Abstract
Background
Clinical practice guidelines have been criticized for paying insufficient attention to the unique needs of patients with advanced age and multiple comorbid conditions. However, little empiric research is available to inform this topic.
Methods
We conducted telephone interviews with staff physicians and nurse practitioners in 4 VA health care systems. Respondents were asked to rate the usefulness of national heart failure guidelines for patients of different ages and levels of comorbid burden on a five point scale and to comment on the reasons for their ratings.
Results
Among 139 clinicians contacted, 65 (47%) completed the interview. Half (49%) were women and 48 (74%) were general internists or family practitioners. On a five-point scale assessing the usefulness of clinical practice guidelines for heart failure, the mean response ranged from 4.4 (+/− 0.7) for patients age <65 years with few comorbidities to 3.5 (+/− 1.2) for patients age >80 years with multiple comorbidities (P<.001). The difference in perceived usefulness varied more by patient age than by the degree of comorbidity (P=.02). Four major concepts underlay the perceived utility of guidelines across different patient types: (a) harms of treatment and patients’ clinical and pharmacologic complexity; (b) expected benefits of treatment; (c) patient preferences and abilities; and (d) confidence in the validity of guideline recommendations.
Conclusions
Clinicians perceive heart failure guidelines to be substantially less useful for patients with older age and greater comorbid burden. Concerns about the clinical and pharmacologic complexity of these patients and the expected benefits of drug therapy were commonly invoked as reasons for this skepticism.
Keywords: clinical practice guidelines, physician attitudes, aged, geriatrics, comorbidity
Introduction
Research on clinician attitudes toward guidelines has played an important role in guideline implementation, as understanding barriers to guideline-recommended care can inform which interventions are most likely to improve adherence to those care practices.1–3
Prior studies have identified a wide variety of factors that underlie clinician attitudes and practices toward guidelines. 4–8 Many of these factors are attributes of clinicians and the health care system, for example clinicians’ confidence in the validity of guideline recommendations and systemic barriers to accessing care.3,7–8 However, patient characteristics have also emerged as important predictors of clinician attitudes toward guidelines, with several studies noting clinician concerns over the appropriateness and feasibility of applying guideline-based care plans to patients with advanced age and multiple comorbidities. 4,6,9 These concerns likely contribute to observed variations in care, as older patients (although not necessarily those with multiple chronic conditions) are less likely to receive guideline-concordant care for a number of common diseases.10–13
Despite documented concerns about applying guidelines to multimorbid older adults, little previous work has quantified the extent to which clinician attitudes toward guidelines vary across patients of different ages and with different levels of comorbid burden, and few studies have systematically explored the reasons that underlie clinician skepticism toward guidelines in these patients.14 To better understand these issues, we conducted a mixed-methods study investigating clinician attitudes about the usefulness of heart failure guidelines for patients with different ages and degrees of comorbid burden. We chose heart failure as a model system because the disease is common, guidelines for care are widely disseminated, and these guidelines recommend a multiplicity of medications with substantial benefits and harms.
Methods
Participants
This study was conducted as part of a telephone-based clinician interview study which aimed to understand why clinicians did not prescribe guideline-recommended medications for heart failure to specific patients under their care. Using computerized clinical data and chart review from VA health care systems in San Francisco, Iowa City, San Antonio, and West Haven, CT (included the parent medical center and outlying community clinics), we identified all outpatients who had heart failure with ejection fraction <=40% and were not receiving angiotensin-blocking medications (ACE inhibitors or angiotensin receptor blockers) or beta blockers. Our study sample comprised the primary care clinicians for these patients – that is, a complete sample of all primary care clinicians at each medical center who cared for at least one outpatient who had systolic heart failure and was not receiving ACE inhibitors/angiotensin receptor blockers and/or beta blockers. Given difficulty contacting the 25 fellows and residents we identified, these trainees were excluded and only staff physicians and nurse practitioners were included for the telephone-based interviews.
