Abstract
Climate change is one of today's most pressing global issues. Policies to guide mitigation and adaptation are needed to avoid the devastating impacts of climate change. The health sector is a significant contributor to greenhouse gas emissions in developed countries, and its climate impact in low-income countries is growing steadily. This paper reviews and discusses the literature regarding health sector mitigation potential, known and hypothetical co-benefits, and the potential of health information technology, such as eHealth, in climate change mitigation and adaptation. The promising role of eHealth as an adaptation strategy to reduce societal vulnerability to climate change, and the link's between mitigation and adaptation, are also discussed. The topic of environmental eHealth has gained little attention to date, despite its potential to contribute to more sustainable and green health care. A growing number of local and global initiatives on ‘green information and communication technology (ICT)’ are now mentioning eHealth as a promising technology with the potential to reduce emission rates from ICT use. However, the embracing of eHealth is slow because of limitations in technological infrastructure, capacity and political will. Further research on potential emissions reductions and co-benefits with green ICT, in terms of health outcomes and economic effectiveness, would be valuable to guide development and implementation of eHealth in health sector mitigation and adaptation policies.
Keywords: climate change, adaptation, mitigation, global warming, eHealth, telemedicine, information and communication technology, greenhouse gas emission, policy
Many consider climate change to be today's most pressing global issue. Its physical, biological and social impacts are widely recognized (1) and evidence is accumulating that we are approaching the point where climate change may have irreversible impacts (2–4). Floods, forest fires and heat waves are more frequent, melting of the summer Arctic sea ice cover has accelerated faster than predicted, and in certain regions the climate is changing more rapidly than ecosystems can adapt (5, 6). Based on current models, 20–70% of all world species face extinction as a result of global warming and the rise in sea level (2). The media often discusses the humanitarian impact of catastrophic climate and weather events. However, under less extreme conditions, climate change may exacerbate disease burdens such as malnutrition, vector-borne illnesses, food and water-borne diseases, and cardio-pulmonary diseases. The 2006 ‘WHO Preventing Disease Through Healthy Environment’ reported there is evidence that 85 of 102 investigated diseases are related to the environment (7). Inconclusive evidence suggests that many of them may be worsened by climate change (8).
Over the past few decades, climate scientists have assessed levels of risk for severely damaging local and global ecosystems, and sought to define an acceptable or tolerable degree of climate change. In 1990, a 2°C increase in the average global warming above pre-industrial levels was discussed as an upper limit and this cut-off has guided policy work since then (9). No actual large-scale threshold in the climate system is, however, clearly linked to two degrees of warming (10). Some environmental thresholds are sensitive to rate of change while others are sensitive to spatial gradients of climate change. Further, even a 1°C increase in temperature above the year 2000 temperature has been proposed as possibly leading to dangerous climate change impacts (11). With the current rate of warming, targeting a 2°C increase by 2100 may be too optimistic (12). Even if greenhouse gas (GHG) emissions are stabilised immediately, surface air temperature will remain high and sea level rise will continue for centuries due to the inherent inertia of climate processes (13, 14). Hence, climate change is a continuous threat and all societal sectors need to develop strategies to reduce the frequency, magnitude and severity of these effects in order to prevent humanitarian and economic crises (8, 15–19). Climate change mitigation strategies are part of these efforts. In this context, this implies reducing emission of GHGs and adaptation strategies aimed at increasing resilience to existing and future climate impacts. The health sector is well positioned to lead by example. This is shown by the UK National Health Service and the New South Wales initiatives in Australia (20, 21).
Health sector mitigation strategies
The health sector is one of the largest economic sectors and has estimated expenditures of US $639 per person-year that corresponds roughly to 8–10% of global gross domestic product (GDP) (22). The US health care industry is the second largest energy consumer among all US industrial sectors, and its inpatients facilities are the second most energy-intensive commercial buildings in the country. The National Health Service (NHS), one of the largest European employers, has a carbon footprint of approximately 20 million tonnes of carbon dioxide (CO2) per year (23). This corresponds to more than 4% of annual emissions (24) and NHS buildings consume energy worth over £410 million annually (20). The health care sector is estimated to contribute 3–8% of the total emissions in developed countries (20, 22), while the percentages are expected to be lower in developing countries. Inhaled anaesthetics from health care facilities are emitted into the atmosphere because of poor waste management and lack of recycling strategies (25). Furthermore, as a mobile business, the health care sector also consumes countless litres of fossil fuel when patients and medical professionals travel to and from appointments, pick up prescriptions, and obtain tests and results. According to the US National Association for Home Care and Hospices, their home health care workers drove approximately 7.7 billion km to provide services in 2006 (www.nahc.org). The health sector, with its focus on health promotion and maintenance, can thus reasonably be expected to have a moral obligation to set a good example (26). The NHS is an organisation that aims to lead by example. Its 2009 Carbon Reduction Strategy for England stated: ‘The rapidly increasing risk of adverse effects on health from climate change is happening on this generation's watch – it will be this generation's legacy’ (20).
In many aspects, the health sector is no different from other industries and organisations. Hence, potential mitigation strategies relevant for the health sector are more or less universal. These include:
Building green, which includes strategies to conserve energy (27, 28)
Efficient energy distribution and use of renewable energy sources (29, 30)
Passive or low-energy cooling, heating and ventilation strategies (30–33)
Strategies for conserving and maintaining water resources (34, 35).
