Abstract
Study Objectives:
Although reports of sleep disturbances are common among individuals with posttraumatic stress disorder (PTSD), results of polysomnographic (PSG) studies have inconsistently documented abnormalities and have therefore suggested “sleep state misperception.” The authors' study objectives were to compare sleep parameters measured objectively and subjectively in the laboratory and at home in civilians with and without trauma exposure and PTSD.
Design:
Cross-sectional study.
Setting:
PSG recordings in a sleep laboratory and actigraphic recordings in participants' homes.
Participants:
One hundred three urban-residing African Americans with and without trauma exposure and PTSD who participated in a larger study.
Interventions:
N/A.
Measurements:
Sleep parameters (total sleep time [TST], sleep onset latency [SOL], and wake after sleep onset [WASO]) were assessed using laboratory PSG and home actigraphy. A sleep diary was completed in the morning after PSG and actigraphy recordings. Habitual TST, SOL, and WASO were assessed using a sleep questionnaire. The Clinician Administered PTSD Scale was administered to assess participants' trauma exposure and PTSD diagnostic status.
Results:
Participants, regardless of their trauma exposure/PTSD status, underestimated WASO in the diary and questionnaire relative to actigraphy and overestimated SOL in the diary relative to PSG. Among participants with current PTSD, TST diary estimates did not differ from the actigraphy measure in contrast with those without current PTSD who overestimated TST. No other significant group differences in discrepancies between subjective and objective sleep measures were found.
Conclusions:
Discrepancies between subjectively and objectively measured sleep parameters were not associated with trauma exposure or PTSD. This challenges prior assertions that individuals with PTSD overreport their sleep disturbances.
Citation:
Kobayashi I; Huntley E; Lavela J; Mellman TA. Subjectively and objectively measured sleep with and without posttraumatic stress disorder and trauma exposure. SLEEP 2012;35(7):957-965.
Keywords: Posttraumatic stress disorder (PTSD), trauma, polysomnography, actigraphy, sleep diary, sleep questionnaire, African Americans
INTRODUCTION
Sleep disturbance such as trouble falling and staying asleep (insomnia) and nightmares about a traumatic event are common symptoms of posttraumatic stress disorder (PTSD) and comprise 2 of its diagnostic criteria.1 Despite the frequent reports of sleep disturbances in PTSD, studies using objective sleep recordings have been inconsistent in documenting objective indices of impaired sleep initiation and maintenance. Some polysomnographic (PSG) studies found indications of sleep impairment (e.g., decreased sleep efficiency, increased wake time after sleep onset [WASO], and the number of awakenings) in individuals with PTSD whereas others failed to find substantial differences in these indices between individuals with and without PTSD.2 The latter set of observations led Lavie3 to conclude that “the subjective reports are out of proportion to the frequency and severity of objective sleep-laboratory findings” in a review article published in the New England Journal of Medicine.
Overestimations of sleep disturbances (e.g., underestimation of total sleep time [TST] and overestimation of sleep onset latency [SOL]) compared with laboratory or home PSG have been reported with insomnia.4–7 However, studies have indicated that there is variability in the accuracy of sleep state perception among people with insomnia.4,6 For example, Means and colleagues6 found that 37% of their participants with insomnia exhibited “slight to moderate underestimates” of their TST relative to both laboratory and home PSG, whereas another 37% “accurately predicted” TST in both settings.
Only a few studies of PTSD have directly examined relative associations and absolute differences between subjectively (i.e., diary and questionnaire) and objectively (i.e., laboratory-based PSG and actigraphy) measured sleep parameters. A summary of research methods and main findings of these studies are presented in Table 1. In the 2 laboratory PSG studies, patients with PTSD overestimated sleep disturbance in a morning sleep diary and a retrospective sleep questionnaire,8,9 whereas in an actigraphic study conducted in participants' homes, women with PTSD underestimated WASO and SOL in a morning sleep diary.10 The environmental setting may have influenced sleep state perception. However, it is not entirely clear whether differences among studies were due to sleep environments or other methodologic differences such as PSG versus actigraphy and different PTSD populations (male versus female, civilian versus veteran). Healthy control participants in the actigraphic study10 also underestimated sleep disturbances to a similar degree as women with PTSD, and the laboratory PSG study8 has found overestimation of SOL in control participants. These findings challenge the assertion that PTSD patient's reports of sleep disturbances are characteristically “out of proportion.”3
Table 1.
