends in Massachusetts. There are income disparities between states [28], known geographic disparities in healthcare [9], and differences in uninsured rates between states [16]. These and other factors will play a large role in how healthcare reform, if mandated by national law in its current form, affects other states. If national healthcare reform is found unconstitutional in the Supreme Court, then there is much less predictive value.
As healthcare costs continue to increase, it is important to consider the financial impact of healthcare reform laws. As noted by Weissman and Bigby, “Before reform, the state provided about $1.4 billion annually in subsidies to institutions to cover services for the uninsured, about $33 million of which came out of the [state’s] general fund. After reform, with revenues redirected to support Commonwealth Care subsidies and expansions of MassHealth (the Massachusetts Medicaid program), a decrease in spending on the uncompensated care pool, and a phasing out of subsidies for managed-care organizations associated with safety-net institutions, the net new spending was $591 million, of which $172 million — less than 1% of the state budget — came from the [state’s] general fund [29]”. Although the state spending attributable to healthcare reform may represent a relatively small proportion of the state budget, like all other states Massachusetts struggles with persistently increasing healthcare costs.
There are currently various models for reimbursement reform under study, including pay for performance. A recent review focusing on different reimbursement models in orthopaedics found an overall low volume of primary literature on the subject, with pay for performance being the most widely investigated [18]. The study found that although pay for performance has received more attention in orthopaedics, it has yet to create “value-driven practices” in orthopaedics [18]. As can be imagined, the incentives in place will have a substantial effect on physician behavior and care delivery. This is a time of considerable change in healthcare delivery in Massachusetts. Many large hospital systems are moving to an Accountable Care Organization model. We have yet to reach an understanding of how this will affect orthopaedic healthcare delivery and reimbursement, and intend to study these issues moving forward.
In considering the Massachusetts experience with healthcare reform, it is difficult to anticipate how the timing of care should factor in the delivery of care because this issue is so closely related to reimbursement. In a system based on global payment with shared risk or pay for performance, delaying elective procedures has a financial benefit to all parties contracted under the established diagnosis. However, although horizontal care delivery systems may defray cost by amortizing the expense over a longer time, it is difficult to say how patient satisfaction might be affected. By delaying nonurgent interventions, the cost of care may be decreased, but the quality metrics may suffer if patients are dissatisfied by the process. As a result, despite decreasing cost, the value of care may decrease if steps are not introduced to maintain (or improve) patient outcomes.
We found that in a population with near-universal health insurance, a government-run health insurance exchange, and novel government-subsidized managed-care plans, there were few insurance-based differences in rates of elective upper extremity orthopaedic surgery at one academic institution. The trends seen in this investigation may herald changes in orthopaedic care delivery as healthcare reform legislation is enacted. Although our findings showed few insurance-based differences in rates of elective surgery, many questions regarding insurance-based disparities remain. As the national minimal essential coverage mandate takes effect, will the increased demand for orthopaedic care lead to longer wait times for elective surgery and overall lower rates of surgery? Evidence from countries with universal public healthcare suggests wait time for elective surgery is a problem, and has contributed to a subset of the population obtaining additional private insurance to obtain faster care [12, 13, 17, 30]. Future study of the wait times for elective surgery in cohorts after healthcare reform will be revealing. Also, if patients in need of orthopaedic care obtain health insurance that reimburses poorly, will these patients continue to have barriers to access? Answers to these and other questions will be available once the provisions in PPACA take effect.
Acknowledgments
We thank Kenny Gundle MD, for generous assistance with study design and manuscript preparation, Jordan Dimitrakov MD, PhD, for guidance with study design and statistical test planning, and Robert “RG” Davis MD, for help with manuscript revision.
Footnotes
Each author certifies that he, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA.
References
- 1.Albright HW, Moreno M, Feeley TW, Walters R, Samuels M, Periera A, Burke TW. The implications of the 2010 Patient Protection and Affordable Care act and the Health Care and Education Reconciliation Act on cancer care delivery. Cancer. 2010;117:1564–1574. doi: 10.1002/cncr.25725. [DOI] [PubMed] [Google Scholar]
- 2.Alosh H, Riley LH, 3rd, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality an examination of United States trends from 1992 to 2005. Spine (Phila PA). 2009;34:1956–1962. doi: 10.1097/BRS.0b013e3181ab930e. [DOI] [PubMed] [Google Scholar]
- 3.An Act Providing Access to Affordable, Quality, Accountable Health Care. HR 334, 187th Leg, (MA 2006).
- 4.Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007;89:2625–2631. doi: 10.2106/JBJS.F.01499. [DOI] [PubMed] [Google Scholar]
- 5.Atlas SJ, Tosteson TD, Hanscom B, Blood EA, Pransky GS, Abdu WA, Andersson GB, Weinstein JN. What is different about worker’s compensation patients? Socioeconomic predictors of baseline disability status among patients with lumbar radiculopathy. Spine (Phila PA). 2007;32:2019–2026. doi: 10.1097/BRS.0b013e318133d69b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brinker MK, O’Connor DP, Pierce P, Spears JW. Payer type has little effect on operative rate and surgeons’ work intensity. Clin Orthop Relat Res. 2006;451:257–262. doi: 10.1097/01.blo.0000229308.90265.96. [DOI] [PubMed] [Google Scholar]
- 7.Cherf J. The impact of healthcare reform on orthopaedic surgeons. AAOS Now. 2010;4. Available at: http://www.aaos.org/news/aaosnow/sep10/advocacy3.asp. Accessed June 1, 2011.
