Abstract
Objective
To assess the evidence for interventions designed to prevent or reduce overweight and obesity in children younger than 2 years.
Data Sources
MEDLINE, the Cochrane Central Register of Controlled Trials, CINAHL, Web of Science, and references from relevant articles.
Study Selection
Included were published studies that evaluated an intervention designed to prevent or reduce overweight or obesity in children younger than 2 years.
Data Extraction
Extracted from eligible studies were measured outcomes, including changes in child weight status, dietary intake, and physical activity and parental attitudes and knowledge about nutrition. Studies were assessed for scientific quality using standard criteria, with an assigned quality score ranging from 0.00 to 2.00 (0.00–0.99 is poor, 1.00–1.49 is fair, and 1.50–2.00 is good).
Data Synthesis
We retrieved 1557 citations; 38 articles were reviewed, and 12 articles representing 10 studies met study inclusion criteria. Eight studies used educational interventions to promote dietary behaviors, and 2 studies used a combination of nutrition education and physical activity. Study settings included home (n=2), clinic (n=3), classroom (n=4), or a combination (n=1). Intervention durations were generally less than 6months and had modest success in affecting measures, such as dietary intake and parental attitudes and knowledge about nutrition. No intervention improved child weight status. Studies were of poor or fair quality (median quality score, 0.86; range, 0.28–1.43).
Conclusions
Few published studies attempted to intervene among children younger than 2 years to prevent or reduce obesity. Limited evidence suggests that interventions may improve dietary intake and parental attitudes and knowledge about nutrition for children in this age group. For clinically important and sustainable effect, future research should focus on designing rigorous interventions that target young children and their families.
The Rate of Obesity Among children has reached epidemic proportions, with more than 25%of preschool children now classified as overweight orobese.1Children who are overweight during the preschool years are more than 5 times as likely to be overweight adolescents, 2 and a growing body of evidence indicates that weight status of young infants is associated with obesity or metabolic risk factors later in life.3–10 Recent studies revealed that weight gain in a child’s first year of life11 and even weight status at age 6 months12 have implications for future obesity status and the development of insulin resistance and other cardiovascular risk factors.
Results of observational studies suggest that exposure to an obesogenic environment often begins in the first 2 years of life. Exposure to high-calorie and low-nutrition foods and beverages,13–15 increased television time,16,17 and high prevalence of excess fruit juice intake18,19 can contribute to weight gain in young children. Other observational studies20–25 demonstrated a beneficial role of breastfeeding in preventing child obesity. These study findings suggest that early childhood, specifically the first 2 years of life, represents a critical window to establish behaviors that will affect later health.
Despite the increasing need for obesity prevention efforts beginning in early childhood, few studies have been performed with a goal of intervening among very young children. A previous review article26 looked broadly at interventions designed to prevent obesity, promote healthy eating and physical activity, and reduce sedentary behaviors in children from birth to age 5 years; however, most investigations targeted children older than 2 years. The review article concluded that parents are receptive to behavioral changes that could promote healthy weight among their young children, but the age range of children included in the review makes it difficult to draw conclusions about interventions designed specifically for infants and toddlers, an age range when eating habits and behaviors are established. Furthermore, the review article did not systematically quantify the quality of studies included. With recent data providing evidence for the importance of the first 2 years of life in the development of obesity,11,12,27 the objective of the systematic review herein is to provide an updated and rigorous review of interventions aimed at improving weight, nutrition, or physical activity among children from birth to age 2 years.
METHODS
We searched MEDLINE from January 1, 1966, to December 14, 2009, and searched Cochrane Central Register of Controlled Trials, Web of Science, and CINAHL through December 14, 2009, for the following keywords: obesity prevention and control, obesity, overweight, and infant and a combination of nutrition, nutrition assessment, nutrition therapy, diet, physical activity, and education. For MEDLINE, Medical Subject Headings were used where available. We restricted our search to studies that were published in the English language.
Citations describing studies that implemented interventions targeted at preventing or reducing overweight or obesity in children younger than 2 years were selected by one of us (P.J.C.) for a full review. Additional studies were identified by a review of the reference lists of included articles. Studies included for this review article met the following inclusion criteria: (1) published in the English language, (2) targeted a population of children between birth and age 2 years, and (3) used a behavioral, educational, or quality improvement–based intervention designed to prevent obesity or to promote healthy nutrition and physical activity. Studies were excluded if they did not report original data.
We assessed the quality of all articles included based on criteria by West et al.28 Every study was rated by 2 of us (P.J.C. and D.K.) in each of the following categories: (1) adequacy of the study population, (2) description of the study intervention, (3) comparability of study subjects, (4) maintenance of comparison groups, (5) measurement of outcomes, (6) appropriateness of the statistical analysis, and (7) control of confounding. Ratings were assigned numerical scores (2 is good; 1, fair; and 0, poor). A composite score was generated for each article by summing the category scores and dividing by the number of categories reviewed. These summary scores were then used to give an overall qualitative rating for the article. Articles with quality scores of 0.00 to 0.99 were considered of poor quality, 1.00 to 1.49 of fair quality, and 1.50 to 2.00 of good quality. There was 100% interrater reliability between the primary reviewers in overall quality score.
