Abstract
Background
We studied the characteristics of ST-elevation myocardial infarction (STEMI) patients from a local acute coronary syndrome (ACS) registry in order to find and build an appropriate acute myocardial infarction (AMI) system of care in Jakarta, Indonesia.
Methods
Data were collected from the Jakarta Acute Coronary Syndrome (JAC) registry 2008–2009, which contained 2103 ACS patients, including 654 acute STEMI patients admitted to the National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Results
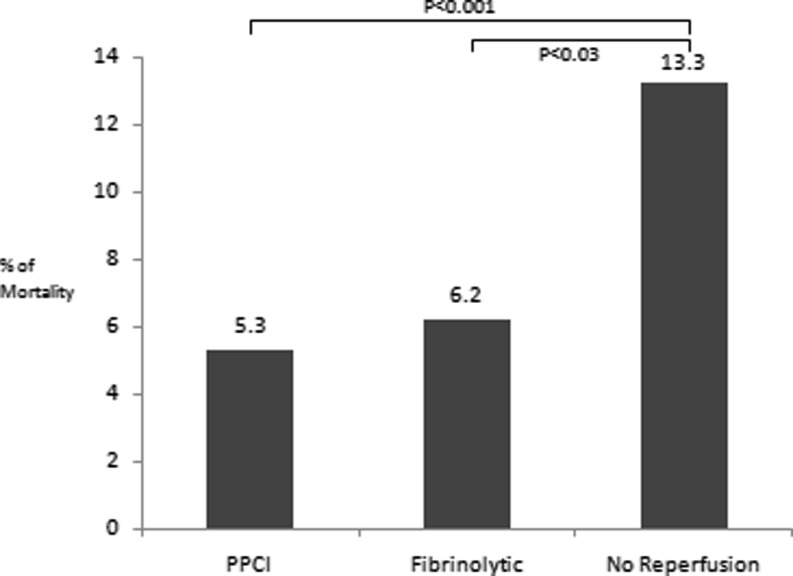
The proportion of patients who did not receive reperfusion therapy was 59% in all STEMI patients and the majority of them (52%) came from inter-hospital referral. The time from onset of infarction to hospital admission was more than 12 h in almost 80% cases and 60% had an anterior wall MI. In-hospital mortality was significantly higher in patients who did not receive reperfusion therapy compared with patients receiving acute reperfusion therapy, either with primary percutaneous coronary intervention (PPCI) or fibrinolytic therapy (13.3% vs 5.3% vs 6.2%, p < 0.001).
Conclusion
The Jakarta Cardiovascular Care Unit Network System was built to improve the care of AMI in Jakarta. This network will harmonise the activities of all hospitals in Jakarta and will provide the best cardiovascular services to the community by giving two reperfusion therapy options (PPCI or pharmaco-invasive strategy) depending on the time needed for the patient to reach the cath-lab.
Keywords: ST-elevation myocardial infarction, System of care, Pharmaco-invasive strategy
Introduction
Tremendous progress has been made in the management of patients with ST-elevation myocardial infarction (STEMI) over the last 20 years [1, 2]. Primary percutaneous coronary intervention (PPCI) is the preferred option for treating STEMI patients. Offering an easy, direct and fast access to this procedure is still difficult due to geographic and structural differences in medical services [3], especially in developing countries. Therefore, each community should find their own system of care of acute myocardial infarction (AMI) based on their AMI characteristics and emergency medical services availability.
The cardiovascular mortality rate in Indonesia is increasing over the years, reaching almost 30% in 2004 compared with only 5% in 1975 [4]. Recently, data from the National Health Survey of Indonesia, which was performed by the Ministry of Health, Republic of Indonesia, showed that cerebro-cardiovascular disease is the leading cause of death in Indonesia [5]. A 13-year cohort study in three districts in the Jakarta province showed that coronary artery disease is the leading cause of mortality in Jakarta, the capital city of Indonesia [6].