Summary of studies examining objectively and subjectively measured sleep in PTSD
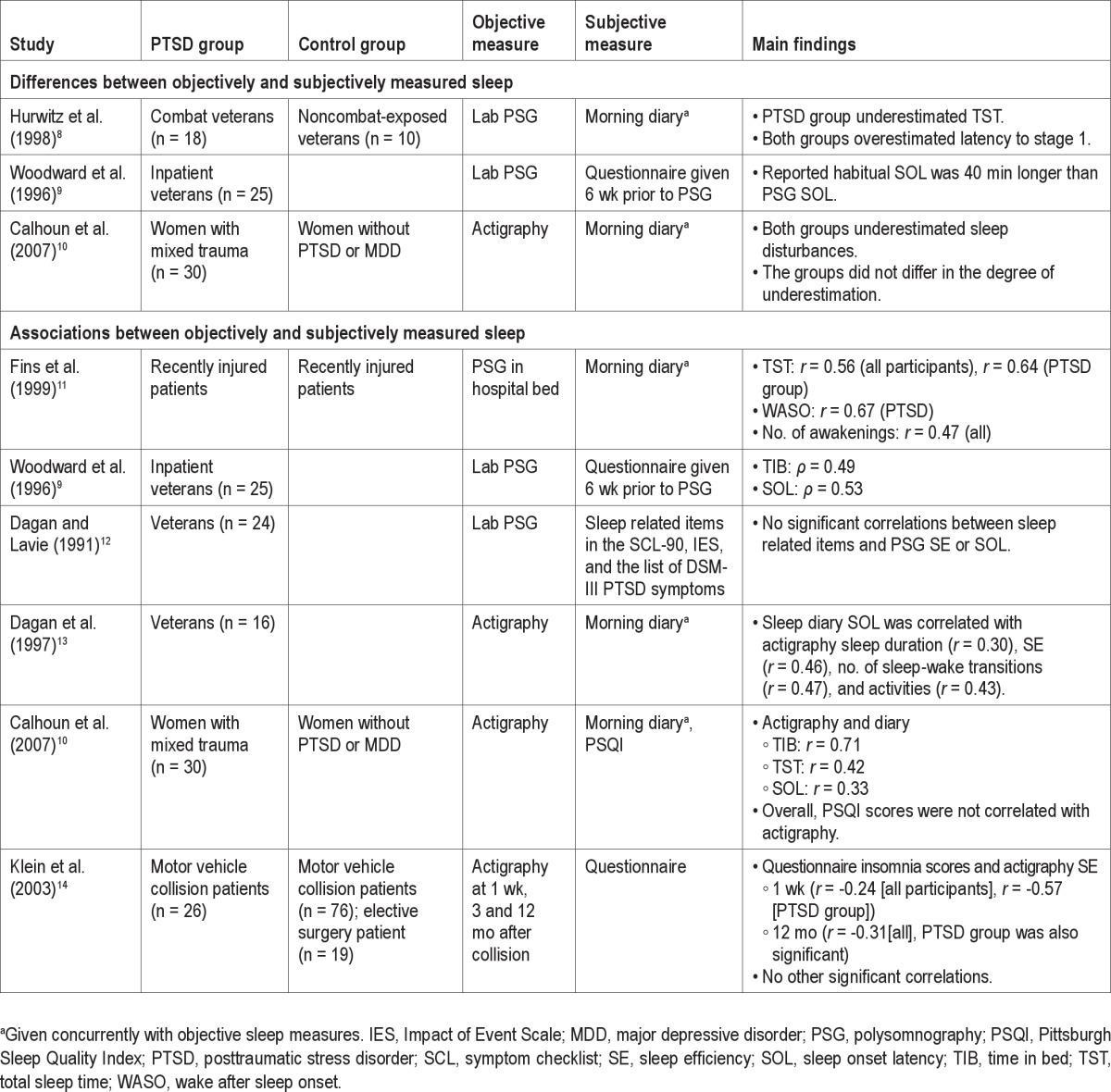
In the aforementioned studies, sleep parameters measured by actigraphy and PSG were correlated with sleep parameters measured by sleep diaries,10,11 but overall, not with measures from the more retrospective sleep questionnaires.10,14 Although correlations do not indicate accuracy of estimation, these findings suggest that morning sleep diaries may better estimate actual sleep than sleep questionnaires.
To better understand relationships between subjectively and objectively measured sleep in PTSD, we analyzed data from our study that recorded subjective and objective sleep of African Americans with and without trauma exposure and PTSD in both participants' homes with actigraphy and in a sleep laboratory with PSG. This group is of interest as some studies suggest that African Americans and other minorities in the United States have higher lifetime prevalence rates of PTSD15,16 than Whites, and African Americans have also been found to have greater sleep impairments compared with other racial groups.17,18 Given prior findings, we hypothesized that participants would overestimate sleep disturbances relative to PSG and underestimate sleep disturbances relative to actigraphy regardless of their trauma exposure/PTSD status.
METHODS
Participants
Participants were 103 African Americans (age 18–35 yr) who completed laboratory PSG and/or actigraphy recording as part of a larger study examining associations between trauma, PTSD, nocturnal blood pressure, and sleep. Participants were recruited from the Washington, DC metropolitan area through flyers and word of mouth. During the initial screening, potential participants were excluded if they were found to have a body mass index ≥ 40, chronic medical conditions (such as severe asthma, cancer, diabetes mellitus, and emphysema) or severe mental disorders (psychotic disorders, bipolar disorder, severe recurrent depression) that required consistent use of medications and/or can affect blood pressure, excessive use of caffeine (> 5 cups of coffee per day or its equivalent), heavy smoking (> 20 cigarettes per day) and drinking (> 14 drinks/wk in men, > 7 drinks/wk in women), use of antihypertensive medication, and regular night shift work or unusual sleep-wake schedules. Additional exclusion criteria were sleep breathing and movement disorders (screened through the first night PSG), current alcohol or drug abuse or dependence (screened through a structured clinical interview), and positive urine toxicology for illicit drugs. Participants' characteristics are presented in Table 2.