Other strategies are more specific for the health care sector and include:
Reducing GHG emissions from anaesthetic gas use and waste management (36, 37)
Increased use of health information technology, such as eHealth (22, 38).
This paper focuses on the relatively unexplored use of eHealth as a health sector climate change mitigation and adaptation strategy.
eHealth in a changing world
Health information technology, also referred to as eHealth, has the potential to make health care a greener business (22, 38). The term eHealth is broad and includes work within a health care organisation where ICT is of central importance. Electronic medical records, home monitoring of vital parameters using mobile technology, as well as electronic health-surveillance systems, are considered eHealth. eHealth applications can be broadly categorized into two groups: the use of distance-spanning technology for health care through telemedicine/virtual visits (i.e. video consultations, remote diagnostics, telehomecare); and the use of electronic documentation of health services (e.g. electronic health records, electronic prescriptions, surveillance systems). The term eHealth is also used interchangeably with telemedicine, telecare or telehealth and describes the utilization of electronic communication to exchange medical information from one site to another. Examples include expert consultations using video technology, teleradiology, and at-home speech therapy using the Internet. The term mobile Health (mHealth) is increasingly popular as mobile technology with network interfaces develops (such as mobile phones and tablet computers).
A gap exists between assumed and empirically demonstrated benefits of eHealth (39–41). Good quality clinical studies are few and usually limited in scope. Nevertheless, eHealth is argued to increase the quality and efficiency of care, reduce erroneous treatments, and improve access to care in remotely populated areas. Initial results from the largest home health care clinical study, the UK Whole System Demonstrator (WSD) program, strongly support these statements. Preliminary outcomes show 15% reduction in emergency room visits, 20% reduction in emergency admissions, 14% reduction in elective admissions, 14% reduction in bed days, and 45% reduction in mortality for patients with chronic heart failure (CHF), chronic obstructive pulmonary disease (COPD) and diabetes. Telemedicine is thus considered one of few reasonable solutions to address the growing number of elderly and chronically ill people in the developed world. Moreover, the need for telemedicine in provision of chronic care for elderly populations in low- and middle-income countries is growing rapidly as a consequence of the significant growth in the elderly population (demographic transition), as well as with the growing burden of chronic diseases in these countries (epidemiologic transition).
eHealth using electronic medical records and electronic prescriptions is valued primarily for its potential to increase efficiency and safe care delivery. For example, these systems have a promising potential to prevent fatal adverse drug reactions (ADRs). Such ADRs cause 5–13% of all hospital admissions in the developed world, and 90% are considered theoretically preventable (42–44). According to the European digital agenda, eHealth is expected to enable health service providers (i.e. public authorities, hospitals) from different member states to work more closely together and this puts pressure on the system to develop solutions to transfer and share medical knowledge in a safe way between care providers and between countries. Telemedicine may further be the only option to provide care for some populations (www.arctichealth.org/telehealth.php). Health care remains unaffordable and inaccessible for disadvantaged people in remote regions, especially in less developed countries, and this limitation is an impediment to breaking the vicious cycle of poverty and poor health. Use of the satellite-based Alaska Federal Health Care Access Network (AFHCAN) is an example of successful health care provision in resource poor and remote areas. AFHCAN provides care among the Alaskan indigenous populations (45). Many and powerful forces are thus in motion that will guide the development of eHealth from regional, national and global perspectives.
Application of eHealth as a climate change mitigation strategy
The success of eHealth as a mitigation strategy that aims to reduce health sector GHG emissions depends strongly on the type of service, need for investment in new equipment, and lifespan of the technology. A full carbon-cost benefit analysis for these applications is not yet feasible since all of the factors contributing to telemedicine's carbon footprint are not adequately studied. Manufacture, distribution, daily use, and subsequent disposal of ICT technology come with environmental costs. One should be prudent when estimating the environmental impact. Fortunately, the number of programmes addressing green and environmental computing or ‘green ICT’ is growing steadily on national and international levels. These programmes are addressing ICT from different angles, including greener manufacturing of components, increased energy efficiency, and enabling more efficient use of existing technology, which includes promoting eHealth in some programmes (46–48). Although the ICT sector contributes to approximately 2% of global carbon emissions, it is strongly believed that this technology has the potential of providing solutions that enable other industry sectors, including the health sector, to reduce part of the remaining 98% of global carbon emissions (46, 47, 49, 50).
Telemedicine is considered the most potent technology for GHG reductions (51). Like many other climate change mitigation strategies, telemedicine has the potential of reducing air pollution, known to be adversely associated with disease and deaths (52), by reducing travel and transportation. Though not all telemedicine applications will reduce travel, the benefits are obvious for home care programmes and outpatient consultations. The telemedicine programme at UC Davis, California, with its 13,000 outpatient consultations over a period of 5 years, has resulted in a savings of 4.7 million miles of travel and a reduction of 1,700 tonnes of CO2 emissions (38). Similar benefits are reported in Scotland (53), Wales (54) and Canada (55). In Canada, it has been estimated that more than 11 million home visits by nurses could be replaced by telecare, which would result in a reduction of about 120 million km of travel and 33.220 tonnes of associated GHG emissions annually (56). Hence, the true potential of eHealth as mitigation strategy is evident when looking at cumulative effects and the larger scale.
