Abstract
This prospective study surveyed the prevalence of peripheral arterial disease (PAD) in Korean patients with coronary arterial disease (CAD) or cerebrovascular disorder (CVD). From March 2010, 576 hospitalized patients in cardiovascular or stroke center were enrolled as the study group. Ankle-brachial index (ABI) was measured and the cut-off point for diagnosing PAD was ≤ 0.9 at rest. A total of 424 hospitalized patients in the Department of Surgery and aged ≥ 50 yr was enrolled as the control group. The prevalence of PAD was significantly higher in the study group than the control group (7.6% vs 1.7%; P < 0.001). To analyze the relationship of other vascular diseases and PAD, the patients were regrouped; group A (no CAD or CVD), group B (CAD only), group C (CVD only), and group D (CAD and CVD). Compared with group A, those with other vascular diseases (group B, C, D) had significantly higher prevalence of PAD, diabetes, dyslipidemia, renal insufficiency and claudication. The trend that patients with CAD or CVD are at risk of PAD is observed in this cross-sectional study in Koreans. Routine ABI measurement is recommended in these high-risk groups for early detection and proper management of PAD.
Keywords: Ankle-Brachial Index, Peripheral Arterial Disease, Prevalence, Coronary Artery Disease, Cerebrovascular Disorder
INTRODUCTION
The risk of peripheral arterial disease (PAD) in patients with coronary artery disease (CAD) or cerebrovascular disorders (CVD) is known to be high in Western population (1). The prognosis of PAD is worse than that of advanced cancer. However, it is usually not dealt with much concern (1). Considering patients with PAD are at high risk of death from cardiovascular origin, three major vascular disorders, including CAD, CVD, and PAD will be managed together (2). However, unfortunately, clinical importance of PAD is usually underestimated, because the majority of the patients are neglecting the chronic symptoms of leg ischemia (3).
Ankle-brachial index (ABI) is known to be useful for detecting PAD in both symptomatic and asymptomatic patients (4). ABI value of 0.90 or less indicates generally the presence of PAD, and lower ABI value is related to higher mortality (5, 6). Many reports on the prevalence of PAD in high risk patients have been published in Western countries. However, there is few data in the prevalence of PAD in Korean population. And also, the prevalence of PAD in high risk patients, such as CAD or CVD, is not known in Korean population.
Therefore, we performed this prospective study to survey the prevalence of PAD using ankle-brachial index (ABI) in Korean patients with CAD or CVD.
MATERIALS AND METHODS
Inclusion and exclusion criteria
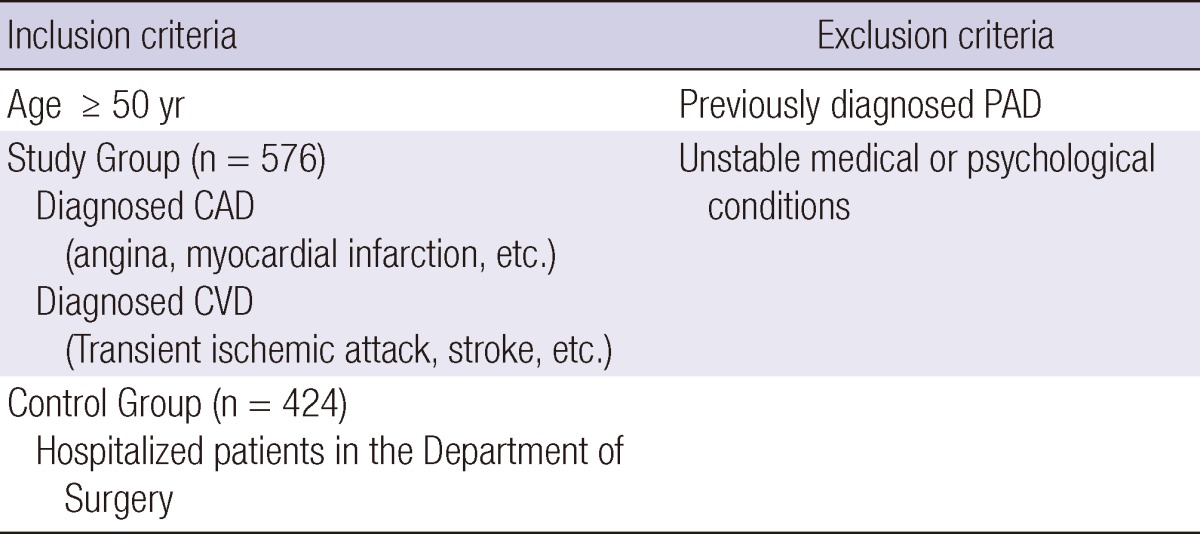
Inclusion criteria for the study group were 1) age ≥ 50 yr old, and 2) hospitalized in Seoul National University Hospital with the diagnosis of CAD or CVD. Study group included patients who were diagnosed as CAD (angina, myocardial infarction) or CVD (ischemic stroke, transient ischemic attack) with or without risk factors (diabetes mellitus, hypercholesterolemia, arterial hypertension, smoking, and high body mass index). Patients admitted in the Department of Surgery for other diseases during the same period and older than 50 yr were enrolled as the control group.