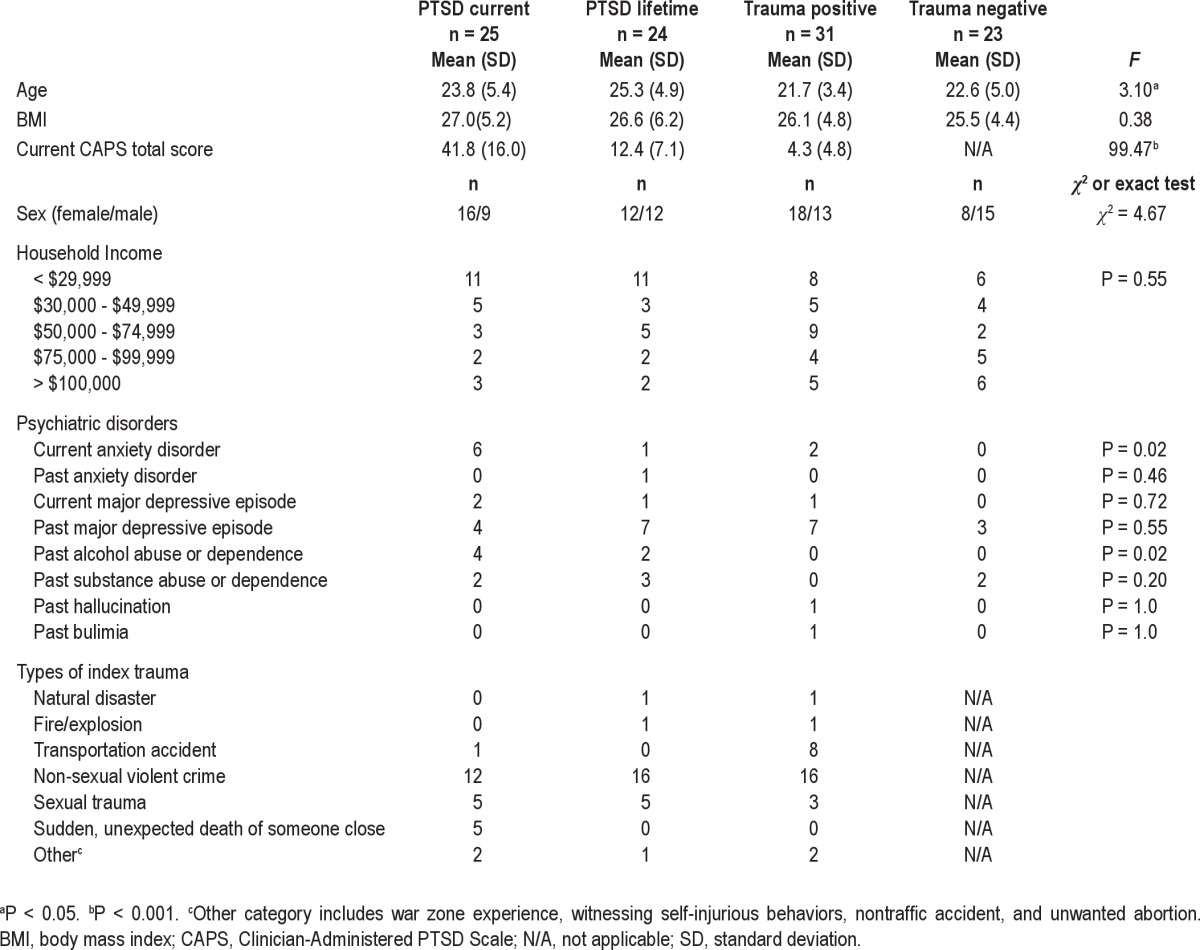
Table 2.
Participants' characteristics
Measures
Objective sleep measures
Participants underwent 2 consecutive overnight polysomnographic (PSG) recordings in the Howard University Clinical Research Unit (CRU). Recordings were conducted using an Embla (Denver, CO) titanium portable unit. PSG collection included a standard electroencephalogram montage with bilateral frontal, central, and occipital leads, 2 electrooculograms, and chin electromyograms and limb electromyograms and respiratory monitors on the first night only. Study staff, who were blinded to participants' PTSD diagnostic status, visually scored sleep records on a computer monitor applying standard criteria.19 All scorers had demonstrated > 90% concordance for scoring epochs with reference records. Participants were instructed to go to bed and arise close to their habitual bedtime and rise time. First-night recordings were used to exclude significant sleep breathing and movement disorders. Participants with an apnea-hypopnea index or periodic limb movement during sleep index greater than 10 were excluded. We analyzed data from the second-night recordings.
Participants completed 2 consecutive days of actigraphic monitoring while engaging in regular activities and sleeping at home. Participants wore an Ambulatory Monitoring Micro Mini-Motionlogger Actigraph (Ardsley, NY) on the wrist of their nondominant hand. Data recorded in the actigraphy unit were downloaded to a computer, and sleep-wake analysis applying the Sadeh algorithm was conducted using Ambulatory Monitoring Action W-2 software. Actigraphy has been validated against PSG with agreement rates for sleep-wake identification of higher than 90%20,21; however, low sensitivity for detecting wake during sleep has been reported.22 Because participants wore ambulatory blood pressure and Holter monitoring devices during the first day, data from the second day were used in the analysis.
During PSG and actigraphy monitoring, participants recorded bedtimes and rise times in a morning sleep diary, and these records were used for determining time in bed.
Subjective sleep measures
Participants completed a sleep questionnaire designed to measure sleep patterns and disturbances during the past month. Information gathered through the questionnaire included habitual bedtime and rising times and SOL on weekdays and weekends, and the number of awakenings per night and average length of each awakening. The questionnaire items were modeled after typical sleep diary questions23,24 to assess sleep for typical nights during the past month. WASO (the number of awakening multiplied by the average length of awakening) and weekday and weekend TSTs (SOL and WASO subtracted from time in bed) were estimated based on the information reported in the questionnaire. Weekday estimates of SOL and TST were used as PSG and actigraphy recordings were done on weekdays.
Participants completed sleep diaries in the morning after PSG and actigraphic recordings. Information reported in the sleep diaries included bedtime, rising time, SOL, the number of awakenings, and length of each awakening. TST and WASO were estimated based on participants' reports on their diaries.
