Abstract
It is well documented that high therapeutic doses of oxazaphosphorines, cyclophosphamide (CP) and ifosfamide (IFO), are associated with cardiomyopathy. This study investigated whether oxazaphosphorines alter the expression of organic cation/carnitine transporter (OCTN2) and antioxidant genes and if so, whether these alterations contribute to CP and IFO-induced cardiotoxicity. Adult male Wistar albino rats were assigned to one of six treatment groups namely, control, L carnitine, CP, IFO, CP plus L carnitine and IFO plus L carnitine. In cardiac and kidney tissues, CP and IFO significantly decreased mRNA and protein expression of OCTN2. Oxazaphosphorines significantly increased serum acyl-carnitine/free carnitine ratio and urinary carnitine excretion and significantly decreased total carnitine in cardiac tissues. Interestingly, carnitine supplementation completely reversed the biochemical and gene expression changes-induced by oxazaphosphorines to the control values, except OCTN2 expression remained inhibited by IFO. Data from this study suggest that: (1) Oxazaphosphorines decreased myocardial carnitine content following the inhibition of OCTN2 mRNA and protein expression in cardiac tissues. (2) Oxazaphosphorine therapy increased urinary loss of carnitine secondary to the inhibition of OCTN2 mRNA and protein expression in proximal tubules of the kidney. (3) Carnitine supplementation attenuates CP but not IFO-induced inhibition of OCTN2 mRNA and protein expression in heart and kidney tissues.
1. Introduction
Even today, 53 years after its introduction, the nitrogen mustard alkylating oxazaphosphorine prodrug cyclophosphamide (CP) and its structural isomer ifosfamide (IFO) are the most widely used in polychemotherapy regimens and immunosuppressive protocols [1, 2]. Several clinical and experimental studies reported that administration of high therapeutic doses of CP can cause lethal cardiotoxicity during or soon after (10 days) administration [3–8]. It is manifested clinically as acute or subacute onset of congestive heart failure, arrhythmias, cardiac tamponade, and myocardial depression [3, 9, 10]. The incidence of CP-induced cardiotoxicity was reported in several clinical studies to be 20–25% with 8–12% mortality [10–12]. However, it seems that low doses of CP can be effective with little toxicity [13]. Although IFO has not been added to the list of antineoplastic therapies associated with major cardiac complications, its cardiotoxicity was reported as isolated clinical cases in cancer patients receiving IFO in combination with other anticancer drugs [14]. Cardiac effects reported with IFO therapy include supraventricular arrhythmias with a 30% incidence of congestive heart failure and dilated cardiomyopathy in patients receiving 16–18 g/m2 of IFO [14, 15]. Earlier and recent studies reported that high doses of CP and IFO induced hemorrhagic myocardial necrosis and increased lactate dehydrogenase and creatine phosphokinase activities [16–18]. Recent study in our laboratory have demonstrated that IFO is usually associated in the setting of nephrotoxicity and increased urinary carnitine loss, with severe cardiotoxicity [19]. The pathogenesis of oxazaphosphorines-induced acute cardiotoxicity was attributed primarily to an increase in oxygen-free radicals and decrease in the antioxidant defense mechanism in the myocardium [4, 17–19].
L carnitine (β-hydroxy-γ-trimethyl-amino-butyric acid) is an essential cofactor for the transport of long-chain fatty acids from cytoplasmic compartment into mitochondria, where β-oxidation enzymes are located [20, 21]. Humans cover their carnitine needs from endogenous synthesis, in liver, kidney, brain and testis, and exogenous dietary sources mainly red meat and dairy products [20, 22]. In rats, the final enzyme in carnitine biosynthetic pathway, γ-butyrobetaine hydroxylase, is found primarily in liver [20, 22]. The effect of L carnitine on long-chain fatty acid oxidation in the heart depends on its intracellular concentration which itself dependent on the activity of organic cation/carnitine transporter (OCTN2). Organic cation/carnitine transporter is sodium-dependent and high-affinity carnitine transporter which mediates carnitine transport across the plasma membrane into the cells and serves to maintain carnitine levels in serum by functioning as a reabsorption transporter of carnitine in proximal tubules after glomerular filtration [20, 23, 24]. Several studies reported that CP and IFO therapy is associated with increased secretion of carnitine derivatives in the urine with subsequent secondary deficiency of the molecule [8, 19, 25–29]. Visarius et al. reported that chloroacetaldehyde (CAA) and thiodiglycolic acid (TDGA), the two major toxic metabolites of oxazaphosphorines, inhibit the oxidation of long-chain fatty acids (carnitine dependent) but not medium chain-fatty acids (carnitine independent) indicating that these compounds either sequester carnitine or inhibit carnitine palmitoyl transferase system [25, 27]. Marthaler et al. was the first to report that IFO therapy is associated with 10-fold increase in urinary carnitine excretion [26]. Using an animal model of carnitine deficiency, recent studies in our laboratory reported, for the first time, that both IFO and CP are associated with severe cardiotoxicity secondary to the increase in urinary losses of carnitine and the decrease in myocardial carnitine content, intramitochondrial CoA-SH and ATP production [8, 19]. In rat kidney tissues, carnitine deficiency and energy starvation were reported to constitute risk factors and should be viewed as a mechanism during CP-induced nephrotoxicity in rats [29]. Recently, it has been demonstrated that carnitine supplementation prevents the development of IFO-induced Fanconi syndrome by increasing intracellular carnitine content and intramitochondrial CoA-SH, with the consequent improvement in ATP production [30]. Recent in vitro study by Ciarimboli et al. has demonstrated, for the first time, that IFO but not CP is a substrate for OCTN2, which provide a cell-specific explanation for IFO-induced fanconi syndrome and offer a new potential target for selective protective interventions in cancer treatment with oxazaphosphorines [31]. Although we have previously reported that CP and IFO induce its organ toxicity by altering carnitine and energy status in mitochondria [8, 19, 30], no mechanism for these effects has been ascertained. Accordingly, the current study has been initiated to investigate whether oxazaphosphorines therapy alters the expression of OCTN2 gene in cardiac and kidney tissues, and if so, whether these alterations contribute to oxazaphosphorines-induced cardiotoxicity.
2. Materials and Methods
2.1. Materials
Endoxan and Holoxan vials (Baxter oncology GmbH, Germany) were gifted from King Khalid University Hospital drug store, King Saud University, Kingdom of Saudi Arabia. Each Endoxan vial contains 500 mg CP, whereas each Holoxan vial contains 1 g IFO in a dry lyophilized powder form. The content of each vial was freshly dissolved in sterile water for injection immediately before injection. L carnitine was kindly supplied by Dr. Zaven Orfalian, Sigma-Tau Pharmaceuticals, Pomezia, Italy. It has been supplied as white powder in a noncommercial plastic bottles contains 100 g, and it was freshly dissolved in normal saline prior to injection. Primers and probes were designed using Primer Express 3.0 (Applied biosystem, USA) and purchased from Metabion International AG (Germany). OCTN2 and GAPDH monoclonal antibodies have been purchased from Santa Cruz biotechnology, Inc. (Heidelberg, Germany). All other chemicals used were of the highest analytical grade.
2.2. Animals
Adult male Wistar albino rats, weighing 180–200 g, were obtained from the Animal Care Center, College of Pharmacy, King Saud University, Riyadh, Kingdom of Saudi Arabia and were housed in metabolic cages under controlled environmental conditions (25°C and a 12 h light/dark cycle). Animals had free access to pulverized standard rat pellet food and tap water. The protocol of this study has been approved by Research Ethics Committee of College of Pharmacy, King Saud University, Riyadh, Kingdom of Saudi Arabia.