Exclusion criteria were previously diagnosed PAD and unstable medical or psychological conditions that would compromise the patient's safety or successful participation in the study. Patient who were unwilling to participate in the study or unable to provide informed consent were not included. These criteria are summarized in Table 1.
Table 1.
Selection criteria
Data Collection
For the study, data on demographics and personal medical history were obtained by patient interview and electronic medical records. Presence of the risk factors for PAD were surveyed, including smoking, body mass index (BMI), hypertension, diabetes mellitus (DM), homocysteinemia, renal dysfunction and dyslipidemia. Height and weight were measured during the index admission and BMI was calculated as kg/m2. Hypertension, dyslipidemia, or diabetes were deemed present if diagnosed by a physician or controlled with medications. Hypertension was defined as a systolic pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg. DM was defined as either taking insulin or glucose lowering agents or fasting plasma glucose level > 140 mg/dL. Dyslipidemia was defined as total cholesterol level > 190 mg/dL, low-density lipoprotein > 115 mg/dL, high-density lipoprotein < 40 mg/dL, or triglyceride levels > 150 mg/dL, and/or if patients were taking lipid-lowering drugs, according to the third report of the National Cholesterol Education Program (NCEP) (7).
For the measurement of ABI, systolic blood pressures in bilateral arms (brachial artery) and ankles (posterior tibial artery or dorsalis pedis artery) were measured by trained physician assistants using a 10-20 cm sphygmomanometer and a handheld Doppler (Hadeco®, Tokyo, Japan). ABI was calculated by dividing the highest ankle systolic pressure by the highest brachial pressure. PAD was defined if ABI was ≤ 0.9 in either leg. Claudication symptom was also noted.
Statistical analysis
The descriptive analysis was expressed with mean ± standard deviation of different variables. The odds ratio (OR) and confidence intervals (CI) were calculated. The chi-square test was used to perform univariate analysis for categorical variables, analysis of variance (ANOVA) and Student t test for continuous variables. Fisher exact test was used to compare the overlap in vascular diseases affecting different territories between SNUH data and TASC II. Logistic regression was used to calculate the odds of PAD associated with CAD or CVD, adjusted for difference in age, diabetes mellitus, and dyslipidemia. All analysis was carried out using SPSS V. 17.0 Windows (SPSS Inc., Chicago, IL, USA). A P value < 0.05 was considered as statistically significant.
Ethics statement
The protocol of this study was approved by the Seoul National University Hospital (SNUH) Institutional Review Boards (IRB No. 1001-002-304), and was performed according to the Declaration of Helsinki. After providing informed consent, one thousand individuals hospitalized in SNUH were enrolled from March to August 2010.
RESULTS
Patient demographics and PAD prevalence
A total of 1,000 patients were analyzed, including 576 in the study group and 424 in the control group. The patients' characteristics are shown in Table 2. According to the study design, the number of CAD and CVD were significantly higher in the study group (P < 0.001, P < 0.001). In the control group, 35 (8.2%) and 14 (3.3%) patients had histories of CAD and CVD, respectively. There were no difference in the smoking history (P = 0.446). The prevalence of dyslipidemia was higher in the study group (52.9% vs 11.4%, P < 0.001). Interestingly, the study group showed better lipid profile than the control group (total cholesterol 148.29 mg/dL vs 162.95 mg/dL, P < 0.001; lower density lipid cholesterol 86 mg/dL vs 108 mg/dL, P < 0.001). The prevalence of PAD, defined by ABI ≤ 0.9, was significantly higher in the study group compared to the control group (7.64% vs 1.65%, P < 0.001). The presence of claudication symptoms was significantly higher in the study group (7.3% vs 0%, P < 0.001).