Measurements and data collection
The survey questions were organized into 3 sections. First, we collected basic demographic information about the clinicians. Second, we asked them to rate the usefulness of national heart failure guidelines for 4 types of patients: (1) patients age less than 65 years with few comorbidities; (2) patients age less than 65 years with multiple comorbidities; (3) patients over age 80 years with few comorbidities; and (4) patients over age 80 years with multiple comorbidities. (In asking these questions, we used the phrases “few comorbidities” and “multiple comorbidities” without specifically operationalizing these terms). Respondents rated the usefulness of heart failure guidelines on a 5-point Likert scale, with anchors of 1 (not at all useful) and 5 (extremely useful). Next, we used an open-ended question to ask respondents why they gave similar or different ratings of guideline usefulness across patients of different age and comorbid burden (e.g., “tell me why you believe that heart failure guidelines are less useful in older patients [and/or] patients with multiple comorbidities”). One clinician had missing data from one patient type. In addition, we were unable to use audio transcripts and thus perform qualitative coding for 2 respondents.
Quantitative analyses
For descriptive purposes, we present results of our Likert scale analyses as means. We used the Wilcoxon signed-rank test to assess differences in the perceived usefulness of guidelines between the youngest/healthiest patient type and the oldest/sickest patient type. To evaluate whether perceived guideline usefulness varied more by patient age or comorbidity, we used ANOVA-based approaches that accounted for repeated measures within study subjects. In doing so, we tested potential interaction effects between patient age and comorbidity. This interaction term did not approach statistical significance (P=0.24), so we did not include it in the final model. All quantitative analyses were conducted using Stata 11 (StataCorp, College Station, TX).
Qualitative Analyses
Interview data were analyzed using content analysis, in which we sought to create a taxonomy of reasons why the usefulness of heart failure guidelines was perceived to be similar or different across patients with varying ages and degrees of comorbid burden.15 To create this taxonomy, two trained research assistants (CP and JAH) independently reviewed 20 interviews across the 4 study sites and identified concepts that emerged from participant responses. The study team then reviewed these concepts to clarify and separate or merge related ideas in order to create a preliminary coding scheme with operational definitions. The research assistants then independently tested this scheme on the initial batch of 20 interviews, focusing on areas where the preliminary scheme failed to capture and adequately distinguish between concepts expressed in the data, lacked definitional clarity, or resulted in discordant results between the independent coders. We then revised the concepts and operational definitions of the coding scheme and retested it on the initial set of interviews plus additional interviews at one of the study sites. After additional minor revisions, the two reviewers then independently applied the coding scheme on the full set of interviews. Disagreements between reviewers were resolved by consensus, with final adjudication by the principal investigator when agreement could not be reached. On the final set of independently-coded reviews (i.e., not part of our test set), reviewers had complete agreement in 83% of interviews in identifying which major domains were discussed. Partial agreement (i.e. agreement on some but not all domains) occurred in 7% of interviews, and no agreement in 10%.
This research was approved by the institutional review boards at the San Francisco, Iowa City, South Texas, and West Haven VA Medical Centers and at the University of California, San Francisco, the University of Iowa, the University of Texas Health Science Center at San Antonio, and Yale University.
Results
Characteristics of subjects
We identified 153 staff physicians and nurse practitioners who provided care for patients in our heart failure cohort. Among these 153 clinicians, 14 had no identifiable contact information. Among the remaining 139 clinicians, 65 (47%) completed the interview. Response rates ranged from 33% to 56% at each site, and were similar for physician and nurse practitioners (58/119 for physicians vs. 7/20 for nurse practitioners, P=0.25). Half (49%) of respondents were women, and the mean time since professional school graduation was 20 (+/-10) years (Table 1).
Table 1.
Characteristics of clinicians
| Characteristic | N(%) |
|---|---|
| Clinician type | |
| Physician | 58 (89%) |
| Nurse practitioner | 7 (11%) |
| Female sex | 32 (49%) |
| Clinician specialty | |
| Internal medicine or family practice | 48 (74%) |
| Geriatrics | 9 (14%) |
| Other or >1 specialty listed | 8 (12%) |
| Years since professional school graduation | |
| 0–10 | 12 (18%) |
| 11–20 | 23 (35%) |
| >20 | 30 (46%) |
| Number of days in clinic per week (median, IQR) | 5 (3.5, 5) |
IQR, interquartile range
Attitudes toward guidelines
On average, clinicians rated guidelines as being less useful in patients with higher age and comorbid burden (Figure 1). While increasing age and comorbid burden were each independently associated with more skeptical perceptions of guideline usefulness (P<.01 for each), the effect was more pronounced for patient age than for degree of comorbidity. On a five-point Likert scale, the difference in perceived usefulness of guidelines was a mean of 0.6 points lower in older patients than in younger ones, compared with a mean of 0.3 points lower in patients with many comorbidities than in those with few comorbidities (P=.02 for difference between age effects and comorbidity effects).