2.3. Experimental Design
To achieve the ultimate goals of this study, a total of 60 adult male Wistar albino rats were used and divided at random into 6 groups of 10 animals each. Rats of group 1 (control group) were received I.P. injection of normal saline (2.5 mL/kg/day) for 10 successive days. Animals in group 2 (carnitine-supplemented group) were given L carnitine (200 mg/kg/day, I.P.) for 10 successive days as previously described [30]. Animals in group 3 (CP group) were received normal saline for 5 days before and 5 days after a single dose of CP (200 mg/kg/I.P.) according to previously published studies [4, 8, 17]. Rats of group 4 (IFO group) were received normal saline for 5 successive days followed by IFO (50 mg/kg/day, I.P.) for 5 successive days according to Sayed-Ahmed et al. [19]. Rats of group 5 (CP-carnitine supplemented rats) were given the same doses of L carnitine as group 2 for 5 days before and 5 days after a single dose of CP as group 3 according to Fatani et al. [8]. Rats of group 6 (IFO-carnitine supplemented rats) were given the same doses of L carnitine as group 2 for 5 days before and 5 days concomitant with IFO as group 4 according to Sayed-Ahmed [30]. Immediately after the last dose of the treatment protocol, 24-hour urine was collected for monitoring urinary carnitine excretion. Animals were then sacrificed by decapitation after exposure to ether in a dessicator kept in a well-functioning hood, and blood samples were obtained. Serum was separated for measurement of serum lactate dehydrogenase (LDH), creatine phosphokinase iso-enzyme (CK-MB) and acyl-carnitine (AC)/free carnitine (FC) ratio. Hearts were quickly excised for measurement of total carnitine and mRNA expression of OCTN2, GPx, and SOD genes. Kidneys were also isolated for quantification of mRNA expression of OCTN2 gene. Moreover, protein expression of OCTN2 was measured in heart and kidney tissues.
2.4. Methods
2.4.1. Quantification of mRNA Expression by Real-Time Polymerase Chain Reaction
Total RNA Extraction —
Total RNA was extracted from heart and kidney tissues by Trizol method according to the standard protocol as previously described [32]. Briefly, RNA was extracted by homogenization (Polytron; Kinematica, Lucerne, Switzerland) in TRIzol reagent (Gibco BRL) at maximum speed for 90–120 s. The homogenate was incubated for 5 min at room temperature. A 1 : 5 volume of chloroform was added, and the tube was vortexes and subjected to centrifugation at 12,000 g for 15 min. The aqueous phase was isolated, and the total RNA was precipitated by absolute ethanol. After centrifugation and washing the total RNA was finally eluted in 20 μL of diethyl pyrocarbonate-treated water. The quantity was characterized using a UV spectrophotometer (NanoDrop 8000, Thermo Scientific, USA). The isolated RNA has a 260/280 ratio of 1.9–2.1.
First-Strand cDNA Synthesis Using SuperScript II RT —
First-strand cDNA was synthesized from 1 μg of total RNA by reverse transcription with a SuperScript first-strand synthesis system kit (Invitrogen, CA, USA), according to the manufacturer's instructions.
Real Time PCR —
Real-time reaction was performed using the KAPA PROBE FAST qPCR kit master mix (KAPA Biosysems, USA) and the 2-ΔΔCt method. GAPDH gene was used as the endogenous control. PCR assay was optimized by varying the PCR conditions such as the concentration of cDNA, primers and probes, amplification cycle number, and annealing temperature. Briefly, a standard 25 μL reaction mixture has contained in final concentration of 1x KAPA PROBE FAST qPCR master mix buffer, 0.4 μM of each forward and reverse primers, 0.2 μM Probe for OCTN2, GPx, SOD and GAPDH (Table 1), 100 ng of cDNA and RNase, and DNase-free water. The reaction was done in an ABI 96-well optical reaction plate placed on ice before cDNA template was added. The standard thermal cycling conditions of initial 50°C for 2 min and 95°C for 10 min followed by 40 cycles at 95°C for 15 second and 60°C for 1 min were used. All reactions were performed using an ABI 7500 System (Applied Biosystem, USA). Experiments were performed in triplets for all data points. Each qPCR reaction included no-template controls.
Table 1.
Primers and probe sequence of the OCTN2, GPx, SOD, and GAPDH genes.
| Gene name | Forward primer | Reverse primer | Probe |
|---|---|---|---|
| OCTN2 | 5-GCGCCTTCCACTATCTTCGA-3 | 5-TTCGTGTTCGGACCAGATCA-3 | FAM-TCCAAGAAGCCTCAGTCGCACCACA-TAMRA |
| GAPDH | 5′-TGGCCTCCAAGGAGTAAGAAAC-3′ | 5′-GGCCTCTCTCTTGCTCTCAGTATC-3′ | FAM-CTGGACCACCCAGCCCAGCAA-TAMRA |
| GPx | 5′-GGTGTTCCAGTGCGCAGAT-3′ | 5′-GGGCTTCTATATCGGGTTCGA-3′ | VIC-CAGCAGGCGCTTTCGCACCAT-TAMRA |
| SOD | 5′-CCACTGCAGGACCTCATTTTAAT-3′ | 5′-TCTCCAACATGCCTCTCTTCATC-3′ | VIC-CTCACTCTAAGAAACATGGCGGTCCAGC-TAMRA |
2.4.2. Western Blot Analysis of OCTN2 Protein
For western blot analysis, heart and kidney tissues were washed with ice-cold PBS, and the protein extracts were prepared using ice-cold cell lysis buffer supplemented with protease inhibitor cocktail (IBI SCIENTIFIC, Peosta, USA). Protein concentrations were measured using the Bradford assay (Bio-Rad, CA, USA) according to manufacturer's protocol. Proteins were separated on 10% sodium dodecyl sulfate-polyacrylamide (SDS-PAGE) gels and transferred to a nitrocellulose membrane. The membrane was blocked with 5% skimmed milk in TBS-T (10 mM Tris-HCl, 150 mM NaCl, 0.25% Tween 20, pH 7.5) at room temperature for 2 h followed by incubation with primary antibody for OCTN2 and GAPDH in TBS and 5% skimmed milk overnight at 4°C. After washing, the membrane was incubated with horseradish peroxidase (HRP) labeled secondary antibody in TBS-T buffer for 2 h at room temperature, followed by three washes with TBS-T. The detection was performed using chemiluminescence assay (Amersham, GE Healthcare, life science, UK). Membranes were exposed to X-ray film to observe the bands (Kodak, Rochester, NY, USA). Protein bands were quantified using the Kodak Scientific ID software.
2.4.3. Assessment of Serum Creatine Kinase (CK-MB) and Lactate Dehydrogenase (LDH) Activity
Serum activities of LDH and CK-MB were determined according to the methods of Buhl and Jackson [33] and Wu and Bowers Jr [34], respectively.
2.4.4. Determination of Carnitine Levels in Serum, Urine, and Cardiac Tissues
Carnitine concentrations were determined in serum, urine, and cardiac tissues according to the method reported by Prieto et al. [35]. In brief, carnitine reacts with acetyl-CoA-forming acetylcarnitine in a reaction mediated by carnitine acetyltransferase enzyme. The liberated CoA-SH reacts with 5,5-dithiobis-(2-nitrobenzoic acid) forming thiophenolate ion, whose generation is proportional to the amount of carnitine and can be measured spectrophotometrically at 412 nm. Serum, urine, and heart tissues were deproteinized with equal volume of ice-cold 0.6 M perchloric acid and allowed to stand in an ice bath for 10 min. The mixture was centrifuged at 1000 ×g at 4°C for 5 min. The supernatant was used directly for measuring free carnitine after neutralization with 1.2 M potassium carbonate. For the assay of total carnitine, a part of supernatant was mixed with 1 M KOH and incubated at 37°C for 20 min for the hydrolysis of acylcarnitines. Carnitine level was computed from a calibration curve for carnitine hydrochloride.
2.5. Statistical Analysis
Differences between obtained values (mean ± SEM, n = 10) were carried out by one-way analysis of variance (ANOVA) followed by the Tukey-Kramer multiple comparison test. P ≤ 0.05 was taken as a criterion for a statistically significant difference.