Table 2.
Demographics and the prevalence of peripheral arterial disease
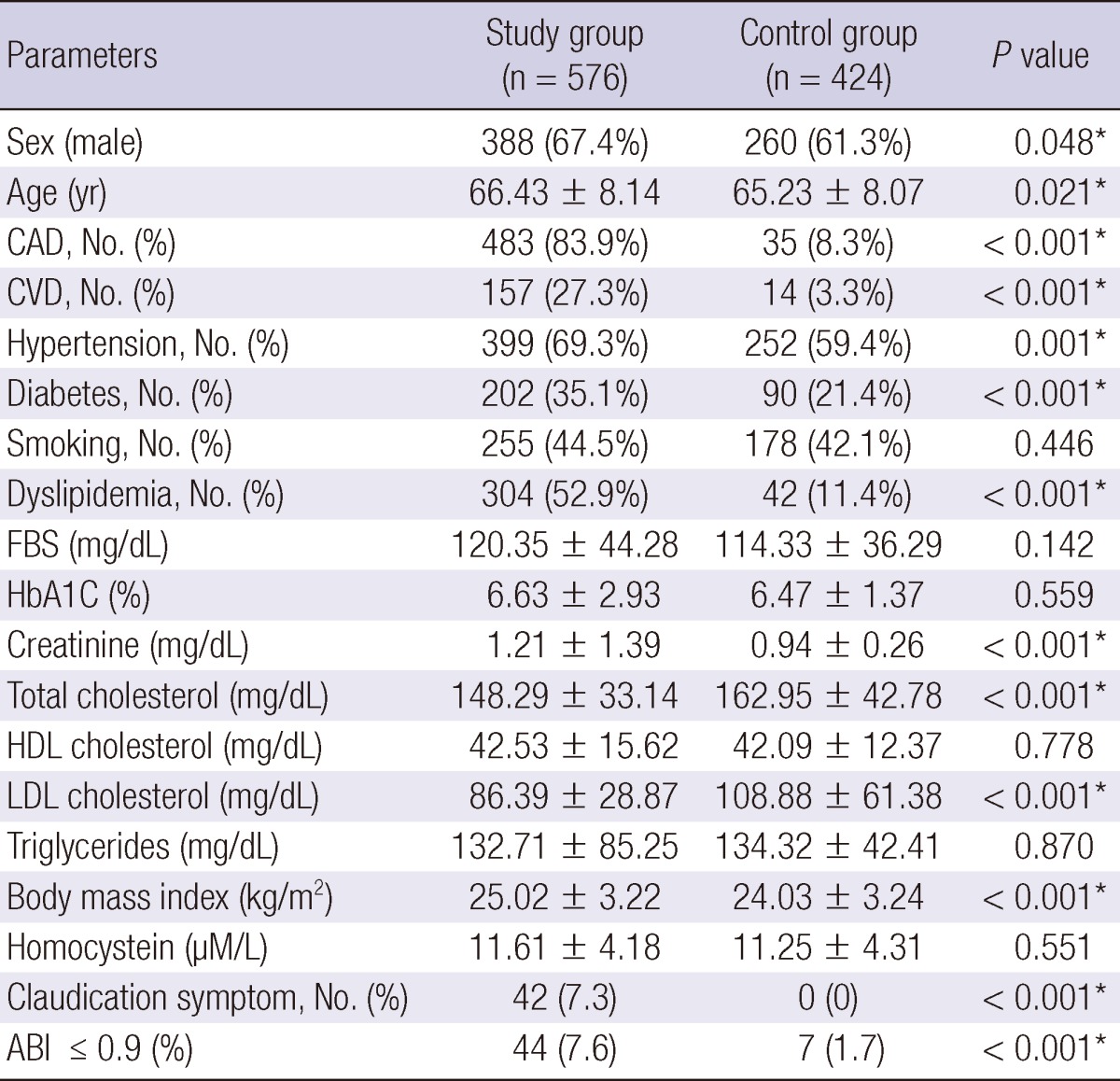
*P < 0.05. CAD, coronary arterial disease; CVD, cerebrovascular disease; FBS, fasting blood sugar; HbA1C, hemoglobin A1C; HDL, high density lipoprotein; LDL, low density lipoprotein.