Figure 1. Clinician attitudes about the usefulness of heart failure guidelines for different types of patients.
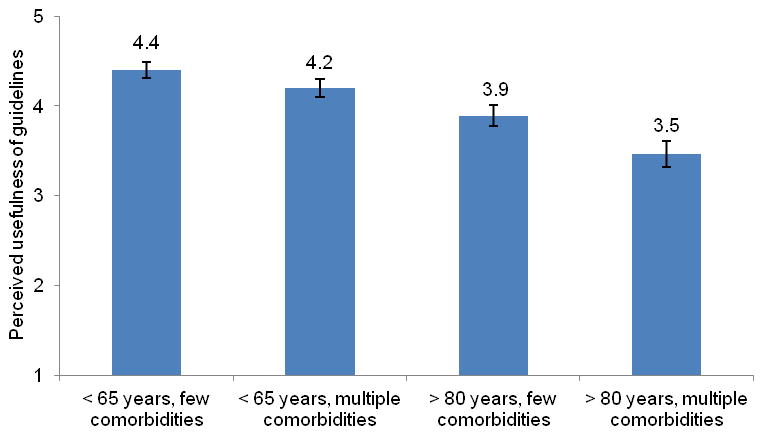
Attitudes toward guidelines were measured on a 5 point scale, from 1 (not at all useful) to 5 (extremely useful). Bars show the mean response for each patient type; error bars show standard error around the mean.
Among 64 clinicians with complete data, 20 (31%) stated that guidelines had similar usefulness across all patient types. In contrast, 36 (56%) rated guidelines as being less useful as patient age and comorbid increased, 6 (9%) rated guidelines as more useful as age and comorbid burden increased, and 2 (3%) reported a mixed pattern.
Next, for each subject we calculated the mean rating of guideline usefulness across all 4 patient types. Respondents who believed that guidelines were equally useful across all patient types had a higher overall rating of guideline usefulness compared with respondents who gave different answers for the patient types (median rating 4.00 vs. 3.75, P=.02).
Reasons for similarities or differences in perceived guideline usefulness for patients of different ages and comorbid burden
Respondents’ answers to the open-ended question of how increasing patient age and comorbid burden affected their attitudes toward guidelines fell into 4 broad domains. These domains included (1) harms and complexity of applying guideline-concordant care, (2) expectation of decreased benefit from treatment, (3) patient preferences and abilities, and (4) confidence in the validity of guideline recommendations. The first three domains were cited only by respondents who believed that guidelines were less useful in patients with greater age and/or comorbid burden. In contrast, the fourth domain was cited both by these respondents and also by those who believed that guidelines were equally applicable across all patient types (Table 2). In addition, we identified a recurring theme relating to individualization of care which cut across all four domains, described in further detail below.
Table 2.
Reasons for perceived similarities or differences in guideline usefulness across a spectrum of age and comorbid burden
| Domain (sub-domain) | Subjects perceiving differences in usefulness of guidelines for different patient types (N=42) N(%) |
Subjects perceiving equal usefulness of guidelines for different patient types (N=20) N(%) |
|---|---|---|
| Harms and complexity | 29 (69%) | 0 (0%) |
| Harms | 11 | |
| Complexity | 14 | |
| Mix of harms/complexity | 8 | |
| Benefits of therapy | 15 (36%) | 0 (0%) |
| Patient preferences and abilities | 7 (17%) | 0 (0%) |
| Patient preferences | 3 | |
| Patient abilities | 5 | |
| Confidence in guideline validity | 7 (17%) | 12 (60%) |
| Other discrete reason | 3 (7%) | 2 (10%) |
| No discernible reason | 5 (12%) | 6 (30%) |
Totals add to >100% because some subjects cited 2 or more domains or sub-domains. “Mix” reflects answers where sub-domains were tightly interwoven.
Qualitative data not available for 2 subjects, and 1 subject provided incomplete ratings for the 4 patient types, precluding assessment of perceived differences in guideline usefulness.