3. Results
Figure 1 shows the effects of oxazaphosphorines, L carnitine, and their combination on cardiotoxicity enzymatic indices, CK-MB (a) and LDH (b), in rats. Administration of a single dose of CP (200 mg/kg) resulted in a significant 77 and 92% increase in serum CK-MB and LDH, respectively, as compared to the control group. Treatment with L carnitine (200 mg/kg/day) for 10 successive days showed non significant changes. Interestingly, administration of L carnitine for 5 days before and 5 days after a single dose of CP resulted in a complete reversal of CP-induced increase in serum CK-MB and LDH to the control values. On the other hand, administration of IFO (50 mg/kg/day) for 5 successive days resulted in 52 and 67% increase in serum CK-MB and LDH, respectively, as compared to the control group. Carnitine supplementation by daily administration of L carnitine for 5 days before and 5 days concomitant with IFO resulted in a complete reversal of IFO-induced increase in serum CK-MB and LDH to the control values.
Figure 1.
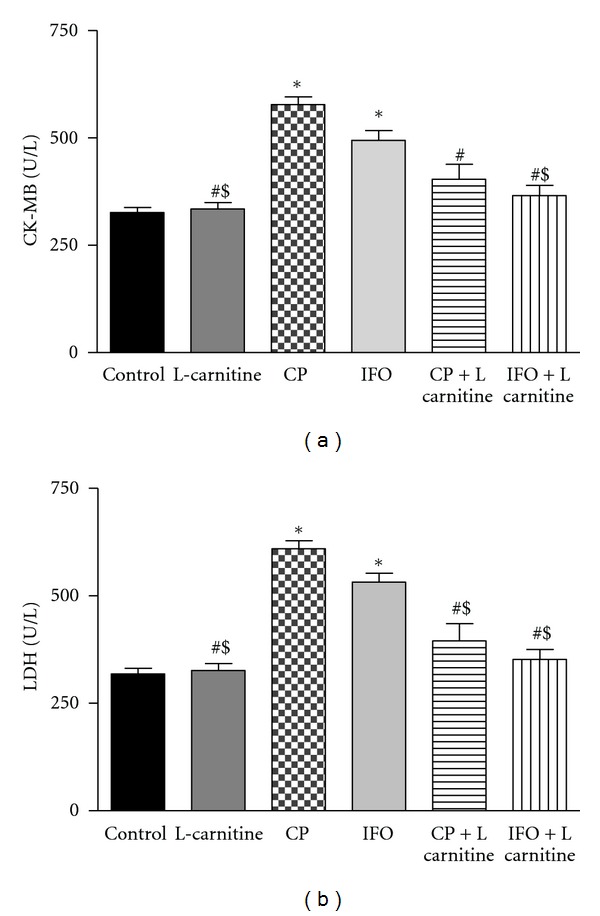
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on serum cardiotoxicity enzymatic indices, CK-MB (a) and LDH (b), in rats. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, cardiac enzymes were measured in serum. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
To investigate the effects of oxazaphosphorines on myocardial carnitine transport, the mRNA and protein expression of OCTN2 was measured in cardiac tissues using RT-PCR and western blot analysis, respectively (Figure 2). Treatment with either CP or IFO significantly decreased the expression of OCTN2 on the mRNA (a) and protein (b) levels in cardiac tissues. A significant 50 and 82% decrease in mRNA expression was obtained after CP and IFO, respectively, as compared to the control group. Similarly, CP and IFO significantly decreased OCTN2 protein expression by 54 and 60%, respectively, as compared to the control group. Daily administration of L carnitine alone for 10 successive days resulted in a significant 33% increase in OCTN2 expression as compared to the control. Interestingly, administration of L carnitine for 5 days before and 5 days after a single dose of CP resulted in a complete reversal of CP-induced decrease in OCTN2 mRNA and protein expression to the control values. Conversely, administration of L carnitine to IFO-treated rats did not affect IFO-induced decrease of OCTN2 expression.
Figure 2.
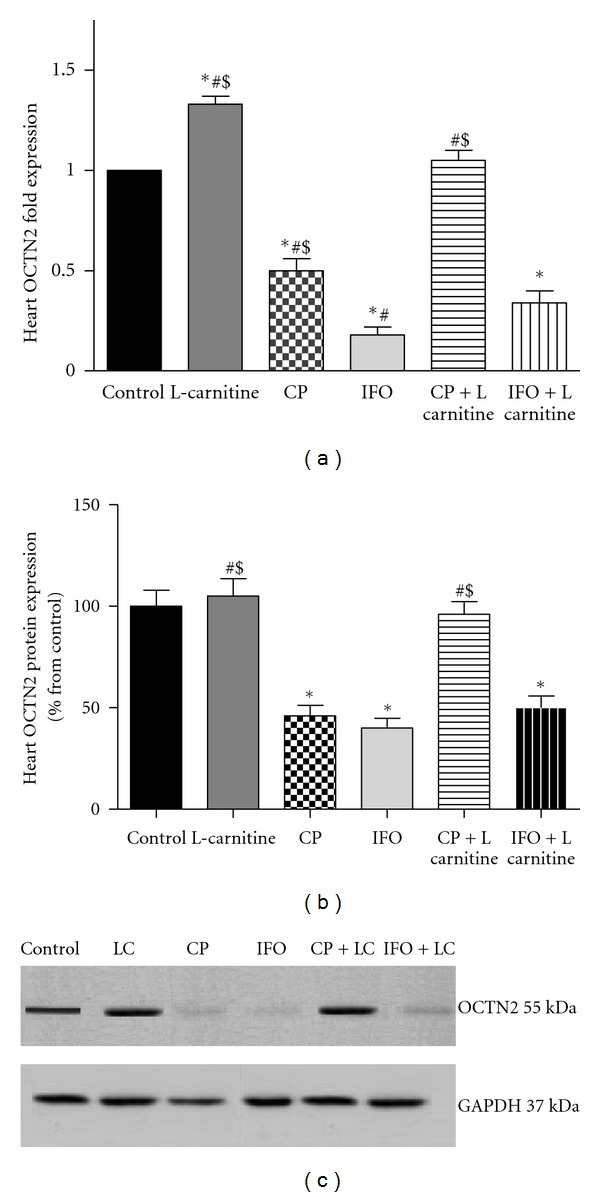
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on organic cation/carnitine transporter (OCTN2) mRNA (a) and protein (b) expression in rat heart tissues. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, total RNA and protein were isolated from heart tissues, then OCTN2 mRNA and protein expression was measured using RT-PCR and western blot analysis, respectively. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
Figure 3 shows the effects of oxazaphosphorines, L carnitine, and their combination on total carnitine levels in rat cardiac tissues. Administration of a single dose of CP and 5 doses of IFO resulted in a significant 52 and 41% decrease in total carnitine level in heart tissues, respectively, as compared to the control group. On the other hand, daily administration of L carnitine alone for 10 successive days resulted in a significant 47% increase as compared to the control rats. Interestingly, administration of L carnitine in combination with CP and IFO resulted in a complete reversal of the decrease in myocardial carnitine content, induced by CP and IFO, to the control values.
Figure 3.