Relationship of other vascular diseases and PAD
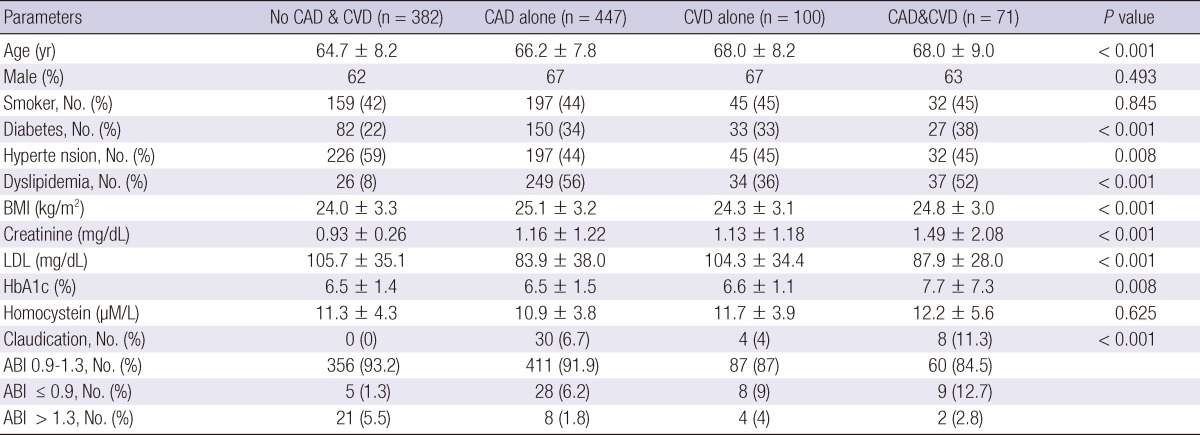
To analyze the relationship of other vascular diseases and PAD, the patients were regrouped; group A (no CAD/no CVD, 38.2%), group B (CAD alone, 44.7%), group C (CVD alone, 10%), and group D (CAD and CVD, 7.1%). Table 3 shows the baseline characteristics by vascular disease groups. Compared with group A, those with major vascular diseases (group B, C, D) had significantly higher prevalence of PAD (P <0.001), diabetes (P < 0.001), dyslipidemia (P < 0.001), and claudication symptoms (P < 0.001). The mean level of serum creatinine was higher in group D.
Table 3.
Relationship of other vascular disease and PAD
CAD, coronary arterial disease; CVD, cerebrovascular disease; BMI, body mass index; LDL, low density lipoprotein; HbA1C, hemoglobin A1C; LDL, low density lipoprotein; ABI, ankle-brachial index; PAD, peripheral artery disease.
