Abstract
INTRODUCTION
The purpose of this study was to determine if hip resurfacing arthroplasty (HRA) and cementless total hip arthroplasty (THA) were comparable in correcting leg length and hip offset in patients with primary osteoarthritis.
METHODS
A retrospective analysis was performed of 80 patients who underwent either HRA or cementless THA for primary osteoarthritis (40 in each group) between 2006 and 2008. Standardised anteroposterior radiographs taken pre-operatively and at one year following surgery were used to calculate the total offset and leg length in both hips.
RESULTS
At one year following surgery, no leg length discrepancy was identified in either group. A difference of 0.39cm (p=0.046) remained between the mean total offset of the operated hip and the contralateral non-operated hip in the HRA group. No difference in offset was observed between the two hips after surgery in the THA group (p=0.875).
CONCLUSIONS
Leg length is restored by HRA and THA. A difference remains in offset after HRA although we attribute this to intentional medialisation of the acetabular cup.
Keywords: Arthroplasty, Replacement, Hip, Leg length inequality, Biomechanics
More than 71,000 primary total hip arthroplasty (THA) procedures were performed in England and Wales in 2009, a figure that has risen annually since the National Joint Registry's inception.1 Cemented procedures are now less popular, dropping from 54% of the total performed in 2005 to 36% in 2009, while cementless surgeries rose from 22% in 2005 to 39% in 2009. This total figure includes hip resurfacing arthroplasty (HRA), which became popular following its reintroduction in the 1990s although a reported rise in complications has led to surgeons using it more selectively.
One appeal of HRA is the reduced wear profile produced over hard-on-soft bearings,2 which are the most commonly used articulation in ‘conventional THA’ (and will herein be referred to as THA in order to differentiate it from HRA). Bone resection of the femur is also reduced,3 which means revision to THA is only as difficult as performing primary THA.4 Finally, the large head required in HRA lowers the risk of dislocation and is associated with higher levels of activity, especially in the young,5 for whom it is mostly indicated.
Irrespective of whether THA or HRA is performed, restoration of normal biomechanical parameters is sought for a number of reasons. Reconstructing offset correlates with improved abductor function6,7 and reduced wear.8 Limb length inequality after hip arthroplasty, however, is a cause of patient dissatisfaction, gait abnormalities, back pain and sciatic nerve palsy, all of which are factors for litigation against the surgeon.9–11
At present, variability exists in the literature as to whether biomechanical restoration between HRA and THA is comparable.12–16 Cementless THA is an important group against which to evaluate HRA since, as mentioned, its usage is increasing proportionately while the absence of cement affords less flexibility in final component orientation and position. Using our cohort of patients who have undergone hip reconstruction, we compared the changes in leg length and offset between HRA and THA groups of patients treated for primary osteoarthritis. Our null hypothesis was that the post-operative femoral offset and the leg length would be equal in both hips.
Methods
A retrospective analysis was performed of patients undergoing HRA or THA between 2006 and 2008. The study inclusion criterium was primary arthroplasty for hip osteoarthritis. Patients were excluded from the study if they had contralateral hip arthroplasty, radiographic evidence of grade 2 or more changes in the contralateral hip using the Kellgren and Lawrence scale17 (Table 1) or inadequate radiographs.
Table 1.
Kellgren and Lawrence grading scale for osteoarthritis17
| Grade | Radiological findings |
|---|---|
| 0 | Normal |
| 1 | Doubtful narrowing of joint space and possible osteophytic lipping |
| 2 | Definite osteophytes, definite narrowing of joint space |
| 3 | Moderate multiple osteophytes, definite narrowing of joints space, some sclerosis and possible deformity of bone contour |
| 4 | Large osteophytes, marked narrowing of joint space, severe sclerosis and definite deformity of bone contour |
Forty consecutive cases of HRA and forty consecutive cases of THA meeting the eligibility criteria were identified. There were 28 men and 12 women in the HRA group with a mean age of 54 years (range: 42–71 years). There were 13 men and 27 women in the THA group with a mean age of 68 years (range: 55–78 years). All operations were performed through the posterior approach by a single surgeon with extensive experience of both HRA and THA, with the aim of correcting leg length discrepancy, restoring offset and ensuring joint stability.
The Birmingham Hip Resurfacing™ (Smith & Nephew, Memphis, TN, US) system was used for all operations in the HRA group. It comprises a cemented femoral head and cementless acetabular shell producing a cobalt-chromium metal-on-metal articulation. All operations in the THA group were performed using the Synergy™ (Smith & Nephew, Memphis, TN, US) femoral system, which is a cementless, hydroxyapatite-coated, proximally porous stem available in standard and high offset versions, and Reflection™ (Smith & Nephew, Memphis, TN, US) acetabular system, which is a cementless, porous coated shell. All surgeries coupled a 32mm cobalt-chromium head with a 20° posterior lipped, highly cross-linked polyethylene liner; no lateralised liners were used.