Clinical interviews
The Clinician Administered PTSD Scale (CAPS)25 is a structured clinical interview designed to produce dichotomous lifetime and current PTSD diagnostic status and continuous symptom severity. In the current study, the most distressing potentially traumatic event (the index event) reported by a participant was assessed at the beginning of the interview to determine whether it met the diagnostic criteria for a traumatic event (Criterion A).1 If the index event met the criteria, the frequency and intensity of each of 17 PTSD symptoms associated with the index event were rated on 5-point scales ranging from 0 (Never [frequency], Not at all [intensity]) to 4 (Daily or almost daily, Extremely). A symptom was considered present when the participant reported at least the frequency rating of 1 and the intensity rating of 2 for the symptom.25
Current and lifetime diagnoses of mood disorders, psychotic disorders, anxiety disorders other than PTSD, substance abuse and dependence, and eating disorders were assessed using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID).26 All CAPS and SCID interviews were conducted by trained staff members (psychology graduate students, medical students, and clinical psychology postdoctoral fellows), and a licensed psychiatrist reviewed all cases. Practice interviews were completed prior to data collection until the trainee and the trainer reached the 90% agreement rate on practice cases.
Other self-report measures
The PTSD Checklist-Civilian Version (PCL) in conjunction with the Life Event Checklist (LEC)25 were administered during the initial meeting to obtain preliminary information regarding participants' trauma exposure and current PTSD symptoms. The LEC includes a list of 16 types of potentially traumatic experiences (e.g., transportation accident, assault with a weapon, sexual assault). Participants were asked to indicate whether they had experienced or witnessed any of these events as an adult or a child and which of those experiences distressed them the most. The PCL is a self-report measure designed to assess manifestations of PTSD symptoms in the past 1-mo period. The PCL consists of 17 items corresponding to the 17 Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) symptoms of PTSD. Participants were instructed to rate each of the symptoms associated with the experience identified by the LEC on a 5-point scale ranging from 1 (Not at all) to 5 (Extremely).
Procedures
The following procedures were approved by the institutional review board at Howard University. Potential participants were given a brief description of the study and screened for eligibility through a brief interview over the phone or in person. Eligible individuals were invited to the initial study session at Howard University with a researcher who further described the study and obtained a written informed consent. During the session, participants completed a self-report survey packet, which included a demographic questionnaire, a sleep questionnaire, the LEC, and PCL.
One hundred eighty-four participants (54%) who completed the self-report survey were invited to the laboratory phase of the study. The subset of participants was selected based on their responses to the LEC and PCL to have adequate representation of individuals in 4 trauma exposure/PTSD categories: PTSD current, PTSD lifetime, trauma positive, and trauma negative (see subsequent paragraphs for the definitions of these categories). One hundred fifty-one of the invited participants (82%) completed the clinical interview. Based on results of the CAPS, participants were categorized into 1 of the 4 groups. The trauma-negative group includes participants who did not report any life events meeting the DSM-IV criteria for a traumatic event. The PTSD-current group included 15 participants who met the full current PTSD diagnostic criteria and 10 who met subthreshold criteria (meeting the criteria for at least 2 of the 3 symptom clusters). Studies have shown that participants with subthreshold PTSD were not significantly different from those who met the full PTSD criteria in terms of social and occupational functioning, treatment-seeking behaviors, and the number of suicide attempts.27,28
Participants who met the full criteria for PTSD in the past but did not currently meet full or subthreshold criteria were categorized into the PTSD-lifetime group. The trauma-positive group included trauma-exposed participants who did not meet full lifetime PTSD or full or subthreshold current PTSD criteria.
After completing the clinical interview, physical examination, and urine screening, participants completed 2 consecutive overnight PSG recordings at the Clinical Research Unit. Approximately 1 wk after the PSG recordings, they completed 2 consecutive 24-hr recordings of actigraphy. One participant was excluded for an apnea-hypopnea index > 10. Participants received $25 for completing the self-report survey, another $25 for the clinical interview, $125 for each PSG recording, and another $125 for completing 1 day of ambulatory blood pressure and Holter monitoring and 2 days of actigraphy recording.
Data Analysis
SPSS (IBM, Armonk, NY) was used to conduct data analyses. An alpha level of 0.05 was used in all analyses. Differences in participants' characteristics between groups were examined using 1-way analyses of variance (ANOVAs) for continuous variables, chi-square tests for categorical variables, and Fisher exact tests for categorical variables with small sample sizes in some cells. Pearson product moment correlation coefficients were computed to examine the associations between objectively and subjectively measured sleep parameters. A series of 2 (sleep measures: subjective versus objective) × 4 (groups) mixed ANOVAs or analyses of covariance (ANCOVAs) with sleep measures as the repeated measure were conducted to examine differences between objectively and subjectively measured sleep parameters (i.e., a main effect of sleep measures) and whether objective-subjective measure discrepancies differed between groups (i.e., an interaction effect of sleep measures and groups). We found that age and past alcohol abuse or dependence were different between groups and were correlated with some of the sleep parameters; therefore, these variables were included as covariates in the analyses of those sleep parameters. We also computed Pearson product moment correlation coefficients to examine whether sex should be included as a covariate because prior studies showed that sex was associated with sleep measures.29,30 When a significant main effect of groups was found in an ANCOVA, post hoc pairwise comparisons of estimated marginal means were performed using least significant difference (LSD). When a significant interaction effect was found, simple effect tests comparing subjective and objective measures within each group were performed. Effect sizes (η2) were computed,31 with η2 = 0.010, 0.059, and 0.138 considered small, medium, and large, respectively.32
Post hoc power analyses using G*power 333 indicated that the analyses were underpowered to detect small sleep measures ×groups interaction effects (power ranging from 16 to 69%), but they were adequately powered to detect medium interaction effects (power ranging from 74 to 100%, only 3 analyses were less than 80%).
