Abstract
In this case report, the authors are presenting a case of a 35-year-old lady who presented to our clinic with recurrent episodes of massive epistaxis and loss of right eye vision for last 6 months following road traffic accident. There was no other significant medical and surgical history. Bleeding episodes were sometimes very severe with loss up to 400–500 cc and would stop spontaneously. She was given multiple blood transfusions after these episodes. A complete otorhinolaryngological examination including rigid endoscopy and coagulation investigation did not reveal any abnormality. CT with contrast of paranasal region showed blood within the right sphenoid sinus with linear fracture of the lateral wall with post-traumatic cavernous pseudoaneurysm of internal carotid artery localised to right sphenoid sinus. That was managed successfully by embolisation using a detachable balloon and a coil. She was followed up in the clinic at 6 weeks and 6 months interval with no symptoms.
Background
Epistaxis is one of the commonest emergencies in otolaryngology. It is estimated that 7–60% of population experience epistaxis of varying severity at some point in their lives.1 There are different causes of epistaxis that includes dryness of the nasal cavity, digital trauma, anticoagulation, hypertension and blood dyscrasias, which are most of the time managed conservatively or may be with nasal packing. Aneurysm of internal carotid artery (ICA) on the other hand can be a source of massive epistaxis and requires a different management as compared with other causes. Although, pseudoaneurysm of ICA is a rare entity. It must be considered among differential diagnosis of intractable epistaxis, especially if there is prior history of trauma. Because of high death rate early diagnosis and treatment is required.
Case presentation
A 35-year-old woman presented to our clinic with recurrent episodes of massive epistaxis and loss of right eye vision for the last 6 months following road traffic accident. There was no other significant medical and surgical history.
Bleeding episodes were sometimes very severe with loss up to 400–500 cc and would stop spontaneously. She was given multiple blood transfusions after these episodes. A complete otorhinolaryngological examination including rigid endoscopy did not reveal any abnormality. She was admitted and relevant laboratory investigations including coagulation profile ordered. The haematocrit and haemoglobin levels were 24.1% and 7.9 g/dl, respectively, and the rest of the haematologic and chemical laboratory values were within the normal range. On the day of admission, she had a massive episode of epistaxis that stopped spontaneously after about 400 ml of blood loss. Repeat haematocrit and haemoglobin levels were 23.1% and 7.1g/dl. The patient was immediately shifted to special care unit and monitored continuously for blood pressure, pulse oximetry and ECG. Two intravenous lines were obtained; fluid resuscitation started and was transfused with two units of pack cells.
Investigations
Hb:7.4, Hct:24.1%
CT scan paranasal sinuses with intravenous contrast
A defect of right lateral wall of the sphenoid sinus was noted which may represent fracture due to past history of RTA. There was evidence of an outpouching protruding into right sphenoid sinus arising from medial aspect of intracavernous portion of the right internal carotid artery measuring approximately 4×4 mm (figure 1A,B), which most likely represented an aneurysm of the right internal carotid artery.
Figure 1.
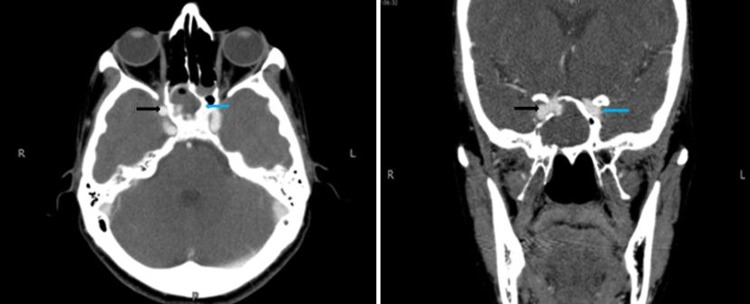
(A) CT, axial view shows blood and contrast within the right sphenoid sinus (blue arrows) with linear fracture of the lateral wall of the right sphenoid sinus (black arrows), R: right, L: left. (B) CT, coronal view view shows blood and contrast within the right sphenoid sinus (blue arrows) with linear fracture of the lateral wall of the right sphenoid sinus (black arrows), R: right, L: left.
Treatment
Angiogram was obtained after right transfemoral catheterisation, which demonstrated a unilateral intracavernous posterior inferior cerebellar artery (PICA) on the right side (figure 2a). Before embolising PICA, cross flow of blood was confirmed from contralateral internal carotid artery, which was present. The pseudoaneurysm was treated with a detachable balloon and coil and postprocedure control angiogram showed occlusion of the pseudoaneurysm (figure 2b). The patient remained stable and was discharged 2 days after the procedure.
Figure 2.
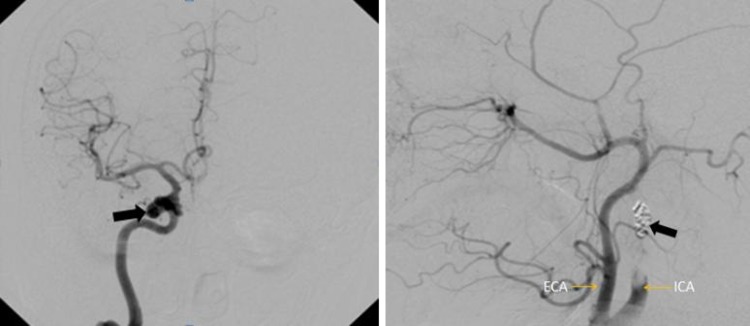
Cerebral angiography shows unilateral intracavernous carotid artery pseudoaneurysm at right side (black arrow) (A) and there was no residual filling after the ballon and coil treatment (black arrow) (B). ECA, external carotid arery, ICA, internal carotid artery.
