Abstract
We hypothesised that the relative importance of physical and psychological risk factors for mechanical low back pain (LBP) might differ importantly according to whether there is underlying spinal pathology, psychological risk factors being more common in patients without demonstrable pathology. If so, epidemiological studies of LBP could benefit from tighter case definitions. To test the hypothesis, we used data from an earlier case-control study on patients with mechanical LBP who had undergone magnetic resonance imaging (MRI) of the lumbosacral spine. MRI scans were classified for the presence of high-intensity zone (HIZ), disc degeneration, disc herniation, and nerve root displacement/compression. Information about symptoms and risk factors was elicited by postal questionnaire. Logistic regression was used to assess associations of MRI abnormalities with symptoms and risk factors, which were characterised by odds ratios (ORs) and 95% confidence intervals (CIs). Among 354 patients (52% response), 306 (86.4%) had at least 1, and 63 (17.8%) had all 4 of all MRI abnormalities. Radiation of pain below the knee (280 patients) and weakness or numbness below the knee (257 patients) were both associated with nerve root deviation/compression (OR 2.5, 95% CI 1.4 to 4.5; and OR 1.8, 95% CI 1.1 to 3.1, respectively). However, we found no evidence for the hypothesised differences in risk factors between patients with and without demonstrable spinal pathology. This suggests that when researching the causes and primary prevention of mechanical LBP, there may be little value in distinguishing between cases according to the presence or absence of the more common forms of potentially underlying spinal pathology.
Keywords: Low back pain, MRI, high intensity zone, disc degeneration, disc prolapse, nerve root compression, symptoms, risk factors
Introduction
The occurrence of low back pain (LBP) has been linked with various abnormalities of the spine on magnetic resonance imaging (MRI), evidence being strongest for disc herniation (protrusion or worse), nerve root deviation/compression, disc degeneration and high intensity zone (HIZ) [7]. However, each of these abnormalities can be found in the absence of symptoms, and many patients with back complaints do not exhibit any demonstrable pathology on MRI.
Most epidemiological studies of LBP have therefore defined cases on the basis of symptoms and/or associated disability (e.g. incapacity for work), rather than by pathology. With this approach, research has pointed fairly consistently to a causal role of physical risks factors such as heavy lifting and frequent bending or twisting of the spine [19]. In addition, psychological mechanisms can play an important part in the development and persistence of LBP. Associations have been found with psychological characteristics such as low mood [18; 26] and tendency to be distressed by common somatic symptoms (somatising tendency) [26; 23]. Moreover, pessimistic health beliefs have been shown to predict poor outcomes in patients with established LBP [29; 9].
We hypothesised that the relative importance of physical and psychological risk factors for mechanical LBP (whether incident or recurrent) might differ according to whether there is demonstrable underlying pathology in the spine, psychological factors having relatively greater impact when pain occurs in the absence of detectable spinal abnormalities. This would accord with the observation that low mood and somatising tendency have been linked also with an increased risk of arm pain [23], which like LBP occurs frequently in the absence of identifiable local pathology, whereas no association was found in a study of hip osteoarthritis in which pathology was confirmed radiologically [5]. If there were substantial differences in risk factors for LBP according to the presence or absence of spinal pathology, that would have implications for the design of future epidemiological research.
To test our hypothesis, we analysed data on patients with LBP investigated by MRI from a previously reported case-control study [24]. In particular, we explored whether the clinical presentation of cases, and the prevalence of their exposure to physical and psychological risk factors, differed according to whether specified abnormalities of the lumbo-sacral spine were present on MRI (we did not use any data from the control group).
Methods
During 2003-06, we prospectively identified a consecutive series of patients aged 20-64 years with LBP, who were resident in the catchment area covered by the radiology services of Southampton General Hospital (the main public hospital in the city of Southampton), and who were referred to that hospital, or to either of two local private hospitals, for MRI of the lumbar spine. Patients whose symptoms arose from external trauma or non-mechanical pathology (e.g. cancer, metabolic bone disease, infection, congenital disorders) were excluded, as were those with previous back surgery.
Potentially eligible patients were sent a postal questionnaire, followed if necessary by a reminder after four weeks. Among other things, this covered: history of LBP and associated symptoms; details of their current or most recent job (including whether they had been in the job when their most recent episode of LBP began, and whether an average working day in the job involved lifting loads heavier than 10 kg (20 lbs) more than 10 times, or working with their back bent or twisted for longer than an hour); pain at four other anatomical sites (neck, shoulder, elbow and wrist/hand) lasting longer than a day at some time during the past four weeks; somatising tendency; low mood; fear-avoidance beliefs; and propensity to consult about LBP if it occurred. The most recent episode of LBP was defined as having started when pain developed after the subject had last been free from the symptom for a month or longer. Somatising tendency was assessed using elements from the Brief Symptom Inventory (BSI) [6], and patients were scored according to how many of five common somatic symptoms (faintness/dizziness, pain in the heart/chest, nausea/upset stomach, trouble getting breath, and hot/cold spells) had been at least moderately distressing in the past week. Low mood (in the past four weeks) was assessed using the mental health section of the SF-36 questionnaire [30], and was graded in approximate thirds of the overall distribution of scores in the study sample. Fear-avoidance beliefs were ascertained through elements of the Fear-Avoidance Beliefs scale of Waddell and colleagues [29], and were classified according to the number of statements (out of a possible total of four) with which the patient agreed. Propensity to consult because of LBP was scored according to answers to two questions – one on whether it was important to see a doctor straight away at the first sign of back trouble, and the other on whether neglecting back complaints could cause permanent health problems.
