Abstract
This study aimed to examine the disturbance of hand sensation in patients with carpal tunnel syndrome (CTS) and assess the usefulness of objective and subjective measures. The study included 64 patients with CTS confirmed by electrophysiological testing. Sensory assessment was made by objective (pressure aesthesiometry) and subjective (hand symptom diagram) measures in different anatomical areas. The results of the subjective and objective testing were correlated with nerve conduction studies by a kappa analysis. Sensory disturbance occurred more frequently in areas innervated by the median nerve (index finger, 94%) but also with great frequency in other areas (little finger, 39%). Pain occurred frequently in anticipated areas (wrist crease, 33%) but also in other areas (little finger, 11%). There was very poor correlation between objective measures and electrophysiological testing or subjective measures. This study does therefore not support the use of objective sensory assessment for the initial diagnosis of CTS. An atypical distribution of symptoms is a common occurrence and should not discourage diagnosis of CTS. The patient's description of symptoms remains the most important tool in diagnosis.
Keywords: Carpal tunnel syndrome, Sensibility
Carpal tunnel syndrome (CTS) is caused by compression of the median nerve and is the most common compressive neuropathy. The median nerve innervates the radial three and a half digits and it is sometimes assumed that this area will be where the disease manifests its symptoms. Clinicians frequently encounter patients with an atypical distribution of symptoms who have a diagnosis of CTS confirmed by nerve conduction studies (NCS) and whose symptoms are relieved by carpal tunnel decompression. These presentations occur with such frequency that many clinicians do not consider an atypical presentation as unusual.
The classical description given by the patient is of waking from sleep with tingling or uncomfortable numbness in the hand that is relieved by vigorously shaking the hand. Disturbances of sensation by paraesthesia, dysaesthesia and pain are the hallmark features of CTS. There are other aspects of the disease such as weakness, trophic changes and muscle wasting but because these are normally seen at later stages of the disease they are less useful in diagnosis. In the context of a classical history for CTS, NCS1 are usually considered the gold standard diagnostic test although this in itself is controversial.2 NCS are not always readily available and can be uncomfortable for the patient. Some would argue that the true gold standard for research should be the resolution of symptoms three months after surgical decompression.
A broad variety of tests exist for CTS; the majority of diagnoses are made by assessment of disturbed sensation through history and examination. Evaluation of sensation that relies on patient history is often termed subjective while tests and examinations performed by the doctor are termed objective. Subjective evaluation can be formalised by use of a hand diagram on which the patient can record the site of their symptoms.3 Objective tests for acute disturbance of sensation measure threshold light touch sensation by evaluation of pressure aesthesiometry with nylon monofilaments.4 Several provocative tests exist that are well established and routinely used in daily practice.5–10 After surgery the success of nerve regeneration can be assessed by evaluation of sensitivity density through two-point discrimination.6 This array of possible examinations and investigations is summarised in Table 1; the list is not exhaustive.
Table 1.
Tests for carpal tunnel syndrome
| Type of evaluation | Specific tests |
|---|---|
| ‘Gold standard’ | Nerve conduction studies |
| Provocative tests | Tinel's sign |
| Phalen's test | |
| Hand elevation test | |
| Carpal compression test | |
| Tourniquet test | |
| Objective measures of sensibility | Pressure aesthesiometry (threshold) |
| Two-point discrimination (density) | |
| Subjective measures of sensibility | Katz hand diagram |
| Patient history |
Subjective evaluation of CTS relies on patient reporting of symptoms and this is notoriously variable. Clinicians often assume that the problem with the variable reporting of symptoms stems from difficulty in remembering or understanding symptoms. Objective tests are attractive to the clinician as to some degree they exclude the self-reporting of symptoms. The objective tests do, however, continue to rely on the patient's response to questions so the subjective element is not entirely excluded.
The aim of this study was to examine the distribution of altered sensation and pain experienced by the patients with CTS and to assess the usefulness of objective and subjective assessment of this distribution.
Methods
From September 2004 to July 2005, 142 consecutive patients with hand dysaesthesia and a diagnosis of CTS confirmed by NCS were evaluated. Patients were excluded if they were pregnant or if they had hypo-/hyperthyroidism, acromegaly, diabetes, cervical spondylopathy, acute dysaesthesia following trauma, generalised peripheral neuropathy, or symptomatic hand or wrist arthritis. Where disease was bilateral (36 cases) we excluded one wrist by random selection using an internet-based random number generator (http://www.random.org/). There remained 64 wrists in 64 patients with CTS. The ratio of women to men was 3:1 and the mean age was 58 years (range: 25–88 years). All patients had their diagnosis confirmed by NCS before clinical assessment, which was performed as follows:
Katz hand diagram (subjective)
Patients were asked to fill out a Katz hand diagram and to report their symptoms using two broad categories. They marked either pain or any non-painful stimuli including tingling, numbness and decreased sensation. We divided the hand diagrams into anatomical areas that included the thenar and hypothenar eminences, the distal palm, each digit, the posterior hand and the forearm. Pain and sensory disturbances were evaluated and recorded separately.