Radiographic assessment
Anteroposterior radiographs of the pelvis were used for assessment. They were obtained using a standardised protocol: the patient was supine with feet parallel using a 100cm focal radiograph distance and the beam aimed at the centre of the image plate, which was positioned to include the iliac crest at its superior edge. The images were obtained pre-operatively and at the first annual follow-up appointment (mean: 13.1 months, range: 11–14 months). All pre-operative radiographs included in this study were additionally templated using the IMPAX™ orthopaedic suite (Agfa HealthCare, Mortsel, Belgium) to identify levels of resection and offer a guide to the expected size of implant needed.
The biomechanical parameters were determined with widely used methods described by Woolson et al18 and Jolles et al19 (Fig 1). Femoral length (used as a surrogate for leg length) was defined as the perpendicular distance from the trans-teardrop line to the most prominent medial point of the lesser trochanter. Cup offset (also known as acetabular offset) was defined as the distance from the centre of rotation of the femoral head to the teardrop along the trans-teardrop line. Femoral offset was defined as the distance from the centre of rotation of the femoral head to the central axis of the femur. The total offset was the summation of the cup offset and femoral offset.
Figure 1.
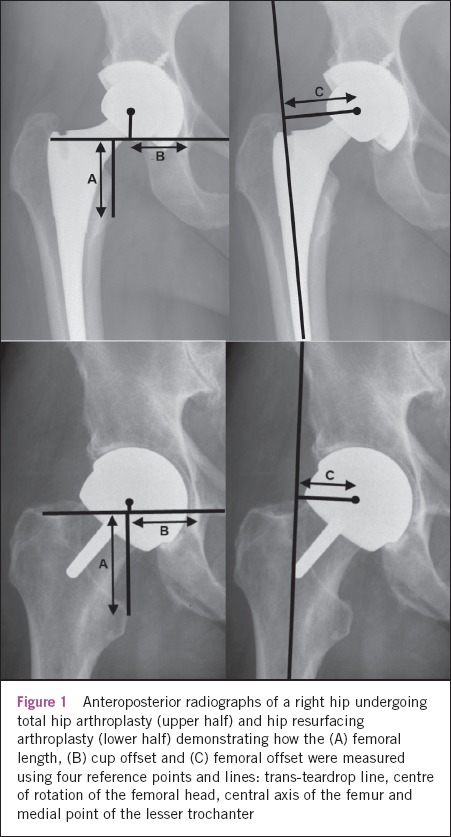
Anteroposterior radiographs of a right hip undergoing total hip arthroplasty (upper half) and hip resurfacing arthroplasty (lower half) demonstrating how the (A) femoral length, (B) cup offset and (C) femoral offset were measured using four reference points and lines: trans-teardrop line, centre of rotation of the femoral head, central axis of the femur and medial point of the lesser trochanter
Measurements were taken of both hips on pre- and postoperative radiographs by two observers (SP and FH) on two occasions at an interval of six weeks.
Statistical analysis
Statistical analysis was carried out using MedCalc® version 11.3.0 (MedCalc Software, Mariakerke, Belgium). The Wilcoxon rank-sum test was used to assess the difference in paired measurements. The Mann–Whitney U test was used to assess the difference in unpaired measurements. A statistical value of p<0.05 was considered to be significant. An intra-class correlation coefficient was used to assess the agreement among raters (inter-rater reliability) and test–retest reliability (intra-rater reliability).
Results
The pre-operative hips were on average shorter than the normal contralateral side in both HRA (0.09cm) and THA (0.29cm) groups but neither group was significantly shorter than the other (p=0.196). The mean cup offset was larger and femoral offset lower in the diseased hips for both groups. While the cup offset was greater in the HRA group (0.35cm vs 0.04cm, p=0.003), which contributed to a larger total offset (0.02 vs -0.25cm), the final difference once femoral offset was taken in account was not statistically significant (p=0.192). In summary, the pre-operative hips in both groups had comparable discrepancies in leg length and total offset (Table 2).
Table 2.