Jakarta is a big metropolitan city with its unique multicultural atmosphere. About 11 million people live in Jakarta with 15,000 people/km2 of density [7]. Recently, traffic congestion has become a serious problem in the community and it is the most common cause of time delay for giving acute reperfusion therapy [8].
Efforts should be made to decrease the cardiovascular disease burden by improving primary and secondary health care. The data from the local ACS registry are very important. They will provide feedback and generate new ideas on how to improve the system of care of ACS and find the most appropriate AMI care system in Jakarta. This article will review the system of care of STEMI patients in the real-world situation in Jakarta, Indonesia, based on a local ACS registry.
Patients and methods
Data were derived from the Jakarta Acute Coronary Syndrome (JAC) Registry database (single-centre registry) from the year 2008–2009, which contained 2103 ACS patients, including 654 acute STEMI patients who were admitted to the National Cardiovascular Center Harapan Kita (NCCHK), Jakarta, Indonesia. The NCCHK acts as a national referral hospital with 24-h cardiovascular services including PPCI capabilities. For PPCI cases, the interventional cardiologist will arrive at the cath-lab in less then 30 min after the first call, whereas cath-lab nurses and radiology staff are available 24 h a day in the hospital. The numbers of PCI cases and operator volume were according to the ACC/AHA guideline recommendations.
For all patients, the initial diagnosis was made based on the history of typical chest pain and the finding of ST-segment elevation on the initial ECG. Time to hospital admission was defined as the time between the onset of chest pain and admission to the emergency department (ED) of NCCHK. All information on demographic characteristics, medical history including physical examination and treatment options were collected from a standardised ACS registry form.
Acute adjunctive therapy was given in the ED using the doses recommended by the ESC and ACC/AHA guidelines.
Statistical methods
Continuous data are presented as mean ± standard deviation or median if the distribution is abnormal. Categorical variables are presented as number and percentages. Chi-square test is used to evaluate differences between two variables. P-value < 0.05 was considered significant. All statistical analysis was performed using statistical package.
Results
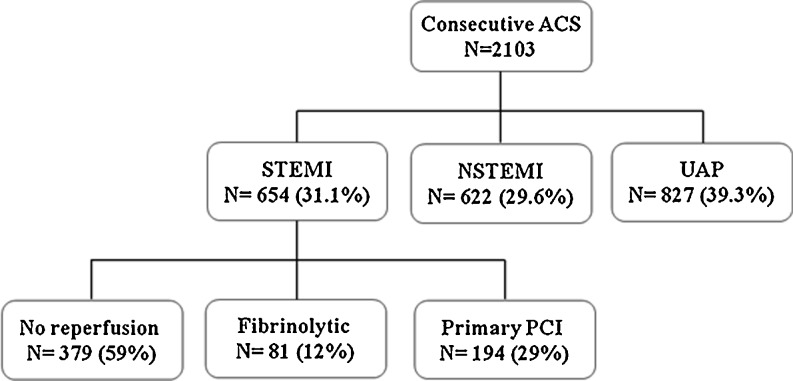
There were 9634 patients admitted to the ED in the year 2009, and ACS was diagnosed in 3402 patients (35%). A valid and complete database was observed and 2103 patients were eligible for analysis (Fig. 1).
Fig. 1.
Patient distribution from the Jakarta Acute Coronary Syndrome registry NSTEMI Non-ST elevation myocardial infarction, UAP unstable angina pectoris
The mean age of the ACS patients was 57.6 ± 10.2 years, of which 77.7% were male and Javanese was the most common race affected (31.5%). Hypertension was the most common risk factor (66%). Most of patients came to the ED by themselves. The characteristics of STEMI patients are listed in Table 1.
Table 1.
