Abstract
Background
Little is known about the influence of in-town fast-food availability on family-level fast-food intake in nonmetropolitan areas.
Purpose
The purpose of the current study was to determine whether the presence of chain fast-food outlets was associated with fast-food intake among adolescents and parents, and to assess whether this relationship was moderated by family access to motor vehicles.
Methods
Telephone surveys were conducted with 1547 adolescent–parent dyads in 32 New Hampshire and Vermont communities between 2007 and 2008. Fast-food intake in the past week was measured through self-report. In-town fast-food outlets were located and enumerated using an onsite audit. Family motor vehicle access was categorized based on the number of vehicles per licensed drivers in the household. Poisson regression was used to determine unadjusted and adjusted risk ratios (RRs). Analyses were conducted in 2011.
Results
About half (52.1%) of adolescents and 34.7% of parents consumed fast food at least once in the past week. Adolescents and parents who lived in towns with five or more fast-food outlets were about 30% more likely to eat fast food compared to those in towns with no fast-food outlets, even after adjusting for individual, family, and town characteristics (RR=1.29, 95% CI= 1.10, 1.51; RR=1.32, 95% CI=1.07,1.62, respectively). Interaction models demonstrated that the influence of in-town fast-food outlets on fast-food intake was strongest among families with low motor vehicle access.
Conclusions
In nonmetropolitan areas, household transportation should be considered as an important moderator of the relationship between in-town fast-food outlets and family intake.
Background
Recent studies have explored the relationship between where people live and what they eat.1–4 Ecologic theorists suggest that dietary behaviors are influenced by food availability within immediate environmental contexts.5–7 Residents of neighborhoods with nutrient-dense food sources (e.g., supermarkets) are hypothesized to have healthier diets than residents of areas with nutrient-poor food sources (e.g., convenience stores).2, 4, 8 However, data supporting this hypothesis are mixed.1,9–14 Evidence supporting a relationship between diet and proximity to supermarkets is stronger than for proximity to restaurants; similarly, research has been more successful in identifying environmental correlates of healthy diets (e.g., fruit/vegetable intake) than unhealthy diets (e.g., high fat intake).1, 9–15
Fast-food restaurants are often considered undesirable community food sources because they offer products high in calories, saturated fat, sodium, and sugar.16–19 With >300,000 fast-food restaurants in the U.S.,20 high intake of fast food is not surprising. In 2008, 37% of Americans’ away-from-home food expenditures were at fast-food restaurants.21 One widely cited study of children aged 4–19 years indicated that 30.3% consumed fast food on a typical day.22 Others have found that >75% of young adults consume fast food at least once per week.23 Among adults, nearly one third report weekly fast-food intake.24
Most research linking community fast-food restaurants with fast-food intake has been conducted in urban areas and with adults, and findings are contradictory.15, 24–26 This lack of consensus may be related to specific household characteristics, such as SES or transportation, that could alter the frequency with which individuals purchase foods from neighborhood outlets.27, 28 For instance, Inagami et al. found that car ownership moderated the association between fast-food outlet concentration and BMI in an urban area.28 The role of motor vehicle access may be greater in nonmetropolitan settings, which are less likely to have well-developed public transportation.
The purpose of this study was to determine whether the presence of in-town fast-food outlets (i.e., all fast-food outlets located within town geographic boundaries) was associated with fast-food intake among adolescents and parents, after adjusting for individual, family, and town characteristics. Secondly, the study assessed whether this relationship was moderated by family motor vehicle access. The hypothesis was that the association between in-town fast-food outlets and intake would be stronger among adolescents and parents with low motor vehicle access.
Methods
Data were collected as part of a larger study of individual, family, and environmental influences on adolescent obesity. The study was approved by the Committee for the Protection of Human Subjects at Dartmouth College.
Study Design
Adolescent and parent fast-food intake were measured through telephone surveys with a community-based cohort, and in-town fast-food outlets were ascertained through onsite community assessments. Detailed information on cohort recruitment has been reported previously.29, 30 Briefly, 87% of students enrolled in Grades 4–6 at 26 randomly selected New Hampshire (NH) and Vermont (VT) public schools were surveyed between 2002 and 2003. Seventy-one percent (n=2631) were subsequently enrolled in a longitudinal telephone survey of adolescent–parent dyads.
Telephone surveys were administered by trained interviewers using a computer-assisted telephone interviewing system. Adolescents and parents were interviewed separately. Whenever possible, the adolescent's mother was interviewed. Parental consent and adolescent assent were obtained at each wave.
Data for the current study were obtained at Wave 4, conducted between 2007 and 2008, when adolescents attended Grades 7–11. The follow-up rate for this wave was 71.6%, providing a sample of 1885 adolescent–parent dyads. Food outlet assessments were conducted in 32 New Hampshire and Vermont towns where the majority (n=1582) of adolescents resided. The final analytic sample includes 1547 adolescent–parent dyads with complete data for the variables of interest. The final sample resembled the baseline sample in terms of adolescent gender and mean age at baseline. Compared to baseline, parents in the final sample were more likely to be white (86.7% vs 92.6%) and to have at least a bachelor's degree (18.4% vs 34.8%).