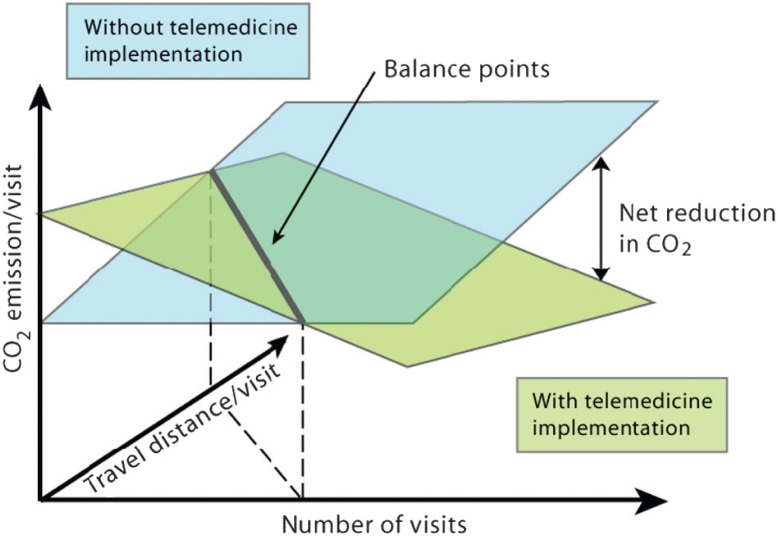
The local carbon reduction potential will depend on a number of factors. First, potential carbon savings are strongly related to the number of users and appointments that can be replaced by virtual visits. Second, the benefits will depend on the distance and type of transportation replaced by technology, that is whether the patient or medical professional typically travels by car, public transportation, or airplane, and the actual distances involved. Based on these factors, it should be possible to determine potential balance points where the introduction of eHealth results in a net reduction in CO2 (Fig. 1).
Fig. 1.
Schematic illustration of the potential net reduction in carbon emission with implementation of telemedicine services (shown in blue). The reduction potential is dependent on the number of visits as well as the carbon emission caused by each user's travel and visit in a traditional care scenario (shown in green). The climate impact from travel depends heavily on the type of transportation (e.g. public transportation, car, or aeroplane) but for simplicity is illustrated as travel distance only. This simplified model does not take into account that each piece of equipment can only serve a limited number of users and visits.
Implementation of eHealth in the form of electronic documentation, for example electronic health records, electronic prescriptions and surveillance systems, is likely to have less climate benefit and is mainly valued for the potential to improve the safety and efficiency of care provided. The GHG reductions following electronic documentations are complex. Although e-documentation might reduce travel, for example when prescriptions are available to the patient directly through the drugstore database, the main climate benefits are achieved through reduced paper use. This in turn lessens the negative impact of the paper industry and prevents unnecessary deforestation. Tropical deforestation is considered the single largest contribution of land-use change to global carbon emissions because it releases 1.5 billion tonnes of carbon each year into the atmosphere (57). However, the introduction of personal computers and electronic documentation are sometimes argued to increase the use of paper products and the straightforward benefits are difficult to estimate.
In summary, potential environmental benefits of eHealth will depend heavily on the existing infrastructure and local need. In countries with well-developed ICT-infrastructures, the actual steps towards carbon savings might be smaller. Countries with poorly developed infrastructures would have to make significant investments in technology for a potentially smaller gain. Nevertheless, eHealth has an important and relatively unexplored potential as a health-sector mitigation strategy. The full potential is far from being reached and could be developed far beyond the examples given in this review. Table 1 exemplifies existing and potential eHealth methodologies, GHG impacts and potential co-benefits that should be further explored.
Table 1.
Examples of eHealth methods and their potential impacts and health co-benefits
| eHealth methods | Direct & indirect greenhouse gas impact | Potential co-benefits and examples of subsequent implications |
|---|---|---|
| Video consultations, e.g. between general practitioner and specialist or specialist and patient | Reduced travel for specialist and/or patient |
|
| Telehomecare, e.g. remote support of self-management in chronic diseases | Reduced travel for patients and specialists |
|
| Remote public health or medical education | Reduced travel for teacher, patient, and/or student |
|
| Virtual visits | Reduced travel for patients and relatives |
|
| Remote diagnostics, e.g. teleradiology, remote auscultations | Reduced travel for patient and/or specialist |
|
| Electronic prescriptions | Reduced travel for patient Reduced paperworkb |
|
| Electronic medical records and referrals | Reduction in travel Reduced paperworkb |
|
Less pollution should result in direct benefits of lower rates of diseases such as respiratory diseases and cardiovascular diseases.
Reduced paperwork should result in less deforestation and lowered emission from paper manufacturing, transport and recycling.
Responding to climate change – eHealth as an adaptation strategy
Regardless of the mitigation strategies applied, there is an urgent need to develop sustainable strategies to adapt to on-going change in weather patterns and climate extremes (58). By anticipating, planning for, and responding to the risks, society can decrease its vulnerability to climate change (1, 15, 18). Adaptive capacity is closely related to a country's level of development, access to technological, political, social and economic resources, and availability of an efficient information infrastructure (1, 59). Vulnerability to climate change is worsened by factors such as poverty, conflicts, and the increasing incidences of infectious diseases such as HIV/AIDS, as well as high prevalences of chronic, non-communicable diseases such as cardiovascular disease. These burdens have overstretched countries’ capabilities in health promotion and improving the well-being of their population. This has diluted their capacities and attention to promoting adaptation to climate change.