Characteristics of STEMI patients (N = 654)
| Variable | Description |
|---|---|
| Location of STEMI, N (%) | |
| - Anterior | 388 (60%) |
| - Non-anterior | 266 (40%) |
| Killip class, N (%) | |
| - I | 439 (70%) |
| - II | 171 (24%) |
| - III | 22 (3%) |
| - IV | 17 (3%) |
| Onset of infarction, N (%) | |
| - < 12 h | 317 (49%) |
| - > 12 h | 337(51%) |
| Door-to-needle time, (minute ) | 38 (10–333) |
| Door-to-balloon time, N (%) | |
| - < 90 min | 87 (44%) |
| - > 90 min | 107 (55%) |
| - Overall median (minute) | 95 |
Door-to-needle time was presented as median (minimal-maximal)
STEMI patients without reperfusion therapy
A subanalysis was performed in STEMI patients not receiving reperfusion therapy. The most common source of referral for these patients was inter-hospital referral (52%), and almost 80% of them reached our hospital with the onset of infarction already more than 12 h (Table 2).
Table 2.
Characteristics of STEMI patients without reperfusion therapy (N = 271)
| Variables | Description, N (%) |
|---|---|
| Source of referral | |
| - Walk in/ ambulance | 85 (31%) |
| - Primary physician | 11 (4%) |
| - Inter-hospital | 140 (52%) |
| - Intra-hospital | 35 (13%) |
| Onset of infarction | |
| - < 12 h | 57 (21%) |
| - >12 h | 211 (78%) |
| Location of infarction | |
| - Anterior | 179 (66%) |
| - Non-anterior | 92 (34%) |
In-hospital mortality was significantly higher among patients who did not receive reperfusion therapy compared with patients who received acute reperfusion therapy, either by PPCI or fibrinolytic therapy (13.3% vs 5.3% vs 6.2%; p < 0.001) (Fig. 2).
Fig. 2.
In-hospital mortality of STEMI patients
Changes in in-hospital mortality
In 2007, the ACS mortality was 6.6% and decreased to 4.1% in 2009, probably due to the more invasive approach in the moderate- to high-risk ACS patient. The Ministry of Health of Indonesia greatly contributes by making a PCI package free of charge for poor people, and this effort has increased the number of PCIs in the hospital (2005 elective PCIs and 276 primary PCIs) in the year of 2010.
Discussion
Improvement in the system of care of AMI is one of the major efforts to decrease the mortality among ACS patients. The JAC registry data showed that Jakarta should build its own AMI system of care, especially for STEMI patients. This is because most STEMI patients (59%) did not receive reperfusion therapy and almost 80% of the patients presented very late (>12 h). It was shown that the patients not receiving reperfusion therapy had an almost two and a half fold increase of in-hospital mortality compared with patients who did receive reperfusion therapy (Fig. 2).
How to build the AMI system of care in Jakarta?
The Joint statement of AHA STEMI/PCI focused update recommendation has recommended (Class I) that each community should develop an appropriate STEMI system of care [9], and the system of care of AMI is different between countries based on local health medical service availability. For example, models of STEMI systems of care include that in Vienna with its city-wide system of care [10], France with the famous SAMU-nationwide system [11], Minneapolis [12] and Mayo clinic [13] with their regional system of care. Although they have some differences in the protocol, all of the systems are using a pharmaco-invasive approach.
Before choosing which strategy could be used for the AMI system of care in Jakarta, it is important to know the problems in the real-world cardiovascular services in Jakarta, and we have observed some time delays and problems identified in daily practice, such as:
Patient delay, such as lack of awareness of cardiac symptoms, fear of hospitals and financial problems;
Delay in making an early diagnosis and treatment in primary hospital/clinic;
Transportation delay due to traffic congestion;
Lack of collaboration between hospitals and doctors;
Lack of ambulance organisation.
To improve the system of care, a multidisciplinary approach is needed to solve the problem, and for that reason, a seminar was held on 22 July 2010, attended by the Governor of Jakarta, General Secretary of the Ministry of Health of the Republic of Indonesia, all the stakeholders, and directors of all hospitals in Jakarta. The emergency team from National Cardiovascular Center Harapan Kita Hospital introduced the idea of building a Jakarta Cardiovascular Care Unit Network System. An agreement was made, and all bodies are highly motivated to build the AMI system of care based on the consideration that is described below.