All food outlets within town limits were identified using a two-step process. An inventory of in-town food outlets was created using two public Internet sites (Google Earth and Yahoo! Yellow Pages). Subsequently, during summer 2007, coding teams systematically drove all in-town street networks to verify and augment the presence and location of all fast-food outlets. Details for these procedures have been described previously.31
Individual and Town Measures
Fast-food intake was measured through self-report by asking adolescents and parents, “In the past 7 days how many times did you eat fast food, for example, food from McDonalds, Burger King, KFC, or Dunkin’ Donuts?” Responses were dichotomized to represent any fast-food consumption versus none in the past week. Parents reported the number of motor vehicles in the household and the number of licensed drivers. Motor vehicle access was calculated and categorized into three groups: less than one (low vehicle access), one (moderate vehicle access), and more than one (high vehicle access) vehicle per licensed driver in the household.
Adolescents reported their grade, school, and if they had a driver's license. Adolescent gender and age were assessed through the baseline adolescent survey. Parent gender, age, and race were assessed through the baseline parent survey. Adolescent race, parent education, and household income were assessed through the Wave-4 parent telephone survey. The highest level of education completed by either parent was used. Single-parent households were identified by asking parents, “Do you have a partner or spouse who lives with you?”
The primary exposure variable was the number of in-town fast-food outlets. Using a structured observation form and manual developed and validated for the current study,31 field coders classified food outlets as either food markets (one of six categories) or eating establishments (fast-food or full-service restaurant). Fast-food outlets were defined as any food outlet where the patron orders at a counter or window.
Fast-food restaurants were further classified as chain (four or more outlets) or locally owned. Fast-food businesses housed in food markets were counted as distinct food outlets (n=43) if the fast-food section had a separate name, logo, entryway, cash register, or employee. Only chain fast-food outlets were used in the current analyses to be consistent with the wording of the fast-food intake survey question. The number of chain fast-food outlets in a town was categorized into three groups, providing a balanced distribution of dyads in each category: no food outlets (16 towns; 486 dyads); 1–4 food outlets (seven towns, 524 dyads); and five or more food outlets (nine towns, 537 dyads).
Town population was determined by the 2007 U.S. Census Population Estimates32 and categorized into four groups: <2499; 2500–4999; 5000–9999; ≥10,000 people. Town median household income was determined by the 2000 U.S. Census33 and categorized into three groups: <$40,000; $40,000–$50,000; >$50,000. Town distance to urban area was derived from the U.S. Census Rural and Urban Classification GIS layer,34 and categorized into four groups representing increments of 10–25 miles.
Statistical Analyses
Poisson regression was used to determine unadjusted and adjusted risk ratios and 95% CIs. Robust,35 cluster36 variance estimates were used to account for the binomial outcome variable37 and the within-school correlation. The relationship between fast-food intake (adolescents’ and parents’) and in-town fast-food outlets was examined in unadjusted and fully adjusted models. The adjusted adolescent and parent models both included parent gender, age, race, education, household income, single-parent status, motor vehicle access, distance from the town center to the nearest urban area, and the town median household income. The adjusted adolescent model also included adolescent age, gender, race, and possession of a driver's license.
The joint effects of in-town fast-food outlets (continuous and with three levels: 0, 1–4, >=5) and motor vehicle access (low, moderate, high) were also modeled, with participants who lived in towns with no fast-food outlets and had low motor vehicle access as the reference group. In the fully adjusted models, it was not possible to include a term representing the town's population because of its near-perfect collinearity with the number of in-town fast-food outlets (r=0.97). To ensure that findings were not an artifact of the highly skewed distribution of the main exposure variable, the interaction analysis was repeated using different in-town fast-food cutoffs (i.e., 0, 1–3, 4–9, 10+) and by truncating down to 29 or 16 maximum fast-food outlets per town. A two-tailed p<0.05 was used to define significance. All analyses were conducted in 2011 using STATA version 11.0.
Results
Sample Characteristics
Adolescents’ ages ranged from 12 to 18 years, with a mean of 14.4 (SD=1.0) years (Table 1). Half were girls and the majority (94.3%) were non-Hispanic white, reflecting the underlying population of New Hampshire and Vermont. Only 5.5% had a driver's license. Most adult participants were mothers (94.2%), and were aged >40 years (77.8%). Almost half (45.8%) indicated that they and/or their spouse had at least a bachelor's degree, and 43% reported a household income >$75,000. Nearly 75% of families lived in towns with a population of <10,000. Eleven percent of dyads lived in households with low vehicle access (i.e., less than one vehicle per licensed driver), whereas 27.5% reported high vehicle access (i.e., more than one vehicle per licensed driver).
Table 1.