MRI examinations were carried out according to the protocol prescribed by the radiologist who accepted the initial referral, and were considered suitable for assessment as part of our study if they included sagittal T1 and T2 weighted images of the lumbosacral spine and also axial T2 weighted images through the L3/L4, L4/L5 and L5/S1 discs. Each scan was assessed according to a standardised protocol by one of two trainee radiologists (JS, PM), who were blinded to clinical histories and questionnaire responses. Each series of images was graded for the presence or absence of HIZ, disc degeneration, disc herniation and nerve root displacement/compression, at each of three spinal levels (L3/L4, L4/L5 and L5/S1). HIZ was defined as a high intensity signal located in the substance of the posterior annulus fibrosus, and clearly dissociated from the signal of the nucleus pulposus in that it was surrounded superiorly, inferiorly, posteriorly and anteriorly by the low intensity signal of the annulus fibrosus and was appreciably brighter than that of the nucleus pulposus [1]. Disc degeneration was graded by comparison of the intensity of the disc signal with reference images in an atlas, according to a scheme published by Jaroscz et al [10]. Disc herniation was defined as protrusion, herniation or sequestration of the disc (i.e. focal disc extension beyond the interspace into the vertebral canal) [20; 3]. Nerve root deviation was diagnosed if a nerve root was displaced dorsally by disc material, and compression if a nerve root was compressed between disc material and the wall of the spinal canal or exit foramen [31; 25]. Patients were classified as positive for an MRI abnormality if they exhibited it at any of the three spinal levels.
To check the repeatability of the MRI classification, a sub-sample of 93 scans was assessed independently by both of the radiologists, and each radiologist re-read 40 of these scans a second time after an interval of at least six months. The selection of scans for this exercise was carried out by a third person (ECH), who had not seen the scans and was unaware of what they showed. Within-observer agreement in the classification of patients was moderate to good with kappa statistics [4] by observer and abnormality ranging from 0.40 to 0.71. Agreement between observers (assessed from their first reading of each scan) was generally reasonable (kappa statistics of 0.50 to 0.67). For disc herniation, the agreement between observers was weaker (kappa = 0.18), largely because one radiologist graded a substantial proportion of patients (42%) as having protrusion where the other classed the patient as having only bulge.
For those scans that were read twice by the same radiologist, classification for the purpose of the current study was based on the first reading. In the subset of scans that were read by both radiologists, discrepancies in the assessment of nerve root deviation/compression were resolved by consensus between the two readers, with input if necessary from a third senior radiologist (MS) experienced in spinal MRI. Other MRI abnormalities, including disc herniation, were deemed to be present if they were diagnosed by either of JS or PM.
Statistical analysis was carried out using Stata Version 11 software [28]. Pairwise associations between MRI abnormalities were characterised by odds ratios (ORs), adjusted for sex and age, with associated 95% confidence intervals (CIs). Associations of MRI abnormalities with symptoms, and with physical and psychological risk factors, were assessed by logistic regression, with the abnormality (present or absent) as the outcome variable and adjustment for sex and age. As well as examining the associations of symptoms and risk factors with individual MRI abnormalities, we also explored their relation to the total number of MRI abnormalities that patients displayed. In this analysis, separate regression models were used to explore risk factors for each of one, two, three and four relative to zero abnormalities. Analysis of associations with occupational physical activities was restricted to the subset of patients whose most recent job was that which they had held when their current episode of LBP began.
Ethical approval for the study was provided by the Southampton and South West Hampshire NHS Research Ethics Committee.
Results
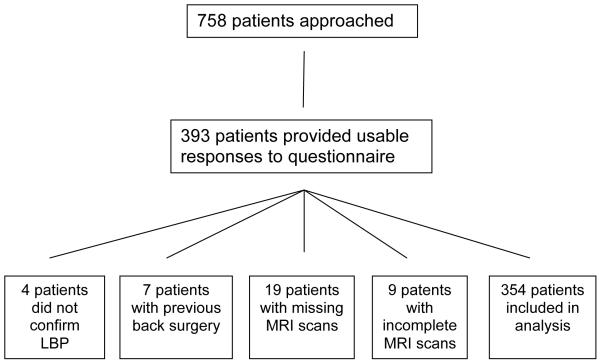
A total of 758 patients were invited to take part in the study, of whom, 393 (52%) provided usable responses to the questionnaire. Of these, four were excluded because they did not confirm LBP in their answers to the questionnaire, seven because they reported previous surgery to the back, 19 because their MRI scans could not be located for assessment, and nine because MRI scans were incomplete.
Table 1 summarises the demographic characteristics and MRI findings of the remaining 354 patients on whom further analysis was based. They included 169 men and 185 women, with ages at the time of MRI examination ranging from 21 to 64 years. The most common of the four MRI abnormalities assessed was disc herniation (66.4% of patients) followed by HIZ (63.0%). Sixty-three patients (17.8%) exhibited all four of the abnormalities, and 48 (13.6%) had none of them.