In addition, a search was conducted of ongoing studies that are testing interventions aimed at reducing or preventing overweight and obesity in children younger than 2 years. The www.clinicaltrials.gov Web site was searched for trials of overweight or obesity among subjects younger than 2 years, and studies that seemed to address our review subject were identified.
RESULTS
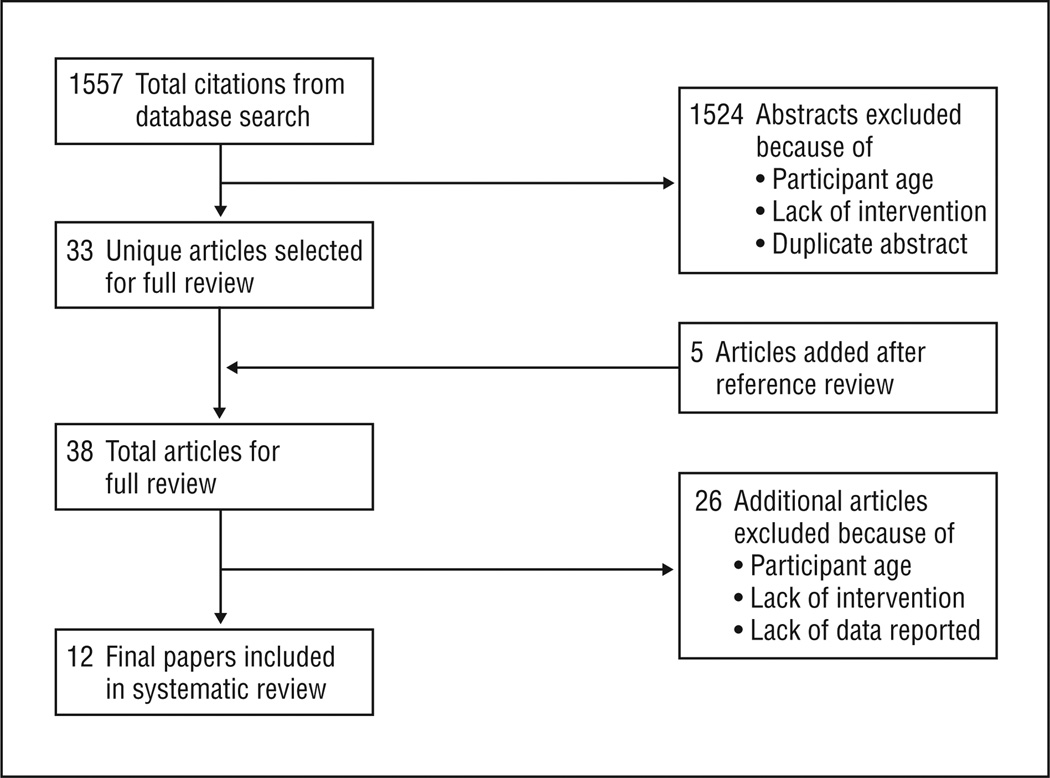
We retrieved 1557 citations from the initial database searches, 1524 of which did not fit the study inclusion criteria based on review of the abstract or were duplicates; 5 articles were added after review of the references of relevant literature. Thirty-eight potentially eligible articles were given a full review, and 26 of these did not fit the inclusion criteria. Twelve articles representing 10 unique studies were selected for final review based on the inclusion criteria (Figure). Three of the articles presented results from the long-term longitudinal Special Turku Coronary Risk Factor Intervention Project for Babies (STRIP) study.29–31 One article about the STRIP study31 involved children aged 4 to 10 years but was included because it reported outcomes from children who were part of the original cohort and were exposed to the intervention initially as infants. Table 1 and Table 2 summarize the included studies and the main findings.
Figure.
Summary of search strategy.
Table 1.