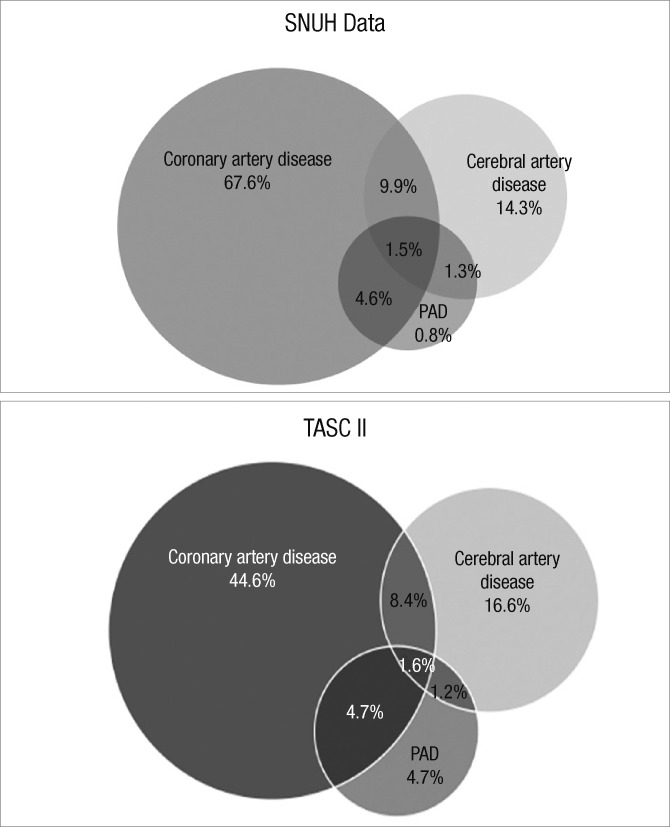
Fig. 1 represents overlaps in vascular diseases affecting different territories. The pattern of overlap was comparable with the data from TASC II (Trans-Atlantic Inter-Society Consensus) documents on the management of PAD (8, 9). Among the patients with symptomatic PAD in TASC II, 4.7% had concomitant CAD, 1.2% had concomitant CVD and 1.6% had both. And about 65% of patients with PAD had clinical evidence of other vascular diseases. In our data, 4.6% had concomitant CAD, 1.3% had concomitant CVD and 1.5% had both. And 90% of the patients with PAD were associated with CAD or CVD in our survey (P = 0.462; Fisher exact test).
Fig. 1.
Typical overlap in vascular diseases affecting different territories. PAD, peripheral artery disease.
Comparison of the risk factors for PAD
Results of univariate analysis for all risk factor are shown in Table 4. Patients with ABI ≤ 0.9 were older (69.9 ± 8.7 vs 65.7 ± 8.05; P < 0.001), had higher prevalence of CAD (72.5% vs 50.7%; P = 0.002) and CVD (35.3% vs 16.1%; P < 