Considerations for choice of reperfusion therapy
Randomised controlled trials (RCTs) have shown the superiority of PPCI over fibrinolysis treatment by reducing the incidence of major adverse cardiac events (MACE) (8% vs 14%). Overall, there is about a 40% reduction in ischaemic events with PPCI compared with lytic treatment [2], but real life may be different from RCTs, and old trials have compared PPCI with stand-alone fibrinolytic treatment. Although the benefit of PPCI was seen in transfer patients in the DANAMI study [14], there was an under-use of PCI in post-fibrinolytic patients, in which the number of rescue PCIs was only 1.9%.
The benefit of fibrinolytic treatment is highest if it is done early after an infarction, as shown by Boersma, by the golden hour of thrombolysis. Within the first three hours after an infarction many lives could be saved reaching 60 lives-saved per 1000 treated patients if the time delay of treatment is no more than one hour [15]. Furthermore, Juliard et al. have shown that the longer the door-to-thrombolysis time, the higher the mortality will be (6.7% vs 1.8%, p < 0.05) [16].
The importance of time delay is also apparent in PPCI [17, 18]. Nallamothu et al. showed that for every 10 min PCI-related time delay (defined as difference between door-to-balloon and door-to-needle time), there will be a 0.94% decrease in mortality benefit (p = 0.006), and there is no benefit if the delay is more than 62 min [19]. Furthermore, Pinto [20] and Betriu [21] showed that multivariate adjusted odds of death were the same for fibrinolytic therapy and PCI, when the PCI-related delay was 114 min (95% CI 96–132 min; p < 0.001). Time delay is very crucial and time to reperfusion is as important for PCI as it is for fibrinolysis.
In the real-world practice in Indonesia, it is difficult to do PPCI in all patients with a door-to-balloon (DTB) time less than 90 min. Data from the Dutch National Cardiovascular Data Registry (NCDR) registry showed that only 57.9% of patients achieve a DTB of <90 min [22], and data from the US National Registry of Myocardial Infarction (NRMI) ¾ analysis showed that only 4.2% patients had a DTB <90 min [23]. Data from the Global Registry of Acute Coronary Events (GRACE) registry showed the mean DTB time and pre-hospital delay were 75 and 120 min in the year 2000–2001, but in the recent years (2005–2006) it is longer (80 and 133 min) [24]. Recent data from the European registry showed that the first medical contact to balloon inflation time varied from 69 to 177 min [25]. All these real-world data show that it is difficult to achieve an appropriate DTB time as recommended by the ESC and AHA guidelines.
Gibson [26] showed the risk of early recurrent MI following thrombolysis was higher in the non-PCI group compared with the PCI group (4.5% vs 1.6%, p < 0.001). This analysis suggested that fibrinolysis should not be used as a stand-alone procedure, and it should be followed by routine angioplasty.
To determine how early an “early” angioplasty should be in post-fibrinolytic patients, the decision should be based on the result of the fibrinolytic treatment. In case of a failed fibrinolysis, immediate rescue PCI is the best option as shown in the REACT trial [27]. For a successful fibrinolysis, routine early invasive approach within 1.6 to 15.7 h after fibrinolytic treatment showed a significantly lower ischaemic event rate compared with a selective invasive approach, as shown by CAPITAL AMI, CARESS-AMI, TRANSFER-AMI, SIAM and GRACIA-1 trials [28]. Overall comparison of pharmaco-invasive strategies including both rescue PCI and routine PCI with stand-alone fibrinolysis showed a 50% reduction in the risk of combined cardiovascular ischaemic events. These data suggest that routine angioplasty should be done within the first 24 h after successful fibrinolytic treatment and immediately in failed fibrinolysis.
Reperfusion strategies for STEMI patients
The role of PCI in an early onset of infarction could be divided into primary PCI, pharmacological reperfusion in combination with PCI (pharmaco-invasive strategy) and rescue PCI after failed pharmacological reperfusion.
The pharmaco-invasive strategy is defined as giving pharmacological reperfusion (fibrinolytic agent) with an invasive strategy/PCI backup [29]. It means that all patients who receive fibrinolytic therapy should be referred to hospitals capable of performing PCI for either rescue PCI in case of failed fibrinolytic, or elective PCI within 3–24 h in successful fibrinolytic cases.