Adolescent, parent/family, and town characteristics and adolescent fast-food intake
| Sample, n | Ate fast food in the last week n (%) | Unadjusted relative risk (95% CI) | Adjusted relative risk (95% CI) | |
|---|---|---|---|---|
| Adolescent | ||||
| Age (years) | ||||
| 12–13 | 294 | 159 (54.1) | ref | ref |
| 14 | 540 | 264 (48.9) | 0.90 (0.79,1.04) | 0.89 (0.80,1.00)* |
| 15 | 490 | 236 (48.2) | 0.89 (0.75,1.06) | 0.91 (0.80,1.04) |
| 16–18 | 223 | 147 (65.9) | 1.22 (1.01,1.47)* | 1.17 (0.97,1.40) |
| Gender | ||||
| Female | 772 | 379 (49.1) | ref | ref |
| Male | 775 | 427 (55.1) | 1.12 (1.01,1.25)* | 1.13 (1.01,1.25)* |
| Race | ||||
| White | 1458 | 756 (51.9) | ref | ref |
| Not White | 89 | 50 (56.2) | 1.08 (0.93,1.26) | 1.06 (0.92,1.21) |
| Driver's License | ||||
| No | 1461 | 749 (51.3) | ref | ref |
| Yes | 85 | 57 (67.1) | 1.31 (1.07,1.60)** | 1.08 (0.90,1.31) |
| Parent/Family | ||||
| Parent Age (years) | ||||
| < 40 | 343 | 191 (55.7) | ref | Ref |
| 40–49 | 965 | 497 (51.5) | 0.93 (0.82,1.05) | 0.99 (0.90,1.09) |
| ≥ 50 | 238 | 118 (49.6) | 0.89 (0.75,1.05) | 0.97 (0.82,1.15) |
| Parent gender | ||||
| Female | 1487 | 771 (51.9) | Ref | Ref |
| Male | 60 | 35 (58.3) | 1.13 (0.86,1.47) | 1.09 (0.82,1.46) |
| Race | ||||
| White | 1433 | 738 (51.5) | Ref | Ref |
| Not White | 114 | 68 (59.7) | 1.16 (0.98,1.38) | 1.09 (0.95,1.26) |
| Single-parent status | ||||
| No | 1290 | 659 (51.1) | Ref | Ref |
| Yes | 257 | 147 (57.2) | 1.12 (1.00,1.25)* | 1.02 (0.89,1.16) |
| Parent education | ||||
| High school diploma or less | 330 | 185 (56.1) | Ref | Ref |
| Some college, technical school, or Associate's degree | 507 | 283 (55.8) | 1.00 (0.89,1.12) | 0.99 (0.90,1.10) |
| Bachelor's degree | 420 | 213 (50.7) | 0.91 (0.77,1.06) | 0.95 (0.84,1.07) |
| Some graduate school or degree | 289 | 124 (42.9) | 0.77 (0.62,0.95)* | 0.87 (0.74,1.03) |
| Household income | ||||
| < $35k | 252 | 150 (59.5) | Ref | Ref |
| $35k–$75k | 614 | 323 (52.6) | 0.88 (0.78,1.00) | 0.94 (0.82,1.07) |
| > $75k | 658 | 324 (49.2) | 0.83 (0.69,0.99)* | 0.90 (0.76,1.06) |
| Motor vehicle accessa | ||||
| Low | 172 | 80 (46.5) | Ref | Ref |
| Moderate | 950 | 492 (51.8) | 1.11 (0.94,1.32) | 1.20 (1.01,1.42)* |
| High | 425 | 234 (55.1) | 1.18 (0.97,1.45) | 1.27 (1.05,1.53)* |
| Town | ||||
| Number of fast-food outlets | ||||
| 0 | 486 | 226 (46.5) | Ref | Ref |
| 1–4 | 524 | 260 (49.6) | 1.07 (0.76,1.50) | 1.07 (0.89,1.29) |
| ≥5 | 537 | 320 (59.6) | 1.28 (1.10,1.50)** | 1.29 (1.10,1.51)** |
| Distance from town center to nearest urban area (miles) | ||||
| 0-14.9 | 363 | 171 (47.1) | Ref | Ref |
| 15–24.9 | 435 | 231 (53.1) | 1.13 (0.77,1.64) | 1.19 (0.99,1.44) |
| 25–39.9 | 251 | 161 (64.1) | 1.36 (0.93,1.99) | 1.47 (1.03,2.09)* |
| 40–65 | 498 | 243 (48.8) | 1.04 (0.71,1.52) | 1.01 (0.76,1.35) |
| Median household income | ||||
| < $40k | 379 | 229 (60.4) | Ref | Ref |
| $40k – $50k | 603 | 293 (48.6) | 0.80 (0.62,1.04) | 0.83 (0.67,1.02) |
| > $50k | 565 | 284 (50.3) | 0.83 (0.64,1.09) | 0.91 (0.69,1.21) |
| Populationb | ||||
| < 2500 | 188 | 97 (51.6) | Ref | |
| 2,500–4,999 | 386 | 167 (43.3) | 0.84 (0.66,1.07) | |
| 5,000–9,999 | 565 | 300 (53.1) | 1.03 (0.72,1.47) | |
| ≥10,000 | 408 | 242 (59.3) | 1.15 (0.90,1.46) |
The 32 study towns covered 1237.6 square miles, with town sizes ranging from 2.0 to 67.2 square miles. Towns were similarly distributed with respect to total population: <2500 (n=11); 2500–4999 (n=7); 5000–9999 (n=8); >=10,000 (n=6). The majority (n=19) of towns were located over 25 miles from the nearest census-defined urban area. Twenty-five towns had a median household income of <$50,000. There were 960 food outlets located in the 32-town sampling area, of which 163 (17.0%) were chain fast-food outlets. The number of chain fast-food outlets per town ranged from 0 to 46; however, most (n=30) towns contained <17.