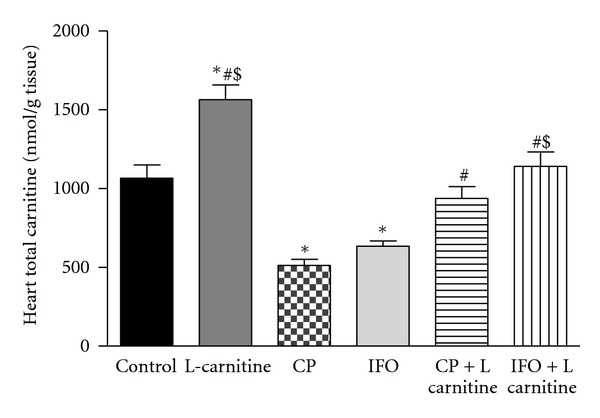
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on the levels of total carnitine in rat heart tissues. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented and IFO carnitine-supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, total carnitine was measured in heart tissues. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
Figure 4 shows the effects of oxazaphosphorines, L carnitine, and their combination on urinary carnitine excretion in rats. Treatment with a single dose of CP and 5 doses of IFO resulted in a significant 132 and 268% increase in carnitine excretion, respectively, as compared to the control group. On the other hand, daily administration of L carnitine alone for 10 successive days resulted in nonsignificant change in urinary carnitine excretion. Interestingly, administration of L carnitine in combination with CP and IFO resulted in a complete reversal of the increase in carnitine excretion, induced by CP and IFO, to the control values. To explain the effects of oxazaphosphorines on carnitine reabsorption/secretion rate, the mRNA and protein expression of OCTN2 gene was measured in kidney tissues using RT-PCR and western blot analysis, respectively (Figure 5). Administration of either CP or IFO alone significantly decreased the expression of OCTN2 on the mRNA (a) and protein (b) levels in kidney tissues. A significant 32 and 87% decrease were obtained after CP and IFO, respectively, as compared to the control group. Similarly, CP and IFO significantly decreased OCTN2 protein expression by 45 and 57%, respectively, as compared to the control group. Daily administration of L carnitine alone for 10 successive days resulted in nonsignificant change in OCTN2 mRNA and protein expression. Interestingly, administration of L carnitine for 5 days before and 5 days after a single dose of CP resulted in a complete reversal of CP-induced decrease in OCTN2 mRNA and protein expression to the control values. Conversely, administration of L carnitine to IFO-treated rats did not affect IFO-induced decrease of OCTN2 expression.
Figure 4.
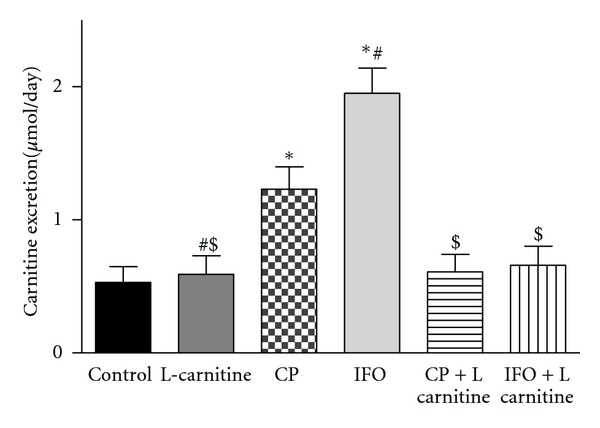
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC) and their combination on urinary carnitine excretion in rats. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented, and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). Immediately after the last dose of the treatment protocol, 24 hour-urine was collected for monitoring urinary carnitine excretion. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
Figure 5.
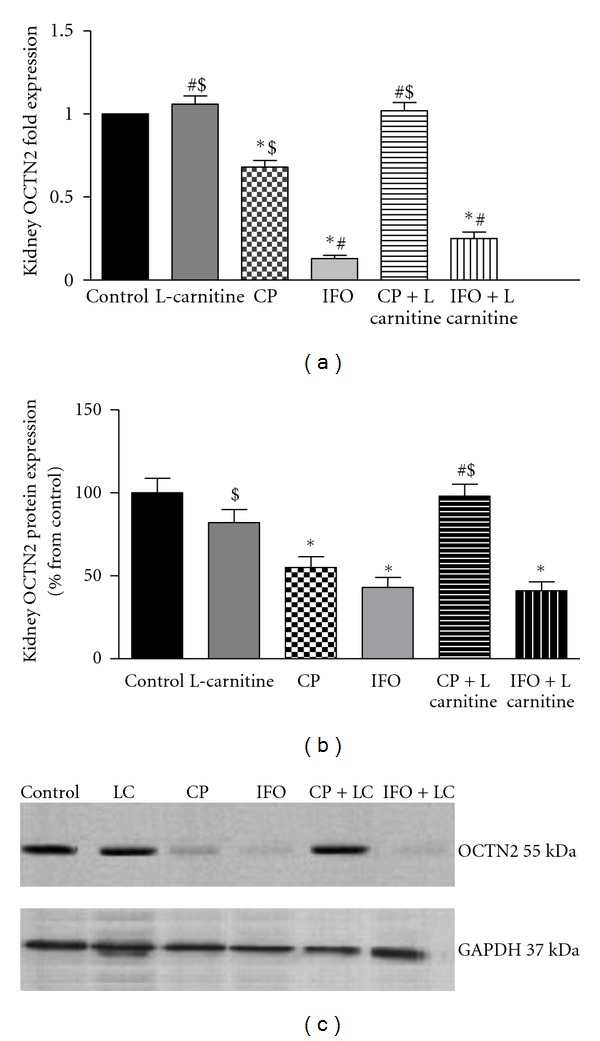
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on organic cation/carnitine transporter (OCTN2) mRNA (a) and protein (b) expression in rat kidney tissues. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, total RNA and protein were isolated from kidney tissues, then OCTN2 mRNA and protein expression was measured using RT-PCR and western blot analysis, respectively. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
To investigate whether oxazaphosphorines therapy is associated with carnitine insufficiency, AC/FC ratio was measured in serum from treated rats (Figure 6). Administration of a single dose of CP (200 mg/kg) and IFO (50 mg/kg/day) for 5 successive days resulted in a significant 183 and 186% increase in serum AC/FC ratio, respectively, as compared to the control group. The normal value for AC/FC is less than 0.4. CP treatment increased AC/FC ratio up to 1.02, whereas IFO increased AC/FC ratio up to 1.03 indicating a state of carnitine insufficiency. On the other hand, daily administration of L carnitine alone for 10 successive days resulted in nonsignificant change in AC/FC. Interestingly, administration of L carnitine in combination with CP or IFO resulted in a complete reversal of the increase in AC/FC, induced by CP and IFO, to the control values.
Figure 6.
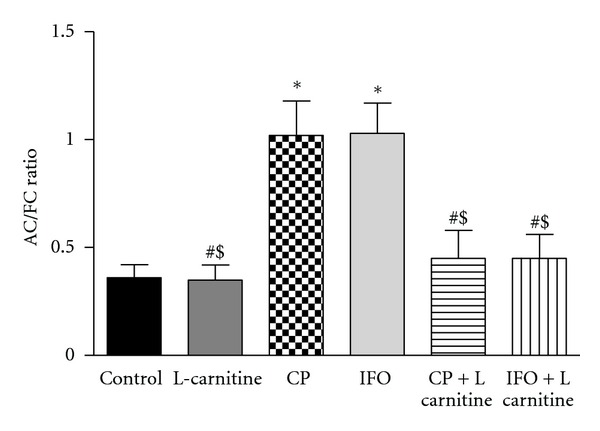
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on serum acyl-carnitine (AC)/free carnitine (FC) ratio in rats. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented, and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, serum was separated, and AC/FC was measured in serum. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
To investigate the effects of oxazaphosphorines-induced oxidative stress, the expression levels of GPx and SOD were measured in heart tissues using RT-PCR (Figure 7). Administration of either CP or IFO alone significantly decreased the expression of GPx (a) and SOD (b) mRNA in heart tissues. A significant 57 and 50% decrease in GPx and 60% decrease in SOD were obtained after CP and IFO treatment, respectively, as compared to the control group. Daily administration of L carnitine alone for 10 successive days resulted in nonsignificant change in the expression of both genes. However, administration of L carnitine to CP and IFO-treated rats completely normalized the decrease in antioxidant enzymes induced by CP and IFO to control values.
Figure 7.