Domain 1: Harms and complexity of applying guideline-concordant care to patients with increasing age and/or comorbidity
This domain included two concepts – harms and complexity – which were often, but not universally, intertwined in respondents’ comments. The first of these concepts focused on the potential harms of heart failure therapy. Respondents expressed concern that older patients and those with multiple comorbidities were more likely to suffer harms from aggressive, guideline-based treatments than younger patients without multimorbidity. One clinician stated:
“We’re so worried about falls, many times they run low heart rates at baseline, so when you add certain agents you can create problems for older adults by trying to follow guidelines too assiduously.”
The concept of harm was often discussed in the context of multimorbidity, polypharmacy, and other forms of clinical complexity. In some interviews, harms were directly attributed to these complexities, with the concepts of harm and complexity tightly interwoven in respondent comments. In others, respondents primarily focused on complexity, providing only an implied link between patient complexity and increased likelihood of harm. For example, one clinician noted that:
“In patients with multiple co-morbidities which require multiple medications, the issue of polypharmacy becomes an overriding guide to therapy and I think trumps the guidelines for specific disease management.”
Similarly, a number of respondents stated that guidelines were less useful for clinically complex patients, but were nonspecific in articulating why. As one clinician stated:
“Because they have multiple co-morbidities … you are balancing lots of other factors, so the guidelines are going to be set for optimum situations and someone with multiple co- morbidities are not going to be optimum”.
Of note, 11 of 29 (38%) of clinicians who cited the domain of “harms and complexity” also discussed issues related to diminished benefits of treatment (see Domain 2). In many cases, this was discussed in terms of a risk-benefit framework in which the ratio of potential benefits to potential risks varied across different types of patients.
Domain 2: Expectation of decreased benefit from treatment in patients with increasing age and/or comorbidity
This domain reflected a belief that the benefits of aggressive, guideline-concordant heart failure treatment are diminished in patients with older age and multimorbidity. In a number of responses, limited life expectancy was cited as a reason for the expectation of decreased benefit. As one respondent commented:
“The more comorbidities and the more frail the patient is, the less likely they are to benefit from any additional medication. They have so many life-limiting illnesses”.
Domain 3: Patient preferences and abilities
This domain included two concepts – patient preferences, and practical issues such as adherence. These concepts, while distinct, are interrelated insofar as patient preferences can affect their medication adherence and motivation to overcome practical barriers to medication use. For the first concept (patient preferences), several clinicians noted that preferences may shift as patients get older and accumulate comorbid burden, which affects the usefulness of guidelines for managing their care. For example, one respondent said:
“As patients get more medically complex, there are issues outside of heart failure that need to be addressed, so there could be…goals of care that override what the guidelines say…. As other things come into the picture the guidelines really become less of detailed map and more of just a starting point.”
Regarding the concept of practical issues, several clinicians stated that guidelines were less useful in patients with older age and/or comorbid burden because of problems with these patients’ ability to adhere to treatment recommendations (e.g., due to visual or cognitive impairment) and to closely monitor drug side effects.
“So the more comorbidities, the less I want to prescribe [because] it becomes really hard for the patients to remember to take the medications and take them in a timely manner.…They are not able to hear, they are not able to see well, they are not able to communicate well, the memory goes down. So it just becomes impossible”.
Domain 4: Confidence in the validity of guideline recommendations
The final domain concerned the evidence basis of guidelines and their validity as a “gold-standard” reference. Several clinicians who believed that heart failure guidelines were less useful in older and more complex patients noted gaps in the evidence base for these patients. In doing so, they noted skepticism that evidence from clinical trials conducted in younger, less clinically complex populations applied to older, more complex patients. As one clinician noted:
“The guidelines are generally directed to people in a certain age bracket and the outliers are the very young and the very old. Clinical trials don’t have 80 year-olds in them.”
This same idea of confidence in guideline recommendations was also cited by clinicians who rated guidelines as equally useful for all patient types (Table 2). However, instead of criticizing the validity of guidelines, these clinicians highlighted the opinion that guidelines represent a gold standard of evidence-based care and should be treated as such regardless of patient age or comorbid burden. One such clinician stated:
“Most guidelines are based on evidence based medicine and I think that it’s important to apply evidence based medicine to the care of patients, particularly to heart failure where we have lots of studies giving us a way to go.”
Cross-cutting theme - individualization of care
In addition to the four discrete domains, we identified a cross-cutting theme relating to the need to individualize care by adapting guideline recommendations to the unique circumstances of each patient. This broad-based theme was exceedingly prevalent, occurring in 48 (76%) interviews. It was commonly cited by clinicians mentioning each of the 4 domains, and by clinicians who did and did not believe that the usefulness of guidelines differed by patient age and comorbidity.