Table 1.
Characteristics of cases
| Characteristic | Men | Women | Both Sexes |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Age (years) | ||||||
| 20-29 | 11 | 6.5 | 17 | 9.2 | 28 | 7.9 |
| 30-39 | 52 | 30.8 | 48 | 25.9 | 100 | 28.2 |
| 40-49 | 53 | 31.4 | 52 | 28.1 | 105 | 29.7 |
| 50-59 | 38 | 22.5 | 53 | 28.6 | 91 | 25.7 |
| 60-69 | 15 | 8.9 | 15 | 8.1 | 30 | 8.5 |
| MRI abnormalities | ||||||
| HIZ | 106 | 62.7 | 117 | 63.2 | 223 | 63.0 |
| Disc degeneration | 75 | 44.4 | 86 | 46.5 | 161 | 45.5 |
| Disc herniation | 124 | 73.4 | 111 | 60.0 | 235 | 66.4 |
| Nerve root deviation/compression | 85 | 50.3 | 77 | 41.6 | 162 | 45.8 |
| Number of MRI abnormalities | ||||||
| 0 | 22 | 13.0 | 26 | 14.1 | 48 | 13.6 |
| 1 | 18 | 10.7 | 34 | 18.4 | 52 | 14.7 |
| 2 | 46 | 27.2 | 50 | 27.0 | 96 | 27.1 |
| 3 | 52 | 30.8 | 43 | 23.2 | 95 | 26.8 |
| 4 | 31 | 18.3 | 32 | 17.3 | 63 | 17.8 |
Table 2 shows the pairwise associations between the four MRI abnormalities. By far the strongest association was between disc herniation and nerve root deviation/compression (OR 10.6, 95%CI 5.8-19.3). Odds ratios for the other associations, all of which were statistically significant, ranged from 1.9 to 2.9.
Table 2. Pairwise associations between MRI abnormalities.
Associations are summarised by odds ratios, adjusted for sex and age (five bands), with 95% CIs in round brackets. Figures in square brackets indicate the numbers of subjects with both of the MRI abnormalities.
| HIZ | Disc degeneration |
Disc herniation |
|
|---|---|---|---|
| Disc degeneration | 2.9 (1.8,4.6) [122] |
||
| Disc herniation | 3.0 (1.8,4.7) [167] |
2.3 (1.4,3.7) [120] |
|
| Nerve root deviation/compression | 1.9 (1.2,3.0) [115] |
2.1 (1.4,3.3) [89] |
10.6 (5.8,19.3) [146] |
The relationship between LBP characteristics and MRI findings is shown in Table 3. Sudden onset of the current episode of pain, reported by 139 patients (39%), was unrelated to any of the abnormalities examined. In contrast, radiation of pain below the knee in the past 12 months (280 patients, 79%) and the presence of weakness or numbness below the knee in the past 12 months (257 patients, 73%) were both significantly associated with nerve root deviation/compression (ORs 2.5 and 1.8 respectively), and to a lesser extent with disc herniation and disc degeneration. Moreover, the prevalence of these symptoms increased with the number of MRI abnormalities present, such that in patients with all four abnormalities, the OR for radiation of pain to below the knee (relative to those with no abnormalities) was 3.9 (95% CI 1.3-11.6).
Table 3.
Associations of MRI abnormalities with characteristics of low back pain
| MRI abnormality |
Sudden onset of current LBP episode |
Radiation below kneea | Associated with weakness or numbness below kneea |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | ORb | (95% CI) | n | ORb | (95% CI) | n | ORb | (95% CI) | |
| HIZ | |||||||||
| Absent | 52 | 1 | - | 98 | 1 | - | 91 | 1 | - |
| Present | 87 | 0.9 | (0.6,1.5) | 182 | 1.3 | (0.8,2.4) | 166 | 1.2 | (0.7,2.0) |
|
Disc
degeneration |
|||||||||
| Absent | 73 | 1 | - | 147 | 1 | - | 134 | 1 | - |
| Present | 66 | 1.2 | (0.8,1.9) | 133 | 1.6 | (0.9,2.8) | 123 | 1.6 | (1.0,2.7) |
|
Disc
herniation |
|||||||||
| Absent | 47 | 1 | - | 92 | 1 | - | 80 | 1 | - |
| Present | 92 | 0.9 | (0.6,1.5) | 188 | 1.2 | (0.7,2.2) | 177 | 1.6 | (1.0,2.7) |
|
Nerve root
deviation/ compression |
|||||||||
| Absent | 75 | 1 | - | 140 | 1 | - | 130 | 1 | - |
| Present | 64 | 1 | (0.6,1.6) | 140 | 2.5 | (1.4,4.5) | 127 | 1.8 | (1.1,3.1) |
|
Number of
MRI abnormalities |
|||||||||
| 0 | 19 | 1 | - | 34 | 1 | - | 30 | 1 | - |
| 1 | 20 | 0.9 | (0.4,2.3) | 39 | 1.5 | (0.5,4.2) | 35 | 1.3 | (0.5,3.3) |
| 2 | 37 | 0.9 | (0.4,1.9) | 72 | 1.3 | (0.5,2.9) | 68 | 1.3 | (0.6,2.8) |
| 3 | 37 | 1 | (0.5,2.2) | 80 | 2.1 | (0.9,5.0) | 74 | 1.9 | (0.9,4.3) |
| 4 | 26 | 1.2 | (0.5,2.6) | 55 | 3.9 | (1.3,11.6) | 50 | 3.1 | (1.2,8.2) |
In past 12 months
Odds ratios adjusted for sex and age (in five bands)
Table 4 shows associations between MRI abnormalities and two well-established physical risk factors for LBP – occupational lifting and work with the back bent or twisted. MRI abnormalities were less likely to be found in the presence of these risk factors than in their absence. In particular, relative to no abnormalities, the OR for the presence of all four abnormalities in patients whose work involved bending or twisting of the back for more than an hour per day was 0.2 (95%CI 0.1-0.8).