Unadjusted Models
Overall, about half of adolescents and one third of parents consumed fast food at least once during the week prior to the survey (Tables 1 and 2). The distribution of fast-food intake in the past week among adolescents and parents was: 0 times (adolescents: n=741, 47.9%; parents: n=1010, 65.3%); 1–2 times (adolescents: n=667, 43.8%; parents: n=477, 30.8%), ≥3 times (n=129, 8.3%; parents: n=60, 3.9%). Adolescent and parent fast-food intake were moderately but significantly correlated (r =0.24, p<0.001). Parents and adolescents residing in a town with at least five fast-food outlets were 1.22–1.28 (95% CI=1.05, 1.41 for parents; 1.10, 1.50 for adolescents) times more likely to eat fast food, compared to participants with no in-town chain fast food.
Table 2.
Parent/family and town characteristics and parent fast-food intake
| Sample, n | Ate fast food in the last week n (%) | Unadjusted relative risk (95% CI) | Adjusted relative risk (95% CI) | |
|---|---|---|---|---|
| Parent/family | ||||
| Parent age (years) | ||||
| < 40 | 343 | 148 (43.2) | Ref | Ref |
| 40–49 | 965 | 315 (32.6) | 0.76 (0.63,0.91)** | 0.85 (0.71,1.01) |
| ≥50 | 238 | 73 (30.7) | 0.71 (0.54,0.94)* | 0.83 (0.64,1.07) |
| Parent gender | ||||
| Female | 1487 | 515 (34.6) | Ref | Ref |
| Male | 60 | 22 (36.7) | 1.06 (0.76,1.48) | 0.96 (0.69,1.35) |
| Parent race | ||||
| White | 1433 | 490 (34.2) | Ref | Ref |
| Not White | 114 | 47 (41.2) | 1.21 (0.94, 1.54) | 1.12 (0.88, 1.42) |
| Single-parent status | ||||
| No | 1290 | 437 (33.9) | Ref | Ref |
| Yes | 257 | 100 (38.9) | 1.15 (1.00,1.32) | 1.05 (0.86,1.28) |
| Parent education | ||||
| High school diploma or less | 330 | 139 (42.1) | Ref | Ref |
| Some college, technical school, or Associate's degree | 507 | 189 (37.3) | 0.89 (0.76,1.03) | 0.90 (0.77,1.06) |
| Bachelor's degree | 420 | 142 (33.8) | 0.80 (0.68,0.95)* | 0.91 (0.75,1.10) |
| Some graduate school or degree | 289 | 66 (22.8) | 0.54 (0.41,0.72)*** | 0.67 (0.51,0.86)** |
| Household income | ||||
| < $35k | 252 | 108 (42.9) | Ref | Ref |
| $35k – $75k | 614 | 217 (35.3) | 0.83 (0.69,0.99)* | 0.90 (0.73,1.10) |
| > $75k | 658 | 206 (31.3) | 0.73 (0.60,0.89)** | 0.88 (0.72,1.07) |
| Motor vehicle accessa | ||||
| Low | 172 | 56 (32.6) | Ref | Ref |
| Moderate | 950 | 320 (33.7) | 1.04 (0.79,1.35) | 1.07 (0.82,1.40) |
| High | 425 | 161 (37.9) | 1.16 (0.87,1.56) | 1.18 (0.88,1.59) |
| Town | ||||
| Number of fast-food outlets | ||||
| 0 | 486 | 158 (32.5) | Ref | Ref |
| 1–4 | 524 | 166 (31.7) | 0.97 (0.64,1.48) | 1.00 (0.78,1.27) |
| ≥5 | 537 | 213 (39.7) | 1.22 (1.05,1.41)** | 1.32 (1.07,1.62)** |
| Distance from town center to nearest urban area (miles) | ||||
| 0–14.9 | 363 | 119 (32.8) | Ref | Ref |
| 15–24.9 | 435 | 140 (32.2) | 0.98 (0.63,1.54) | 1.13 (0.87,1.47) |
| 25–39.9 | 251 | 116 (46.2) | 1.41 (0.88,2.26) | 1.80 (1.24,2.62)** |
| 40–65 | 498 | 162 (32.5) | 0.99 (0.63,1.56) | 1.24 (0.87,1.75) |
| Median household income | ||||
| < $40k | 379 | 136 (35.9) | Ref | Ref |
| $40k – $50k | 603 | 208 (34.5) | 0.96 (0.72,1.28) | 1.06 (0.86,1.30) |
| > $50k | 565 | 193 (34.2) | 0.95 (0.70,1.29) | 1.30 (0.97,1.73) |
| Populationb | ||||
| <2500 | 188 | 63 (33.5) | Ref | |
| 2,500–4,999 | 386 | 116 (30.1) | 0.90 (0.68,1.18) | |
| 5,000–9,999 | 565 | 195 (34.5) | 1.03 (0.67,1.58) | |
| >=10,000 | 408 | 163 (40.0) | 1.19 (0.92,1.55) |
Low = less than one vehicle per licensed driver, moderate = one vehicle per licensed driver, high = more than one vehicle per licensed driver.
Population was not included in adjusted models.
p < 0.05
p < 0.01
Male gender, older age, having a driver's license, living in a single-parent home, lower parental education, and lower household income were associated with adolescent fast-food consumption. Parents who consumed fast food were more likely to be younger, less educated, and to report a household income of <$35,000. Fast-food intake among adolescents or parents was unrelated to town population, distance to urban area or town median household income. Results were similar when fast-food intake was modeled as an ordinal variable (i.e., 0, 1, 2+ times in the past week).