Primary PCI as recommended by guidelines can not be performed in all STEMI patients in Jakarta and neither can it work perfectly in a city with a well-organised cardiovascular emergency network system due to several limitations. Time delay is central for decision making in choosing reperfusion therapy, whether bringing the patient to the treatment (bringing the patient to PPCI) or bringing the treatment to the patient (giving an intravenous fibrinolytic agent in the pre-hospital setting) [3]. A wise approach, therefore, may be combining the two strategies, by giving fibrinolytic therapy as soon as possible in the pre-hospital setting and immediately referring the patient to a hospital capable of performing PCI for either immediate or elective coronary angiography within 3–24 h. Nowadays, the pharmaco-invasive strategy is widely adopted throughout the world. In Jakarta, the pharmaco-invasive strategy looks feasible and can be applied for an AMI system of care.
Therapeutic strategies for AMI in Jakarta
Some initiatives that should be undertaken are:
- Pre-hospital setting:
- Automated External Defibrillators (AED) and Basic Life Support (BLS) should be introduced in the community. This needs collaboration between the Indonesian Heart Association, the Indonesian Heart Foundation and the Government of Jakarta;
- Pre-hospital ECG activation is needed for an early accurate diagnosis;
- A patient transfer protocol and destination protocol should be designed.
In-hospital setting: the mission of the strategy is to reduce time delays for reperfusion therapy and increase the use of reperfusion therapy in STEMI patients.
Post-discharge state: a secondary prevention program is needed.
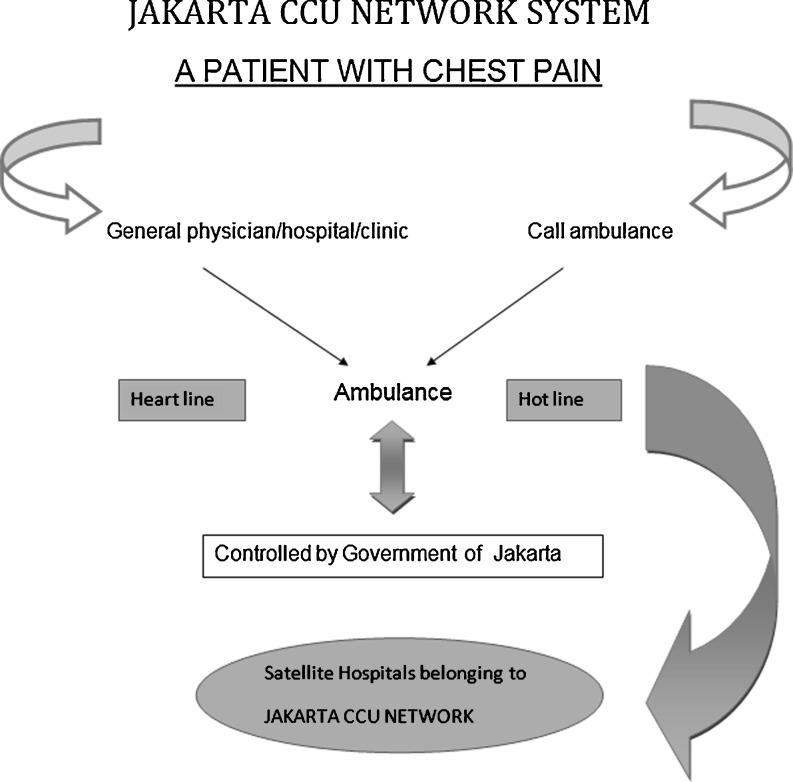
A suggested model for an AMI system of care in Jakarta is shown in Fig. 3. A patient with chest pain will either come to the primary hospital/primary physician, clinic and/or call an ambulance through the hotline. Twelve-lead ECG recording will be transmitted immediately to be evaluated by the cardiologist on duty (through the heart line) and the diagnosis is made followed by choice of reperfusion therapy. Primary PCI is preferred if:
Estimated door-to-balloon time is less than 90 min,
Fibrinolytic therapy is contraindicated.