Table 4. Associations of MRI abnormalities with occupational physical activities.
Analysis was restricted to the 270 patients who were in their most recent paid job at the time their current episode of LBP began
| MRI abnormality | Lifting weights >10 kg more than 10 timesa |
Work with back bent or twisted for >1 houra |
||||
|---|---|---|---|---|---|---|
| n | ORb | (95% CI) | n | ORb | (95% CI) | |
| HIZ | ||||||
| Absent | 27 | 1 | - | 22 | 1 | - |
| Present | 35 | 0.7 | (0.4,1.3) | 25 | 0.6 | (0.3,1.2) |
| Disc degeneration | ||||||
| Absent | 38 | 1 | - | 31 | 1 | - |
| Present | 24 | 0.8 | (0.4,1.4) | 16 | 0.6 | (0.3,1.2) |
| Disc herniation | ||||||
| Absent | 23 | 1 | - | 19 | 1 | - |
| Present | 39 | 0.7 | (0.4,1.2) | 28 | 0.6 | (0.3,1.2) |
|
Nerve root
deviation/compression |
||||||
| Absent | 33 | 1 | - | 30 | 1 | - |
| Present | 29 | 0.9 | (0.5,1.6) | 17 | 0.5 | (0.3,1.0) |
|
Numbers of
MRI abnormalities |
||||||
| 0 | 14 | 1 | - | 11 | 1 | - |
| 1 | 7 | 0.5 | (0.2,1.6) | 7 | 0.8 | (0.2,2.5) |
| 2 | 13 | 0.5 | (0.2,1.2) | 12 | 0.6 | (0.2,1.6) |
| 3 | 18 | 0.5 | (0.2,1.3) | 13 | 0.5 | (0.2,1.2) |
| 4 | 10 | 0.5 | (0.2,1.3) | 4 | 0.2 | (0.1,0.8) |
Activity in an average working day in job held at time current episode of LBP began
Odds ratio adjusted for sex and age (in five bands)
Tables 5 and 6 show associations of MRI abnormalities with somatising tendency, report of pain at other anatomical sites, low mood, fear-avoidance beliefs, and propensity to consult because of LBP. None of these psychological risk factors showed clear differences in prevalence according to whether MRI abnormalities were present or absent.
Table 5.
Associations of MRI abnormalities with report of somatic symptoms
| MRI abnormality | Number of distressing somatic symptoms in past weeka |
Number of anatomical sites painful in past 4 weeksb |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 |
1 |
2+ |
0 |
1 |
2+ |
|||||||||
| n | n | ORc | (95% CI) | n | ORc | (95% CI) | n | n | ORc | (95% CI) | n | ORc | (95% CI) | |
|
|
||||||||||||||
| HIZ | ||||||||||||||
| Absent | 67 | 29 | 1 | - | 34 | 1 | - | 76 | 26 | 1 | - | 29 | 1 | - |
| Present | 119 | 52 | 1 | (0.6,1.8) | 45 | 0.7 | (0.4,1.3) | 119 | 48 | 1.1 | (0.6,1.9) | 52 | 1.2 | (0.7,2.0) |
| Disc degeneration | ||||||||||||||
| Absent | 96 | 44 | 1 | - | 46 | 1 | - | 114 | 41 | 1 | - | 38 | 1 | - |
| Present | 90 | 37 | 0.8 | (0.5,1.4) | 33 | 0.7 | (0.4,1.3) | 81 | 33 | 1.1 | (0.6,1.9) | 43 | 1.6 | (0.9,2.8) |
| Disc herniation | ||||||||||||||
| Absent | 60 | 28 | 1 | - | 28 | 1 | - | 61 | 27 | 1 | - | 30 | 1 | - |
| Present | 126 | 53 | 1.1 | (0.6,2.0) | 51 | 1.1 | (0.6,1.9) | 134 | 47 | 0.8 | (0.5,1.4) | 51 | 0.9 | (0.5,1.6) |
|
Nerve root
deviation/compression |
||||||||||||||
| Absent | 95 | 46 | 1 | - | 46 | 1 | - | 98 | 45 | 1 | - | 47 | 1 | - |
| Present | 91 | 35 | 0.8 | (0.5,1.5) | 33 | 0.9 | (0.5,1.5) | 97 | 29 | 0.6 | (0.4,1.1) | 34 | 0.8 | (0.5,1.3) |
|
Numbers of MRI
abnormalities |
||||||||||||||
| 0 | 27 | 7 | 1 | - | 14 | 1 | - | 27 | 12 | 1 | - | 9 | 1 | - |
| 1 | 17 | 17 | 4.2 | (1.3,13.6) | 14 | 1.4 | (0.5,4.2) | 23 | 11 | 0.8 | (0.3,2.5) | 18 | 1.9 | (0.7,5.5) |
| 2 | 55 | 23 | 1.5 | (0.5,4.1) | 17 | 0.7 | (0.3,1.8) | 59 | 18 | 0.7 | (0.3,1.7) | 18 | 0.9 | (0.3,2.4) |
| 3 | 49 | 22 | 2.2 | (0.8,6.2) | 22 | 1.1 | (0.4,2.6) | 54 | 22 | 0.7 | (0.3,1.7) | 18 | 1 | (0.4,2.7) |
| 4 | 38 | 12 | 1.2 | (0.4,3.6) | 12 | 0.8 | (0.3,2.1) | 32 | 11 | 0.8 | (0.3,2.2) | 18 | 1.8 | (0.7,4.9) |
From total of five symptoms – faintness/dizziness, pains in heart/chest, nausea/upset stomach, trouble getting breath, hot/cold spells
From a total of four anatomical sites – neck, shoulder, elbow, wrist/hand
Odds ratios adjusted for sex and age (in five bands)
Table 6.