In addition to making the health sector greener, eHealth has potential to help societies significantly adapt and reduce their vulnerability to climate change. Table 2 provides examples of promising eHealth adaptation strategies, and describes their potential benefits and limitations. These strategies include the use of telemedicine and mobile technology in anthropogenic and natural disasters (60–63), provision of point-of-care diagnostic tools (64), strengthening of public health surveillance using mobile technologies, and promoting knowledge, awareness and preparedness among the public, volunteers and health workers in regions with large burdens of disease (65–67).
Table 2.
Examples of potential eHealth adaptation strategies
| eHealth adaptation strategies | Impacts and benefits | Limitations and needs |
|---|---|---|
| Telemedicine in disasters |
|
|
| Point-of-care diagnostics for disease outbreaks |
|
|
| Public health surveillance of disease and mapping strategies using mobile devices |
|
|
| Remote education in preparedness and adaptation for health professionals and the public |
|
|
Ideally, adaptation strategies aimed at reducing vulnerability to climate change should be sustainable and avoid the counterproductive effects where adaptation leads to further increases in GHG emissions. By disregarding the link between mitigation and adaptation, societies can undermine effectiveness due to unaddressed conflicts between the two (68). For example, the use of air-conditioning to combat the negative health impact of heat waves can increase the carbon emissions and contribute to the increase in frequency of heat waves. Therefore, it is important to develop other strategies for mitigating urban heat islands through urban designs that reduce the need for air-conditioning (69). From this perspective, eHealth is a highly promising strategy that strengthens the argument to include health information technology in national and global strategies to combat and adapt to global warming.
Toward large-scale implementation of eHealth
The number of telemedicine programmes is constantly growing, but the rate of eHealth technology development poorly reflects the diffusion of eHealth services in actual clinical use. Different obstacles and challenges exist in the implementation of eHealth as an efficient climate change mitigation and adaptation strategy.
First, required and existing resources vary considerably across countries and regions. Countries with the least resources are typically the ones that would benefit the most from using eHealth to provide care in remote regions and disaster sites. There is a widespread opinion that eHealth is expensive and there is, indeed, a lack of independent, objective monitoring and evaluation of programmes to determine the actual financial benefit from adoption and use of ICT in health care (39–41). Moreover, there is a need to resolve the question of how to divide costs and benefits when technology is used to share information among different health care providers. Nevertheless, the introduction of telemedicine is likely to have important co-benefits that should be considered in health economic evaluations. Examples include: (1) increased quality of care and efficiency; (2) reduced operating costs of clinical services; (3) reduced administrative costs; and (4) increased opportunities for providing care to poor regions.
Second, the lack of infrastructure and slow adaptation of ICT by many countries, particularly in less developed regions, are a major impediment for establishing and up-scaling the use of eHealth. Complex geographical structures in archipelagic or mountainous nations, such as Indonesia and Pakistan, make the build-up of cable/digital infrastructure difficult and costly. Nonetheless, mobile networks, including the mobile broadband IT, are rapidly expanding and provide opportunities for wide scale implementation of eHealth. Slow adaptation of eHealth can also be attributed to lack of experience in ICT. User attitudes toward eHealth are strongly dependent on the purpose of the technology, organisational readiness and perceived benefits (70–72). A robust infrastructure is needed to ensure that the technique works even in case of natural or anthropogenic disasters. Hence, politicians and decision makers have a responsibility to ensure that the building of new ICT infrastructure complies with these needs and takes into account resilience to climate change.
Third, lack of standardisation, even in high-income countries, dilutes the effectiveness, functionality and sustainability of eHealth implementation in the long term. A growing number of initiatives focus on developing standards for eHealth applications. Countries that are new to eHealth should assess these guidelines carefully to ensure efficient implementation, interoperability and protection of the patient integrity and confidentiality (73–75). Estonia is a country that clearly demonstrates the benefits of interoperability. Despite being a country that is relatively new to eHealth, Estonia is the first country that implemented a nationwide electronic health record. In 2005, the Estonian Ministry of Social Affairs launched a new eHealth concept composed by four separate, but integrated, solutions: electronic health records, digital images, digital registration, and digital prescriptions.
Fourth, there is a widespread lack of awareness and political will to invest in eHealth, especially in resource-constrained countries. Implementing eHealth to address climate issues has not been taken into consideration by high-income countries with well-developed health infrastructure. Successful implementation thus requires joint and multidisciplinary efforts by governmental representatives, politicians and national and local stakeholders from the health care sector, industry (ICT, security) and organisations protecting patient rights.