Trials With Nonrandomized Designs
| Source, y | Design | Study Population | Intervention | Outcome | Result | Study Limitation |
Quality Score |
|---|---|---|---|---|---|---|---|
| Wolman et al,32 2008 | Cohort | Children aged 18–30 mo, 9 subjects | Educational and activity-based program, 2-h weekly class session for 11 wk, 45-min physical activity and 45-min parental education per session | Qualitative evaluation of study components by participants after completion of 11-wk program | Parents liked parental and child exercise programs, interactive discussions, and opportunities to share ideas; parents disliked lack of variation in activity and focus on nutritional theory | Small sample size, no or inappropriate control group, high loss to follow-up, poor treatment of confounding, outcomes unvalidated or poorly defined | 0.28 (Poor) |
| Klohe-Lehman et al,33 2007 | Before and after | Overweight or obese mothers of children aged 1–3 y, 235 dyads | Educational and activity-based program, 8 weekly 2-h classes (30-min exercise) focused on nutritious food choices and healthy lifestyle modifications with aim of maternal weight loss | Maternal BMI, child weight and BMI for age, maternal activity by pedometer readings, child activity, maternal and child dietary intake (24-h food recall, 2-d diet record), assessed at 0, 8, 24 wk | Mean (SD) maternal weight loss of −2.7 (−2.8) kg between 0–24 wk, child caloric intake decreased between 0 and 8 wk, child BMI for age increased, activity increased for mothers and children between 0 and 8 wk | No or inappropriate control group, high loss to follow-up, poor treatment of confounding | 0.86 (Poor) |
| Horodynski and Stommel,34 2006 | Quasi-experimental | Children aged 11–25 mo, 62 intervention and 73 control | Educational program (NEAT), 4 group 90-min weekly class sessions and 18 individual home-based reinforcement activities focused on positive eating behaviors for toddlers, parenting skills | Parental knowledge of healthy eating habits, assessed at 0, 1, 6 mo | Intervention group more knowledgeable vs control group (P < .01) at 1 and 6 mo, no difference in change in caregivers’ self-efficacy scores at 6 mo between groups | Small sample size, poor treatment of confounding, outcomes unvalidated or poorly defined | 0.86 (Poor) |
| Horodynski et al,35 2004 | Quasi-experimental | Children aged 12–36 mo, 19 intervention and 19 control | Educational program (NEAT), 3 group 90-min class sessions over 6 mo focused on food safety, recognition of satiety and feeding self-regulation, managing family meals | Parental knowledge, attitude, and mealtime practices; caregiver and toddler dietary intake (24-h dietary recall); assessed at 0 and 6 mo | No significant differences found between groups for any outcome at 6 mo | Small sample size, poor treatment of confounding, outcomes unvalidated or poorly defined | 0.86 (Poor) |
| Worobey et al,36 2004 | Before and after | Children aged <72 mo, 60 subjects | Educational program (PORSCHE), 8-mo duration, individualized home visits weekly, monthly, or bimonthly focused on improved nutrition, supplementing diet with vitamins, eating healthier snacks | Dietary intake (parental interview, 24-h dietary recall), cognitive and physical development, assessed at 0 and 8 mo | 17% Reduction in mean caloric intake (P< .05), no reduction in nutrients, no change in cognitive development | Small sample size, no or inappropriate control group, poor treatment of confounding, limited detail of study intervention reported | 0.64 (Poor) |
| Adam et al,37 1985 | Cohort | Mothers of newborns, 49 intervention and 54 control | Educational program, 20-min group meeting and handout at discharge from nursery, handout again at first well-child care visit, focused on delayed introduction of solid foods and juices until after age 4 mo | Feeding practice, perception of health (standardized interview), assessed monthly until age 4 mo | Reduction of nonrecommended foods introduced at age 1 mo (26%vs 6%, P< .01) with continued effect at age 4 mo (94% vs 64%, P< .02), increased maternal perception of child health in treatment group | Small sample size, high loss to follow-up, poor treatment of confounding | 0.71 (Poor) |
| Pisacano et al,38 1978 | Cohort | Newborns in authors’ practice, 80 intervention (1970) and 50 control (1964) | Educational program given in clinic (Prudent Diet) focused on infant cereals and fresh fruit given before age 3 mo, no excess sugar, excessive milk consumption discouraged, control group received conventional diet information | Prevalence of overweight in study populations (weight percentile >1 SD over height percentile), assessed at age 3 y for each group | Proportion overweight in intervention group was 1.28%, proportion overweight in control group was 25.5% | Small sample size, no or inappropriate control group, poor treatment of confounding, limited detail of study intervention reported, outcomes unvalidated or poorly defined | 0.57 (Poor) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); NEAT, Nutrition Education Aimed at Toddlers; PORSCHE, Prevention-Oriented System for Child Health.
Table 2.