Multivariate Models
Compared to participants living in a town with no fast-food outlets, adolescents and parents with five or more in-town fast-food outlets were about 30% more likely to eat fast food in the preceding week, even after adjusting for individual, family, and town characteristics (RR=1.29, 95% CI=1.10, 1.51; RR=1.32, 95% CI=1.07,1.62, respectively). Compared to families with low vehicle access, adolescents in families with moderate or high vehicle access were more likely to consume fast food (RR=1.20, 95% CI=1.00, 1.42; RR=1.27, 95% CI=1.05, 1.54, respectively). Adolescent fast-food intake also was associated with older age and male gender; among parents, intake was associated with low parent education. For parents and adolescents, living 25–39.9 miles from an urban area was associated with higher fast-food intake compared to living less than 15 miles.
Interaction
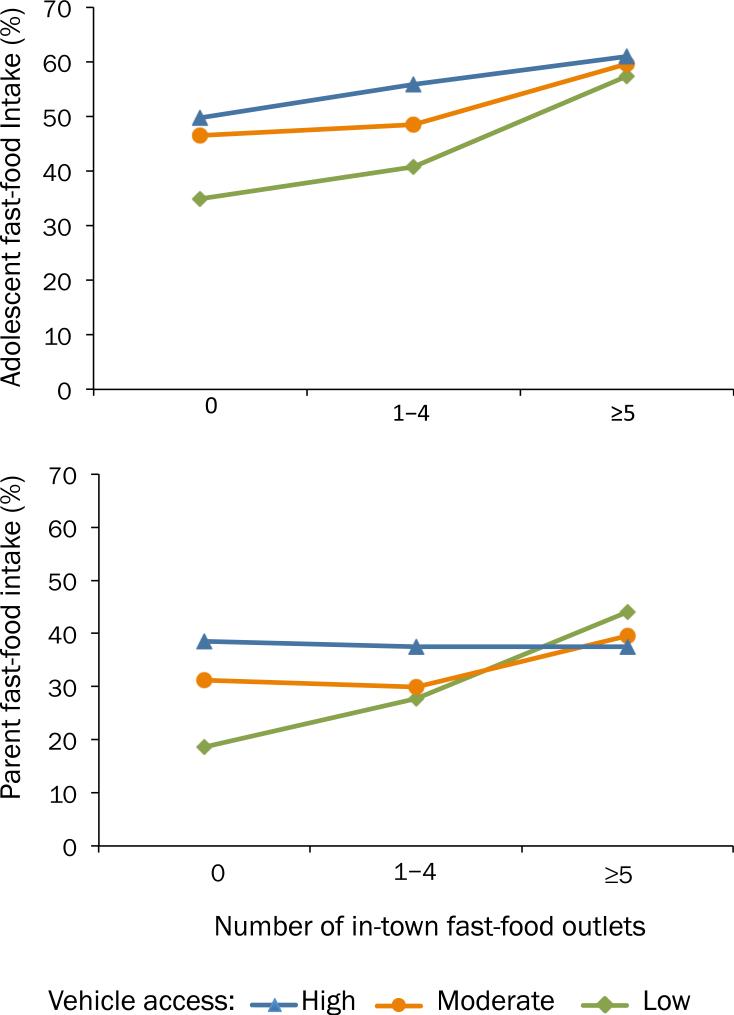
Figure 1 illustrates the crude association between adolescent and parent fast-food intake, motor vehicle access, and in-town fast-food outlets. There was a positive association between in-town fast-food outlets and intake among adolescents and parents with low motor vehicle access. This association was attenuated as access to motor vehicles increased, especially among parents. Fast-food intake among adolescents and parents who lived in towns with no fast-food outlets was positively associated with motor vehicle access, such that families with low access were less likely to eat fast food compared to families with high access (adolescents: 34.9% vs 49.7%, p=0.08; parents: 18.6% vs 38.5%, p=0.02, respectively). Fast-food intake among adolescents and parents who lived in towns with five or more fast-food outlets was similar regardless of their vehicle access.
Figure 1.
Prevalence of adolescent and parent fast-food intake by in-town fast-food outlets and family motor vehicle access
After adjustments, the interactions between fast-food outlets as a continuous variable and vehicle access were significant in the adolescent and parent models (p<0.01 for both). Fast-food intake increased with the number of in-town fast-food outlets (measured continuously) among families with low (test of trend: adolescent, p<0.001; parent, p<0.05) or moderate (test of trend: adolescent, p<0.05; parent, p=0.01) vehicle access but not among families with high vehicle access (test of trend: adolescent, p=0.61; parent, p=0.99). The adjusted, joint effects of in-town fast-food outlets (measured categorically) and motor vehicle access on fast-food intake, using a common reference category of low motor vehicle access and no fast-food outlets, are detailed in Table 3.
Table 3.