Policy implications
One way to promote the use of eHealth is through national policies that create incentives for mitigation and adaptation actions in the health care sector. Governments that include eHealth in policy documents are more likely to adopt the technology than those who do not (76). Several green ICT initiatives present strategies for reducing the carbon footprint from ICT use (47). However, these may have little impact on the health sector due to lack of awareness among decision makers. Motivation to use the technology will increase by monitoring and quantifying progress in estimated emission reductions in the health sector in a way that makes international comparisons possible. In this way, the health sector has the potential to serve as an important model for other organisations and societal sectors in reducing GHG emissions. Hence, to explore fully the potential of eHealth as a climate change mitigation and adaptation strategy, it is important to target the health sector specifically. Using eHealth as climate policy may motivate health sector decision makers to commit to eHealth since it also offers co-benefits such as reduced long term costs, increased access to health care, and improved quality of health care services.
A wide range of policies and instruments exist, and examples of outcomes are legislation, regulation, action plans and decisions about positive incentives for citizens and industry. Different climate policies have different impacts on environmental effectiveness, cost effectiveness, and distributional effects that include equity and institutional feasibility (2). In terms of eHealth, policies that support technology and capacity development and build sustainable structures are of critical importance. This requires policy development at international, national, provincial and district levels, with top-down and bottom-up perspectives. Based on differences in legal and regulatory frameworks, as well as health care organisational structures, goals must be independently defined in each country and by each region, although ideally they should be based on the same technological platforms. In terms of disaster preparedness, eHealth or telemedicine policies may need to be developed on an international level in order to ensure that necessary aid is provided instantly and efficiently regardless of geographic origin (58). Thus, it is strongly recommended that infrastructure and services be based on global standards (74, 77), which will also allow efficient integration of new solutions without unnecessary extra costs.
Part of the policy agenda is to identify responsible and consultative bodies, as well as experts and national authorities, who work under ministerial supervision. At the national level, actions guided by boards of national decision makers and advisors, or the creation of national competence centres, can deal with challenges such as legal, regulatory or structural issues that delay or hinder the development of eHealth. They can also develop, inform, and evaluate progress in relation to the goal. At the provincial and district levels, health sector decision makers and health care providers have responsibilities to implement, evaluate, and improve guidelines and standards set at a national level. This must be done in dialogue with their suppliers and users. In essence, actions are needed at all levels of society for a successful outcome.
There is limited knowledge on the environmental impact of eHealth, and examples of eHealth as adaptation strategy are few. However, global trends towards green ICT strongly suggest that eHealth is a promising solution to reduce the health sector's carbon footprint. More research to provide an evidence base for local and global initiatives to develop green eHealth solutions and policies are therefore welcome.
Acknowledgements
This work was partly undertaken within the Umeå Centre for Global Health Research, with support from FAS, the Swedish Council for Working Life and Social Research (grant no. 2006-1512).
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Confalonieri U, Menne B, Akhtar R. Climate change 2007: impacts, adaptation and vulnerability. Contribution of working group II to the fourth assessment report of the intergovernmental panel of climate change. Cambridge, UK: Cambridge University Press; 2007. [Google Scholar]
- 2.Pachauri RK, Reisinger A, editors. Geneva, Switzerland: IPCC; 2007. Climate Change 2007: Synthesis Report. Contribution of working groups I, II and III to the fourth assessment report of the intergovernmental panel of climate change. p. 104. [Google Scholar]
- 3.Lenton TM. Arctic climate tipping points. Ambio. 2012;41:10–22. doi: 10.1007/s13280-011-0221-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duarte CM, Lenton TM, Wadhams P, Wassmann P. Abrupt climate change in the Arctic. Nat Clim Chang. 2011;2:60–62. [Google Scholar]
- 5.Post E, Forchhammer MC, Bret-Harte MS, Callaghan TV, Christensen TR, Elberling B, et al. Ecological dynamics across the arctic associated with recent climate change. Science. 2009;325:1355–8. doi: 10.1126/science.1173113. [DOI] [PubMed] [Google Scholar]