RESULTS
Participants' Characteristics
Participants' characteristics for each trauma exposure/PTSD group are presented in Table 2. A 1-way ANOVA and post hoc test using LSD indicated that the PTSD-lifetime group was significantly older than the trauma-positive (P = 0.004) and the trauma-negative (P = 0.05) groups. Fisher exact tests indicated disproportionate distribution of diagnoses of current anxiety disorder cases (P = 0.02) and past alcohol abuse or dependence (P = 0.02) among the groups (highest rates with current PTSD). In addition, age and past alcohol abuse or dependence were significantly correlated with some of the dependent variables in the main analyses. Specifically, age was correlated with WASO measured by PSG (r = 0.21, P = 0.04) and the sleep questionnaire (r = 0.27, P = 0.006), and TST measured by the sleep questionnaire (r = −0.26, P = 0.01) and the sleep diary concurrent with PSG (r = −0.25, P = 0.02). Past alcohol abuse or dependence was correlated with WASO measured by the sleep questionnaire (r = 0.24, P = 0.02). Sex was correlated with TST and WASO measured by actigrapy (r = 0.26, P = 0.01 for both). Therefore, age, sex, and past alcohol abuse or dependence were included as covariates in the analyses of the correlated sleep parameters.
Correlations Between Objectively and Subjectively Measured Sleep Parameters
These correlations are presented in Table 3. The sleep questionnaire was not significantly correlated with the objective measures for any sleep parameters. In the PTSD-current group, the sleep diary was significantly correlated with PSG and actigraphy for all sleep parameters except SOL measured by actigraphy. Overall, correlations between actigraphy and the diary were low for SOL. TST measured by the diary was significantly correlated with both PSG and actigraphy in all of the groups except PTSD lifetime. For WASO, correlations between the diary and PSG were significant or marginally significant in all of the groups except trauma positive.
Table 3.
Correlation coefficients between subjectively and objectively measured sleep parameters

Objective Measures and Morning Sleep Diaries
Table 4 presents means and standard deviations of TST, SOL, and WASO measured by PSG, actigraphy, and morning diaries for each group, as well as results of 2 (sleep measures: sleep diary versus objective measure) × 4 (groups) mixed ANOVAs or ANCOVAs. An ANOVA comparing WASO measured by actigraphy and the diary revealed a significant main effect of measures, indicating underestimation of WASO relative to actigraphy. However, there were no significant interactions, which indicate that the extent of underestimation of WASO did not differ between groups. For SOL, we also found a significant main effect of measures, but not an interaction. Participants overestimated SOL relative to PSG. A significant interaction effect was found in the ANCOVA comparing TST measured by actigraphy and the diary. Post hoc simple effect tests comparing actigraphy and diary TST within each group indicated that participants in the PTSD-lifetime, trauma-positive, and trauma-negative groups overestimated TST, whereas in PTSD-current participants, TST measured by actigraphy and the diary were not significantly different (Figure 1).
Table 4.
Means, standard deviations, and results of ANOVA/ANCOVA comparing PSG and actigraphy to sleep diaries
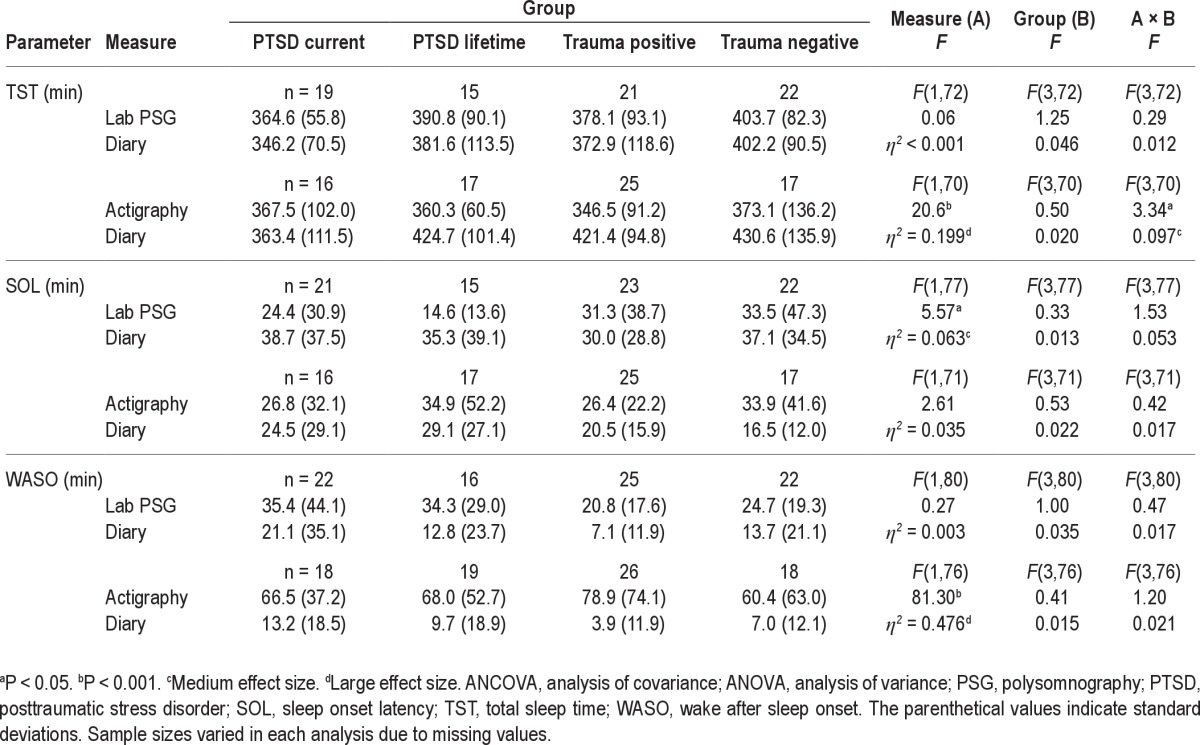
Figure 1.