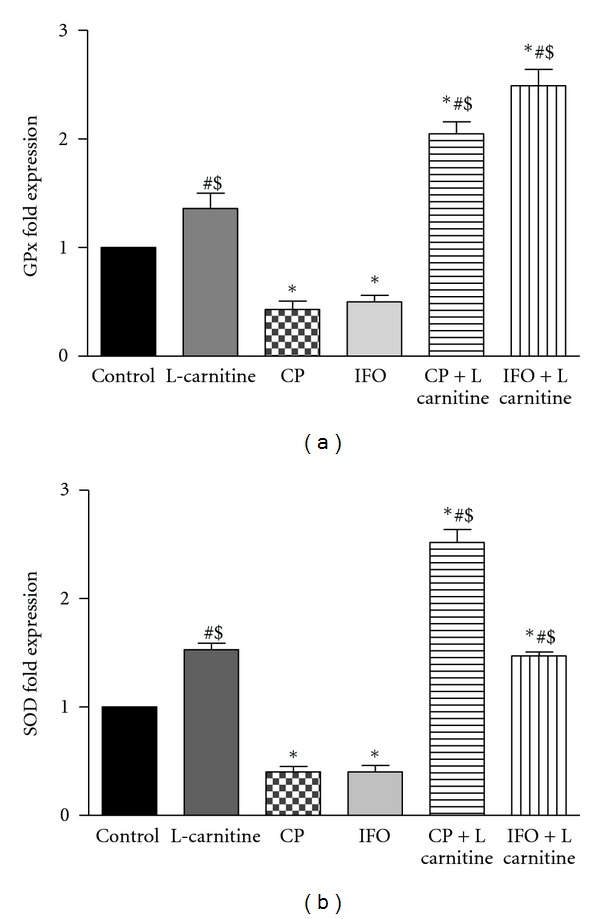
Effects of cyclophosphamide (CP), ifosfamide (IFO), L carnitine (LC), and their combination on glutathione peroxides (GPx) (a) and superoxide dismutase (SOD) (b) mRNA expression in rat heart tissues. Rats were randomly divided into 6 different groups of 10 animals each: control, L carnitine, CP, IFO, CP carnitine supplemented, and IFO carnitine supplemented. Carnitine supplementation was induced in rats by daily intraperitoneal injection of L carnitine (200 mg/kg/day) for 10 successive days. CP cardiotoxicity was induced in rats by administration of a single dose of CP (200 mg/kg). IFO cardiotoxicity was induced in rats by administration of IFO (50 mg/kg/day, I.P.) for 5 successive days. CP-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days after a single dose of CP (200 mg/kg). IFO-carnitine-supplemented rats were given the same doses of L carnitine (200 mg/kg/day) for 5 days before and 5 days concomitant with IFO (50 mg/kg/day, I.P.). At the end of the treatment protocol, total RNA was isolated from heart tissues and GPx and SOD mRNA expression was measured using RT-PCR. Data are presented as mean ± S.E.M. (n = 10). *, #, and $ indicate significant change from control, CP and IFO, respectively, at P < 0.05 using ANOVA followed by Tukey-Kramer as a post-ANOVA test.
4. Discussion
It is well documented, on the experimental and clinical levels, that administration of high therapeutic doses of CP and IFO is associated with cardiotoxicity [3, 4, 7, 9–12, 14–17]. Although cardiotoxicity is related to dosage, previous anthracycline and thoracic irradiation-based regimen, age, and the presence of left ventricular dysfunction, no definitive risk factors in CP- and IFO-induced cardiotoxicity have yet been identified. Recent studies in our laboratory has demonstrated, for the first time, that carnitine deficiency and energy starvation provoke CP and IFO-induced acute cardiotoxicity and nephropathy in rats [8, 19, 29, 30]. However, up to date in the literature, we could not find any study investigating the molecular mechanism whereby CP and IFO induce secondary carnitine deficiency. Taken together, this prompted us to investigate, for the first time, whether CP and IFO alter the expression of OCTN2 gene in cardiac and kidney tissues, and, if so, whether these alterations contribute to CP and IFO-induced cardiotoxicity.
Under normal physiological conditions, L carnitine is highly conserved since 95% of the filtered L carnitine is reabsorbed at the proximal tubular level by specific sodium-dependent, high affinity OCTN2 [23]. In the current study, the observed decrease in cardiac carnitine content following oxazaphosphorines therapy could be due to the inhibition of endogenous synthesis and/or inhibition of tubular reabsorption of carnitine. Since kidney is one of major sites for endogenous carnitine biosynthesis, and 95% of filtered carnitine is reabsorbed by the proximal tubules of the nephron [23]; therefore, oxazaphosphorine-induced acute nephropathy may lead to inhibition of endogenous carnitine biosynthesis and increases its urinary losses with the consequent secondary deficiency of the molecule [29, 30]. This is in line with current data which showed that urinary carnitine excretion was increased by administration of CP and IFO. This hypothesis is in line with the only clinical study performed on 5 patients with advanced soft tissue sarcoma and reported that IFO-increased urinary carnitine excretion by factor of 10 [26]. Several studies have reported that increased urinary excretion of carnitine should be viewed as an early marker in chemotherapy-induced nephrotoxicity [36–38].
In the current study, the observed decrease in cardiac carnitine content by CP and IFO treatment was parallel to the increase in serum AC/FC and urinary carnitine excretion, indicating an impaired uptake of carnitine by cardiac myocytes. The most important carrier in carnitine uptake is the OCTN2. Physiologically OCTN2 is involved in the intestinal absorption, myocardial transport, and renal reabsorption of L carnitine and also plays a major role in tissue distribution. Variations in transport rates and in levels of expressed mRNA are also found in different tissues [39–41]. Data presented here clearly demonstrate that oxazaphosphorines markedly inhibited OCTN2 mRNA and protein expression in both heart and kidney tissues. This effect could be a secondary event following CP- and IFO-induced DNA double-strand break with the consequent inhibition of RNA and protein synthesis as a part of its cytotoxic mechanism. It appears that oxazaphosphorines-induced generation of free radicals, oxidative and nitrosative stress could be the cause of decreased OCTN2 mRNA expression [8, 17, 19, 30, 42]. In addition, OCTN2 is directly inhibited by a number of xenobiotics, including the antibiotic emetine and the ion channel blockers quintine and verapamil, zwitterionic compounds such as the b-lactam antibiotics cephaloridine, cefepime, ceftazidime, and cefluprenam [43, 44].
In the current study, the observed downregulation of OCTN2 mRNA expression was parallel to the progressive increase in cardiotoxicity enzymatic indices, LDH and CK-MB, which may point to the possible contribution of decreased expression of OCTN2 during development of oxazaphosphorines-induced cardiotoxicity. In our laboratory, decreased cardiac carnitine content following inhibition of OCTN2 mRNA expression has been reported in chronic doxorubicin cardiomyopathic rat model [45]. The possibility that there is a flux of carnitine from cytosol to extracellular through OCTN2 or membrane holes produced by CP and IFO actions cannot be ruled out. Depletion of the heart from carnitine by oxazaphosphorines would impair the beta-oxidation of long-chain fatty acids with the consequent decrease in ATP production which renders the cardiac cells vulnerable to damage by oxazaphosphorines with the consequent leakage of cardiac enzymes. This was supported by the marked decrease of ATP levels in heart tissues and the marked increase in cardiac enzymes observed after treatment with both CP and IFO [8, 17, 19, 46].
Under our experimental condition, carnitine supplementation completely restored CP but not IFO-induced inhibition of OCTN2 mRNA expression in both heart and kidney tissues to its normal values. Our results are consistent with the recent in vitro study on human kidney cells which has demonstrated, for the first time, that IFO but not CP is a substrate for OCTN2, which provide a cell-specific explanation for IFO but not CP-induced fanconi syndrome and offer a new potential target for selective protective interventions in cancer treatment with oxazaphosphorines [31]. Authors added that coadministration of cimetidine, a known competitive substrate of human OCTN2, completely prevented this IFO-induced toxicity [31]. Therefore, it seems that IFO produced irreversible inhibition of OCTN2 mRNA expression and that carnitine has nothing to do with the inhibition of OCTN2 mRNA expression by IFO. However, it remains unclear why L carnitine normalized cardiac carnitine content and urinary carnitine excretion in IFO-treated rats despite irreversible inhibition of OCTN2 expression. A possible explanation for this is that carnitine supplementation for 10 days will increase the extracellular concentration of L carnitine that might enter the cells, under this condition, by simple diffusion independent of its carrier, OCTN2. Moreover, L carnitine through its previously reported antioxidant defense against generation of reactive oxygen species (ROS) [47–50] could protect against CP-induced inhibition of OCTN2 mRNA expression in cardiac and kidney tissues. Carnitine has a protective effect on lipid peroxidation by reducing the formation of hydrogen peroxide [51, 52] and is associated with buffering of excess acyl-CoA, which is potentially toxic to the cells. It also improved the antioxidant status in rats and showed free radical scavenging activity as well [53]. In addition, L carnitine prevents the accumulation of free fatty acids and their toxic intermediates, thus preventing their harmful effects on mitochondrial and cell membranes [53]. The protective effect of L carnitine on kidney and heart tissues has been proved in some models involving oxidative stress [54, 55].