Joint effects of fast-food outlets and motor vehicle access on adolescent and parent fast-food intake
| Adolescent fast-food intakea | |||
|---|---|---|---|
| Vehicle Accessb | ARR (95% CI) by number of fast-food outlets |
||
| 0 Outlets | 1–4 Outlets | 5+ Outlets | |
| Low | 1 (Ref) | 1.29 (0.79, 2.11) | 1.69 (1.09,2.63)* |
| Moderate | 1.51 (0.96,2.38) | 1.53 (0.96, 2.43) | 1.88 (1.26,2.82)** |
| High | 1.64 (1.03,2.61)* | 1.83 (1.11,3.02)* | 1.91 (1.27,2.89)** |
| Parent fast-food intakec | |||
|---|---|---|---|
| Vehicle Accessb | ARR (95% CI) By Number of Fast Food Outlets |
||
| 0 Outlets | 1–4 Outlets | 5+ Outlets | |
| Low | 1 (Ref) | 1.71 (0.58,5.01) | 2.51 (1.13,5.55)* |
| Moderate | 1.77 (0.73,4.31) | 1.82 (0.74,4.47) | 2.27 (1.02,5.06)* |
| High | 2.18 (0.99,4.80) | 2.29 (1.00,5.26) | 2.21 (1.00,4.91) |
The sample size from the left to right, for both models, was 43, 282, and 161 for low vehicle access; 54, 334, and 136, for moderate vehicle access; and 75, 334, and 128 for high vehicle access.
Adolescent model is adjusted for adolescents’ age, gender, race, and drivers’ license, parents’ age, gender, race, single-parent status, education, and household income, and the distance from the town center to the nearest urban area, and the town median household income.
Low = less than one vehicle per licensed driver, moderate = one vehicle per licensed driver, high = more than one vehicle per licensed driver.
Parent model is adjusted for parents’ age, gender, race, single-parent status, education, and household income, and the distance from the town center to the nearest urban area, and the town median household income.
p < 0.05
p < 0.01
ARR, adjusted risk ratio
Compared to the referent group, adolescents had an overall higher risk of consuming fast food if they lived in a household with high motor vehicle access (RR 1.64 to 1.91) or a town with five or more fast-food outlets (RR 1.69 to 1.91). Regardless of vehicle access, parents had higher intake if they lived in towns with five or more fast-food outlets (RR 2.21 to 2.51). Although the risk ratios for parents with high vehicle access were similar to the ratios for five or more outlets, the p-value was p=0.05. Additional analyses using different cutoffs for in-town fast-food outlets did not substantially change the findings.
Discussion
This study provides evidence for the complex interplay between individual and environmental influences on dietary behavior. Among adolescents, within each level of motor vehicle access, fast-food intake was positively associated with the number of in-town fast-food outlets. However, the magnitude of the increase was greatest among adolescents with low vehicle access. In households with low motor vehicle access, adjusted analyses demonstrated a 69% increase in fast-food intake between adolescents living in towns with five or more versus no chain fast-food outlets. In contrast, among adolescents with moderate or high vehicle access, the difference in fast-food intake between participants living in towns with none versus at least five fast-food outlets was 16%–25%.
Results for parents were somewhat similar, although the larger CIs suggest greater variation among adults. These results demonstrated a strong effect of the fast-food environment among parents with low vehicle access on fast-food intake, with this effect attenuated as access to motor vehicles increased. Although the relative risks for 1–4 outlets were not significant in the main effects models (Tables 1 and 2), the significant test of trend indicates that fast-food intake increases with in-town fast-food outlets measured continuously. Furthermore, in the interaction models, the risk ratios for 1–4 outlets support a dose–response relationship. The moderate correlation between adolescent and parent fast-food intake indicates that motivations or opportunities for fast-food purchases may differ between adolescents and adults.38–41 To our knowledge, this is the first study to examine the joint effects of in-town fast-food outlets with household motor vehicle access on fast-food intake in nonmetropolitan areas.
Consistent with the study hypotheses, the results indicate that adolescents and parents residing in towns with numerous fast-food outlets are more likely to consume fast food, and in-town fast food conferred a stronger influence on families with limited household transportation. These results are consistent with those of Inagami et al. who found that people who did not own a car and lived in urban neighborhoods with a high concentration of fast food had a higher BMI than those who did not own a car and lived in areas with no fast-food outlets, after controlling for individual and neighborhood characteristics. They concluded that the local fast-food environment had a stronger association with BMI for residents with no car access.28 Given the discrepant geographic areas (i.e., highly urban vs nonmetropolitan) between these two studies, the congruence of findings warrants further attention to the potential moderating influence of vehicle ownership.
This study contributes to the increasing body of literature showing an association between the community food environment and individual dietary behavior,9–15, 42 and it is the first to examine the association in adolescents. Further, the current study examines the relationship between intake and food environments in nonmetropolitan towns, identified as a geographic area warranting further attention.42 The findings also demonstrate that the relationship between the built environment and individual behavior is multifaceted, and environmental influences pose differential risks depending on individual- or family-level attributes. Recent studies examining fast-food exposure and intake have revealed additional moderators, including low household income and specific personality traits,27, 43 suggesting that more-refined approaches are needed to explain under what circumstances or for which populations the built environment may influence diet.
Town was selected as the geographic unit of analysis for several reasons. In New Hampshire and Vermont, town boundaries define the local political structure, which has considerable authority in making development and commercial decisions. Unlike other U.S. regions, in these two states, town boundaries are equivalent to school district boundaries, and are thus especially relevant to children's environments. Finally, the majority of Northern New England towns are discrete geographic units with large expanses of undeveloped land between compact town centers, creating clearly demarcated, easily identifiable boundaries. Future research should examine alternative geographic boundaries (e.g., buffer zones).