Among respondents who believed that guideline usefulness differed across patients of different ages and comorbid burden, age and comorbidity were commonly cited as reasons that care needed to be individualized, although a more general proclivity to individualization was also discussed. For example, one such respondent stated:
“Each patient is a unique situation and is not going to be the same as another patient. So we cannot go by the universal guidelines. We have to go by the individual patient, by the patient’s comfort, how is he feeling and how is he doing”.
Among respondents who believed that guidelines were similarly useful across patient types, many stated that individualization was important for all patients. However, they did not frame the need to individualize care as being disproportionately influenced by age or comorbid burden. As one such clinician commented:
“I think the guidelines in heart failure are very helpful, [but] that doesn’t change the fact that I have to individualize it to the patient. Whether they are young, old, or have comorbidities or don’t have comorbidities, I have to look at the whole picture. The guideline is an isolated piece of evidence that then has to be incorporated into that patient’s individual health care status.”
Discussion
In this mixed-methods study, we found that many clinicians believed that the usefulness of heart guidelines varied substantially across patients with different ages and degrees of comorbid burden. Over half of respondents stated that guidelines were less useful as patients got older and/or accumulated greater comorbid burden, with age exerting a greater effect on attitudes than level of comorbid burden. We identified 4 major domains of reasons why clinicians believed the usefulness of heart failure guidelines differed across these factors, including concern about medication harms and clinical complexity, the expected benefits of treatment, patient preferences and ability to adhere to complex medication regimens, and concerns about the validity and evidence basis of guidelines. In addition, more than three-quarters of respondents mentioned the importance of individualizing therapy – including a large number of respondents who felt that guidelines were equally applicable for different types of patients, noting that individualization is important for all patients and not just those who are old and clinically complex.
Our main finding – that the perceived usefulness of heart failure guidelines declines substantially as age and comorbid burden increase – suggests dissatisfaction among clinicians for how guidelines help them manage these vulnerable populations. One prominent area that respondents highlighted was an expectation of lower benefits and greater harms of aggressive therapy in older, clinically complex patients. Although this shifting ratio of benefits to harms has been observed in the setting of aggressive glycemic control for older adults with diabetes, existing data are more reassuring for the care of older heart failure patients.16–18 The SENIORS trial and other studies suggest that the benefits and tolerability of angiotensin inhibition and beta blockers persist into older age. 19–24 However, while these reassuring findings for the treatment of heart failure in the old-old merit discussion and dissemination, the great heterogeneity of health status and comorbid burden among older adults creates uncertainty about the applicability of findings from any clinical trial to a given individual patient.19,25 Thus, many clinicians may reasonably question the applicability of results from heart failure trials – even those conducted in older adults - to different types of older adults (e.g., older adults with different life expectancies, patterns of comorbid illness, frailty and functional status, and goals of care)
As a result, guidelines for heart failure may be most useful when they augment their standard treatment recommendations with a suggested approach to decision-making for older adults that provides guidance on prioritizing care, accounting for comorbid conditions, and factoring in the role of estimated life expectancy in deciding which standard treatment options are or are not warranted for an individual patient.26–27 This approach requires development of a broad, widely endorsed framework for balancing benefits and harms of disease treatments in older, clinically complex patients that can be incorporated into guidelines for specific diseases. 14,28–29
One interesting finding was that patient age had a bigger impact on clinician attitudes than did comorbid burden. Our study was not designed to precisely quantify the relative contribution of each characteristic toward clinician attitudes, and we did not directly inquire about the relative role of each in decision-making. However, it is possible that physicians may in part have envisioned age as a proxy for comorbidity, frailty, geriatric syndromes, and patient attitudes. 30 A number of clinicians’ statements appeared to conflate age and comorbid burden (often along the lines that in older patients one needs to account for other comorbidities). Similarly, some of the patient characteristics that clinicians cited as situations in which guidelines are less useful, such as visual and cognitive impairment, may have been considered a part of old age rather than as separate phenomena. To that extent, greater physician education may be needed to disentangle the respective prognostic implications of age, comorbid burden, and geriatric syndromes (including frailty) to help guide best practices for decision-making.31
Our study has several limitations. While we surveyed clinicians from 4 geographically dispersed sites, including both hospital- and community-based clinic settings, it is unclear how our results generalize to clinicians outside the VA health care system or to conditions other than heart failure. In addition, our interview protocol did not aggressively probe clinician attitudes beyond their open-ended responses, limiting our ability to conduct more in-depth explorations of clinician beliefs and opinions. Third, although the basic tenets of heart failure guidelines are widely known, we did not assess how accurately clinicians understood the actual content of heart failure guidelines. There is also the potential for training bias in our coding of reasons for non-prescribing, insofar as the subset of the interviews used to develop our coding scheme and train coders were also included in the final data analysis. Finally, clinicians may fail to distinguish between guidelines and performance measures, which lack the subtlety of guidelines and formulate relatively simplistic assessments of appropriate vs. inappropriate care.