Associations of MRI abnormalities with low mood, fear-avoidance beliefs and propensity to consult for low-back pain
| Characteristic | SF-36 Mental health scorea |
Fear-avoidance beliefsb (number of statements agreed) |
Propensity to consult for LBPc (number of statements agreed) |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| best |
Intermediate |
Worst |
0 |
1 - 2 |
3 - 4 |
0 |
1 |
2 |
|||||||||||||
| n | n | ORd | (95% CI) | n | ORd | (95% CI) | n | n | ORd | (95% CI) | n | ORd | (95% CI) | n | n | ORd | (95% CI) | n | ORd | (95% CI) | |
| HIZ | |||||||||||||||||||||
| Absent | 41 | 45 | 1 | - | 45 | 1 | - | 32 | 74 | 1 | - | 24 | 1 | - | 31 | 33 | 1 | - | 66 | 1 | - |
| Present | 63 | 64 | 1 | (0.6,1.7) | 89 | 1.3 | (0.8,2.2) | 50 | 113 | 1 | (0.6,1.6) | 55 | 1.4 | (0.7,2.8) | 55 | 78 | 1.3 | (0.7,2.4) | 85 | 0.7 | (0.4,1.3) |
|
Disc
degeneration |
|||||||||||||||||||||
| Absent | 62 | 53 | 1 | - | 72 | 1 | - | 45 | 100 | 1 | - | 43 | 1 | - | 52 | 53 | 1 | - | 83 | 1 | - |
| Present | 42 | 56 | 1.6 | (0.9,2.7) | 62 | 1.3 | (0.8,2.2) | 37 | 87 | 1 | (0.6,1.8) | 36 | 0.9 | (0.4,1.6) | 34 | 58 | 1.6 | (0.9,2.8) | 68 | 1.2 | (0.7,2.1) |
| Disc herniation | |||||||||||||||||||||
| Absent | 35 | 37 | 1 | - | 44 | 1 | - | 30 | 61 | 1 | - | 25 | 1 | - | 29 | 30 | 1 | - | 57 | 1 | - |
| Present | 69 | 72 | 1 | (0.6,1.8) | 90 | 1.1 | (0.6,1.9) | 52 | 126 | 1.2 | (0.7,2.1) | 54 | 1.3 | (0.7,2.6) | 57 | 81 | 1.5 | (0.8,2.8) | 94 | 0.8 | (0.5,1.5) |
|
Nerve root
deviation/ compression |
|||||||||||||||||||||
| Absent | 53 | 54 | 1 | - | 81 | 1 | - | 44 | 102 | 1 | - | 42 | 1 | - | 57 | 51 | 1 | - | 80 | 1 | - |
| Present | 51 | 55 | 1.1 | (0.6,1.9) | 53 | 0.7 | (0.4,1.2) | 38 | 85 | 1 | (0.6,1.6) | 37 | 1 | (0.6,2.0) | 29 | 60 | 2.4 | (1.3,4.3) | 71 | 1.8 | (1.0,3.2) |
|
Numbers of MRI
abnormalities |
|||||||||||||||||||||
| 0 | 18 | 12 | 1 | - | 18 | 1 | - | 15 | 25 | 1 | - | 8 | 1 | - | 12 | 12 | 1 | - | 24 | 1 | - |
| 1 | 9 | 16 | 4.2 | (1.1,15.9) | 24 | 3.5 | (1.1,10.9) | 10 | 27 | 1.9 | (0.6,5.7) | 11 | 1.5 | (0.4,6.8) | 17 | 8 | 0.4 | (0.1,1.7) | 23 | 1.2 | (0.4,3.4) |
| 2 | 30 | 32 | 1.6 | (0.7,4.1) | 33 | 1.1 | (0.4,2.6) | 18 | 57 | 2.1 | (0.8,5.0) | 21 | 2.4 | (0.7,7.9) | 26 | 28 | 0.9 | (0.3,2.5) | 42 | 0.8 | (0.3,2.0) |
| 3 | 32 | 29 | 1.3 | (0.5,3.4) | 32 | 1.1 | (0.5,2.5) | 25 | 42 | 1 | (0.4,2.4) | 27 | 1.8 | (0.6,5.5) | 18 | 39 | 2 | (0.7,5.5) | 37 | 0.8 | (0.3,2.3) |
| 4 | 15 | 20 | 1.9 | (0.7,5.5) | 27 | 2 | (0.8,5.3) | 14 | 36 | 1.5 | (0.6,3.9) | 12 | 1.4 | (0.4,5.1) | 13 | 24 | 1.7 | (0.5,5.5) | 25 | 0.9 | (0.3,2.6) |
Data were missing for 7 cases
Data were missing for 6 cases
Data were missing for 6 cases
Odds ratio adjusted for sex and age (in five bands)
Discussion
In this sample of patients with mechanical LBP investigated by MRI, clinical presentation differed according to the presence or absence of MRI abnormalities in the lumbar spine, nerve root displacement/compression being substantially more frequent when pain radiated to below the knee or was associated with weakness or numbness below the knee. However, we found no strong indications of differences in the prevalence of either physical or psychological risk factors between patients with and without demonstrable spinal pathology. If anything, and contrary to our original hypothesis, physical risk factors appeared to be more common in patients with no MRI abnormalities.