It is well documented that L carnitine performs a crucial role in the energy production in the heart by controlling the influx of long-chain fatty acids into mitochondria [56]. The total body content of carnitine in adults amounts to 50–100 mmol, most of it being localized in skeletal muscles [26]. Carnitine is present in both plasma and tissue as FC or bound to fatty acids as AC with relatively high concentration in cardiac tissues [57]. Under normal physiological conditions, 80% of total serum carnitine is FC, and 20% is AC with normal AC/FC ratio of 0.25 [58, 59]. Earlier studies reported that increased ratio of AC/FC greater than 0.4 is abnormal and creates a pathological condition known as carnitine insufficiency in which there is insufficient FC relative to increased metabolic needs [58–60]. Moreover, it has been reported that AC/FC ratio is very sensitive to metabolic changes and equals to the intramitochondrial acyl-CoA/CoA-SH ratio [60].
In this study, oxazaphosphorine therapy increased serum AC/FC ratio although serum total carnitine is not changed by CP and IFO as previously reported in our laboratory [8, 19]. This effect could be a consequence of carnitine insufficiency when esterified carnitine is exported out of the mitochondria. Previous study reported that increased serum AC could indicate impaired transport of long-chain fatty acids into mitochondria and abnormal beta-oxidation pathway [58]. Moreover, the observed increase in serum AC/FC ratio by oxazaphosphorines was parallel to the increase in cardiotoxicity enzymatic indices, LDH and CK-MB, which may point to the possible consideration of serum AC/FC ratio as an index of oxazaphosphorines-induced acute cardiotoxicity. It is well known that L carnitine is an essential cofactor for mitochondrial transport and oxidation of long-chain fatty acids which are the preferred substrates for ATP production in normal, well-oxygenated adult myocardium [61].
Damage, at the cellular level by oxidants, is attenuated by antioxidant enzymes such as SOD, GPx, and catalase [62]. In the current study, oxazaphosphorines significantly decreased the expression of GPx and SOD in heart tissues. Cardiotoxicity secondary to the decrease in antioxidant capacity of the heart is caused by extensive range of anticancer agents such as CP and IFO [19, 63]. Increased generation of ROS by CP [7, 64] and IFO [19] may cause membrane injury by increased lipid peroxidation associated with decline in the activities of cellular antioxidants [65]. Superoxide dismutase is one of the major enzymatic antioxidant mechanisms against superoxide radical and prevents heart toxicity induced by oxazaphosphorines [46]. Data presented here showed that CP and IFO decreased the expression of SOD and GPx which is reversed by carnitine supplementation. The antioxidant activity of L carnitine and its natural short-chain derivatives has been previously reported [13, 16, 22, 25]. Our results are in good agreement with several authors who demonstrated that oxazaphosphorines induce its cardiotoxicity via increasing the generation of ROS and decreasing the activity and expression of antioxidant enzymes in cardiac tissues [7, 19, 63].
5. Conclusions
Data from this study suggest that (1) oxazaphosphorines decreased myocardial carnitine content following the inhibition of OCTN2 mRNA and protein expression in cardiac tissues. (2) Oxazaphosphorines therapy increased urinary loss of carnitine secondary to the inhibition of OCTN2 mRNA and protein expression in proximal tubules of the kidney. (3) The progressive increase in cardiotoxicity enzymatic indices and the decrease in OCTN2 mRNA expression may point to the possible contribution of OCTN2 as a mechanism during development of oxazaphosphorines-induced cardiotoxicity. (4) Serum AC/FC ratio should be viewed as an index of oxazaphosphorines-induced acute cardiotoxicity. (5) Carnitine supplementation attenuates CP but not IFO-induced inhibition of OCTN2 expression in heart and kidney tissues. L carnitine is a leading candidate and should be given along with oxazaphosphorines-based chemotherapy to block their multiple organ toxicity and to permit larger doses of these drugs to be administered, thereby killing more cancer cells and increasing the chances of patient survival.
Conflict of Interests
All authors declare that there is no conflict of interests.
Acknowledgments
The present work was supported by operating grant from the National Plan for Science and Technology, King Saud University (09-BIO939-02).
References
- 1.Shore S. Review of the nitrogen mustards. Hahnemann Monthly. 1947;82(11):461–470. [PubMed] [Google Scholar]
- 2.Baumann F, Preiss R. Cyclophosphamide and related anticancer drugs. Journal of Chromatography B. 2001;764(1-2):173–192. doi: 10.1016/s0378-4347(01)00279-1. [DOI] [PubMed] [Google Scholar]
- 3.Shanholtz C. Acute life-threatening toxicity of cancer treatment. Critical Care Clinics. 2001;17(3):483–502. doi: 10.1016/s0749-0704(05)70196-2. [DOI] [PubMed] [Google Scholar]
- 4.Mythili Y, Sudharsan PT, Selvakumar E, Varalakshmi P. Protective effect of DL-α-lipoic acid on cyclophosphamide induced oxidative cardiac injury. Chemico-Biological Interactions. 2004;151(1):13–19. doi: 10.1016/j.cbi.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Morandi P, Ruffini PA, Benvenuto GM, Raimondi R, Fosser V. Cardiac toxicity of high-dose chemotherapy. Bone Marrow Transplantation. 2005;35(4):323–334. doi: 10.1038/sj.bmt.1704763. [DOI] [PubMed] [Google Scholar]
- 6.Katayama M, Imai Y, Hashimoto H, et al. Fulminant fatal cardiotoxicity following cyclophosphamide therapy. Journal of Cardiology. 2009;54(2):330–334. doi: 10.1016/j.jjcc.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Todorova V, Vanderpool D, Blossom S, et al. Oral glutamine protects against cyclophosphamide-induced cardiotoxicity in experimental rats through increase of cardiac glutathione. Nutrition. 2009;25(7-8):812–817. doi: 10.1016/j.nut.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Fatani AG, Darweesh AQ, Rizwan L, Aleisa AM, Al-Shabanah OA, Sayed-Ahmed MM. Carnitine deficiency aggravates cyclophosphamide-induced cardiotoxicity in rats. Chemotherapy. 2010;56(1):71–81. doi: 10.1159/000298822. [DOI] [PubMed] [Google Scholar]
- 9.Mills BA, Roberts RW. Cyclophosphamide-induced cardiomyopathy. A report of two cases and review of the English literature. Cancer. 1979;43(6):2223–2226. doi: 10.1002/1097-0142(197906)43:6<2223::aid-cncr2820430610>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg MA, Antin JH, Guinan EC, Rappeport JM. Cyclophosphamide cardiotoxicity: an analysis of dosing as a risk factor. Blood. 1986;86(5):1114–1118. [PubMed] [Google Scholar]
- 11.Gottdiener JS, Appelbaum FR, Ferrans VJ. Cardiotoxicity associated with high-dose cyclophosphamide therapy. Archives of Internal Medicine. 1981;141(6):758–763. [PubMed] [Google Scholar]