Trials With Randomized Controlled Designs
| Source, y | Study Population | Intervention | Outcome | Result | Study Limitation |
Quality Score |
|---|---|---|---|---|---|---|
| Kavanagh et al,39 2008 | Infants aged 3–10 wk, exclusive formula users, 44 intervention and 57 control | Educational program consisting of one 45- to 60-min session led by WIC educator focused on recognizing signs of infant satiety and limiting formula volume, control arm was general infant feeding guidelines | Weight gain (g/wk), formula intake (48-h intake diary [mL/d]), caregiver feeding attitudes, assessed at 0 and 4 mo | No difference in weight gain or formula intake in intervention group vs control group, no change in parental behavior, increase in proportion of parents who were concerned about feeding infant too much in intervention group only | Small sample size, high loss to follow-up | 1.43 (Fair) |
| Talvia et al,31 2004 | Finnish children of original cohorts29,30 enrolled at ages 4–10 y | Same as Lagström et al29 | Primary was dietary composition (4-d food diary), assessed yearly | Small reduction in fat and cholesterol intake in intervention group, overall increase in carbohydrate intake in intervention group | High loss to follow-up, limited detail of study intervention reported | 1.43 (Fair) |
| Harvey-Berino and Rourke,40 2003 | Children aged 9–36 mo, mothers with BMI >25, 20 intervention and 20 control | Educational program, 11 home sessions over 16 wk, treatment arm was OPPS applied to healthy eating and exercise behaviors, control arm was parenting support education | Anthropomorphics (child WHZ score, maternal BMI), diet (3-d food diary), eating behavior (child feeding questionnaire), assessed at 0 and 16 wk | Maternal BMI decreased (not significant) in OPPS arm, no difference in proportion of children overweight, child energy intake decreased in OPPS arm (not significant), OPPS arm decreased restrictive eating habits | Small sample size | 1.43 (Fair) |
| Simell et al,30 2000 | Finnish children enrolled at age 7 mo, followed up for 3 y | Same as Lagström et al29 | Same as Lagström et al29 plus serum cholesterol and child anthropomorphic measures, assessed at 8, 13, 24, 36 mo | Intervention group consumed fewer calories at 8 and 13 mo and less saturated fat at all time points, lower serum cholesterol levels (boys only), no effect on anthropomorphics | Limited detail of study intervention reported | 1.43 (Fair) |
| Lagström et al,29 1997 | Finnish children enrolled at age 5 mo, followed up for 4 y, 540 intervention and 522 control | Educational program (STRIP for Babies) led by nutritionist and pediatrician at well-child care visits and focused on reduction of fat and cholesterol intake, control arm was standard dietary anticipatory guidance | Primary was dietary intake of fat and cholesterol, secondary was dietary nutrient intake (3- or 4-d food diaries), assessed at 8, 13, 24, 36, 48 mo | Small reduction in fat and cholesterol intake in intervention group, total calories consumed were the same for both groups, no difference in vitamin or mineral intake | High loss to follow-up, limited detail of study intervention reported | 1.43 (Fair) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); OPPS, Obesity Prevention plus Parenting Support; STRIP, Special Turku Coronary Risk Factor Intervention Project; WHZ, weight-for-height z score; WIC, women, infants, and children.
Of the articles included in this review, 3 studies29–31,39,40 (discussed in 5 articles) were randomized controlled trials, 2 were before-and-after studies,33,36 2 were quasiexperimental studies,34,35 and 3 were cohort studies. 32,37,38 Three studies37–39 looked specifically at interventions provided to mothers of newborns, 1 study34 looked at interventions for children aged 1 to 2 years, and 6 studies29–33,35,36,40 (discussed in 8 articles) included older children as a part of the sample. The numbers of participants in the included studies ranged from 9 to 1062.
Of 12 articles reviewed, we judged 5 to be of fair quality (score range, 1.00–1.49)29–31,39,40 and 7 to be of poor quality (score range, 0.00–0.99).32–38 As a group, quality was limited by small sample sizes,32,35,36,39,40 lack of or inappropriate control groups,32,33,36 high sample proportion lost to follow-up,29,31,33,37,39 inadequate treatment of confounding,32–38 low level of detail reported about study interventions,29–31,33–38 and outcome measures that were unvalidated or poorly defined.33–36 Studies were of poor or fair quality (median quality score, 0.86; range, 0.28–1.43).
INTERVENTION TYPES
Eight studies29–31,34–40 (discussed in 10 articles) used an intervention that focused on education, and 2 studies32,33 combined an educational intervention with a program of guided physical activity. Of the educational interventions, 6 programs sought to improve parental attitudes and knowledge about nutrition for infants,29–33,36,37 (discussed in 7 articles) and 4 programs supplemented this teaching with recommendations for specific behaviors that could improve eating habits, such as teaching how to look for signs of infant satiety.34,35,39,40 Although most educational programs were focused on healthy nutrition for children, 1 study33 targeted maternal nutritional and physical activity habits, with the hypothesis that improved behaviors would be adopted by their children. Of the interventions that included physical activity, 1 study33 used exercise sessions for the mother only, and 1 study32 combined a session for mothers and children.
Two studies36,40 used home visits to implement the study intervention, 3 studies29–31,37,38 (discussed in 5 articles) used interventions deployed during routine clinic visits or in the nursery, and 4 studies32,33,35,39 used interventions that were given in classrooms outside of the home or clinic. One study34 combined classroom sessions outside of the home or clinic with home visits. Interventions in 5 studies32–35,39 were led by a nutritionist, in 2 studies37,38 by physicians, in 1 study36 by a nurse, and in 1 study40 by a trained peer educator. The STRIP study29–31 used an intervention that was delivered by a multidisciplinary team composed of a nutritionist, nurse, and physician.
OUTCOMES ASSESSED
Five articles30,33,38–40 measured objective clinical outcomes such as maternal body mass index or change in child weight status as a primary outcome of the study. Ten articles29–31,33–37,39,40 examined behavioral habits such as parental report of child dietary intake or physical activity as outcomes. Three articles34,35,39 examined parental attitude or knowledge about nutrition as a primary outcome of the studies. One article32 used a qualitative description of parental response to the intervention as an outcome. One article36 examined cognitive development as a secondary outcome.
