Abstract
Neonatal lupus is a rare syndrome resulting from passively transferred maternal autoantibodies during pregnancy. A male infant was delivered at term to a 29-year-old primiparous woman who was diagnosed of systemic lupus erythematosus 2 years earlier and had detectable levels of autoantibodies (antinuclear antibody (ANA), anti-dsDNA, anti-Ro and anti-La/SSB) in second trimester. However, the pregnancy was otherwise uneventful. He presented at the age of 8 week with a widespread hypopigmented macular rash on the trunk and patchy alopecia involving the hair line and the occipito-parietal regions of 3 weeks duration, anaemia and symptomatic thrombocytopaenia. Serologic test for autoantibodies was positive for ANA and anti-La/SSB. Further evaluation was normal. He was managed conservatively with blood products and topical corticosteroids. Mother was also advised to avoid direct exposure to sunlight and fluorescent light. Haematological parameters gradually normalised over 2 months and the skin lesions resolved completely by the age of 6 months.
Background
We describe this case of neonatal lupus syndrome in a Nigerian child to highlight its occurrence in African settings, although previously unreported. Also, this report showed that neonatal lupus may present with potentially life-threatening haematological disorders but they are amenable to prompt treatment.
Case presentation
A male infant was delivered at 38th week gestational age with a birth weight of 3.2 kilogram via spontaneous vertex delivery to a 29-year-old primiparous woman. This mother was diagnosed of systemic lupus erythematosus (SLE) 2 years earlier and had detectable levels of autoantibodies (antinuclear antibody (ANA), anti-dsDNA, anti-Ro and anti-La/SSB) at 14th week of conception of this baby. Her serological tests for hepatitis B, HIV and syphillis were negative. Serial fetal monitoring was normal. The infant was admitted into our paediatric ward at the age of 8 weeks with rash and patchy hair loss of 3 weeks duration, pallor of 1 week duration, cutaneous bleeds and haematuria 2 days before presentation. The rash did not respond to topical antifungals. He had received prophylactic intramuscular vitamin K 1 mg at birth and mother was not on warfarin or anticonvulsant medications.
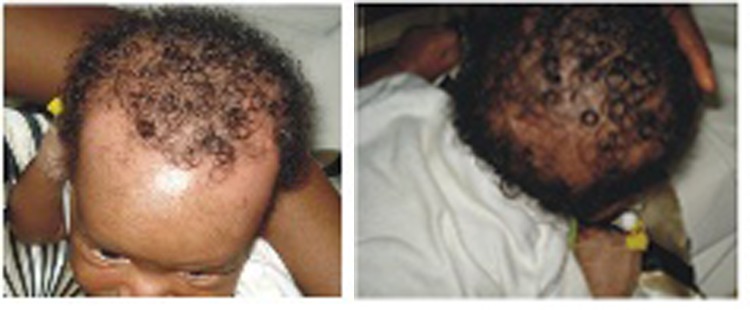
On physical examination, the boy was very pale but afebrile. His respiratory rate was 52 cycles per min, pulse rate was 126 beats per min, regular and heart sounds were normal. His weight was 4.5 kilograms. There were purpuric and petechial haemorrhages on the face (figure 1), as well as hypopigmented macular lesions on the trunk (figure 2). There was patchy alopecia involving several regions of the scalp (figure 3A,B). There were no subcutaneous nodules or hepatosplenomegaly. Other systemic examinations were normal.
Figure 1.

Cutaneuos bleeds in neonatal lupus syndrome with thrombocytopaenia and anaemia.
Figure 2.

Cutaneous lupus manifesting as dyspigmented lesions in an 8-week-old African infant. Lesions gradually disappeared by the age of 6 months without sequelae, coinciding with the absence of anti-La/SSB antibodies in the infant.
Figure 3.
(A) Patchy hair loss along the hair-line in neonatal lupus syndrome. (B) Patchy alopecia in the parieto-occipital region in neonatal lupus syndrome.