- 6.Ford JD. Dangerous climate change and the importance of adaptation for the Arctic's Inuit population. Environ Res Lett. 2009;2(2) http://iopscience.iop.org/1748-9326/4/2/024006/ [Google Scholar]
- 7.Prüss-Üstün A, Corvalán C. Preventing disease through healthy environments, Towards an estimate of the environmental burden of disease. Geneva, WHO. 2006. Available from: http://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf [cited 20 March 2012]
- 8.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–69. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- 9.Rijsberman FJ, Swart RJ, editors. Stockholm Environmental Institute; 1990. Targets and indicators of climate change; p. 166. ISBN: 91-88116-21-2. [Google Scholar]
- 10.Lenton TM. Beyond 2°C: redefining dangerous climate change for physical systems. WIREs Clim Change. 2011;2:451–61. [Google Scholar]
- 11.Hansen J, Sato M, Ruedy R, Lo K, Lea DW, Medina-Elizade M. Global temperature change. Proc Natl Acad Sci USA. 2006;103:14288–93. doi: 10.1073/pnas.0606291103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huber M, Knutti R. Anthropogenic and natural warming inferred from changes in Earth's energy balance. Nat Geosci. 2012;5:31–6. [Google Scholar]
- 13.Wigley TM. The climate change commitment. Science. 2005;307:1766–9. doi: 10.1126/science.1103934. [DOI] [PubMed] [Google Scholar]
- 14.Plattner GK. Terrestrial ecosystem inertia. Nat Geosci. 2009;2:467–8. [Google Scholar]
- 15.Ebi KL. Climate change and health risks: assessing and responding to them through ‘adaptive management’. Health Aff (Millwood) 2011;30:924–30. doi: 10.1377/hlthaff.2011.0071. [DOI] [PubMed] [Google Scholar]
- 16.Zhang DD, Lee HF, Wang C, Li B, Pei Q, Zhang J. The causality analysis of climate change and large-scale human crisis. Proc Natl Acad Sci USA. 2011;108:17296–301. doi: 10.1073/pnas.1104268108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogner H, Zhou D, Bradley R, Crabbé P, Edenhofer O, Hare B, et al. Climate change 2007: mitigation. In: Metz B, Davidson OR, Bosch PR, Dave R, Meyer LA, editors. Contribution of working group III to the fourth assessment report of the intergovernmental panel on climate change. Cambridge, UK/New York: Cambridge University Press; 2007. [Google Scholar]
- 18.Bowen KJ, Friel S, Ebi KL, Butler CD, Miller F, McMichael AJ. Governing for a Healthy Population: towards an understanding of how decision-making will determine our global health in a changing climate. Int J Environ Res Public Health. 2012;9:55–72. doi: 10.3390/ijerph9010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sovacool BK, D'Agostino AL, Meenawat H, Rawlani A. Expert views of climate change adaptation in least developed Asia. J Environ Manage. 2012;97:78–88. doi: 10.1016/j.jenvman.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Saving Carbon, Improving Health, NHS carbon reduction strategy for England. 2009. Available from: http://www.sdu.nhs.uk/documents/publications/1237308334_qylG_saving_carbon,_improving_health_nhs_carbon_reducti.pdf [cited 15 March 2012].
- 21.Pencheon D, Rissel CE, Hadfield G, Madden L. Health sector leadership in mitigating climate change: experience from the UK and NSW. New South Wales Public Health Bulletin. 2009;20(12):173–6. doi: 10.1071/NB09044. [DOI] [PubMed] [Google Scholar]
- 22.Health in the green economy. co-benefits to health of climate change mitigation. Health care facilities, Preliminary findings-initial review. 2011. Available from: http://www.who.int/hia/hgebrief_health.pdf [cited 15 March 2012]
- 23.Sustainability in the NHS, Health check. 2012. Available from: http://www.sdu.nhs.uk/publications-resources/89/Sustainability-in-the-NHS-Health-Check-2012/ [cited 22 March 2012].
- 24.Department of Energy and Climate Change. Statistical release, 2011 UK greenhouse gas emissions, provisional figures and 2010 UK greenhouse gas emissions, final figures by fuel type and end-user. 2012. Available from: http://www.decc.gov.uk/assets/decc/11/stats/climate-change/4817-2011-uk-greenhouse-gas-emissions-provisional-figur.pdf [cited 25 April 2012]
- 25.World Health Organization. Safe health-care waste management. 2004 Available from: http://www.healthcarewaste.org/fileadmin/user_upload/resources/WHO-HCWM-policy-paper-2004.pdf [cited 15 March 2012]
- 26.Stott R, Godlee F. What should we do about climate change? Health professionals need to act now, collectively and individually. BMJ. 2006;333:983–4. doi: 10.1136/bmj.39028.427164.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Houghton A. Health impact assessments. A tool for designing climate change resilience into green building and planning projects. J Green Build. 2011;6:66–87. [Google Scholar]
- 28.Younger M, Morrow-Almeida HR, Vindigni SM, Dannenberg AL. The built environment, climate change, and health: opportunities for co-benefits. Am J Prev Med. 2008;35:517–26. doi: 10.1016/j.amepre.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 29.Vine E. Adaptation of California's electricity sector to climate change. Clim Change. 2012;111:75–99. [Google Scholar]
- 30.Omer AM. Renewable building energy systems and passive human comfort solutions. Renew Sust Energ Rev. 2008;12:1562–87. [Google Scholar]