The study sample was primarily white and restricted to residents of Northern New England. However, reported fast-food intake was comparable to prior studies from geographic regions with more diverse populations.23–25, 44, 45 Motor vehicle access was surprisingly high, with only 11% of families having fewer than one vehicle per licensed driver in the household. The study should be replicated in other nonmetro settings with lower household vehicle access.
The number of in-town fast-food outlets was highly correlated with overall town population, so one cannot exclude the possibility that an unidentified variable accounted for the association between fast-food intake and town size. The self-report fast-food intake question did not assess what specific foods or beverages were consumed or whether the fast-food outlets visited were within participants’ residential town. Further, the question did not list all fast-food outlets that were counted as exposures; this may have underestimated the association between fast-food outlets and intake. For consistency with survey terminology, only chain fast-food outlets were included in the townwide measure. Future studies should examine the potential influence of locally owned fast-food outlets, which offer similar types of calorically dense food.
Increasingly, public health guidelines emphasize the creation of healthy environments to prevent obesity.46, 47 Targeting strategies to specific geographic areas and identifying the most vulnerable populations will utilize resources more efficiently. This study suggests that families, especially adolescent children within families with low household transportation, may be most responsive to changes in fast-food availability in their immediate environment. In contrast, families with high motor vehicle access are less influenced by the fast-food environment in their town of residence and thus a broader approach may be needed to modify their fast-food intake.
Acknowledgments
This work was supported by the National Institute of Environmental Health Sciences, Grant No. R01 ES014218.
We thank Jennie Brentrup, Caitlin Cunningham, Nick DeFrancis, and Erik Marquez for community data collection, and Sandy Beauregard for data management.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Griskes K, van Lenthe F, Avendano-Pabon M, Brug J. A systematic review of environmental factors and obesogenic dietary intakes among adults: Are we getting closer to understanding obesogenic environments? Obes Rev. 2011;12(5):e95–e106. doi: 10.1111/j.1467-789X.2010.00769.x. [DOI] [PubMed] [Google Scholar]
- 2.Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating healthy food and eating environments: Policy and environmental approaches. Annu Rev Public Health. 2008;29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 3.Larson NI, Story MT, Nelson MC. Neighborhood environments: Disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 4.Ford PB, Dzewaltowski DA. Disparities in obesity prevalence due to variation in the retail food environment: Three testable hypotheses. Nutr Rev. 2008;66(4):216–28. doi: 10.1111/j.1753-4887.2008.00026.x. [DOI] [PubMed] [Google Scholar]
- 5.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006;16(1):89–108. doi: 10.1353/foc.2006.0009. [DOI] [PubMed] [Google Scholar]
- 6.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280(5368):1371–74. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 7.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315(7106):477–80. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR., Jr Associations of the local food environment with diet quality--a comparison of assessments based on surveys and geographic information systems: The multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167(8):917–24. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: The atherosclerosis risk in communities study. Am J Public Health. 2002;92(11):1761–7. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laraia BA, Siega-Riz AM, Kaufman JS, Jones SJ. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med. 2004;39(5):869–75. doi: 10.1016/j.ypmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Zenk SN, Schulz AJ, Hollis-Neely T, et al. Fruit and vegetable intake in African Americans income and store characteristics. Am J Prev Med. 2005;29(1):1–9. doi: 10.1016/j.amepre.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the U.S. food stamp program. Public Health Nutr. 2004;7(8):1081–8. doi: 10.1079/PHN2004648. [DOI] [PubMed] [Google Scholar]
- 13.Michimi A, Wimberly MC. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous united states. Int J Health Geogr. 2010;9:49. doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodor JN, Rose D, Farley TA, Swalm C, Scott SK. Neighbourhood fruit and vegetable availability and consumption: The role of small food stores in an urban environment. Public Health Nutr. 2008;11(4):413–20. doi: 10.1017/S1368980007000493. [DOI] [PubMed] [Google Scholar]
- 15.Fraser LK, Edwards KL, Cade J, Clarke GP. The geography of fast food outlets: A review. Int J Environ Res Public Health. 2010;7(5):2290–2308. doi: 10.3390/ijerph7052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prentice AM, Jebb SA. Fast foods, energy density and obesity: A possible mechanistic link. Obes Rev. 2003;4(4):187–94. doi: 10.1046/j.1467-789x.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 17.O'Donnell SI, Hoerr SL, Mendoza JA, Tsuei Goh E. Nutrient quality of fast food kids meals. Am J Clin Nutr. 2008;88(5):1388–95. doi: 10.3945/ajcn.2008.26197. [DOI] [PubMed] [Google Scholar]
- 18.Huang C, Dumanovsky T, Silver LD, Nonas C, Bassett MT. Calories from beverages purchased at 2 major coffee chains in new york city, 2007. Prev Chronic Dis. 2009;6(4):A118. [PMC free article] [PubMed] [Google Scholar]
- 19.Dunford E, Webster J, Barzi F, Neal B. Nutrient content of products served by leading australian fast food chains. Appetite. 2010;55(3):484–9. doi: 10.1016/j.appet.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 20.The NPD Group U.S. restaurant count down by 5,551 from last year; independents declined by 2 percent and chain units remained stable. www.npd.com/press/releases/press_110124.html.