Investigations
Laboratory investigations showed haematuria, haemoglobin concentration of 3.1 g/dl, haematocrit was 15%, total white blood cell count was 9000 cells/µL with lymphocyte predominance, white cell morphology was normal, there were no blast cells; platelet count was 40 000 cells/µL; reticulocyte count was 3%, red blood cells were normocytic-normochromic. Liver and renal function tests were normal. Haemoculture for bacteria yielded no growth. Serology was positive for ANA and anti-La/SSB antibodies. ECG and Doppler echocardiography findings were normal.
Differential diagnosis
-
▶
Transient leukaemia (myeloproliferative syndrome)
-
▶
Infant leukaemia.
Treatment
He was transfused with freshly donated blood and platelet concentrates. He was also treated with topical corticosteroids. Mother was advised to avoid direct exposure of the baby to sunlight and fluorescent light.
Outcome and follow-up
Haematological parameters gradually returned to normal after 8 weeks and skin lesions resolved completely by the age of 6 months when the passively transferred autoantibodies were no longer detectable.
Discussion
Neonatal lupus is a rare syndrome resulting from passively transferred maternal IgG autoantibodies, usually anti-Ro/SSA or anti-La/SSB, occurring between the 12th and 16th week of gestation. U1RNP autoantibodies may however be responsible in few cases.1 2 SLE has rarely been reported among black Africans but Adelowo et al3 described 66 adult cases in Nigeria. Only about 2 per cent of babies born to mothers with autoantibodies develop neonatal lupus.2 The maternal antibodies bind to fetal cardiac tissue and skin causing autoimmune damage and clinical features that may partly depend on fetal genetic subsceptibility.4 5 The most severe outcome in the affected newborn is complete heart block which is often associated with anti-Ro/SSA antibodies.4 In a review of 54 cases of neonatal lupus in Chinese literature, Sun et al6 found that anti-Ro/SSA, anti-La/SSB or both were present in over 90 per cent of infant-mother pairs despite some mothers being asymptomatic initially. We confirmed the diagnosis of neonatal lupus syndrome in our patient through the detection anti-La/SSB autoantibodies in both the infant and his mother, which is a major diagnostic criterion of the American Research Registry for Neonatal Lupus.7
This patient presented with widespread hypopigmented macules on the trunk. Cutaneous lupus typically presents as erythematous macules, annular plaques or polycyclic rash with mild central atrophy and raised borders, with a predilection for the face, scalp and trunk.6 7 They usually regress over a few months coinciding with the catabolism of the transferred antibodies in the infant.6 7 Although there is no scarring, various changes including dyspigmentation can occur in cutaneous lupus. In a review of 57 cases of cutaneous neonatal lupus without heart block, Neiman et al7 found that 25 per cent of cases of cutaneous neonatal lupus had sequelae including dyspigmentation and telangiectasia. Also, in a case series of neonatal lupus, Weston et al8 reported three babies who had dyspigmentation that spontaneously cleared within 22 months, without scarring or atrophy. Dyspigmentation occurred early in our patient and healed completely in mid-infancy, but more case studies are needed to show the trend of manifestations of neonatal lupus in our region. Histologic findings in cutaneous neonatal lupus include basal cell vasculopathy and dermal mononuclear infilterates.9 10 Skin biopsy however, was not done in our patient.
Haematologic derangement is an important manifestation of neonatal lupus as evidenced in our patient who had both anaemia and thrombocytopenia. In the Chinese series, Sun et al6 described haematologic manifestations in nearly half of the cases including anaemia in about 25 per cent of cases and both anaemia and thrombocytopaenia in over 11 per cent.6 These manifestations are usually mild and self-limiting but rarely they can be life-threatening. Hence, symptomatic systemic disorders should be treated promptly in neonatal lupus. Selander et al11 had described a neonate with neonatal lupus syndrome who had severe liver and haematological disease, and died in early neonatal period without cardiac or cutaneous involvement. Similarly, Wolach et al12 reported a case of aplastic anaemia in neonatal lupus that manifested severe anaemia and evidence of immune suppression of haematopoiesis. The infant died of Gram-negative sepsis and coagulopathy, despite packed red blood transfusions and steroid therapy.12 In contrast, our patient had severe anaemia and thrombocytopAenia requiring transfusion initially but he gradually recovered over a few weeks. Haematuria could have been due to thrombocytopAenia in our patient, as further renal evaluations were normal. Other rarely reported features in neonatal lupus include proteinuria and elevated serum creatinine.13 14
Although anaemia and thrombocytopaenia occur in infant leukemia and transient leukemia (myeloproliferative syndrome), these haematologic diseases are also characterised by high leucocyte counts, blast cells in the peripheral blood film and hepatosplenomegaly which were absent in this case.15 Furthermore, subcutaneous nodules, known as leukemia cutis, are found in infant leukemia.15
Learning points.