STUDY FINDINGS
Six studies29–31,33,34,36–38 were successful in affecting process measures of interest such as parental report of child dietary intake, parental knowledge of healthy nutritional behaviors, and parental attitudes. Overall, these improvements were modest. In the STRIP study,29–31 Finnish children were randomized at age 8 months to receive usual care or an intervention that included individualized nutritional counseling in the clinic at the time of well-child care visits by a nutritionist with a focus on reducing saturated fat and cholesterol consumption. The study demonstrated a small but statistically significant reduction in the intervention group vs the control group at each time point for daily fat intake (reduction of 3–5 g/d, P < .001), fat as a percentage of dietary intake (reduction of 1.7%–3.0%, P < .001), and cholesterol consumption (reduction of 20–29 mg/dL, P < .001) between age 8 months and 4 years (to convert cholesterol concentration to millimoles per liter, multiply by 0.0259). Total serum cholesterol (reduction of 11–16 mg/dL) and non–high-density lipoprotein cholesterol (reduction of 9–14 mg/dL) concentrations were lower for the intervention group compared with the control group for boys (P < .001 for both), but there was no difference between the intervention and control groups for girls. There was no statistically significant difference in overall energy intake or in the mean child weight between the groups. Differences in fat intake as a percentage of total caloric intake between the intervention and control groups persisted (reduction of 1.4%–2.6%, P < .001) over 10 years of follow-up in the entire STRIP study.
Similar to results of the STRIP study, outcome measures such as maternal body mass index, child weight-for-age percentile, or percentage of overweight children were generally unaffected by other interventions examined. One study38 evaluating an educational intervention emphasizing healthy infant nutrition delivered by a pediatrician as part of routine care showed a reduction in the prevalence of overweight children compared with a historical control group from the same clinic practice (reductions of 25.5% for the control group and 1.28% for the intervention group, P value unreported). The study had significant limitations that might bias the findings, including the use of a historical control group, the definition of overweight as a weight percentile 1 SD greater than the height (rather than weight-for-length percentile), and a higher prevalence of overweight among the control group at baseline.
Kavanagh et al39 conducted a clinical trial to test the effectiveness of a single educational session aimed at parents of formula-fed newborns, with the aim of reducing overfeeding and excessive infant weight gain. Parents (n=101) of formula-fed infants aged 3 to 10 weeks were recruited from 2 women, infants, and children clinics in Sacramento, California, and were randomized to 1 of 2 educational sessions conducted by clinic educators. The control session gave parents general information about infant feeding, and the intervention session added information about recognizing infant satiety cues and about limiting the volume of formula feeds to 177 mL (6 oz) per feed. There were no differences in formula intake between the control and intervention groups before and after the intervention. Infant weight, weight gain, and infant length were greater in the intervention group vs the control group. However, it was difficult to draw firm conclusions because of the lack of statistical power (a priori estimation, 125 patients per arm) and the observed 74% of the sample lost to follow up.
A small randomized trial (n=43) performed by Harvey-Berino and Rourke40 among a population of Native American children used an educational intervention designed around improving parenting skills and nutrition given by peer educators in the home over a 16-week period. Children of parents undergoing the intervention had a decrease in energy intake from their baseline values (mean [SD] reductions of −39.2 [−89.4] kcal/kg/d in the intervention group vs 6.8 [55.4] kcal/kg/d in the control group) and had decreased weight-for-height scores (mean [SD] reductions of −0.27 [−1.10] in the intervention group vs 0.31 [1.10] in the control group) (P=.06 for both).
One study36 included measures of child growth and cognitive development but found no association between nutritional counseling to reduce calorie or fat intake and physical or cognitive development. However, it is unclear if the study was sufficiently powered to show such associations.
Most studies were also limited by significant dropout rates (median, 32%; range, 7%–74%). Rates were similar regardless of study intervention location (home, clinic, classroom, community, etc).
ONGOING STUDIES
Multiple studies are ongoing to evaluate the role of obesity prevention interventions among children younger than 2 years. Four articles describing the design of studies that target children younger than 2 years (the Infant Feeding Activity and Nutrition Trial [INFANT],41 Making Our Mealtimes Special [MOMS],42 NOURISH,43 and Healthy Beginnings Trial44) were identified by our primary search but were excluded from this review because they were in progress. An additional search of ongoing studies on www.clinicaltrials.gov retrieved a total of 265 studies. Of these, 8 studies in progress seemed to match our inclusion criteria and are listed in Table 3.
Table 3.