0.001). Diabetes and dyslipidemia were significantly higher in patients with ABI ≤ 0.9. A tendency of higher homocysteine and creatinine level was also seen in patients with ABI ≤ 0.9. By univariate analysis, CAD and CVD were associated with an increased prevalence of PAD. Especially patients with both CAD and CVD were at highest risk (adjusted odds ratio [OR] 8.076, 95% confidence interval [CI] 2.309-28.243) (Table 5).
Table 4.
Comparison of the presence of cardiovascular risk factors according to the ABI values
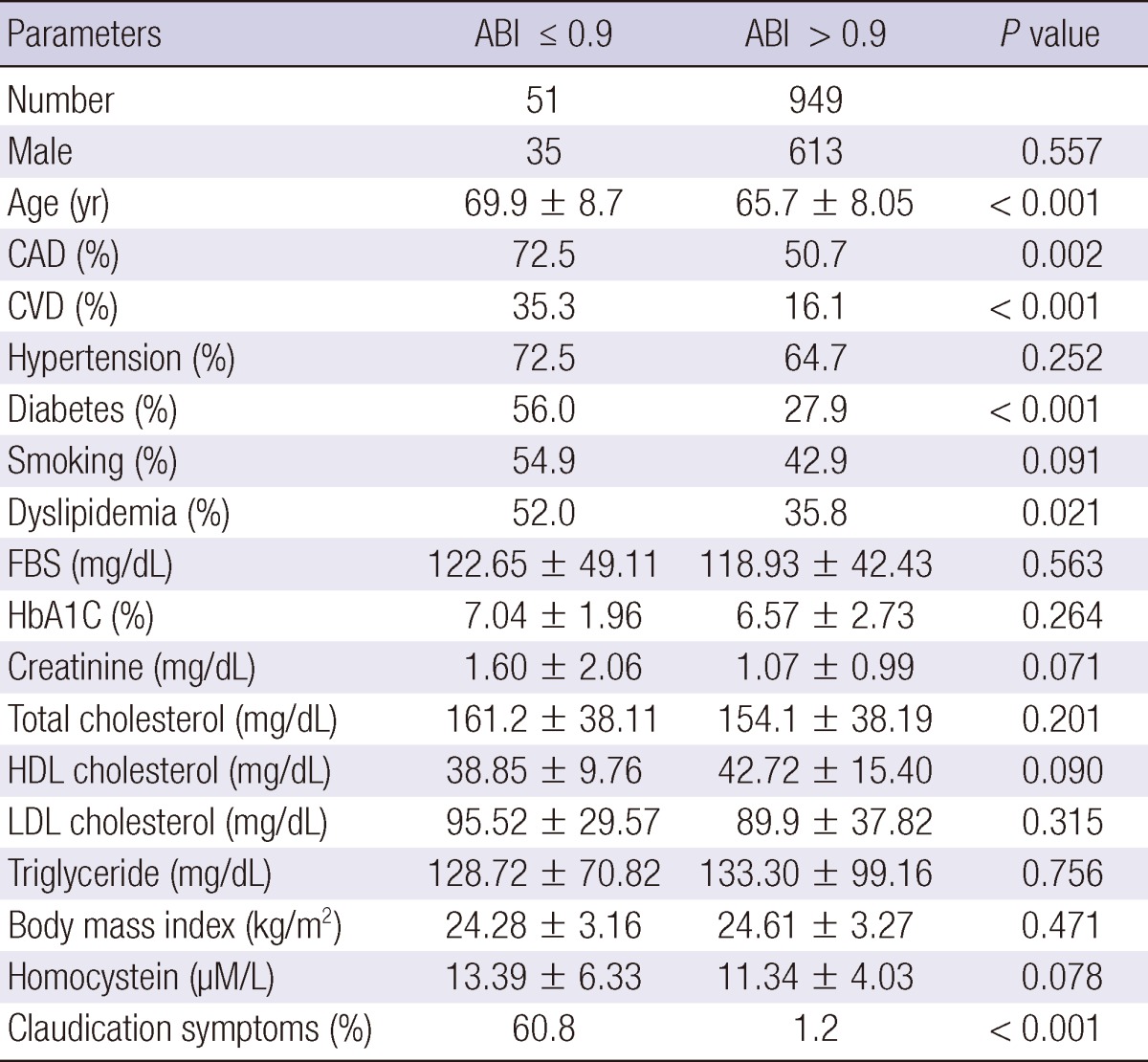
CAD, coronary arterial disease; CVD, cerebrovascular disease; FBS, fasting blood sugar; HbA1C, hemoglobin A1C; HDL, high density lipoprotein; LDL, low density lipoprotein.
Table 5.
Odds ratio for PAD in major vascular diseases
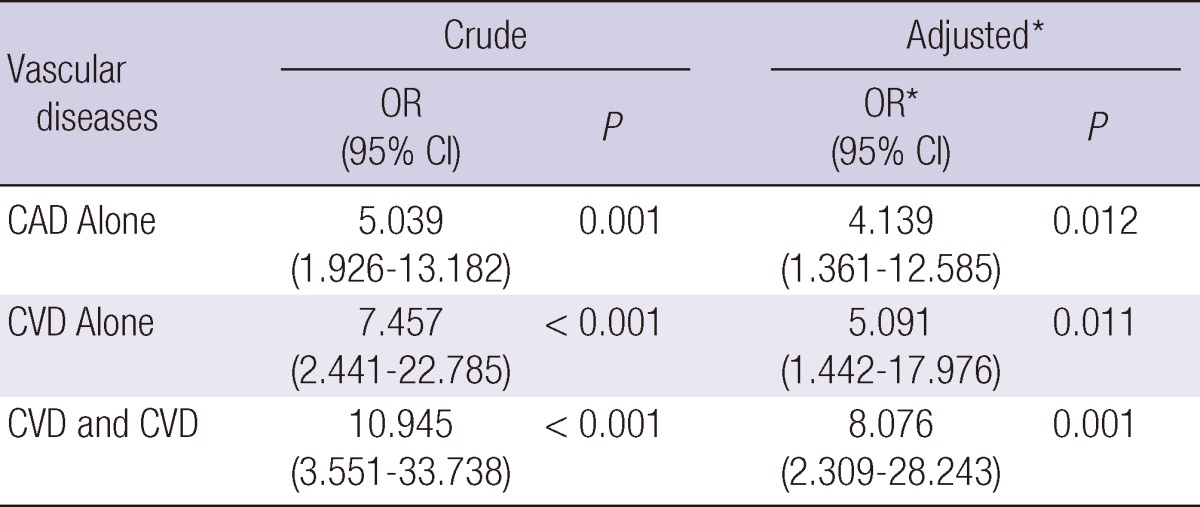
Risk of PAD significantly increased with CAD or CVD. *Adjusted for age, diabetes mellitus, dyslipidemia. OR, Odds ratio; CI, confidence interval; CAD, coronary arterial disease; CVD, cerebrovascular disease; PAD, peripheral artery disease.