Outcome and follow-up
Postprocedure the patient remained stable and was discharged 2 days after the procedure.
She followed up in the clinic at 6 weeks and 6 months interval with no symptoms.
Discussion
Aneurysms of cavernous part of ICA are rare and comprise of only 3–5% of all intracranial aneurysms.2 Majority of cases occur secondary to trauma. The hallmark of post-traumatic pseudoaneurysm is delayed, progressively more severe and sometimes fatal epistaxis and mortality reported in these cases is 30–50%.3 4 There are various mechanisms which can result in pseudoaneurysm after trauma. An intimal tear resulting from trauma can be augmented with dissection of blood that can result in decrease blood flow and hence, intraluminal thrombus formation.5 Theoretically, patients with pseudoaneurysms of the cranial ICA are at risk for distal thromboembolism, continued enlargement leading to occlusion of vessel and intracranial bleeding.6
Although PICAs may be asymptomatic but at times they may present with massive epistaxis as cavernous part of aneurysm bleed in to sphenoid sinus that then present as nasal bleeding.7 The cavernous PICAs are in close anatomic proximity to cavernous structures thus may be associated with their injury. Immediate complete or partial ipsilateral monocular visual loss caused by either compression or laceration of the optic nerve, or thrombosis of the ophthalmic artery is common. The occulomotor nerve and the ophthalmic and maxillary divisions of the trigeminal nerve are less frequently involved. The combination of head injury, monocular blindness and epistaxis constitutes Maurer’s triad.8
The gold standard for diagnosis of PICAs is angiography. An alternative to this is a less invasive procedure that is, three-dimensional CT angiography.9 CT and MRI may provide information to suggest the possibility of aneurysm.
Treatment may be surgical or medical. Surgical options include direct clipping, wrapping, trapping and carotid artery ligation.10 However, endovascular techniques have shown promising results.11 12 Among these techniques detachable balloons and coils have been successfully used in the treatment of these aneurysms. In addition, a test occlusion of the ICA can be performed with a non-detachable balloon to determine the adequacy of collateral blood flow to the brain. Detachable balloons also allow for not merely the proximal occlusion of the ICA, but also occlusion of the segment of the ICA distal to the aneurysm. In this manner, collateral blood flow to the aneurysm can be prevented and the likelihood of a rebleed as well as delayed embolic strokes reduced.
Although, PICA is a rare entity. It must be considered among differential diagnosis of intractable epistaxis, especially if there is prior history of trauma. Because of high death rate early diagnosis and treatment is required.
Learning points.
Pseudoaneurysm of ICA should be a differential in cases of intractable epistaxis.
Early identification on the basis of history, examination and radiology is crucial.
Early referral to tertiary care hospital is mandatory to save life of the patient since treatment of this cause of epistaxis is different.
Early angiography and embolisation with coiling can be lifesaving.
Acknowledgments
Dr Mohammad Ali, Fellow interventional Radiology, Aga Khan University for helping in reading angiographic and CT scan films.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Moñux A, Tomás M, Kaiser C, et al. Conservative management of epistaxis. J Laryngol Otol 1990;104:868–70. [DOI] [PubMed] [Google Scholar]
- 2.Li MH, Li YD, Gao BL, et al. A new covered stent designed for intracranial vasculature: application in the management of pseudoaneurysms of the cranial internal carotid artery. AJNR Am J Neuroradiol 2007;28:1579–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goleas J, Mikhael MA, Paige ML, et al. Intracavernous carotid artery aneurysm presenting as recurrent epistaxis. Ann Otol Rhinol Laryngol 1991;100:577–9. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky A, Luntz M, Veller B, et al. Intrasphenoid mycotic aneurysm of the internal carotid artery. Otolaryngol Head Neck Surg 2003;128:887–90. [DOI] [PubMed] [Google Scholar]
- 5.Radkowski D, McGill TJ, Healy GB, et al. Penetrating trauma of the oropharynx in children. Laryngoscope 1993;103:991–4. [DOI] [PubMed] [Google Scholar]
- 6.Maras D, Lioupis C, Magoufis G, et al. Covered stent-graft treatment of traumatic internal carotid artery pseudoaneurysms: a review. Cardiovasc Intervent Radiol 2006;29:958–68. [DOI] [PubMed] [Google Scholar]
- 7.Bhatoe HS, Suryanarayana KV, Gill HS. Recurrent massive epistaxis due to traumatic intracavernous internal carotid artery aneurysm. J Laryngol Otol 1995;109:650–2. [DOI] [PubMed] [Google Scholar]
- 8.Maurer JJ, Mills M, German WJ. Triad of unilateral blindness, orbital fractures and massive epistaxis after head injury. J Neurosurg 1961;18:837–40. [DOI] [PubMed] [Google Scholar]
- 9.Chen D, Concus AP, Halbach VV, et al. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope 1998;108:326–31. [DOI] [PubMed] [Google Scholar]
- 10.Kadyrov NA, Friedman JA, Nichols DA, et al. Endovascular treatment of an internal carotid artery pseudoaneurysm following transsphenoidal surgery. Case report. J Neurosurg 2002;96:624–7. [DOI] [PubMed] [Google Scholar]
- 11.Bell RS, Vo AH, Roberts R, et al. Wartime traumatic aneurysms: acute presentation, diagnosis, and multimodal treatment of 64 craniocervical arterial injuries. Neurosurgery 2010;66:66–79; discussion 79. [DOI] [PubMed] [Google Scholar]
- 12.Luo CB, Teng MM, Chang FC, et al. Endovascular management of the traumatic cerebral aneurysms associated with traumatic carotid cavernous fistulas. AJNR Am J Neuroradiol 2004;25:501–5. [PMC free article] [PubMed] [Google Scholar]