Difference in biomechanical parameters between the pre-operated and contralateral hip with the data split by implant group
| Femoral length (cm) | Cup offset (cm) | Femoral offset (cm) | Total offset (cm) | ||
|---|---|---|---|---|---|
| HRA | Mean (SD) | -0.09 (0.59) | 0.35 (0.55) | -0.33 (0.77) | 0.02 (0.82) |
| Range | -1.40 to 1.12 | -1.13 to 1.94 | -1.86 to 1.21 | -1.58 to 2.24 | |
| THA | Mean (SD) | -0.29 (0.78) | 0.04 (0.42) | -0.29 (0.58) | -0.25 (0.66) |
| Range | -3.72 to 1.13 | -0.84 to 1.05 | -1.57 to 0.81 | -1.43 to 0.77 | |
| p-value | 0.196 | 0.003 | 0.923 | 0.192 |
HRA = hip resurfacing arthroplasty; THA = total hip arthroplasty
After surgery, the hips in the HRA group were similar in femoral length (p=0.268) but not total offset, which was lower on the operated side (8.69 vs 9.08cm, p=0.046). Splitting the total offset into its two components shows its failure to recreate cup offset, from which this reduction originates, with the mean cup offset 0.36cm lower on the operated hip (Table 3).
Table 3.
Differences between the mean biomechanical parameters of the post-operative and contralateral hip for hip resurfacing arthroplasty
| Femoral length (cm) | Cup offset (cm) | Femoral offset (cm) | Total offset (cm) | ||
|---|---|---|---|---|---|
| Operated hip | Mean (SD) | 4.40 (0.60) | 3.93 (0.51) | 4.76 (0.92) | 8.69 (1.17) |
| Range | 3.40–4.71 | 2.80–4.98 | 2.59–6.82 | 5.88–10.90 | |
| Contralateral hip | Mean (SD) | 4.62 (0.63) | 4.29 (0.62) | 4.79 (0.84) | 9.08 (1.00) |
| Range | 3.23–4.92 | 2.89–5.30 | 3.52–7.07 | 7.03–1.20 | |
| p-value | 0.268 | <0.0001 | 0.430 | 0.046 |
SD = standard deviation
Although hips in the THA group remained shorter by a mean of 0.22cm, this difference was not significant (p=0.059). Like the HRA group, the cup offset was lower on the operated hip (3.73cm vs 3.99cm, p=0.017) although, in contrast, the total offset was also comparable (8.19cm vs 8.39cm, p=0.875) (Table 4).
Table 4.
Differences between the mean biomechanical parameters of the post-operative and contralateral hip for total hip arthroplasty
| Femoral length (cm) | Cup offset (cm) | Femoral offset (cm) | Total offset (cm) | ||
|---|---|---|---|---|---|
| Operated hip | Mean (SD) | 4.42 (0.88) | 3.73 (0.48) | 4.46 (0.79) | 8.19 (0.91) |
| Range | 2.90–7.26 | 3.09–4.86 | 3.34–6.26 | 6.72–10.73 | |
| Contralateral hip | Mean (SD) | 4.58 (0.53) | 3.99 (0.62) | 4.38 (0.74) | 8.37 (0.99) |
| Range | 3.50–6.08 | 3.12–5.65 | 2.90–5.65 | 6.39–10.42 | |
| p-value | 0.059 | 0.017 | 0.875 | 0.875 |
SD = standard deviation
Inter-rater and intra-rater agreement was classed20 as good to excellent for all categories (Table 5). It was greatest when measuring leg length, which relied on bony landmarks, rather than offset, which relied on the observers' identification of the femoral head centre and the central femoral axis.
Table 5.
Reliability of each biomechanical measure
| Intra-class correlation coefficient | ||
|---|---|---|
| Inter-rater reliability (95% CI) | Intra-rater reliability (95% CI) | |
| Femoral length | 0.93 (0.87–0.99) | 0.91 (0.86–0.96) |
| Cup offset | 0.83 (0.77–0.89) | 0.86 (0.78–0.93) |
| Femoral offset | 0.78 (0.72–0.84) | 0.74 (0.69–0.79) |
CI = confidence interval
Discussion
This study evaluated the differences produced in leg length and hip offset after two methods of hip arthroplasty. Our null hypothesis was that HRA and THA would be comparable in biomechanical correction. However, HRA was found to correct leg length but not total offset while THA was able to correct both these parameters.
There are strengths with this work. We excluded those with evidence of joint space narrowing on the contralateral limb, which allowed us to determine whether the arthroplasty performed restored the hip back to its ‘normal’ state in the entire cohort. To further minimise bias against one particular group, all operations were performed by a single surgeon, thereby minimising surgical variability in determining bone resection and component positioning. Furthermore, the method of analysis was reproducible between observers and on retesting.