The LBP patients whom we studied had all been referred for investigation by MRI, and of those eligible for inclusion in the study, only 52% satisfactorily completed questionnaires. To the extent that referral of LBP patients for MRI is more likely when the symptom is persistent and disabling, this outcome will reflect a combination of incidence, persistence and disability. However, that should not have been a limitation, since all of the risk factors examined have been shown to relate these different aspects of LBP. In some cases the decision to perform MRI may have been influenced by the pattern of symptoms or by findings on earlier imaging, and it is possible that some patients chose to participate because they knew what had been found on their scan. However, such selection would have led to bias only if the association of spinal abnormalities with symptoms or risk factors were systematically different in participants as compared with non-participants – for example, if patients exposed to occupational lifting were less likely to take part when they knew that they had a herniated disc, whereas among patients unexposed to occupational lifting, knowledge of a herniated disc had no influence on participation. Important systematically differential selection of this sort seems unlikely.
In theory, patients’ knowledge of their MRI findings might also have influenced their recall and reporting of symptoms or risk factors. However, it is difficult to conceive why, for example, people with LBP would be more likely to remember occupational lifting if they had no MRI abnormalities than if MRI abnormalities had been observed.
Psychological risk factors were assessed shortly after patients presented for MRI, and therefore when LBP was already present. Thus, it is possible that they may have been modified by the occurrence of the back complaint, which in some cases had been present for many years. However, to the extent that all of the patients had symptoms of sufficient severity to warrant investigation by MRI, this is unlikely to have biased associations with specific findings on MRI.
Because patients might have moved to new employment since the onset of their LBP, our analysis of associations with occupational physical activities was restricted to patients who were in their most recent job when their current episode of LBP began. It remains possible that some patients, while continuing in the same job, may have modified their duties at work as a consequence of their back problem. Again, however, there is no obvious reason why such changes should have occurred differentially in patients with and without spinal pathology.
Another possible limitation of the study method was inaccuracy in the classification of MRI abnormalities. MRI assessments were conducted blind to clinical details and questionnaire responses, and therefore such errors would be expected, if anything, to obscure associations with clinical presentations and risk factors. The repeatability of MRI classification, both within and between observers, was generally moderate or good, and although it was poorer for disc herniation, clear relationships were found between MRI abnormalities, including disc herniation, and the presence of symptoms in the leg. Associations of nerve root deviation/compression and disc herniation with pain and neurological symptoms in the leg were not unexpected, but they suggest that the method of MRI classification was reasonably accurate.
Despite this, and contrary to our prior hypothesis, we found no indication that physical risk factors were more prevalent among patients with MRI abnormalities, or psychological risk factors in patients who did not have MRI abnormalities. Occupational bending and twisting was less common in patients with demonstrable spinal pathology than in those without, while the prevalence of psychological risk factors was little different in those with and without positive MRI findings. This should not be taken to imply that activities such as bending and twisting have no influence on the development of spinal pathology. However, it suggests that any impact is lower than that on LBP that occurs in the absence of demonstrable pathology.
As shown in an earlier systematic review, the four MRI abnormalities that we examined in our study are by no means perfect indicators of underlying pathology in patients with LBP [7]. Individually, each abnormality is likely to be responsible for fewer than half of the cases of LBP in which it is found. Nevertheless, if risk factors differed importantly according to whether LBP arises from such abnormalities, we would expect the difference to have been apparent in our analysis, and especially where multiple pathology was observed as compared with none at all. We cannot exclude the possibility of differential associations with other risk factors that we did not investigate. However, those that we studied have shown the strongest and most consistent associations with LBP in previous research.