Clinical Trials in Progress That Evaluate Obesity Prevention or Reduction Interventions in Children Younger Than 2 Years
| Clinical Trial | Location | clinicaltrials.gov Identifier |
|---|---|---|
| Trim Tots Pre-School Obesity Prevention Programme | Institute of Child Health, London, England | NCT00675662 |
| Prevention of Overweight in Infancy (POInz) | University of Otago, Dunedin, New Zealand | NCT00892983 |
| Feeding Young Children Study: Bottle Weaning Intervention (FYCS) | Montefiore Medical Center, New York, New York | NCT00756626 |
| Healthy Sleeping and Feeding During Infancy | Penn State University, Hershey, Pennsylvania | NCT00125580 |
| Vaasa Childhood Obesity Primary Prevention Study (VACOPP) | University of Tampere, Vaasa, Finland | NCT00970710 |
| European Childhood Obesity Project | University of Munich, Munich, Germany | NCT00338689 |
| The SLeeping and Intake Methods Taught to Infants and Mothers Early in Life (SLIMTIME) Project | Penn State University | NCT00359242 |
| Addressing Health Literacy and Numeracy to Prevent Childhood Obesity (GreenLight) | Vanderbilt University, Nashville, Tennessee; University of Miami, Miami, Florida; University of North Carolina, Chapel Hill; New York University, New York | NCT01040897 |
COMMENT
Although awareness about the importance of early prevention of obesity has increased, few published studies describe interventions targeting children younger than 2 years. This review builds on information in a previous review by Campbell and Hesketh,26 which primarily focused on interventions targeting older children. An additional 6 studies that investigated interventions specifically directed at children younger than 2 years were examined herein. We added an objective assessment of the methodological quality of all included studies.
Of 10 studies reviewed, only 4 were randomized trials, and they were judged to be of only fair quality. Most of the remaining studies were constrained by study designs that led to poorer quality of evidence and were further limited by minimal information provided about the intervention details. Six studies demonstrated small but statistically significant changes in process measures, such as improvement in activity level or reduction in fat consumption, but none showed a significant effect on child weight status. It is difficult to discern if this lack of improvement was primarily because of small sample sizes, short intervention periods, weak dose effects, or ineffective interventions.
Nevertheless, this review demonstrates the feasibility of interventions targeted for children younger than 2 years to affect important mediators of childhood obesity and cardiovascular disease. In the single study31 that investigated a long-term intervention and outcomes, twice-yearly nutritional education provided by a dietician as part of a well-child care visit continued to reduce dietary fat intake at follow-up 10 years after initiation of the intervention. Although the study was not designed to look at child weight status as an outcome, the potential usefulness of such an integrated approach is evident and could be adapted for obesity prevention.
This review has several important limitations. The paucity of randomized controlled trials, small study populations, and heterogeneity of interventions and study settings make it challenging to draw overarching conclusions. Six of 10 studies reviewed selected infants who had 1 or more risk factors for childhood obesity; however, because none of the studies specifically limited enrollment to children who were overweight or obese, the lack of demonstrated effect on child weight status may be the result of bias due to the inclusion of infants who were not exposed to an obesogenic environment at baseline. Seven of 12 articles reviewed were judged to be of poor quality, making it more difficult to interpret negative findings. Most articles that were judged to be of fair quality were from a single study (the STRIP study) among a Finnish population, limiting generalizability of the results. Because we reviewed only English-language literature, there may be publication bias that misinforms our conclusions.
As evidence builds that infant weight status is closely linked to the development of child and adult obesity and its associated consequences, it is imperative to develop, implement, and rigorously assess interventions designed specifically for this age group. Observational studies of infants and their families have identified several developmentally unique aspects of feeding practices and physical activity that are associated with obesity or unhealthy behaviors in later childhood and adulthood. These include but are not limited to breastfeeding exclusivity and duration, 20–22 introduction of sweetened beverages,19 and television viewing.16,17 Family-centered interventions in infancy and early childhood should target these behaviors and apply rigorous study designs to examine their effect on infant growth trajectories, as well as on family health behaviors.
Ongoing studies should help to clarify the role of interventions to prevent the development of early childhood obesity. Our review identified 12 rigorous ongoing intervention trials that include children younger than 2 years and that aim to prevent obesity or associated behaviors. Our research group is conducting a National Institutes of Health–funded randomized controlled study addressing health literacy and health communication issues to help promote improved lifestyle behaviors and to prevent obesity development among children in the first 2 years of life (clinicaltrials.gov identifier NCT01040897). Evidence from the studies reviewed herein should help guide future efforts to develop feasible interventions based in the home, clinic, classroom, or community to support healthier infant growth and development.
Acknowledgments
Funding/Support: This study was supported in part by the Veterans Affairs Quality Scholars Fellowship Program (Dr Ciampa); Robert Wood Johnson Generalist Physician Scholars Program (Dr Sanders), career development award K23 HD051817 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Dr Perrin), career development award 5K23 DK065294 from the National Institute of Diabetes and Digestive and Kidney Diseases (Dr Rothman), and grant R01 HD059794 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Author Contributions: Study concept and design: Kumar, Sanders, and Rothman. Acquisition of data: Ciampa, Kumar, and Perrin. Analysis and interpretation of data: Ciampa, Kumar, Barkin, Sanders, Yin, Perrin, and Rothman. Drafting of the manuscript: Ciampa, Kumar, and Sanders. Critical revision of the manuscript for important intellectual con-tent: Kumar, Barkin, Sanders, Yin, Perrin, and Rothman. Administrative, technical, and material support: Ciampa and Sanders. Study supervision: Barkin, Sanders, and Rothman.