- 12.Steinherz LJ, Steinherz PG, Mangiacasale D. Cardiac changes with cyclophosphamide. Medical and Pediatric Oncology. 1981;9(5):417–422. doi: 10.1002/mpo.2950090502. [DOI] [PubMed] [Google Scholar]
- 13.Nicolini A, Mancini PA, Ferrari P, et al. Oral low-dose cyclophosphamide in metastatic hormone refractory prostate cancer (MHRPC) Biomedicine and Pharmacotherapy. 2004;58(8):447–450. doi: 10.1016/j.biopha.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Kandylis K, Vassilomanolakis M, Tsoussis S, Efremidis AP. Ifosfamide cardiotoxicity in humans. Cancer Chemotherapy and Pharmacology. 1989;24(6):395–396. doi: 10.1007/BF00257451. [DOI] [PubMed] [Google Scholar]
- 15.Quezado ZMN, Wilson WH, Cunnion RE, et al. High-dose ifosfamide is associated with severe, reversible cardiac dysfunction. Annals of Internal Medicine. 1993;118(1):31–36. doi: 10.7326/0003-4819-118-1-199301010-00006. [DOI] [PubMed] [Google Scholar]
- 16.Buckner C, Rudolph R, Fefer A, et al. High-dose cyclophosphamide therapy for malignant disease. Toxicity, tumor response, and the effects of stored autologous marrow. Cancer. 1972;29:357–365. [Google Scholar]
- 17.Nagi MN, Al-Shabanah OA, Hafez MM, Sayed-Ahmed MM. Thymoquinone supplementation attenuates cyclophosphamide-induced cardiotoxicity in rats. Journal of Biochemical and Molecular Toxicology. 2011;25(3):135–142. doi: 10.1002/jbt.20369. [DOI] [PubMed] [Google Scholar]
- 18.Sehirli O, Sakarcan A, Velioglu-Ogunc A, et al. Resveratrol improves ifosfamide-induced Fanconi syndrome in rats. Toxicology and Applied Pharmacology. 2007;222(1):33–41. doi: 10.1016/j.taap.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 19.Sayed-Ahmed MM, Darweesh AQ, Fatani AJ. Carnitine deficiency and oxidative stress provoke cardiotoxicity in an ifosfamide-induced Fanconi Syndrome rat model. Oxidative Medicine and Cellular Longevity. 2010;3(4):266–274. doi: 10.4161/oxim.3.4.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bremer J. Carnitine. Metabolism and functions. Physiological Reviews. 1983;63(4):1420–1480. doi: 10.1152/physrev.1983.63.4.1420. [DOI] [PubMed] [Google Scholar]
- 21.Kunau WH, Dommes V, Schulz H. β-oxidation of fatty acids in mitochondria, peroxisomes, and bacteria: a century of continued progress. Progress in Lipid Research. 1995;34(4):267–342. doi: 10.1016/0163-7827(95)00011-9. [DOI] [PubMed] [Google Scholar]
- 22.Vaz FM, Wanders RJA. Carnitine biosynthesis in mammals. Biochemical Journal. 2002;361(3):417–429. doi: 10.1042/0264-6021:3610417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamai I, Ohashi R, Nezu JI, et al. Molecular and functional identification of sodium ion-dependent, high affinity human carnitine transporter OCTN2. Journal of Biological Chemistry. 1998;273(32):20378–20382. doi: 10.1074/jbc.273.32.20378. [DOI] [PubMed] [Google Scholar]
- 24.Maeda T, Wakasawa T, Funabashi M, et al. Regulation of Octn2 transporter (SLC22A5) by peroxisome proliferator activated receptor alpha. Biological and Pharmaceutical Bulletin. 2008;31(6):1230–1236. doi: 10.1248/bpb.31.1230. [DOI] [PubMed] [Google Scholar]
- 25.Visarius TM, Bähler H, Küpfer A, Cerny T, Lauterburg BH. Thiodiglycolic acid is excreted by humans receiving ifosfamide and inhibits mitochondrial function in rats. Drug Metabolism and Disposition. 1998;26(3):193–196. [PubMed] [Google Scholar]
- 26.Marthaler NP, Visarius T, Küpfer A, Lauterburg BH. Increased urinary losses of carnitine during ifosfamide chemotherapy. Cancer Chemotherapy and Pharmacology. 1999;44(2):170–172. doi: 10.1007/s002800050963. [DOI] [PubMed] [Google Scholar]
- 27.Visarius TM, Stucki JW, Lauterburg BH. Inhibition and stimulation of long-chain fatty acid oxidation by chloroacetaldehyde and methylene blue in rats. Journal of Pharmacology and Experimental Therapeutics. 1999;289(2):820–824. [PubMed] [Google Scholar]
- 28.Graziano F, Bisonni R, Catalano V, et al. Potential role of levocarnitine supplementation for the treatment of chemotherapy-induced fatigue in non-anaemic cancer patients. British Journal of Cancer. 2002;86(12):1854–1857. doi: 10.1038/sj.bjc.6600413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sayed-Ahmed MM. Progression of cyclophosphamide-induced acute renal metabolic damage in carnitine-depleted rat model. Clinical and Experimental Nephrology. 2010;14(5):418–426. doi: 10.1007/s10157-010-0321-0. [DOI] [PubMed] [Google Scholar]
- 30.Sayed-Ahmed MM. L-Carnitine attenuates ifosfamide-induced carnitine deficiency and decreased intramitochondrial CoA-SH in rat kidney tissues. Journal of Nephrology. 2011;24(4):490–498. doi: 10.5301/JN.2011.6447. [DOI] [PubMed] [Google Scholar]
- 31.Ciarimboli G, Holle SK, Vollenbröcker B, et al. New clues for nephrotoxicity induced by ifosfamide: preferential renal uptake via the human organic cation transporter 2. Molecular Pharmaceutics. 2011;8(1):270–279. doi: 10.1021/mp100329u. [DOI] [PubMed] [Google Scholar]
- 32.Chomczynski P. A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. BioTechniques. 1993;15(3):532–537. [PubMed] [Google Scholar]
- 33.Buhl SN, Jackson KY. Optimal conditions and comparison of lactate dehydrogenase catalysis of the lactate to pyruvate and pyruvate to lactate reactions in human serum at 25, 30, and 37°C. Clinical Chemistry. 1978;24(5):828–831. [PubMed] [Google Scholar]
- 34.Wu AHB, Bowers GN., Jr. Evaluation and comparison of immunoinhibition and immunoprecipitation methods for differentiating MB from BB and macro forms of creatine kinase isoenzymes in patients and healthy individuals. Clinical Chemistry. 1982;28(10):2017–2021. [PubMed] [Google Scholar]
- 35.Prieto JA, Andrade F, Aldámiz-Echevarría L, Sanjurjo P. Determination of free and total carnitine in plasma by an enzymatic reaction and spectrophotometric quantitation spectrophotometric determination of carnitine. Clinical Biochemistry. 2006;39(10):1022–1027. doi: 10.1016/j.clinbiochem.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 36.Heuberger W, Berardi S, Jacky E, Pey P, Krähenbühl S. Increased urinary excretion of carnitine in patients treated with cisplatin. European Journal of Clinical Pharmacology. 1998;54(7):503–508. doi: 10.1007/s002280050504. [DOI] [PubMed] [Google Scholar]
- 37.Mancinelli A, D’Iddio S, Bisonni R, Graziano F, Lippe P, Calvani M. Urinary excretion of l-carnitine and its short-chain acetyl-l-carnitine in patients undergoing carboplatin treatment. Cancer Chemotherapy and Pharmacology. 2007;60(1):19–26. doi: 10.1007/s00280-006-0341-3. [DOI] [PubMed] [Google Scholar]
- 38.Haschke M, Vitins T, Lüde S, et al. Urinary excretion of carnitine as a marker of proximal tubular damage associated with platin-based antineoplastic drugs. Nephrology Dialysis Transplantation. 2010;25(2):426–433. doi: 10.1093/ndt/gfp456. [DOI] [PubMed] [Google Scholar]
- 39.Ramsay RR, Gandour RD, van der Leij FR. Molecular enzymology of carnitine transfer and transport. Biochimica et Biophysica Acta. 2001;1546(1):21–43. doi: 10.1016/s0167-4838(01)00147-9. [DOI] [PubMed] [Google Scholar]