DISCUSSION
Because atherosclerosis is a systemic disease, major atherosclerotic vascular diseases, including CAD, CVD, and PAD are related to each other. PAD represents an independent risk indicator of cardiovascular disease and cerebrovascular disease (10). Long-term prognosis of patients with PAD is significantly worse than patients with coronary artery disease (1). Despite its association with severe health risks, PAD remains underestimated or even neglected by clinicians or general population and routine PAD screening is seldom undertaken, especially in Korea (11).
To our knowledge, this is the first study ever reported the prevalence of PAD in high risk group of Korean patients with CAD or CVD. We found a higher prevalence of the unrecognized PAD in the study group (patients with CAD or CVD) compared to the control group (7.6% vs 1.7%, P < 0.001). The result of this study strongly suggests a need for routine screening of PAD in the high risk patients in Korea.
The prevalence of PAD in general population varies depending on the risk factors, including age, race, and gender. According to a previous study in a rural area in Korea, low ABI (< 0.9) was detected in 2.2% of men and 1.8% of women (12). This value was lower than that in a Western study showing higher prevalence of PAD in African-Americans (7.8%) and Caucasians (4.4%) (13). The prevalence of PAD in patients with CAD or CVD will also vary from country to country. In TASC II data based on REACH survey, 9.5% of patients with CAD alone and 6.7% of patients with CVD alone had PAD. Patients with both CAD and CVD had PAD in 16% cumulatively (9). In a Slovenian study, a total of 42% of patients with CAD and 36% of patients with CVD had PAD (14). Although the prevalence of PAD in patients with CAD or CVD are higher than that of general population in Korea and Western countries, but absolute percentage of PAD seems to be low in Korean population. However, we do not have enough evidences to conclude that real ethnic difference exists in Korean population. Large population-based epidemiologic studies are required.
The ankle-brachial index (ABI) is considered as a reliable method for diagnosing PAD (15). The association of low ABI (< 0.90) with risks of all-cause and CAD mortality was well established (6). Given the importance of the early detection and management of PAD, this diagnostic tool is useful in both symptomatic and asymptomatic patients. Another merit of ABI is that it is very easy to measure in the office or bedside and highly reproducible and reliable (15). Therefore, clinical practitioners should be familiar with the ABI measurement and utilize the ABI to detect PAD patients early.
Interestingly, the study group showed better lipid profile than the control group. This result might be due to taking medications for dyslipidemia. Almost all of the patients (99%) with dyslipidemia in the study group were currently receiving lipid-lowering therapy.
This study has some limitations. First, the control group was based on hospitalized patients, not in the general population. However, the incidence of PAD in the control group in our study was comparable with that in population-based researches. Salvatore and colleagues have shown that the overall prevalence of undiagnosed PAD in Sicily of Italy was 2.3% (16). We got a similar result of 1.7% in our control group. The real PAD prevalence in Korea should be studied in large population-based epidemiologic studies. Second, our study design is only a cross sectional study, not a cohort study. Long-term follow-up cohort studies are required to clarify the impacts of PAD on co-existing vascular disease. Third, diabetes and end stage renal disease are another important risk factors for PAD, which were not included in this study. That is because the ABI values in these groups of patients are not reliable due to the widespread vascular calcifications, which usually result in higher ABI value due to incompressible arteries. We are now conducting another study in these groups using toe-brachial index and aortic calcification index.
In conclusion, patients with CAD or CVD have higher risk for PAD. ABI should be performed regularly in high-risk patient group for early detection and proper management of PAD.
Footnotes
The work was supported by the Korean Society for Vascular Surgery (Yong Kak Lee- Astellas Scholarship, 2010).