The main limitation of this work is that it is not a randomised study. However, since the indications for HRA are more limited following the publication of adverse reports in specific patient groups, this was not possible. The refinement in indications is illustrated by the differing patient demographics between the two groups: the HRA group contained younger patients with a male dominance. To minimise variability further in the patient groups, we therefore included those only operated on for a single indication: osteoarthritis.
An early report of HRA from de Smet et al concluded that it met expectations in restoring leg length and offset.21 These conclusions were based on a single cohort of 310 HRA patients and only leg length was measured. Furthermore, measurements were pre- and post-surgery of the operated hip only. They noted only no clear change in this value and did not compare values to those of the contra-lateral hip.
Silva et al12 compared two similar groups to those in our study (HRA versus cementless THA) although the values measured differed. They measured horizontal and vertical femoral offset to show an 8mm decrease in horizontal offset in their HRA group and a 5mm increase in their THA group compared to the normal contralateral side. Vertical offset increased by 2.4–2.9mm in both groups compared to the normal contralateral side. This global increase in offset in the THA group may be attributable to the use of a high offset femoral implant. In contrast, we used both normal and high offset stems, which allowed a further option for anatomic reconstruction and may explain why no significant difference was seen in offset values in our THA group compared with the contralateral hip. Concerning leg length, that of Silva et al's HRA group was still shorter by 2mm although it was equal in the THA group.
A subsequent randomised study by Girard et al also contained a cementless THA group.14 They noted horizontal femoral offset significantly larger by 5mm than the contralateral side in the THA group and lower by 3mm in the HRA group, with the difference between these values also reaching statistical significance. Final leg length was 3mm longer in the THA group and 2mm shorter in the SRA group compared to the contralateral side, with more patients in this group falling within the standard deviation. While Silva et al thus concluded that there are biomechanical limitations to HRA that will not change offset and can only increase length by 1cm,12 Girard et al suggested that HRA is more accurate for anatomical restoration.14
Other studies evaluating leg length and offset in HRA and THA have used cemented implants, either as a hybrid system (cemented stem and cementless shell) or dually cemented (both stem and cup). Two studies investigating hybrid systems13,16 have compared post-operative values against pre-operative values of the operated hip to determine the changes produced by surgery though they agreed in only three areas: firstly, that leg length increased after both HRA and THA; secondly, that cup offset reduced after THA; and thirdly, that femoral offset decreased after HRA.
Of these two studies, Loughead et al has described using the contralateral hip additionally as a control in the methodology although they note only that the absolute differences between these measures was small in the results.13 It may be inferred from this statement that both HRA and hybrid THA restored offset and leg length even though no supplemental data were presented in the paper to support this. Fully cemented THA was assessed by Robb et al15 in a similar manner to our study although their results do contrast with ours. They observed no difference between HRA and cemented THA groups for leg length and cup offset when comparing the operated and contralateral side. However, femoral and total offset were found to be more accurately restored with HRA.
It is likely that differences in operative technique to other study groups contributed towards our differing results. In particular, in the HRA group we noted a lower total offset than for the normal hip. This came from a lower cup offset, which would indicate we have medialised the acetabular component. Assuming that medialisation would lead to greater acetabular bone resection, it is unclear whether this is normal practice. Our results would corroborate early published data22 even though other authors argue that an equal amount of bone is removed between the two procedures,23 especially in men, and perhaps even less is resected in women.24
While loss of bone stock is never desired in any joint arthroplasty, the question arises whether medialisation is in fact a necessary step in HRA. Risk factors for early failure and increased metal ion release include small component size and high abduction angle of the acetabular component.25,26 This can be combated by using a large cup, which in turn is facilitated by medialisation to ensure superior coverage and thus host bone contact with the screwless, cementless implant. Furthermore, medialisation allows the acetabular component to be placed in a more shallow inclination for the same reasons and also facilitates anterior coverage, which should lessen the likelihood of psoas impingement. It may therefore be that our practice leads to improved survivorship although this was not evaluated in this study.
Both implants were able to eliminate the pre-existing leg length discrepancy. The THA group benefited from the availability of different head lengths to achieve this although correct assessment of the required height of the neck cut was invariably contributory. HRA is not modular and so leg length is more difficult to correct. We nevertheless achieved length by placing the resection guide proximal to the head–neck junction at the level templated for on radiographs.
Conclusions
Leg length is restored by HRA and THA. A difference remains in offset in the HRA group although we attribute this to intentional medialisation of the acetabular cup.
Conflicts of Interest
Fares Haddad receives research funding from Smith & Nephew.