Fig. 3.
Suggested model of AMI system of care in Jakarta (Jakarta Cardiovascular Care Unit Network System) CCU Cardiovascular Care Unit
If not, fibrinolytic therapy will be given (streptokinase 1.5 million unit or alteplase 100 mg, intravenously) in the ED/primary hospital or during transportation. The patient will be referred to the nearest PCI-capable hospital that belongs to the Jakarta CCU Network. An evaluation will be made in the receiving centre, including physical examination and 12-lead ECG. Rescue PCI will be done immediately in case of failed fibrinolytic and elective coronary angiography/PCI within 3–24 h for successful fibrinolytic treatment.
Of note:
The ambulance network is coordinated by the government of Jakarta
If possible, PPCI patients will be transferred directly to the cath-lab (bypassing the ED or PCI hospital);
The hotline number is the direct line ambulance telephone number (118), and there are 44 ambulance units spread out in Jakarta and organised centrally;
ECG transmission will be by internet service
The heart line is the receiving centre telephone number in the National Cardiovascular Center Harapan Kita Hospital and is manned 24 h a day.
Study limitation
The data were collected from a single-centre registry and the coverage of ACS patients for analysis was 62% from all ACS admissions. However, since our hospital is the only national cardiac referral hospital in Jakarta and daily experience matches the characteristics of STEMI patients as reported above, the reported data should be representative for all ACS patients admitted to the ED.
Conclusions
Analysis of the JAC registry showed a proportion of patients currently not receiving reperfusion therapy of 59% of all STEMI patients; the majority of them (52%) were from inter-hospital referrals. The time from onset of infarction to hospital admission was more than 12 h in almost 80% cases.
Network organisation is central to optimising patient care at the acute stage of an MI and there is a strong need to build a well-organised cardiovascular care unit network system in Jakarta. This involves a multidisciplinary approach that should give an appropriate diagnosis and initial treatment with rapid and safe transport to a PCI-capable hospital.
A pharmaco-invasive strategy looks feasible in which fibrinolytic therapy will be given in pre-hospital setting if the expected time to transfer for PCI is delayed, followed by coronary angiography/angioplasty.
A multidisciplinary team approach is the best way to design a network, harmonising the activities of all hospitals in Jakarta that will give the best cardiovascular services to the community by providing two reperfusion therapy options (PPCI or pharmaco-invasive strategy) depending on the time needed for the patient to reach the cath-lab. And last, but not least, the effectiveness of the system should be monitored by recording simple quality indicators in ongoing registries.
References
- 1.Dalby M, Bouzamondo A, Lechat P, et al. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation 2003;1809–14. [DOI] [PubMed]
- 2.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 3.Danchin N. System of care for ST-segment elevation myocardial infarction. Impact of different models on clinical outcomes. J Am Coll Cardiol Intv. 2009;2:901–8. doi: 10.1016/j.jcin.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 4.Kusmana D. Jakarta Cardiovascular Study: The city that promotes Indonesia Healthy Heart, Report I 2006.
- 5.National Health Survey 2006, Ministry of Health, Republic of Indonesia, 2006.
- 6.Kusmana D. The influence of smoking or stop smoking followed by regular exercise and/or effect of physical exertion on survival in Jakarta population: a 13 years cohort study. Dissertation of PhD thesis, Faculty of Medicine, University of Indonesia, 2002.
- 7.Jakarta Demographic Survey 2010, Government of Jakarta, Indonesia.
- 8.Galenta Y, Dharma S. ST-segment elevation myocardial infarction characteristic in National Cardiovascular Center Harapan Kita. Abstract session in the 19th Annual Scientific Meeting of Indonesian Heart Association, Jakarta, April 2010.