- 8.Committee on the Consequences of Uninsurance, Institute of Medicine, Board on Health Care Services. Care Without Coverage: Too Little, Too Late. Washington, DC: National Academy Press; 2002.
- 9.Fisher ES, Bell JE, Tomek IM, Esty AR, Goodman DG. A Dartmouth Atlas surgery report: Trends and regional variation in hip, knee, and shoulder replacement. Available at: http://www.dartmouthatlas.org/downloads/reports/Joint_Replacement_0410.pdf. Accessed January 25, 2012. [PubMed]
- 10.Gundle KR, McGlaston TJ, Ramappa AJ. Effect of insurance status on the rate of surgery following a meniscal tear. J Bone Joint Surg Am. 2010;92:2452–2456. doi: 10.2106/JBJS.I.01369. [DOI] [PubMed] [Google Scholar]
- 11.Hinman H, Bozic KJ. Impact of payer type on resource utilization, outcomes, and access to care in total hip arthroplasty. J Arthroplasty. 2008;23(6 suppl 1):9–14. doi: 10.1016/j.arth.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Jofre-Bonet M. Public health care and private insurance demand: the waiting time as a link. Health Care Manag Sci. 2000;3:51–71. doi: 10.1023/A:1019024903898. [DOI] [PubMed] [Google Scholar]
- 13.Johar M, Jones G, Keane M, Savage E, Stavrunova O. Waiting times for elective surgery and the decision to buy private health insurance. Health Econ. 2011;20(suppl 1):68–86. doi: 10.1002/hec.1707. [DOI] [PubMed] [Google Scholar]
- 14.Kaiser Commission on Medicaid and the Uninsured. Massachusetts health care reform: three years later. September 2009. Available at: http://www.kff.org/uninsured/upload/7777-02.pdf. Accessed: November 9, 2011.
- 15.Kaiser Family Foundation, statehealthfacts.org. Massachusetts: health insurance coverage of the total population, states (2008-2009), U.S. (2009). Available at: http://www.statehealthfacts.org/profileind.jsp?cmprgn=1&cat=3&rgn=23&ind=125&sub=39. Accessed November 7, 2011.
- 16.Kaiser Family Foundation, statehealthfacts.org. Health Insurance Coverage of the Total Population, states (2009-2010), U.S. (2010). Available at: http://www.statehealthfacts.org/comparetable.jsp?ind=125&cat=3. Accessed January 25, 2012.
- 17.King D, Mossialos E. The determinants of private medical insurance prevalence in England, 1997–2000. Health Serv Res. 2005;40:195–212. doi: 10.1111/j.1475-6773.2005.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lansky D, Nwachukwu BU, Bozic KJ. Using financial incentives to improve value in orthopaedics. Clin Orthop Relat Res. 2011 Oct 15. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 19.Lemaire A, Cook C, Tackett S, Mendes DM, Shortell CK. The impact of race and insurance type on the outcome of endovascular abdominal aortic aneurysm (AAA) repair. J Vasc Surg. 2008;47:1172–1180. doi: 10.1016/j.jvs.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 20.Long S, Phadera L, The Urban Institute. Estimates of health insurance coverage in Massachusetts from the 2009 Massachusetts Health Insurance Survey. Massachusetts Division of Health Care Finance and Policy. Available at: http://www.mass.gov/eohhs/docs/dhcfp/r/pubs/09/his-policy-brief-estimates-oct-2009.pdf. Accessed November 9, 2011.
- 21.Manchikanti L, Hirsch JA. Patient Protection and Affordable Care Act of 2010: a primer for neurointerventionalists. J Neurointerv Surg. 2012;4:141–146. doi: 10.1136/neurintsurg-2011-010036. [DOI] [PubMed] [Google Scholar]
- 22.Matlock D, Earnest M, Epstein A. Utilization of elective hip and knee arthroscopy by age and payer. Clin Orthop Relat Res. 2008;466:914–919. doi: 10.1007/s11999-008-0122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicholson GP. Arthroscopic acromioplasty: a comparison between workers’ compensation and non-workers’ compensation populations. J Bone Joint Surg Am. 2003;85:682–689. [PubMed] [Google Scholar]
- 24.The Patient Protection and Affordable Care Act, HR 3590, 111th Cong, (2010).
- 25.Rosen H, Saleh F, Lipsitz S, Rogers SO, Jr, Gawande AA. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144:1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 26.Skaggs DL, Lehmann CL, Rice C, Killelea BK, Bauer RM, Kay RM, Vitale MG. Access to orthopaedic care for children with medicaid versus private insurance: results of a national survey. J Pediatr Orthop. 2006;26:400–404. doi: 10.1097/01.bpo.0000217715.87857.24. [DOI] [PubMed] [Google Scholar]
- 27.US Census Bureau. American FactFinder. Profile of general population and housing characteristics: 2010, Massachusetts. Available at: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed November 7, 2011.
- 28.US Census Bureau. State median income. American Community Survey. State median family income by family size (3-year, LIHEAP). Available at: http://www.census.gov/hhes/www/income/data/statemedian. Accessed January 25, 2012.
- 29.Weissman JS, Bigby J. Massachusetts health care reform: near-universal coverage at what cost? N Engl J Med. 2009;361:2012–2015. doi: 10.1056/NEJMp0909295. [DOI] [PubMed] [Google Scholar]
- 30.Williams B, Whatmough P, McGill J, Rushton L. Impact of private funding on access to elective hospital treatment in the regions of England and Wales. National records survey. Eur J Public Health. 2001;11:402–406. doi: 10.1093/eurpub/11.4.402. [DOI] [PubMed] [Google Scholar]