Financial Disclosure: None reported.
REFERENCES
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Nader PR, O’Brien M, Houts R. National Institute of Child Health and Human Development Early Child Care Research Network. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 3.Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics. 2002;109(2):194–199. doi: 10.1542/peds.109.2.194. [DOI] [PubMed] [Google Scholar]
- 4.Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77(6):1374–1378. doi: 10.1093/ajcn/77.6.1374. [DOI] [PubMed] [Google Scholar]
- 5.Eid EE. Follow-up study of physical growth of children who had excessive weight gain in first six months of life. Br Med J. 1970;2(5701):74–76. doi: 10.1136/bmj.2.5701.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gunnarsdottir I, Thorsdottir I. Relationship between growth and feeding in infancy and body mass index at the age of 6 years. Int J Obes Relat Metab Disord. 2003;27(12):1523–1527. doi: 10.1038/sj.ijo.0802438. [DOI] [PubMed] [Google Scholar]
- 7.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. [Accessed September 13, 2010];BMJ. 2005 331(7522):929. doi: 10.1136/bmj.38586.411273.E0. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1261184/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro PO, Victora CG. Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obes Rev. 2005;6(2):143–154. doi: 10.1111/j.1467-789X.2005.00183.x. [DOI] [PubMed] [Google Scholar]
- 9.Dennison BA, Edmunds LS, Stratton HH, Pruzek RM. Rapid infant weight gain predicts childhood overweight. Obesity (Silver Spring) 2006;14(3):491–499. doi: 10.1038/oby.2006.64. [DOI] [PubMed] [Google Scholar]
- 10.Hui LL, Schooling CM, Leung SS, et al. Birth weight, infant growth, and childhood body mass index: Hong Kong’s children of 1997 birth cohort. Arch Pediatr Adolesc Med. 2008;162(3):212–218. doi: 10.1001/archpediatrics.2007.62. [DOI] [PubMed] [Google Scholar]
- 11.Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA. 2009;301(21):2234–2242. doi: 10.1001/jama.2009.761. [DOI] [PubMed] [Google Scholar]
- 12.Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics. 2009;123(4):1177–1183. doi: 10.1542/peds.2008-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox MK, Reidy K, Novak T, Ziegler P. Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc. 2006;106(suppl 1)(1):S28–S42. doi: 10.1016/j.jada.2005.09.034. [DOI] [PubMed] [Google Scholar]
- 14.Mannino ML, Lee Y, Mitchell DC, Smiciklas-Wright H, Birch LL. The quality of girls’diets declines and tracks across middle childhood. Int J Behav Nutr Phys Act. 2004;1(1):5. doi: 10.1186/1479-5868-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoerr SL, Lee SY, Schiffman RF, Horodynski MO, McKelvey L. Beverage consumption of mother-toddler dyads in families with limited incomes. J Pediatr Nurs. 2006;21(6):403–411. doi: 10.1016/j.pedn.2006.01.035. [DOI] [PubMed] [Google Scholar]
- 16.Certain LK, Kahn RS. Prevalence, correlates, and trajectory of television viewing among infants and toddlers. Pediatrics. 2002;109(4):634–642. doi: 10.1542/peds.109.4.634. [DOI] [PubMed] [Google Scholar]
- 17.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 18.Marshall TA, Levy SM, Broffitt B, Eichenberger-Gilmore JM, Stumbo PJ. Patterns of beverage consumption during the transition stage of infant nutrition. J Am Diet Assoc. 2003;103(10):1350–1353. doi: 10.1016/s0002-8223(03)01078-2. [DOI] [PubMed] [Google Scholar]
- 19.Faith MS, Dennison BA, Edmunds LS, Stratton HH. Fruit juice intake predicts increased adiposity gain in children from low-income families: weight status-byenvironment interaction. Pediatrics. 2006;118(5):2066–2075. doi: 10.1542/peds.2006-1117. [DOI] [PubMed] [Google Scholar]
- 20.Dietz WH. Breastfeeding may help prevent childhood overweight. JAMA. 2001;285(19):2506–2507. doi: 10.1001/jama.285.19.2506. [DOI] [PubMed] [Google Scholar]
- 21.von Kries R, Koletzko B, Sauerwald T, et al. Breast feeding and obesity: cross sectional study. BMJ. 1999;319(7203):147–150. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dewey KG. Growth characteristics of breast-fed compared to formula-fed infants. Biol Neonate. 1998;74(2):94–105. doi: 10.1159/000014016. [DOI] [PubMed] [Google Scholar]
- 23.Arenz S, Rückerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity—a systematic review. Int J Obes Relat Metab Disord. 2004;28(10):1247–1256. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- 24.Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162(5):397–403. doi: 10.1093/aje/kwi222. [DOI] [PubMed] [Google Scholar]
- 25.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115(5):1367–1377. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 26.Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years: a systematic review of the literature. Obes Rev. 2007;8(4):327–338. doi: 10.1111/j.1467-789X.2006.00305.x. [DOI] [PubMed] [Google Scholar]