-
▶
This case highlights the occurrence of this rare disorder in an African child.
-
▶
Also, this report showed that it may present with potentially life-threatening haematological disorders.
-
▶
Prompt conservative management ensures a good outcome.
Acknowledgments
The authors acknowledge Dr Okiroro Igosewe, consultant paediatrician, Delta State University Teaching Hospital, Ughara, Delta State, Nigeria.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Tseng CE, Buyon JP. Neonatal lupus syndromes. Rheum Dis Clin North Am 1997;23:31–54 [DOI] [PubMed] [Google Scholar]
- 2.Lee LA, Frank MB, McCubbin VR, et al. Autoantibodies of neonatal lupus erythematosus. J Invest Dermatol 1994;102:963–6 [DOI] [PubMed] [Google Scholar]
- 3.Adelowo OO, Oguntona SA. Pattern of systemic lupus erythematosus among Nigerians. Clin Rheumatol 2009;28:699–703 [DOI] [PubMed] [Google Scholar]
- 4.Ho SY, Esscher E, Anderson RH, et al. Anatomy of congenital complete heart block and relation to maternal anti-Ro antibodies. Am J Cardiol 1986;58:291–4 [DOI] [PubMed] [Google Scholar]
- 5.Clancy RM, Backer CB, Yin X, et al. Genetic association of cutaneous neonatal lupus with HLA class II and tumor necrosis factor alpha: implications for pathogenesis. Arthritis Rheum 2004;50:2598–603 [DOI] [PubMed] [Google Scholar]
- 6.Sun W, Yuan T, Chen L, et al. Neonatal lupus erythematosus: three case reports and review of the Chinese literature. Clin Pediatr 2010;49:627–34 [DOI] [PubMed] [Google Scholar]
- 7.Neiman AR, Lee LA, Weston WL, et al. Cutaneous manifestations of neonatal lupus without heart block: characteristics of mothers and children enrolled in a national registry. J Pediatr 2000;137:674–80 [DOI] [PubMed] [Google Scholar]
- 8.Weston WL, Morelli JG, Lee LA. The clinical spectrum of anti-Ro-positive cutaneous neonatal lupus erythematosus. J Am Acad Dermatol 1999;40:675–81 [DOI] [PubMed] [Google Scholar]
- 9.David-Bajar KM, Davis BM. Pathology, immunopathology, and immunohistochemistry in cutaneous lupus erythematosus. Lupus 1997;6:145–57 [DOI] [PubMed] [Google Scholar]
- 10.Baltaci M, Fritsch P. Histologic features of cutaneous lupus erythematosus. Autoimmun Rev 2009;8:467–73 [DOI] [PubMed] [Google Scholar]
- 11.Selander B, Cedergren S, Domanski H. A case of severe neonatal lupus erythematosus without cardiac or cutaneous involvement. Acta Paediatr 1998;87:105–7 [DOI] [PubMed] [Google Scholar]
- 12.Wolach B, Choc L, Pomeranz A, et al. Aplastic anemia in neonatal lupus erythematosus. Am J Dis Child 1993;147:941–4 [DOI] [PubMed] [Google Scholar]
- 13.Feng SF, Zheng CZ, Li M, et al. Six cases of neonatal lupus erythematosus. Chin J Dermatol 1993;26:279–81 [Google Scholar]
- 14.Chen JQ, Jiang HJ, Tan ZT, et al. Immune response in neonatal lupus erythematosus. J Appl Clin Pediatr 1997;12:14–6 [Google Scholar]
- 15.Tubergen DG, Bleyer A. The Leukemias. In: Kliegman RM, Behrman RE, Jenson HB, eds. Nelson Textbook of Pediatrics. 18th Edition. Philadelphia, PA: Saunders Elsevier; 2007:495 [Google Scholar]