Relatively few previous studies have explored risk factors for low back pain associated with specified spinal pathology. In an early case-control investigation, Kelsey found that risk of clinically diagnosed herniated lumbar intervertebral disc was only minimally increased in relation to lifting, and was unrelated to stressful life events [15]. However, in a second study, there were clear associations with occupational lifting, especially if carried out with the body twisted [14]. In a third study, she found associations with frequent non-occupational lifting and twisting while lifting [22], but not with use of weight-lifting equipment [21]. In a Finnish case-control study, hospital treatment for herniated lumbar intervertebral disc was more common in blue collar workers [8], and in a Danish register-based study, surgery for herniated lumbar disc was more frequent among assistant nurses (an occupation that involved heavy lifting) than in the general population [11]. More recently, a case-control study in Germany found that acute lumbar disc herniation was related to bending, but an association with lifting and carrying was limited to patients with concomitant osteochondrosis or spondylosis [27]. Cases also reported more psychological pressures at work than the controls. A study of 49 Korean military conscripts with symptomatic lumbar disc herniation confirmed by MRI showed associations with both depression and anxiety in comparison with healthy controls [16]. Disc degeneration of the lumbar spine has been reported to occur more commonly in foundry workers (a physically demanding job) than in the general population of men [17], and in another study, was related to heavier lifetime physical loading of the spine [2], although in neither of these studies was the back necessarily painful.
We have identified only one earlier study that compared risk factors for LBP according to the presence of spinal pathology. In a cohort of Finnish workers from the metal industry, low job control carried an increased risk of subsequent hospitalisation for back disorders other than of the intervertebral disc, where as no corresponding association was observed for disc disorders [13]. Moreover, hospital admission for disc disorders was differentially associated with heavy smoking and high body mass index [12]. However, the completeness and reliability with which disc disorders were ascertained is unclear.
Unlike these earlier investigations, our study did not estimate the risk of LBP, either with or without spinal pathology, according to the presence of risk factors. To do so would have required a control group of patients with no LBP. Rather, we sought evidence of differential associations with risk factors according to whether spinal pathology was present or absent.
In summary, our study did not support the hypothesis that physical risk factors are relatively more important as risk factors for mechanical LBP arising from spinal pathology, and psychological risk factors for LBP that occurs in the absence of demonstrable pathology. This failure to detect predicted differential associations with risk factors is unlikely to be explained by errors in the ascertainment of risk factors or classification of MRI findings. When researching the causes and primary prevention of LBP, there may be little value in distinguishing between cases according to the presence or absence of the more common forms of potentially underlying spinal pathology.
Short summary.
In patients with low back pain investigated by magnetic resonance imaging, absence of demonstrable spinal pathology was not associated differentially with psychological risk factors.
Figure 1.
Acknowledgements
This research was supported by the European Commission under the Quality of Life and Management of Living Resources programme, project QLK4-2002-02650 (VIBRISKS). Clare Harris was funded by a grant from the Colt Foundation. We thank Ken Cox for his assistance with computing, the staff of the three radiology departments at which patients were recruited, and the patients who gave up time to take part in the study.
Footnotes
Conflicts of Interest: None
References
- 1.Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disk on magnetic reonance imaging. British Journal of Radiology. 1992;65:361–369. doi: 10.1259/0007-1285-65-773-361. [DOI] [PubMed] [Google Scholar]
- 2.Battié MC, Videman T, Gibbons LE, Fisher LD, Manninen H, Gill K. Determinants of lumbar disc degeneration: a study relating lifetime exposures and magnetic resonance imaging findings in identical twins. Spine. 1995;20:2601–2612. [PubMed] [Google Scholar]
- 3.Brant-Zawadzki M, Jensen M, Obuchowski N, Ross J, Modic M. Interobserver and intraobserver variability in interpretation of lumbar disk abnormalities: A comparison of two nomenclatures. Spine. 1995;20:1257–1264. doi: 10.1097/00007632-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Cohen J. A Coefficient of Agreement for Nominal Scales. Educational and Psychological Measurement. 1960;20(1):37–46. [Google Scholar]
- 5.Croft P, Lewis M, Jones C Wynn, Coggon D, Cooper C. Health status in patients awaiting hip replacement for osteoarthritis. Rheumatology. 2002;41:1001–7. doi: 10.1093/rheumatology/41.9.1001. [DOI] [PubMed] [Google Scholar]