- 27.Benjamin SE, Rifas-Shiman SL, Taveras EM, et al. Early child care and adiposity at ages 1 and 3 years. Pediatrics. 2009;124(2):555–562. doi: 10.1542/peds.2008-2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.West S, King V, Carey TS, et al. Systems to rate the strength of scientific evidence. Evid Rep Technol Assess (Summ) 2002;(47):1–11. [PMC free article] [PubMed] [Google Scholar]
- 29.Lagström H, Jokinen E, Seppänen R, et al. Nutrient intakes by young children in a prospective randomized trial of a low-saturated fat, low-cholesterol diet: the STRIP Baby Project: Special Turku Coronary Risk Factor Intervention Project for Babies. Arch Pediatr Adolesc Med. 1997;151(2):181–188. doi: 10.1001/archpedi.1997.02170390071013. [DOI] [PubMed] [Google Scholar]
- 30.Simell O, Niinikoski H, Rönnemaa T, et al. Special Turku Coronary Risk Factor Intervention Project for Babies (STRIP) Am J Clin Nutr. 2000;72(suppl)(5):1316S–1331S. doi: 10.1093/ajcn/72.5.1316s. [DOI] [PubMed] [Google Scholar]
- 31.Talvia S, Lagström H, Räsänen M, et al. A randomized intervention since infancy to reduce intake of saturated fat: calorie (energy) and nutrient intakes up to the age of 10 years in the Special Turku Coronary Risk Factor Intervention Project. Arch Pediatr Adolesc Med. 2004;158(1):41–47. doi: 10.1001/archpedi.158.1.41. [DOI] [PubMed] [Google Scholar]
- 32.Wolman J, Skelly E, Kolotourou M, Lawson M, Sacher P. Tackling toddler obesity through a pilot community-based family intervention. Community Pract. 2008;81(1):28–31. [PubMed] [Google Scholar]
- 33.Klohe-Lehman DM, Freeland-Graves J, Clarke KK, et al. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. J Am Coll Nutr. 2007;26(3):196–208. doi: 10.1080/07315724.2007.10719602. [DOI] [PubMed] [Google Scholar]
- 34.Horodynski MA, Stommel M. Nutrition Education Aimed at Toddlers: an intervention study [published correction appears in Pediatr Nurs. 2006; 32(1):96] Pediatr Nurs. 2005;31(5):364–372. [PubMed] [Google Scholar]
- 35.Horodynski MA, Hoerr S, Coleman G. Nutrition education aimed at toddlers: a pilot program for rural, low-income families. Fam Community Health. 2004;27(2):103–113. doi: 10.1097/00003727-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Worobey J, Pisuk J, Decker K. Diet and behavior in at-risk children: evaluation of an early intervention program. Public Health Nurs. 2004;21(2):122–127. doi: 10.1111/j.0737-1209.2004.021205.x. [DOI] [PubMed] [Google Scholar]
- 37.Adam HM, Stern EK, Stein RE. Anticipatory guidance: amodest intervention in the nursery. Pediatrics. 1985;76(5):781–786. [PubMed] [Google Scholar]
- 38.Pisacano JC, Lichter H, Ritter J, Siegal AP. An attempt at prevention of obesity in infancy. Pediatrics. 1978;61(3):360–364. doi: 10.1542/peds.61.3.360. [DOI] [PubMed] [Google Scholar]
- 39.Kavanagh KF, Cohen RJ, Heinig MJ, Dewey KG. Educational intervention to modify bottle-feeding behaviors among formula-feeding mothers in the WIC program: impact on infant formula intake and weight gain. J Nutr Educ Behav. 2008;40(4):244–250. doi: 10.1016/j.jneb.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 40.Harvey-Berino J, Rourke J. Obesity prevention in preschool native-American children: a pilot study using home visiting. Obes Res. 2003;11(5):606–611. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- 41.Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster-randomised controlled trial. [Accessed September 13, 2010];BMC Public Health. 2008 8:103. doi: 10.1186/1471-2458-8-103. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2346474/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Groner JA, Skybo T, Murray-Johnson L, et al. Anticipatory guidance for prevention of childhood obesity: design of the MOMS project. Clin Pediatr (Phila) 2009;48(5):483–492. doi: 10.1177/0009922809331799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Daniels LA, Magarey A, Battistutta D, et al. The NOURISH randomised control trial: positive feeding practices and food preferences in early childhood—a primary prevention program for childhood obesity. [Accessed September 13, 2010];BMC Public Health. 2009 9:387. doi: 10.1186/1471-2458-9-387. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2770488/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wen LM, Baur LA, Rissel C, Wardle K, Alperstein G, Simpson JM. Early intervention of multiple home visits to prevent childhood obesity in a disadvantaged population: a home-based randomised controlled trial (Healthy Beginnings Trial) [Accessed September 13, 2010];BMC Public Health. 2007 7:76. doi: 10.1186/1471-2458-7-76. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1877802/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]