- 21.Economic Research Service Food CPI and expenditures, Table 15. www.ers.usda.gov/briefing/CPIfoodandexpenditures/data/table15.htm.
- 22.Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113(1 Pt 1):112–8. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 23.Larson NI, Neumark-Sztainer DR, Story MT, Wall MM, Harnack LJ, Eisenberg ME. Fast food intake: Longitudinal trends during the transition to young adulthood and correlates of intake. J Adolesc Health. 2008;43(1):79–86. doi: 10.1016/j.jadohealth.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR, Franco M. Fast-food consumption, diet quality, and neighborhood exposure to fast food: The multi-ethnic study of atherosclerosis. Am J Epidemiol. 2009;170(1):29–36. doi: 10.1093/aje/kwp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:35. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: Are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr. 2010;13(11):1757–63. doi: 10.1017/S1368980010001564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores: Longitudinal associations with diet in young to middle-aged adults: The CARDIA study. Arch Intern Med. 2011;171(13):1162–70. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inagami S, Cohen DA, Brown AF, Asch SM. Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health. 2009;86(5):683–95. doi: 10.1007/s11524-009-9379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dalton MA, Adachi-Mejia AM, Longacre MR, et al. Parental rules and monitoring of children's movie viewing associated with children's risk for smoking and drinking. Pediatrics. 2006;118(5):1932–42. doi: 10.1542/peds.2005-3082. [DOI] [PubMed] [Google Scholar]
- 30.Dalton MA, Longacre MR, Drake KM, et al. Built environment predictors of active travel to school among rural adolescents. Am J Prev Med. 2011;40(3):312–319. doi: 10.1016/j.amepre.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Longacre MR, Primack BA, Owens PM, et al. Public directory data sources do not accurately characterize the food environment in two predominantly rural states. J Am Diet Assoc. 2011;111(4):577–82. doi: 10.1016/j.jada.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Census Bureau Population estimates: Cities and towns – minor civil divisions, 2000-2007. www.census.gov/popest/cities/SUB-EST2007-5.html.
- 33.U.S. Census Bureau U.S. Census Bureau American Fact Finder. factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=gn10_select_state.
- 34.U.S. Census Bureau UA/UC Census 2000 boundary files. www.census.gov/geo/www/ua/ua_bdfile.html.
- 35.Huber PJ. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Vol. 1. University of California Press; Berkeley, CA: 1967. The behavior of maximum liklihood estimates under nonstandard conditions. pp. 221–33. [Google Scholar]
- 36.Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. J Financial Quantitative Analysis. 1989;24:333–55. [Google Scholar]
- 37.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 38.French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: Associations with nutrient intake, food choices and behavioral and psychosocial variables. Int J Obes Relat Metab Disord. 2001;25(12):1823–33. doi: 10.1038/sj.ijo.0801820. [DOI] [PubMed] [Google Scholar]
- 39.Blake CE, Wethington E, Farrell TJ, Bisogni CA, Devine CM. Behavioral contexts, food-choice coping strategies, and dietary quality of a multiethnic sample of employed parents. J Am Diet Assoc. 2011;111(3):401–7. doi: 10.1016/j.jada.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lucan SC, Barg FK, Long JA. Promoters and barriers to fruit, vegetable, and fast-food consumption among urban, low-income African Americans--a qualitative approach. Am J Public Health. 2010;100(4):631–5. doi: 10.2105/AJPH.2009.172692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bauer KW, Larson NI, Nelson MC, Story M, Neumark-Sztainer D. Socio-environmental, personal and behavioural predictors of fast-food intake among adolescents. Public Health Nutr. 2009;12(10):1767–74. doi: 10.1017/S1368980008004394. [DOI] [PubMed] [Google Scholar]
- 42.Fleischhacker SE, Evenson KR, Rodriguez DA, Ammerman AS. A systematic review of fast food access studies. Obes Rev. 2011;12(5):e460–71. doi: 10.1111/j.1467-789X.2010.00715.x. [DOI] [PubMed] [Google Scholar]
- 43.Paquet C, Daniel M, Knauper B, Gauvin L, Kestens Y, Dube L. Interactive effects of reward sensitivity and residential fast-food restaurant exposure on fast-food consumption. Am J Clin Nutr. 2010;91(3):771–6. doi: 10.3945/ajcn.2009.28648. [DOI] [PubMed] [Google Scholar]
- 44.Bowman SA, Vinyard BT. Fast food consumption of U.S. adults: Impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23(2):163–8. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 45.Paeratakul S, Ferdinand DP, Champagne CM, Ryan DH, Bray GA. Fast-food consumption among U.S. adults and children: Dietary and nutrient intake profile. J Am Diet Assoc. 2003;103(10):1332–8. doi: 10.1016/s0002-8223(03)01086-1. [DOI] [PubMed] [Google Scholar]
- 46.Khan LK, Sobush K, Keener D, et al. Recommended community strategies and measurements to prevent obesity in the U.S. MMWR Recomm Rep. 2009;58(RR-7):1–26. [PubMed] [Google Scholar]
- 47.IOM . Local government actions to prevent childhood obesity. The National Academic Press; Washington, DC: 2009. [PubMed] [Google Scholar]