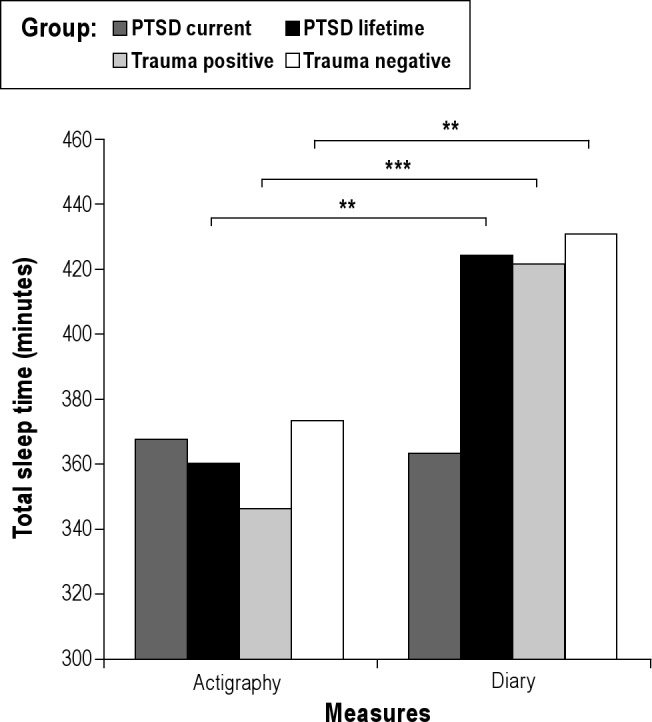
Interaction effect between measure and group on total sleep time. **P < 0.01, ***P < 0.001.
We performed the same ANOVAs and ANCOVAs, excluding participants meeting only the current subthreshold PTSD criteria from the PTSD-current group. This did not result in any changes in which effects were significant.
Objective Measures and the Sleep Questionnaire
Means and standard deviations of TST, SOL, and WASO measured by PSG, actigraphy, and the sleep questionnaire for each group, as well as results of 2 (sleep measures: sleep questionnaire versus objective measure) × 4 (groups) mixed ANOVAs and ANCOVAs are presented in Table 5. An ANCOVA comparing WASO measured by actigraphy and the questionnaire showed a significant main effect of measure, indicating that participants underestimated WASO relative to actigraphy. An ANCOVA comparing PSG and the sleep questionnaire showed a significant main effect of groups on TST. Post hoc analyses using LSD revealed that the PTSD-current group had shorter TST compared with the PTSD-lifetime (P = 0.006) and that the trauma-positive group had shorter TST compared with the PTSD-lifetime (P = 0.005) and the trauma-negative (P = 0.04) groups. Although the interaction was not significant in the ANOVA comparing SOL measured by PSG and the questionnaire, the effect size was medium (η2 = 0.070). Examination of the mean SOL within each group indicated that the discrepancies between PSG and the questionnaire were greatest in the trauma-negative group (14.7 min underestimation) and smallest in the PTSD-current group (7.1 min overestimation).
Table 5.
Means, standard deviations, and results of ANOVA/ANCOVA comparing PSG and actigraphy to a sleep questionnaire
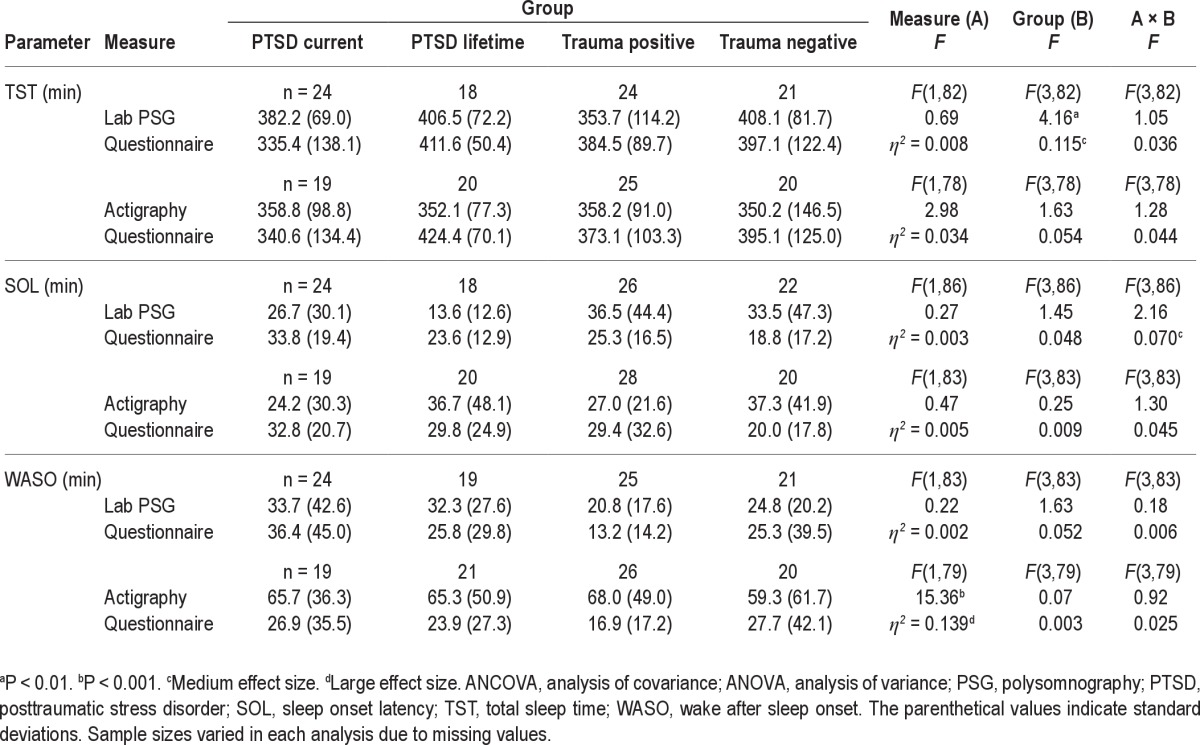
We repeated the same ANOVAs and ANCOVAs, excluding participants meeting only the current subthreshold PTSD criteria from the PTSD-current group. An ANCOVA comparing WASO measured by PSG and the questionnaire revealed a significant main effect of group, F(3,73) = 4.64, P = 0.005. Post hoc analyses using LSD indicated that the PTSD-current group had more WASO in comparison with the other 3 groups (PTSD lifetime, P = 0.008; trauma positive, P < 0.001; trauma negative, P = 0.009). There were no other significant changes from the original analyses.