Semmes–Weinstein monofilament (objective)
Pressure density aesthesiometry was assessed by an investigator (RA), who was not aware of the results of the NCS at the time of testing. The equipment used was the Semmes–Weinstein monofilament system (SWM, Research Design Inc, Houston, TX, US).4,11 As these tests are heavily dependant on patient understanding, the patients underwent an education session that consisted of demonstration of pressure aesthesiometry on the foot. All patients reported normal aesthesiometry on the foot.
Each hand digit was assessed once with each nylon fibre. The nylon fibre was held at a right angle to the skin and depressed until either the patient felt the stimulation or until the fibre bent. Progressively larger fibres were used until the patient was able to identify the pressure; the array of fibres used in this study was 2.83, 3.61, 4.31 and 4.56. There is controversy about whether an unrecognised 3.61 filament should be considered as normal (high threshold) or abnormal (low threshold). These two eventualities are displayed in Table 2.
Table 2.
Difference between low and high threshold Semmes–Weinstein monofilament test
| Finest monofilament sensed by patient | Low threshold test | High threshold test |
|---|---|---|
| 2.83 | Normal | Normal |
| 3.61 | Abnormal | Normal |
| 4.31 | Abnormal | Abnormal |
| 4.46 | Abnormal | Abnormal |
Statistical analysis of agreement was performed with a kappa analysis using SPSS® version 13 (SPSS Inc, Chicago, IL, US). Simple calculations were made with Microsoft® Excel® 2008.
Results
Non-painful sensory disturbance (tingling, numbness or decreased sensation) occurred in all patients. The index finger was the most common location (94%) followed by the middle finger (91%), distal palm (84%), ring finger (72%), thumb (69%), thenar eminence (63%), little finger (39%), dorsal hand (31%), hypothenar eminence (25%) and forearm (13%) (Fig 1).
Figure 1.
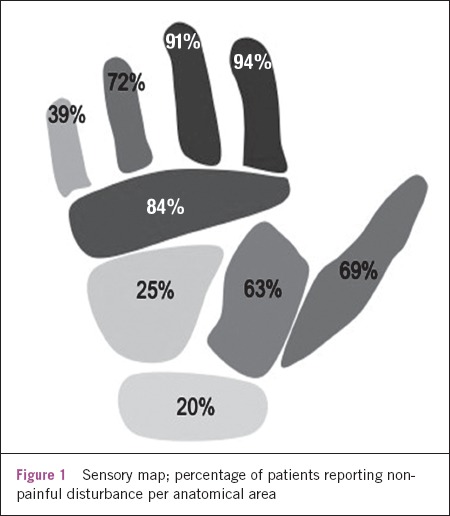
Sensory map; percentage of patients reporting nonpainful disturbance per anatomical area
Pain was less common than non-painful disturbance and reported in 59% of patients. Pain occurred in the wrist crease (33%), thenar eminence (27%), forearm (20%), middle finger (23%), index finger (22%), ring finger (19%), distal palm (16%), thumb (14%), dorsal hand (11%), little finger (11%) and hypothenar eminence (6%) (Fig 2).
Figure 2.
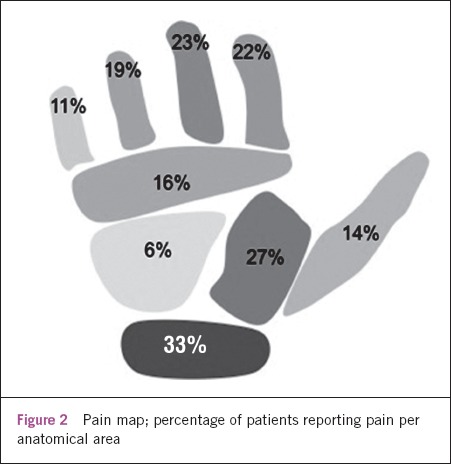
Pain map; percentage of patients reporting pain per anatomical area
The results of the SWM objective tests were considered in both low and high threshold modes. The cut off for the high threshold test was 4.31 whereas for the low threshold it was 3.61. Where the patient did not recognise a 3.61 monofilament and this was considered as normal (high threshold), the sensitivity of the test at the thenar eminence was 28%, 22% at the middle finger, 22% at the index finger, 20% at the thumb, 16% at the ring finger and 13% at the little finger. As expected, pressure aesthesiometry had a higher sensitivity when an unrecognised monofilament of 3.61 was considered as abnormal (low threshold). With a low threshold the sensitivity at the thenar eminence was 73%, 64% at the middle finger, 61% at the index finger, 59% at the thumb, 52% at the ring finger and 44% at the little finger.