The burden of heart failure falls disproportionately on older and clinically complex patients, yet clinicians believe that guidelines for heart failure management are less useful in these groups. Our findings suggest that guidelines are not meeting the needs of clinicians for these populations. Thoughtful, evidence-based approaches that help guide clinicians on how to individualize care are likely to help address this usefulness gap, and should be a priority as guidelines are updated and developed.
Acknowledgments
The authors thank Laura Goldbaum, RN, for her assistance conducting the telephone interviews, and Mary Jo Pugh, RN, PhD, Peter Kaboli, MD, and Lynne Iannone, MS for their assistance with study planning and regulatory considerations.
Support:
This research was supported by the VA Health Services Research and Development Service (IAF 06-080-02, Dr. Steinman and CD2 07-025-3, Dr. Sudore) and by the National Institute on Aging (K23 AG030999, Dr. Steinman and K24 AG028443, Dr. Fried), the American Federation for Aging Research (K23 AG030999, Dr. Steinman), and the National Palliative Care Research Center (Dr. Sudore).
Footnotes
Conflicts of interest
None of the authors has financial conflicts of interest with the content discussed in this manuscript.
Access to data:
Dr. Steinman had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior presentation:
This research was presented at the Society of General Internal Medicine Annual Meeting, Phoenix, May 2011
The funders had no role in the design, analysis, interpretation, or decision to publish this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) Circulation. 2010;122(6):585–596. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]
- 2.Forman DE, Cannon CP, Hernandez AF, Liang L, Yancy C, Fonarow GC. Influence of age on the management of heart failure: findings from Get With the Guidelines-Heart Failure (GWTG-HF) Am Heart J. 2009;157(6):1010–1017. doi: 10.1016/j.ahj.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. Jama. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 4.Powell-Cope GM, Luther S, Neugaard B, Vara J, Nelson A. Provider-perceived barriers and facilitators for ischaemic heart disease (IHD) guideline adherence. J Eval Clin Pract. 2004;10(2):227–239. doi: 10.1111/j.1365-2753.2003.00450.x. [DOI] [PubMed] [Google Scholar]
- 5.Kasje WN, Denig P, de Graeff PA, Haaijer-Ruskamp FM. Perceived barriers for treatment of chronic heart failure in general practice; are they affecting performance? BMC Fam Pract. 2005;6(1):19. doi: 10.1186/1471-2296-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasje WN, Denig P, Stewart RE, de Graeff PA, Haaijer-Ruskamp FM. Physician, organisational and patient characteristics explaining the use of angiotensin converting enzyme inhibitors in heart failure treatment: a multilevel study. Eur J Clin Pharmacol. 2005;61(2):145–151. doi: 10.1007/s00228-005-0897-6. [DOI] [PubMed] [Google Scholar]
- 7.Hickling JA, Nazareth I, Rogers S. The barriers to effective management of heart failure in general practice. Br J Gen Pract. 2001;51(469):615–618. [PMC free article] [PubMed] [Google Scholar]
- 8.Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta-synthesis of GPs’ attitudes to clinical practice guidelines. Br J Gen Pract. 2007;57(545):971–978. doi: 10.3399/096016407782604820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuat A, Hungin AP, Murphy JJ. Barriers to accurate diagnosis and effective management of heart failure in primary care: qualitative study. Bmj. 2003;326(7382):196. doi: 10.1136/bmj.326.7382.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhry SI, Berlowitz DR, Concato J. Do age and comorbidity affect intensity of pharmacological therapy for poorly controlled diabetes mellitus? J Am Geriatr Soc. 2005;53(7):1214–1216. doi: 10.1111/j.1532-5415.2005.53370.x. [DOI] [PubMed] [Google Scholar]