DISCUSSION
This study compared sleep parameters measured by objective (i.e., PSG and actigraphy) and subjective (i.e., diary and questionnaire) assessments in urban-residing African Americans with and without trauma exposure and PTSD. The current study expands on prior studies by using both laboratory PSG and home actigraphy and including participants in 4 different trauma exposure/PTSD categories.
We hypothesized that participants would underestimate sleep disturbance relative to actigraphy regardless of their trauma exposure/PTSD status. Consistent with this hypothesis, we found that participants underestimated WASO in both the diary and questionnaire relative to actigraphy, which likely reflects limited awareness and memory of awakenings during sleep. Considering the lack of discrepancies for WASO between PSG and the subjective measures, other explanations could include effects of actigraphy limitations for detecting wake22 and/or home sleep environments. It is therefore possible that the current study underestimated the difference between reported and actual WASO. Results regarding SOL and TST did not support the hypothesis. Participants' estimates of SOL did not significantly differ from actigraphy measure, and for TST, discrepancies between actigraphy and the diary were different between groups (i.e., an interaction between measures and groups). Specifically, TST measured by the diary did not significantly diverge from the actigraphy measure (4-min difference) in the PTSD- current group, but participants in the other groups, in contrast, overestimated TST (on average, 64, 75, and 58 min of overestimation in PTSD-lifetime, trauma-positive, and trauma-negative groups, respectively). Individuals with PTSD did not misperceive their sleep state, but rather they appeared to have a more accurate perception, which is contrary to the prior statement in the literature that “patients are generally unaware of the true nature of their sleep disturbances.”3 We speculated that nighttime hypervigilance at home in participants with current PTSD might have heightened their awareness of their own sleep state. Considering that such differences between individuals with and without current PTSD were not found in laboratory TST, it is possible that people with current PTSD are more vigilant in monitoring their sleep at home than in the laboratory, where they might feel safer monitored by staff.9 However, it is not clear whether the laboratory versus home differences were due to setting or the use of PSG versus actigraphy.
We also hypothesized that participants would overestimate sleep disturbance relative to PSG regardless of groups. Overall, results were not consistent with this hypothesis except for SOL measured by the diary. Participants, regardless of their PTSD/trauma exposure status, overestimated SOL in the diary. For SOL measured by the questionnaire, the trauma-negative and -positive groups underestimated SOL whereas PTSD-current and -lifetime groups overestimated SOL. Although the effect size of this measure by group interaction was medium, the objective-subjective discrepancy of the PTSD-current group (7.1 min) was the smallest among the groups. When TST measured by PSG and the questionnaire were compared, participants in the PTSD-current group considerably underestimated TST (46.8 min) compared with the other groups, although this interaction was not statistically significant. As participants estimated their habitual TST at home in the questionnaire, it may be another indication of PTSD participant's hypervigilance at home that could be attenuated in a sleep laboratory setting.9
Results did not substantially change when we excluded participants who only met the subthreshold PTSD criteria, which suggest that individuals meeting the full and subthreshold PTSD diagnostic criteria may not be different in terms of abilities to estimate their own sleep states. However, the results should not be considered conclusive as these exploratory analyses were conducted with small numbers of participants in the PTSD-current subgroups.
Overall, ANOVA/ANCOVAs indicated that discrepancies between the sleep questionnaire and objective measures were no less than for the sleep diary. Analyses, however, revealed that objective sleep measures were not correlated with the sleep questionnaire, which is consistent with the prior findings.10,14 As correlation coefficients reflect the degree of covariation of 2 variables, the lack of correlation does not necessarily indicate substantial differences between the questionnaire and the objective measures. Nevertheless, results of sleep questionnaires should be interpreted with caution, especially when used in correlational analyses. On the other hand, sleep diary measures were correlated with the objective measures, especially with the PSG in both the PTSD-current and the trauma-negative groups. Given the results of both ANOVA/ANCOVAs and correlations, sleep diaries appear to be appropriate tools for estimating TST in both individuals with and without PTSD.
Although the study expanded on prior studies, it has limitations. Because the parent study was not designed to investigate the specific focus of this report, PSG and actigraphy were not conducted in both laboratory and home, which did not allow us to determine whether the differences between PSG and actigraphy results were due to differences in objective measures or sleep environments. PSG and actigraphy data used in the analyses were collected only over 1 night. Therefore, chance occurrences of the night might have affected the results. Our analyses were also not adequately powered to detect small size interaction effects. Although this study included both male and female participants having been exposed to a wide variety of traumatic events, it included only a nonclinical sample of civilian, urban-residing African Americans. In addition, PTSD symptom severity of most PTSD-current participants was in a mild-moderate range.34 These participant characteristics may limit the generalizability of the findings. Treatment-seeking patients with more severe PTSD may be more inclined to overreport their sleep disturbances.