- 31.Fong KF, Chow TT, Lee CK, Lin Z, Chan LS. Solar hybrid cooling system for high-tech offices in subtropical climate – Radiant cooling by absorption refrigeration and desiccant dehumidification. Energy Conv Manag. 2011;52:2883–94. [Google Scholar]
- 32.Short CA, Cook MJ, Woods A. Low energy ventilation and cooling within an urban heat island. Renew Energy. 2009;34:2022–9. [Google Scholar]
- 33.Short CA, Lomas KJ, Woods A. Design strategy for low-energy ventilation and cooling within an urban heat island. Build Res Informat. 2004;32:187–206. [Google Scholar]
- 34.Hanak E, Lund JR. Adapting California's water management to climate change. Clim Change. 2012;111:17–44. [Google Scholar]
- 35.United Nations Educational Scientific and Cultural Organization. Water in a changing world. 2009. Available from: http://unesdoc.unesco.org/images/0018/001819/181993e.pdf [cited 10 March 2012]
- 36.Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg. 2010;111:92–98. doi: 10.1213/ANE.0b013e3181e058d7. [DOI] [PubMed] [Google Scholar]
- 37.Barwise JA, Lancaster LJ, Michaels D, Pope JE, Berry JM. An initial evaluation of a novel anesthetic scavenging interface. Anesth Analg. 2011;113:1064–7. doi: 10.1213/ANE.0b013e31822c9a2c. [DOI] [PubMed] [Google Scholar]
- 38.Yellowlees PM, Chorba K, Parish MB, Wynn-Jones H, Nafiz N. Telemedicine can make healthcare greener. Telemed J e-Health. 2010;16:230–3. doi: 10.1089/tmj.2009.0105. [DOI] [PubMed] [Google Scholar]
- 39.Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8:e1000387. doi: 10.1371/journal.pmed.1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peeters JM, Mistiaen P, Francke AL. Costs and financial benefits of video communication compared to usual care at home: a systematic review. J Telemed Telecare. 2011;17:403–411. doi: 10.1258/jtt.2011.110405. [DOI] [PubMed] [Google Scholar]
- 41.Hailey D, Roine R, Ohinmaa A. Systematic review of evidence for the benefits of telemedicine. J Telemed Telecare. 2002;8:S1–S30. doi: 10.1258/1357633021937604. [DOI] [PubMed] [Google Scholar]
- 42.Wester K, Jonsson AK, Spigset O, Druid H, Hagg S. Incidence of fatal adverse drug reactions: a population based study. Br J Clin Pharmacol. 2008;65:573–9. doi: 10.1111/j.1365-2125.2007.03064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mjorndal T, Boman MD, Hagg S, Backstrom M, Wiholm BE, Wahlin A, et al. Adverse drug reactions as a cause for admissions to a department of internal medicine. Pharmacoepidemiol Drug Saf. 2002;11:65–72. doi: 10.1002/pds.667. [DOI] [PubMed] [Google Scholar]
- 44.Alexopoulou A, Dourakis SP, Mantzoukis D, Pitsariotis T, Kandyli A, Deutsch M, et al. Adverse drug reactions as a cause of hospital admissions: a 6-month experience in a single center in Greece. Eur J Intern Med. 2008;19:505–10. doi: 10.1016/j.ejim.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 45.Hudson HE. Rural telemedicine: lessons from Alaska for developing regions. Telemed J E Health. 2005;11:460–7. doi: 10.1089/tmj.2005.11.460. [DOI] [PubMed] [Google Scholar]
- 46.WWF Sweden. The potential global CO2 reductions from ICT. Identifying and assessing the opportunities to reduce the first billion tonnes of CO2. 2008. Available from: http://www.wwf.se/source.php/1183710/identifying_the_1st_billion_tonnes_ict.pdf [cited 10 March 2012].
- 47.OECD. Towards green ICT strategies: assessing policies and programmes on ICT and the environment. 2009. Available from: http://www.oecd.org/dataoecd/47/12/42825130.pdf [cited 8 March 2012]
- 48.Forge S, Blackman C, Bohlin E, Cave M. Green knowledge society, an ICT policy agenda to 2015 for Europe's future knowledge society. A study for the Ministry of Enterprise, Energy and Communications, Government Offices of Sweden by SCF Associates Ltd. Final Report September 2009. Available from: http://ec.europa.eu/information_society/eeurope/i2010/docs/i2010_high_level_group/green_knowledge_society.pdf [cited 15 March 2012].
- 49.The Climate Group. SMART 2020: enabling the low carbon economy in the information age. A report by The Climate Group on behalf of the Global eSustainability Initiative (GeSI) 2008. 2008. Available from: http://www.gesi.org/LinkClick.aspx?fileticket=tbp5WRTHUoY%3d&tabid=60 [cited 8 March 2012].
- 50.Roeth H, Wokech L. ICTs and climate change mitigation in emerging economies. Centre for Development Informatics, Institute for Development Policy and Management, SED; 2011. Available from: http://www.niccd.org/RoethWokeckClimateChangeMitigationICTs.pdf [cited 9 March 2012]
- 51.Smith AC, Patterson V, Scott RE. Reducing your carbon footprint: how telemedicine helps. BMJ. 2007;335:1060. doi: 10.1136/bmj.39402.471863.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haines A, McMichael AJ, Smith KR, Roberts I, Woodcock J, Markandya A, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet. 2009;374:2104–14. doi: 10.1016/S0140-6736(09)61759-1. [DOI] [PubMed] [Google Scholar]
- 53.Wootton R, Tait A, Croft A. Environmental aspects of health care in the Grampian NHS region and the place of telehealth. J Telemed Telecare. 2010;16:215–20. doi: 10.1258/jtt.2010.004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lewis D, Tranter G, Axford AT. Use of videoconferencing in wales to reduce carbon dioxide emissions, travel costs and time. J Telemed Telecare. 2009;15:137–8. doi: 10.1258/jtt.2009.003010. [DOI] [PubMed] [Google Scholar]