- 6.Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- 7.Endean A, Palmer KT, Coggon D. Potential of MRI findings to refine case definition for mechanical low back pain in epidemiological studies: a systematic review. Spine. doi: 10.1097/BRS.0b013e3181cd9adb. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heliövaara M. Occupation and risk of herniated lumbar intervertebral disc or sciatica leading to hospitalization. J Chron Dis. 1987;40:259–264. doi: 10.1016/0021-9681(87)90162-7. [DOI] [PubMed] [Google Scholar]
- 9.Iles RA, Davidson M, Taylor NF. Psychological predictors of failure to return to work in non-chronic, non-specific low back pain; a systematic review. Occup Environ Med. 2008;65:505–517. doi: 10.1136/oem.2007.036046. [DOI] [PubMed] [Google Scholar]
- 10.Jarosz J, Bingham J, Pemberton J, Sambrook P, Spector T. An atlas for scoring cervical and lumbar disk degeneration. Springer Verlag; London: 1997. [Google Scholar]
- 11.Jørgensen S, Hein HO, Gyntelberg F. Heavy lifting at work and risk of genital prolapsed and herniated lumbar disc in assistant nurses. Occup Med. 1994;44:47–49. doi: 10.1093/occmed/44.1.47. [DOI] [PubMed] [Google Scholar]
- 12.Kaila-Kangas L, Leino-Arjas P, Riihimäki H, Luukkonen R, Kirjonen J. Smoking and overweight as predictors of hospitalization for back disorders. Spine. 2003;28:1860–8. doi: 10.1097/01.BRS.0000083284.47176.80. [DOI] [PubMed] [Google Scholar]
- 13.Kaila-Kangas L, Kivimäki M, Riihimäki H, Luukkonen R, Kirjonen J, Leino-Arjas P. Psychosocial factors at work as predictors of hospitalization for back disorders: a 28-year follow-up of industrial employees. Spine. 2004;29:1823–30. doi: 10.1097/01.brs.0000134572.46151.0a. [DOI] [PubMed] [Google Scholar]
- 14.Kelsey JL, Githens PB, White AA, Holford TR, Walter SD, O’Connor T, Ostfeld AM, Weil U, Southwick WO, Calogero JA. An epidemiologic study of lifting and twisting on the job and risk for acute prolapsed lumbar intervertebral disc. J Orthop Res. 1984;2:61–66. doi: 10.1002/jor.1100020110. [DOI] [PubMed] [Google Scholar]
- 15.Kelsey JL. An epidemiological study of acute herniated lumbar intervertebral discs. Rheumatol Rehabil. 1975;14:144–159. doi: 10.1093/rheumatology/14.3.144. [DOI] [PubMed] [Google Scholar]
- 16.Kim T-S, Pae C-U, Hong C-K, Kim J-J, Lee C-U, Lee S-J, Paik I-H, Lee C. Interrelationships among pain, disability and psychological factors in young Korean conscripts with lumbar disc herniation. Military Med. 2006;171:1113–1116. doi: 10.7205/milmed.171.11.1113. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence JS, Molyneux MK, Dingwall-Fordyce I. Rheumatism in foundry workers. Br J Industr Med. 1966;23:42–52. doi: 10.1136/oem.23.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 19.Lötters F, Burdorf A, Kuiper J, Miedama H. Model for the work-relatedness of low-back pain. Scand J Work Environ Health. 2003;29:431–440. doi: 10.5271/sjweh.749. [DOI] [PubMed] [Google Scholar]
- 20.Masaryk TJ, Ross JS, Modic MT, Boumphrey F, Bohlman H, Wilber G. High resolution MR imaging of a sequestered lumbar intervertebral disks. Am J Neuroradiol. 1988;9:351–358. doi: 10.2214/ajr.150.5.1155. [DOI] [PubMed] [Google Scholar]
- 21.Mundlt DJ, Kelsey JL, Golden AL, Golden AL, Panjabi MM, Pastides H, Berg AT, Sklar J, Hosea T, Northeast Collaborative Group on Low Back pain An epidemiologic study of sports and weight lifting as possible risk factors for herniated lumbar and cervical discs. Am J Sports Med. 1993;21:854–860. doi: 10.1177/036354659302100617. [DOI] [PubMed] [Google Scholar]
- 22.Mundt DJ, Kelsey JL, Golden AL, Pastides H, Berg AT, Sklar J, Hosea T, Panjabi MM, North east Collaborative Group on Low Back Pain An epidemiologic study of non-occupational lifting as a risk factor for herniated lumbar intervertebral disc. Spine. 1993;18:595–602. doi: 10.1097/00007632-199304000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Palmer KT, Calnan M, Wainwright D, Poole J, O’Neill C, Winterbottom A, Watkins C, Coggon D. Disabling musculoskeletal pain and its relation to somatisation: a community-based postal survey. Occup Med. 2005;55:612–617. doi: 10.1093/occmed/kqi142. [DOI] [PubMed] [Google Scholar]
- 24.Palmer KT, Harris EC, Griffin MJ, Bennett J, Reading I, Sampson M, Coggon D. Case-control study of low-back pain referred for magnetic resonance imaging, with special focus on whole-body vibration. Scand J Work Environ Health. 2008;34:364–373. doi: 10.5271/sjweh.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pfirrmann C, Dora C, Schmid M, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: Reliability study with surgical correlation. Radiology. 2004;230:583–8. doi: 10.1148/radiol.2302021289. [DOI] [PubMed] [Google Scholar]
- 26.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohort studies of low back pain. Spine. 2002;27:E109–120. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 27.Seidler A, Bolm-Audorff U, Siol T, Henkel N, Fuchs C, Schug H, Leheta F, Marquardt G, Schmitt E, Ulrich PT, Beck W, Missala A, Elsner G. Occupational risk factors for symptomatic lumbar disc herniation; a case-control study. Occup Environ Med. 2003;60:821–830. doi: 10.1136/oem.60.11.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.StataCorp . Stata Statistical Software: Release 11. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- 29.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE. SF-36 Health Status Questionnaire. Institute for the Improvement of Medical Care and Health, New England Medical Center Hospital, Quality Quest Inc; Boston, MA: 1989. [Google Scholar]
- 31.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: Prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]