The correlation between the subjective and objective tests was evaluated (Table 3). Where non-recognition of a monofilament of 3.61 was considered normal (high threshold), the sensitivity was poor (best sensitivity was 28% at thenar eminence) and when non-recognition was considered abnormal (low threshold), the specificity was poor (best specificity was 14% at index finger). The correlation between the subjective and objective tests was very poor and in many cases negative. The best correlation between the subjective diagram and SWM test was with a 3.61 cut-off as normal at the thenar eminence (kappa value 0.044).
Table 3.
Sensitivity of each test at anatomical sites
| Findings | Thumb | Index finger | Middle finger | Ring finger | Little finger | Thenar eminence | Wrist crease |
|---|---|---|---|---|---|---|---|
| Tingling, numbness, decreased sensation on hand diagram | 69% | 94% | 91% | 72% | 39% | 63% | 20% |
| Pain on hand diagram | 14% | 22% | 23% | 19% | 11% | 27% | 33% |
| Abnormal SWM test using high threshold (3.61 normal) | 20% | 22% | 22% | 16% | 13% | 28% | |
| Abnormal SWM test using low threshold (3.61 abnormal) | 59% | 61% | 64% | 52% | 44% | 73% | |
| Correlation of hand diagram and SWM test (with 3.61 as normal) | -0.05 | -0.04 | 0.013 | -0.06 | 0.07 | -0.13 | |
| Correlation of hand diagram and SWM test (with 3.61 as abnormal) | -0.01 | -0.04 | -0.09 | -0.05 | -0.12 | 0.04 |
Discussion
The symptoms reported by patients during history-taking are the cornerstone of a diagnosis of CTS but these vary considerably. Subjective measures such as the Katz hand diagram or objective ones such as pressure aesthesiometry are commonly undertaken. We found that the distribution of symptoms in CTS does not closely match the anatomy of the median nerve. In both the subjective and objective tests over 10% of patients were found to have symptoms in the little finger. These findings are not inconsistent with those of other investigators; Elfar et al demonstrated that the most symptomatic digit can, in some cases, be the ring or little fingers.12 A number of explanations have been proposed for this discrepancy, including patient error in describing symptoms, true functional overlay and the presence of a Martin–Gruber anastomosis. The Martin–Gruber anastomosis is a connection between the median nerve and ulnar nerve that may exist in over 20% of individuals.13 It is usually unilateral.
The subjective hand diagram relies on patients accurately remembering and interpreting their symptoms. The objective test removes this element of patient recollection. Another advantage of the objective test is that patients are only asked simple dichotomous questions whereas in the subjective test they are asked to remember all of the symptoms and record them on a diagram, which may be overwhelming and challenging for the patients. The objective test is not fully objective as it still relies on the patient's interpretation of the examination; the test is subject to the same functional overlay as in the subjective evaluation. The symptoms of CTS are typically more severe at night. It is uncommon for a clinician to evaluate a patient at the peak of their symptoms and for this reason recollected symptoms may offer a more accurate description of the disease than current ones even though they are viewed through the prism of patient memory.
We found that non-painful sensory disturbance is described more frequently in the area innervated by the median nerve but it also occurs commonly elsewhere. Sensory symptoms in CTS at the index finger occur in 94% of cases but the little finger is involved in 39% and the forearm in 13%. Although the sensory disturbance in CTS generally matches the anatomical distribution of the median nerve, variations occur with such frequency that a diagnosis of CTS should not be excluded if the area of sensory symptoms does not match the classical median nerve distribution.
Pain appeared most commonly at the site of compression (at the wrist crease) and appeared to follow the median nerve distribution into the fingers. Pain was even reported in the forearm or arm in more than 20% of patients.