Despite these limitations, the information obtained in this study adds to the existing literature on objectively and subjectively measured sleep in PTSD. Overall, our findings did not reveal overestimation of sleep disturbances by individuals with PTSD, which is consistent with prior findings and challenges the assertion that individuals with PTSD overreport their sleep disturbances. In fact, our data indicate that PTSD is associated with more accurate estimations of total sleep duration in a home environment. Future studies should explore effects of different sleep settings (e.g., home and laboratory) using both PSG and actigraphy.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Work for this study was performed at Department of Psychiatry, Howard University, Washington, DC. This study was supported by NIMH grant 5K24MH001917-1, NHLBI grant 5R01HL087995-03, and NCRR grant 1UL1RR031975-01 to Dr. Mellman.
Footnotes
A commentary on this article appears in this issue on page 897.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. fourth edition - text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiology. 2007;44:660–9. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- 3.Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001;345:1825–32. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- 4.Carskadon M, Dement W, Mitler M, Guilleminault C, Zarcone V, Spiegel R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. Am J Psychiatry. 1976;133:1382–8. doi: 10.1176/ajp.133.12.1382. [DOI] [PubMed] [Google Scholar]
- 5.Frankel BL, Coursey RD, Buchbinder R, Snyder F. Recorded and reported sleep in chronic primary insomnia. Arch Gen Psychiatry. 1976;33:615–23. doi: 10.1001/archpsyc.1976.01770050067011. [DOI] [PubMed] [Google Scholar]
- 6.Means MK, Edinger JD, Glenn DM, Fins AI. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 2003;4:285–96. doi: 10.1016/s1389-9457(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 7.Coates TJ, Killen JD, George J, Marchini E, Silverman S, Thoresen C. Estimating sleep parameters: A multitrait-multimethod analysis. J Consult Clin Psychol. 1982;50:345–52. [PubMed] [Google Scholar]
- 8.Hurwitz TD, Mahowald MW, Kuskowski M, Engdahl BE. Polysomnographic sleep is not clinically impaired in Vietnam combat veterans with chronic posttraumatic stress disorder. Biol Psychiatry. 1998;44:1066–73. doi: 10.1016/s0006-3223(98)00089-4. [DOI] [PubMed] [Google Scholar]
- 9.Woodward SH, Bliwise DL, Friedman MJ, Gusman DF. Subjective versus objective sleep in Vietnam combat veterans hospitalized for PTSD. J Trauma Stress. 1996;9:137–43. doi: 10.1007/BF02116839. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun PS, Wiley M, Dennis MF, Means MK, Edinger JD, Beckham JC. Objective evidence of sleep disturbance in women with posttraumatic stress disorder. J Trauma Stress. 2007;20:1009–18. doi: 10.1002/jts.20255. [DOI] [PubMed] [Google Scholar]
- 11.Fins AL, Mellman TA, Bustamante VA, Torres J, David D, Nolan B. The relationship between subjective and objective sleep in recently traumatized patients. Sleep. 1999;22:S248–9. [Google Scholar]
- 12.Dagan Y, Lavie P. Sleep disorders in war-related PTSD patients: how reliable are the subjective assessments? Sleep Res. 1991;20:177. [Google Scholar]
- 13.Dagan Y, Zinger Y, Lavie P. Actigraphic sleep monitoring in posttraumatic stress disorder (PTSD) patients. J Psychosom Res. 1997;42:577–81. doi: 10.1016/s0022-3999(97)00013-5. [DOI] [PubMed] [Google Scholar]
- 14.Klein E, Koren D, Arnon I, Lavie P. Sleep complaints are not corroborated by objective sleep measures in post-traumatic stress disorder: a 1-year prospective study in survivors of motor vehicle crashes. J Sleep Res. 2003;12:35–41. doi: 10.1046/j.1365-2869.2003.00334.x. [DOI] [PubMed] [Google Scholar]
- 15.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 16.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE Project. Psychosom Med. 2008;70:410–6. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iber C, Ancoli-Israel S, Chesson A, Quan ST, et al. The AASM manual for the scoring of sleep and associated events. Rules, terminology and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 20.Ancoli-Israel S. Actigraphy. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia, PA: Saunders; 2000. pp. 1295–301. [Google Scholar]
- 21.Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18:288–302. doi: 10.1093/sleep/18.4.288. [DOI] [PubMed] [Google Scholar]
- 22.Paquet J, Kawinska A, Carrier J. Wake detection capacity of actigraphy during sleep. Sleep. 2007;30:1362–9. doi: 10.1093/sleep/30.10.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morin CM. Insomnia: psychological assessment and management. New York: Guilford Press; 1993. [Google Scholar]
- 24.Monk TH, Reynolds CF, III, Kupfer DJ, et al. The Pittsburgh sleep diary. J Sleep Res. 1994;3:111–20. [PubMed] [Google Scholar]
- 25.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 26.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York: Biometrics Research; 2002. [Google Scholar]
- 27.Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154:1114–9. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- 28.Zlotnick C, Franklin CL, Zimmerman M. Does “subthreshold” posttraumatic stress disorder have any clinical relevance? Compr Psychiatry. 2002;43:413–9. doi: 10.1053/comp.2002.35900. [DOI] [PubMed] [Google Scholar]
- 29.Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- 30.Roehrs T, Kapke A, Roth T, Breslau N. Sex differences in the polysomnographic sleep of young adults: a community-based study. Sleep Med. 2006;7:49–53. doi: 10.1016/j.sleep.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Levine TR, Hullett CR. Eta squared, partial eta squared, and misreporting of effect size in communication research. Hum Commun Res. 2002;28:612–25. [Google Scholar]
- 32.Cohen J. Statistical power analysis for the behavior sciences. Hillsdale, NJ: Laurence Erlbaum Associates; 1988. [Google Scholar]
- 33.Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behav Res Method Ins C. 1996;28:1–11. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 34.Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–56. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]