References
- 1.Welten GM, Schouten O, Hoeks SE, Chonchol M, Vidakovic R, van Domburg RT, Bax JJ, van Sambeek MR, Poldermans D. Long-term prognosis of patients with peripheral arterial disease: a comparison in patients with coronary artery disease. J Am Coll Cardiol. 2008;51:1588–1596. doi: 10.1016/j.jacc.2007.11.077. [DOI] [PubMed] [Google Scholar]
- 2.Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, Browner D. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381–386. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 3.Bendermacher BL, Teijink JA, Willigendael EM, Bartelink ML, Peters RJ, de Bie RA, Büller HR, Boiten J, Langenberg M, Prins MH. A clinical prediction model for the presence of peripheral arterial disease: the benefit of screening individuals before initiation of measurement of the ankle-brachial index: an observational study. Vasc Med. 2007;12:5–11. doi: 10.1177/1358863X07076827. [DOI] [PubMed] [Google Scholar]
- 4.Sprynger M, Fassotte C, Verhaeghe R. The ankle-brachial pressure index and a standardized questionnaire are easy and useful tools to detect peripheral arterial disease in non-claudicating patients at high risk. Int Angiol. 2007;26:239–244. [PubMed] [Google Scholar]
- 5.Baxter GM, Polak JF. Lower limb colour flow imaging: a comparison with ankle: brachial measurements and angiography. Clin Radiol. 1993;47:91–95. doi: 10.1016/s0009-9260(05)81179-1. [DOI] [PubMed] [Google Scholar]
- 6.Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, Howard BV. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation. 2004;109:733–739. doi: 10.1161/01.CIR.0000112642.63927.54. [DOI] [PubMed] [Google Scholar]
- 7.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third report of the NCEP expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 8.Björck M, Bergqvist D, Eliasson K, Jansson I, Karlström L, Kragsterman B, Lundell A, Malmstedt J, Nordanstig J, Norgren L, et al. Twenty years with the Swedvasc Registry. Eur J Vasc Endovasc Surg. 2008;35:129–130. doi: 10.1016/j.ejvs.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295:180–189. doi: 10.1001/jama.295.2.180. [DOI] [PubMed] [Google Scholar]
- 10.Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, Wolfson SK Cardiovascular Heart Study (CHS) Collaborative Research Group. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Circulation. 1993;88:837–845. doi: 10.1161/01.cir.88.3.837. [DOI] [PubMed] [Google Scholar]
- 11.Hirsch AT, Murphy TP, Lovell MB, Twillman G, Treat-Jacobson D, Harwood EM, Mohler ER, 3rd, Creager MA, Hobson RW, 2nd, Robertson RM, et al. Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation. 2007;116:2086–2094. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 12.Kweon SS, Shin MH, Park KS, Nam HS, Jeong SK, Ryu SY, Chung EK, Choi JS. Distribution of the ankle-brachial index and associated cardiovascular risk factors in a population of middle-aged and elderly Koreans. J Korean Med Sci. 2005;20:373–378. doi: 10.3346/jkms.2005.20.3.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kullo IJ, Bailey KR, Kardia SL, Mosley TH, Jr, Boerwinkle E, Turner ST. Ethnic differences in peripheral arterial disease in the NHLBI Genetic Epidemiology Network of Arteriopathy (GENOA) study. Vasc Med. 2003;8:237–242. doi: 10.1191/1358863x03vm511oa. [DOI] [PubMed] [Google Scholar]
- 14.Poredos P, Jug B. The prevalence of peripheral arterial disease in high risk subjects and coronary or cerebrovascular patients. Angiology. 2007;58:309–315. doi: 10.1177/0003319707302494. [DOI] [PubMed] [Google Scholar]
- 15.Holland-Letz T, Endres HG, Biedermann S, Mahn M, Kunert J, Groh S, Pittrow D, von Bilderling P, Sternitzky R, Diehm C. Reproducibility and reliability of the ankle-brachial index as assessed by vascular experts, family physicians and nurses. Vasc Med. 2007;12:105–112. doi: 10.1177/1358863X07077281. [DOI] [PubMed] [Google Scholar]
- 16.Santo Signorelli S, Anzaldi M, Fiore V, Catanzaro S, Simili M, Torrisi B, Neri S. Study on unrecognized peripheral arterial disease (PAD) by ankle/brachial index and arterial comorbidity in Catania, Sicily, Italy. Angiology. 2010;61:524–529. doi: 10.1177/0003319710371614. [DOI] [PubMed] [Google Scholar]