- 9.Kushner FG, Hand M, Smith SC, et al. 2009 Focused Updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 10.Kalla K, Christ G, Karnik R, et al. Implementation of guidelines improves the standard of care: the Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (Vienna STEMI registry) Circulation. 2006;113:2398–405. doi: 10.1161/CIRCULATIONAHA.105.586198. [DOI] [PubMed] [Google Scholar]
- 11.Danchin N, Coste P, Ferrieres J, et al. Comparison of thrombolysis followed by broad use of percutaneous coronary intervention with primary percutaneous coronary intervention for ST-segment elevation acute myocardial infarction: data from the French registry on acute ST-elevation myocardial infarction (FAST-MI) Circulation. 2008;118:268–76. doi: 10.1161/CIRCULATIONAHA.107.762765. [DOI] [PubMed] [Google Scholar]
- 12.Henry TD, Scott WS, Burke MN, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 13.Ting HH, Rihal CS, Gersh BJ, et al. Regional system of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the MAYO Clinic STEMI protocol. Circulation. 2007;116:729–36. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 14.Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733–42. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]
- 15.Boersma E, Maas AC, Deckers JW, et al. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–5. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 16.Juliard JM, Feldman LJ, Golmard JL, et al. Relation of mortality of primary angioplasty during acute myocardial infarction to door-to-Thrombolysis in Myocardial Infarction (TIMI) time. Am J Cardiol. 2003;91:1401–1405. doi: 10.1016/S0002-9149(03)00388-6. [DOI] [PubMed] [Google Scholar]
- 17.Cannon CP, Gibson M, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–7. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 18.Luca G, Suryapranata H, Ottervanger JP, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction. Circulation. 2004;109:1223–5. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 19.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol. 2003;92:824–6. doi: 10.1016/S0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 20.Pinto DS, Kirtane AJ, Nallamothu BK, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: Implications when selecting a reperfusion strategy. Circulation. 2006;114:2019–25. doi: 10.1161/CIRCULATIONAHA.106.638353. [DOI] [PubMed] [Google Scholar]
- 21.Betriu A, Masotti M. Comparison of mortality rates in acute myocardial infarction treated by percutaneous coronary intervention versus fibrinolysis. Am J Cardiol. 2005;95:100–1. doi: 10.1016/j.amjcard.2004.08.069. [DOI] [PubMed] [Google Scholar]
- 22.Rathore SS, Curtis JP, Chen J, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:1807–13. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nallamothu BK, Bates ER, Herrin J, et al. NRMI Investigators. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)- 3/4 analysis. Circulation. 2005;111:761–7. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 24.Eagle KA, Nallamothu BK, Mehta RH, et al. for the Global Registry of Acute Coronary Events (GRACE) Investigators. Trends in acute reperfusion therapy for ST-segment elevation myocardial infarction from 1999 to 2006: we are getting better but we have got a long way to go. Eur Heart J. 2008;29:609–17. doi: 10.1093/eurheartj/ehn069. [DOI] [PubMed] [Google Scholar]
- 25.Widimsky P, Wijns W, Fajadet J, et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J. 2010;31:943–57. doi: 10.1093/eurheartj/ehp492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gibson CM, Karha J, Murphy SA, et al. Early and long-term clinical outcomes associated with reinfarction following fibrinolytic administration in the thrombolysis in myocardial infarction trials. J Am Coll Cardiol. 2003;42:7–16. doi: 10.1016/S0735-1097(03)00506-0. [DOI] [PubMed] [Google Scholar]
- 27.Gershlick AH, Stephens-Lloyd A, Hughes S, et al. for the REACT Trial Investigators. Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction. N Engl J Med. 2005;353:2758–68. doi: 10.1056/NEJMoa050849. [DOI] [PubMed] [Google Scholar]
- 28.Verheugt FWA. Routine angioplasty after fibrinolysis—How early should “early” be? N Engl J Med. 2009;360:2779–81. doi: 10.1056/NEJMe0902460. [DOI] [PubMed] [Google Scholar]
- 29.Werf F. Pharmaco-invasive vs. Facilitated percutaneous coronary intervention strategies for ST-segment elevation acute myocardial infarction patients in the new ESC Guidelines. Eur Heart J. 2009;30:2817. doi: 10.1093/eurheartj/ehp409. [DOI] [PubMed] [Google Scholar]