- 11.Sinha S, Goldstein M, Penrod J, et al. Brief report: beta-blocker use among veterans with systolic heart failure. J Gen Intern Med. 2006;21(12):1306–1309. doi: 10.1111/j.1525-1497.2006.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356(24):2496–2504. doi: 10.1056/NEJMsa066253. [DOI] [PubMed] [Google Scholar]
- 13.Min LC, Wenger NS, Fung C, et al. Multimorbidity is associated with better quality of care among vulnerable elders. Med Care. 2007;45(6):480–488. doi: 10.1097/MLR.0b013e318030fff9. [DOI] [PubMed] [Google Scholar]
- 14.Fried TR, Tinetti ME, Iannone L. Primary care clinicians’ experiences with treatment decision making for older persons with multiple conditions. Arch Intern Med. 2011;171(1):75–80. doi: 10.1001/archinternmed.2010.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenfield S, Billimek J, Pellegrini F, et al. Comorbidity affects the relationship between glycemic control and cardiovascular outcomes in diabetes: a cohort study. Ann Intern Med. 2009;151(12):854–860. doi: 10.7326/0003-4819-151-12-200912150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Huang ES, Zhang Q, Gandra N, Chin MH, Meltzer DO. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med. 2008;149(1):11–19. doi: 10.7326/0003-4819-149-1-200807010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51(5 Suppl):S265–280. doi: 10.1046/j.1532-5415.51.5s.1.x. Guidelines. [DOI] [PubMed] [Google Scholar]
- 19.Scott IA, Guyatt GH. Cautionary tales in the interpretation of clinical studies involving older persons. Arch Intern Med. 2010;170(7):587–595. doi: 10.1001/archinternmed.2010.18. [DOI] [PubMed] [Google Scholar]
- 20.Dulin BR, Krum H. Drug therapy of chronic heart failure in the elderly: the current state of clinical-trial evidence. Curr Opin Cardiol. 2006;21(4):393–399. doi: 10.1097/01.hco.0000231411.15049.20. [DOI] [PubMed] [Google Scholar]
- 21.Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS) Eur Heart J. 2005;26(3):215–225. doi: 10.1093/eurheartj/ehi115. [DOI] [PubMed] [Google Scholar]
- 22.Erdmann E, Lechat P, Verkenne P, Wiemann H. Results from post-hoc analyses of the CIBIS II trial: effect of bisoprolol in high-risk patient groups with chronic heart failure. Eur J Heart Fail. 2001;3(4):469–479. doi: 10.1016/s1388-9842(01)00174-x. [DOI] [PubMed] [Google Scholar]
- 23.Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344(22):1651–1658. doi: 10.1056/NEJM200105313442201. [DOI] [PubMed] [Google Scholar]
- 24.Deedwania PC, Gottlieb S, Ghali JK, Waagstein F, Wikstrand JC. Efficacy, safety and tolerability of beta-adrenergic blockade with metoprolol CR/XL in elderly patients with heart failure. Eur Heart J. 2004;25(15):1300–1309. doi: 10.1016/j.ehj.2004.05.022. [DOI] [PubMed] [Google Scholar]
- 25.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 26.Reuben DB. Medical care for the final years of life: “When you’re 83, it’s not going to be 20 years”. JAMA. 2009;302(24):2686–2694. doi: 10.1001/jama.2009.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tinetti ME, Bogardus ST, Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351(27):2870–2874. doi: 10.1056/NEJMsb042458. [DOI] [PubMed] [Google Scholar]
- 28.Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. Jama. 2001;285(21):2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 29.Fried TR, Tinetti M, Agostini J, Iannone L, Towle V. Health outcome prioritization to elicit preferences of older persons with multiple health conditions. Patient Educ Couns. 2011;83(2):278–282. doi: 10.1016/j.pec.2010.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296(19):2336–2342. doi: 10.1001/jama.296.19.2336. [DOI] [PubMed] [Google Scholar]
- 31.Steinman MA, Lund BC, Miao Y, Boscardin WJ, Kaboli PJ. Geriatric conditions, medication use, and risk of adverse drug events in a predominantly male, older veteran population. J Am Geriatr Soc. 2011;59(4):615–621. doi: 10.1111/j.1532-5415.2011.03331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