- 55.Masino C, Rubinstein E, Lem L, Purdy B, Rossos PG. The impact of telemedicine on greenhouse gas emissions at an academic health science center in Canada. Telemed J E Health. 2010;16:973–6. doi: 10.1089/tmj.2010.0057. [DOI] [PubMed] [Google Scholar]
- 56.Scott RE, Perverseff T, Lefebre N. Reducing environmental impact: an example of how e-health can reduce environmental impact and concomitantly improve health; Proceedings of The 1st Annual Conference on e-Health: The Virtual Dimensions of Health and Environment—Empower, Enhance, Enforce; 2009. Apr, pp. 101–10. [Google Scholar]
- 57.Gullison RE, Frumhoff PC, Canadell JG, Field CB, Nepstad DC, Hayhoe K, et al. Environment. Tropical forests and climate policy. Science. 2007;316:985–6. doi: 10.1126/science.1136163. [DOI] [PubMed] [Google Scholar]
- 58.Bremer R. Policy development in disaster preparedness and management: lessons learned from the January 2001 earthquake in Gujarat, India. Prehosp Disaster Med. 2003;18:372–84. doi: 10.1017/s1049023x00001345. [DOI] [PubMed] [Google Scholar]
- 59.Preston BL, Stafford-Smith M. Framing vulnerability and adaptive capacity assessment: Discussion paper; 2009. CSIRO Climate Adaptation Flagship Working paper No. 2. [Google Scholar]
- 60.Chan TC, Killeen J, Griswold W, Lenert L. Information technology and emergency medical care during disasters. 2004;11:1229–36. doi: 10.1197/j.aem.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 61.Nicogossian AE, Doarn CR. Armenia 1988 earthquake and telemedicine: lessons learned and forgotten. Telemed J E Health. 2011;17:741–5. doi: 10.1089/tmj.2011.0118. [DOI] [PubMed] [Google Scholar]
- 62.Doarn CR, Merrell RC. Spacebridge to Armenia: a look back at its impact on telemedicine in disaster response. Telemed J E Health. 2011;17:546–52. doi: 10.1089/tmj.2010.0212. [DOI] [PubMed] [Google Scholar]
- 63.Nasu Y, Ashida N, Kanzaki H, Sagawa S, Tsuji M. Efficient health information management systems using wireless communications technology to aid disaster victims. J Med Syst. 2011. http://www.springerlink.com/content/1221u80628k8814m/?MUD=MP. [DOI] [PubMed]
- 64.Kost GJ, Tran NK, Tuntideelert M, Kulrattanamaneeporn S, Peungposop N. Katrina, the tsunami, and point-of-care testing: optimizing rapid response diagnosis in disasters. Am J Clin Pathol. 2006;126:513–520. doi: 10.1309/NWU5E6T0L4PFCBD9. [DOI] [PubMed] [Google Scholar]
- 65.Bollinger RC, McKenzie-White J, Gupta A. Building a global health education network for clinical care and research. The benefits and challenges of distance learning tools. Lessons learned from the Hopkins Center for Clinical Global Health Education. Infect Dis Clin North Am. 2011;25:385. doi: 10.1016/j.idc.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mars M. Health capacity development through telemedicine in Africa. Yearb Med Inform. 2010:87–93. [PubMed] [Google Scholar]
- 67.Mars M. Building the capacity to build capacity in e-health in Sub-Saharan Africa: the KwaZulu-Natal experience. Telemed e-Health. 2012;18:32–7. doi: 10.1089/tmj.2011.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kane S, Shogren JF. Linking adaptation and mitigation in climate change policy. 2000 [Google Scholar]
- 69.Rizwan AM, Dennis YCL, Liu CH. A review on the generation, determination and mitigation of Urban Heat Island. J Environ Sci. 2008;20:120–8. doi: 10.1016/s1001-0742(08)60019-4. [DOI] [PubMed] [Google Scholar]
- 70.Jennett P, Yeo M, Pauls M, Graham J. Organizational readiness for telemedicine: implications for success and failure. J Telemed Telecare. 2003;9:S27–S30. doi: 10.1258/135763303322596183. [DOI] [PubMed] [Google Scholar]
- 71.Martiniuk A, Negin J, Hersch F, Dalipanda T, Jagilli R, Houasia P, et al. Telemedicine in the Solomon Islands: 2006 to 2009. J Telemed Telecare. 2011;17:251–6. doi: 10.1258/jtt.2011.100920. [DOI] [PubMed] [Google Scholar]
- 72.Cheng KG, Ernesto F, Ovalle-Bahamon RE, Truong KN. Barriers to acceptance of personal digital assistants for HIV/AIDS data collection in Angola. Int J Med Inform. 2011;80:579–85. doi: 10.1016/j.ijmedinf.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Desai D, Wu G, Zaman MH. Tackling HIV through robust diagnostics in the developing world: current status and future opportunities. Lab Chip. 2011;11:194–211. doi: 10.1039/c0lc00340a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Safety and security on the Internet. Challenges and advances in Member States. Global Observatory for eHealth series. 2011;4 Available from: http://www.who.int/goe/publications/goe_security_web.pdf [cited 15 March 2012]. [Google Scholar]
- 75.DeNardis L. Standards and eHealth. ITU-T Technology Watch Report 2011. Available from: http://www.itu.int/dms_pub/itu-t/oth/23/01/T23010000120003PDFE.pdf [cited 23 March 2012].
- 76.Lang A, Mertes A. E-health policy and deployment activities in Europe. Telemed e-Health. 2011;17:262–8. doi: 10.1089/tmj.2010.0174. [DOI] [PubMed] [Google Scholar]
- 77.Farberow B, Hatton V, Leenknecht C, Goldberg LR, Hornung CA, Reyes B. Caveat emptor: the need for evidence, regulation, and certification of home telehealth systems for the management of chronic conditions. Am J Med Qual. 2008;23:208–14. doi: 10.1177/1062860608315123. [DOI] [PubMed] [Google Scholar]