- 40.Lamhonwah AM, Skaug J, Scherer SW, Tein I. A third human carnitine/organic cation transporter (OCTN3) as a candidate for the 5q31 Crohn’s disease locus (IBD5) Biochemical and Biophysical Research Communications. 2003;301(1):98–101. doi: 10.1016/s0006-291x(02)02946-7. [DOI] [PubMed] [Google Scholar]
- 41.Xuan W, Lamhonwah AM, Librach C, Jarvi K, Tein I. Characterization of organic cation/carnitine transporter family in human sperm. Biochemical and Biophysical Research Communications. 2003;306(1):121–128. doi: 10.1016/s0006-291x(03)00930-6. [DOI] [PubMed] [Google Scholar]
- 42.Abraham P, Rabi S. Nitrosative stress, protein tyrosine nitration, PARP activation and NAD depletion in the kidneys of rats after single dose of cyclophosphamide. Clinical and Experimental Nephrology. 2009;13(4):281–287. doi: 10.1007/s10157-009-0160-z. [DOI] [PubMed] [Google Scholar]
- 43.Ganapathy ME, Huang W, Rajan DP, et al. β-Lactam antibiotics as substrates for OCTN2, an organic cation/carnitine transporter. Journal of Biological Chemistry. 2000;275(3):1699–1707. doi: 10.1074/jbc.275.3.1699. [DOI] [PubMed] [Google Scholar]
- 44.Wagner CA, Lükewille U, Kaltenbach S, et al. Functional and pharmacological characterization of human Na+-carnitine cotransporter hOCTN2. American Journal of Physiology. 2000;279(3):F584–F591. doi: 10.1152/ajprenal.2000.279.3.F584. [DOI] [PubMed] [Google Scholar]
- 45.Sayed-Ahmed MM, Al-Shabanah OA, Hafez MM, Aleisa AM, Al-Rejaie SS. Inhibition of gene expression of heart fatty acid binding protein and organic cation/carnitine transporter in doxorubicin cardiomyopathic rat model. European Journal of Pharmacology. 2010;640(1–3):143–149. doi: 10.1016/j.ejphar.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Asiri YA. Probucol attenuates cyclophosphamideinduced oxidative apoptosis, p53 and Bax signal expression in rat cardiac tissues. Oxidative Medicine and Cellular Longevity. 2010;3(5):308–316. doi: 10.4161/oxim.3.5.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fritz IB, Arrigoni-Martelli E. Sites of action of carnitine and its derivatives on the cardiovascular system: interactions with membranes. Trends in Pharmacological Sciences. 1993;14(10):355–360. doi: 10.1016/0165-6147(93)90093-y. [DOI] [PubMed] [Google Scholar]
- 48.Sayed-Ahmed MM, Shouman SA, Rezk BM, Khalifa MH, Osman AMM, El-Merzabani MM. Propionyl-L-carnitine as potential protective agent against adriamycin-induced impairment of fatty acid beta-oxidation in isolated heart mitochondria. Pharmacological Research. 2000;41(2):143–150. doi: 10.1006/phrs.1999.0583. [DOI] [PubMed] [Google Scholar]
- 49.Sayed-Ahmed MM, Khattab MM, Gad MZ, Mostafa N. L-carnitine prevents the progression of atherosclerotic lesions in hypercholesterolaemic rabbits. Pharmacological Research. 2001;44(3):235–242. doi: 10.1006/phrs.2001.0852. [DOI] [PubMed] [Google Scholar]
- 50.Al-Majed AA, Sayed-Ahmed MM, Al-Omar FA, Al-Yahya AA, Aleisa AM, Al-Shabanah OA. Carnitine esters prevent oxidative stress damage and energy depletion following transient forebrain ischaemia in the rat hippocampus. Clinical and Experimental Pharmacology and Physiology. 2006;33(8):725–733. doi: 10.1111/j.1440-1681.2006.04425.x. [DOI] [PubMed] [Google Scholar]
- 51.Augustyniak A, Skrzydlewska E. The influence of L-carnitine suplementation on the antioxidative abilities of serum and the central nervous system of ethanol-induced rats. Metabolic Brain Disease. 2010;25(4):381–389. doi: 10.1007/s11011-010-9217-7. [DOI] [PubMed] [Google Scholar]
- 52.Bodea F, Bocea A, Decea N. L-carnitine decreases oxidative stress induced by experimental hypobaric hypoxia. Pediatric Endocrinology, Diabetes, and Metabolism. 2010;16(2):78–81. [PubMed] [Google Scholar]
- 53.Liu J. The effects and mechanisms of mitochondrial nutrient α-lipoic acid on improving age-associated mitochondrial and cognitive dysfunction: an overview. Neurochemical Research. 2008;33(1):194–203. doi: 10.1007/s11064-007-9403-0. [DOI] [PubMed] [Google Scholar]
- 54.Chen HH, Sue YM, Chen CH, et al. Peroxisome proliferator-activated receptor alpha plays a crucial role in l-carnitine anti-apoptosis effect in renal tubular cells. Nephrology Dialysis Transplantation. 2009;24(10):3042–3049. doi: 10.1093/ndt/gfp258. [DOI] [PubMed] [Google Scholar]
- 55.Ozsoy SY, Ozsoy B, Ozyildiz Z, Aytekin I. Protective effect of L-carnitine on experimental lead toxicity in rats: a clinical, histopathological and immunohistochemical study. Biotechnic and Histochemistry. 2010;86(6):436–443. doi: 10.3109/10520295.2010.529825. [DOI] [PubMed] [Google Scholar]
- 56.Goa KL, Brogden RN. l-Carnitine: a preliminary review of its pharmacokinetics, and its therapeutic use in ischaemic cardiac disease and primary and secondary carnitine deficiencies in relationship to its role in fatty acid metabolism. Drugs. 1987;34(1):1–24. doi: 10.2165/00003495-198734010-00001. [DOI] [PubMed] [Google Scholar]
- 57.Luo X, Reichetzer B, Trines J, Benson LN, Lehotay DC. L-carnitine attenuates doxorubicin-induced lipid peroxidation in rats. Free Radical Biology and Medicine. 1999;26(9-10):1158–1165. doi: 10.1016/s0891-5849(98)00303-7. [DOI] [PubMed] [Google Scholar]
- 58.Campos Y, Huertas R, Lorenzo G, et al. Plasma carnitine insufficiency and effectiveness of L-carnitine therapy in patients with mitochondrial myopathy. Muscle and Nerve. 1993;16(2):150–153. doi: 10.1002/mus.880160205. [DOI] [PubMed] [Google Scholar]
- 59.Bohles H, Evangeliou A, Bervoets K, Eckert I, Sewell A. Carnitine esters in metabolic disease. European Journal of Pediatrics. 1994;153(1):S57–S61. doi: 10.1007/BF02138779. [DOI] [PubMed] [Google Scholar]
- 60.Winter SC, Zorn EM, Vance WH. Carnitine deficiency. Lancet. 1990;335(8695):981–982. [PubMed] [Google Scholar]
- 61.Neely JR, Morgan HE. Relationship between carbohydrate and lipid metabolism and the energy balance of heart muscle. Annual Review of Physiology. 1974;36:413–459. doi: 10.1146/annurev.ph.36.030174.002213. [DOI] [PubMed] [Google Scholar]
- 62.Koc A, Duru M, Ciralik H, Akcan R, Sogut S. Protective agent, erdosteine, against cisplatin-induced hepatic oxidant injury in rats. Molecular and Cellular Biochemistry. 2005;278(1-2):79–84. doi: 10.1007/s11010-005-6630-z. [DOI] [PubMed] [Google Scholar]
- 63.Tiersten A, Wo J, Jacobson C, et al. Cardiac toxicity observed in association with high-dose cyclophosphamide-based chemotherapy for metastatic breast cancer. Breast. 2004;13(4):341–346. doi: 10.1016/j.breast.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 64.Selvakumar E, Prahalathan C, Sudharsan PT, Varalakshmi P. Protective effect of lipoic acid on cyclophosphamide-induced testicular toxicity. Clinica Chimica Acta. 2006;367(1-2):114–119. doi: 10.1016/j.cca.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 65.Kumar SA, Sudhahar V, Varalakshmi P. Protective role of eicosapentaenoate-lipoate (EPA-LA) derivative in combating oxidative hepatocellular injury in hypercholesterolemic atherogenesis. Atherosclerosis. 2006;189(1):115–122. doi: 10.1016/j.atherosclerosis.2005.11.037. [DOI] [PubMed] [Google Scholar]