References
- 1.National Joint Registry. 7th Annual Report 2010. Hemel Hempstead: NJR; 2010. [Google Scholar]
- 2.Goldsmith AA, Dowson D, Isaac GH, Lancaster JG. A comparative joint simulator study of the wear of metal-on-metal and alternative material combinations in hip replacements. Proc Inst Mech Eng H. 2000;214:39–47. doi: 10.1243/0954411001535228. [DOI] [PubMed] [Google Scholar]
- 3.Su EP, Sheehan M, Su SL. Comparison of bone removed during total hip arthroplasty with a resurfacing or conventional femoral component: a cadaveric study. J Arthroplasty. 2010;25:325–329. doi: 10.1016/j.arth.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Ball ST, Le Duff MJ, Amstutz HC. Early results of conversion of a failed femoral component in hip resurfacing arthroplasty. J Bone Joint Surg Am. 2007;89:735–741. doi: 10.2106/JBJS.F.00708. [DOI] [PubMed] [Google Scholar]
- 5.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 6.Asayama I, Naito M, Fujisawa M, Kambe T. Relationship between radiographic measurements of reconstructed hip joint position and the Trendelenburg sign. J Arthroplasty. 2002;17:747–751. doi: 10.1054/arth.2002.33552. [DOI] [PubMed] [Google Scholar]
- 7.Kiyama T, Naito M, Shinoda T, Maeyama A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J Arthroplasty. 2010;25:76–80. doi: 10.1016/j.arth.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Little NJ, Busch CA, Gallagher JA, et al. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467:2,895–2,900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark CR, Huddleston HD, Schoch EP 3rd, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:38–45. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka R, Shigematsu M, Motooka T, et al. Factors influencing the improvement of gait ability after total hip arthroplasty. J Arthroplasty. 2010;25:982–985. doi: 10.1016/j.arth.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 11.Hofmann AA, Skrzynski MC. Leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits! Orthopedics. 2000;23:943–944. doi: 10.3928/0147-7447-20000901-20. [DOI] [PubMed] [Google Scholar]
- 12.Silva M, Lee KH, Heisel C, et al. The biomechanical results of total hip resurfacing arthroplasty. J Bone Joint Surg Am. 2004;86:40–46. doi: 10.2106/00004623-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Loughead JM, Chesney D, Holland JP, McCaskie AW. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg Br. 2005;87:163–166. doi: 10.1302/0301-620x.87b2.15151. [DOI] [PubMed] [Google Scholar]
- 14.Girard J, Lavigne M, Vendittoli PA, Roy AG. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88:721–726. doi: 10.1302/0301-620X.88B6.17447. [DOI] [PubMed] [Google Scholar]
- 15.Robb C, Harris R, O'Dwyer K, Aslam N. Radiographic assessment of biomechanical parameters following hip resurfacing and cemented total hip arthroplasty. Hip Int. 2009;19:251–256. doi: 10.1177/112070000901900311. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad R, Gillespie G, Annamalai S, et al. Leg length and offset following hip resurfacing and hip replacement. Hip Int. 2009;19:136–140. doi: 10.1177/112070000901900210. [DOI] [PubMed] [Google Scholar]
- 17.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14:159–164. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 19.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 21.de Smet KA, Pattyn C, Verdonk R. Early results of primary Birmingham hip resurfacing using a hybrid metal-on-metal couple. Hip Int. 2002;12:158–162. doi: 10.1177/112070000201200225. [DOI] [PubMed] [Google Scholar]
- 22.Loughead JM, Starks I, Chesney D, et al. Removal of acetabular bone in resurfacing arthroplasty of the hip: a comparison with hybrid total hip arthroplasty. J Bone Joint Surg Br. 2006;88:31–34. doi: 10.1302/0301-620X.88B1.16764. [DOI] [PubMed] [Google Scholar]
- 23.Vendittoli PA, Lavigne M, Girard J, Roy AG. A randomised study comparing resection of acetabular bone at resurfacing and total hip replacement. J Bone Joint Surg Br. 2006;88:997–1,002. doi: 10.1302/0301-620X.88B8.17615. [DOI] [PubMed] [Google Scholar]
- 24.Moonot P, Singh PJ, Cronin MD, et al. Birmingham hip resurfacing: is acetabular bone conserved? J Bone Joint Surg Br. 2008;90:319–323. doi: 10.1302/0301-620X.90B3.18803. [DOI] [PubMed] [Google Scholar]
- 25.Ollivere B, Darrah C, Barker T, et al. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br. 2009;91:1,025–1,030. doi: 10.1302/0301-620X.91B8.21701. [DOI] [PubMed] [Google Scholar]
- 26.De Haan R, Pattyn C, Gill HS, et al. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1,291–1,297. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]