Objective clinical measures require specialised equipment and are more time-consuming than subjective assessment. We found that objective measurement of abnormal sensation correlates poorly with both NCS and subjective measures. This is consistent with Pagel et al, who found that where a low threshold was used, the test had an unacceptably poor specificity and where the threshold was high, the sensitivity was poor.14 Although SWM testing is often used in the course of diagnosing hand dysaesthesia, there is little in the literature to support its reliability for this purpose. Some investigators have suggested using low threshold SWM testing in conjunction with a provocative test to overcome the problem of poor specificity.15
Conclusions
Subjective assessment with a hand diagram is reflective of patient history and forms a valuable record of the patient's experience. Although the symptoms on a hand diagram appear in the area innervated by the median nerve, they are never precise. Objective testing is neither a suitable single test nor an adequate surrogate for subjective testing and in the context of NCS it is redundant. In CTS sensory disturbance occurs most frequently in the median nerve distribution but an atypical distribution of symptoms should not discourage a diagnosis of CTS. The patient's description of his or her symptoms remains the most important tool in the diagnosis of CTS.
References
- 1.Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90:2,587–2,593. doi: 10.2106/JBJS.G.01362. [DOI] [PubMed] [Google Scholar]
- 2.Bachmann LM, Jüni P, Reichenbach S, et al. Consequences of different diagnostic ‘gold standards’ in test accuracy research: carpal tunnel syndrome as an example. Int J Epidemiol. 2005;34:953–955. doi: 10.1093/ije/dyi105. [DOI] [PubMed] [Google Scholar]
- 3.Katz JN, Stirrat CR. A self-administered hand diagram for the diagnosis of carpal tunnel syndrome. J Hand Surg Am. 1990;15:360–363. doi: 10.1016/0363-5023(90)90124-a. [DOI] [PubMed] [Google Scholar]
- 4.Patel MR, Bassini L. A comparison of five tests for determining hand sensibility. J Reconstr Microsurg. 1999;15:523–526. doi: 10.1055/s-2007-1000132. [DOI] [PubMed] [Google Scholar]
- 5.de Krom MC, Knipschild PG, Kester AD, Spaans F. Efficacy of provocative tests for diagnosis of carpal tunnel syndrome. Lancet. 1990;335:393–395. doi: 10.1016/0140-6736(90)90218-t. [DOI] [PubMed] [Google Scholar]
- 6.Brüske J, Bednarski M, Grzelec H, Zyluk A. The usefulness of the Phalen test and the Hoffman–Tinel sign in the diagnosis of carpal tunnel syndrome. Acta Orthop Belg. 2002;68:141–145. [PubMed] [Google Scholar]
- 7.Phalen GS. The carpal-tunnel syndrome. Seventeen years' experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48:211–228. [PubMed] [Google Scholar]
- 8.Amirfeyz R, Gozzard C, Leslie IJ. Hand elevation test for assessment of carpal tunnel syndrome. J Hand Surg Br. 2005;30:361–364. doi: 10.1016/j.jhsb.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 9.González del Pino J, Delgado-Martínez AD, González González I, Lovic A. Value of the carpal compression test in the diagnosis of carpal tunnel syndrome. J Hand Surg Br. 1997;22:38–41. doi: 10.1016/s0266-7681(97)80012-5. [DOI] [PubMed] [Google Scholar]
- 10.Tekeoglu I, Dogan A, Demir G, Dolar E. The pneumatic compression test and modified pneumatic compression test in the diagnosis of carpal tunnel syndrome. J Hand Surg Eur Vol. 2007;32:697–699. doi: 10.1016/J.JHSE.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Gillenson SP, Parets N, Bear-Lehman J, Stanton DB. The effect of wrist position on testing light touch sensation using the Semmes–Weinstein pressure aesthesiometer: a preliminary study. J Hand Ther. 1998;11:27–31. doi: 10.1016/s0894-1130(98)80057-4. [DOI] [PubMed] [Google Scholar]
- 12.Elfar JC, Yaseen Z, Stern PJ, Kiefhaber TR. Individual finger sensibility in carpal tunnel syndrome. J Hand Surg Am. 2010;35:1,807–1,812. doi: 10.1016/j.jhsa.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodriguez-Niedenführ M, Vazquez T, Parkin I, et al. Martin–Gruber anastomosis revisited. Clin Anat. 2002;15:129–134. doi: 10.1002/ca.1107. [DOI] [PubMed] [Google Scholar]
- 14.Pagel KJ, Kaul MP, Dryden JD. Lack of utility of Semmes–Weinstein monofilament testing in suspected carpal tunnel syndrome. Am J Phys Med Rehabil. 2002;81:597–600. doi: 10.1097/00002060-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Gellman H, Gelberman RH, Tan AM, Botte MJ. Carpal tunnel syndrome. An evaluation of the provocative diagnostic tests. J Bone Joint Surg Am. 1986;68:735–737. [PubMed] [Google Scholar]


