Introduction
Cardiac catheterisation and percutaneous coronary interventions (PCI) are increasingly performed via the radial artery. Compared with the femoral approach there are several advantages. For example, patients can be mobilised more rapidly [1, 2]. Also complications such as access site bleeding occur less frequently and are often less severe compared with the femoral approach. However, although rare, vascular complications can occur when cardiac catheterisation is performed using the radial approach. The literature concerning this subject is scarce. Cardiologists should be aware of the possible complications when using the radial artery as the access site.
We describe a patient in which a rare complication occurred. Also its subsequent diagnosis and management are described.
Case report
In a 79-year-old-woman a cardiac catheterisation was performed. She was evaluated because of exercise-related dyspnoea. Her medical history revealed a pneumectomy on the left side because of tuberculosis 58 years earlier and paroxysmal atrial fibrillation.
After local anaesthesia the right radial artery was punctured. A 5F sheath was introduced. A guidewire was advanced (0.035 inch with a soft curled end) through the radial, brachial, axillary and subclavian artery. Despite several attempts the ascending aorta could not be reached, the guidewire repeatedly entered the descending aorta.
Suddenly, while attempting to access the ascending aorta with the guidewire, the patient complained of severe pain in the right axillary region, the neck and in the region of the right ear. The pain subsided after removal of the guidewire from the arterial system. Patient remained haemodynamically stable, there were no signs of neurological deficits. The pulsations at the right radial artery and the right carotid artery were normal. There were no signs of limb ischaemia.
The procedure was continued via the femoral artery. No signs of obstructive coronary artery disease were found during coronary angiography.
After cardiac catheterisation a chest X-ray was performed (Fig. 1a). Compared with a preprocedural chest X-ray (Fig. 1b) slight consolidation of the medial, upper mediastinal region on the right side was seen. A CT angiogram indicated extravasation of contrast medium from the right subclavian artery, located between the origin of the right carotid artery and the origin of right vertebral artery, and a large haematoma (Fig. 2a). Subsequently a coated stent was placed at the site of leakage (Fig. 2b) via the femoral artery. The patient’s recovery was uneventful and she could be discharged from the hospital the following day.
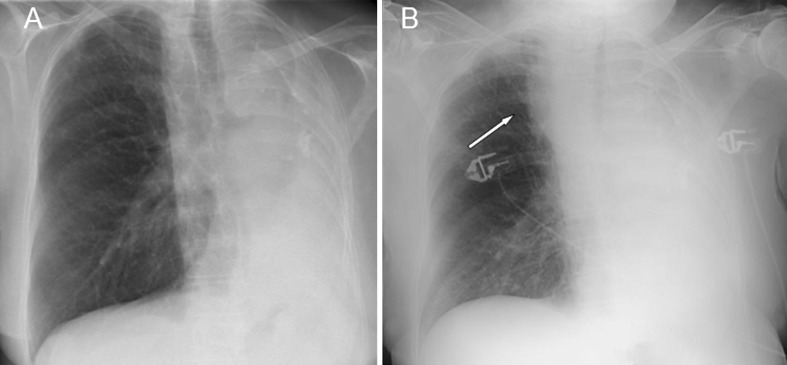
Fig. 1.
a Preprocedural chest X-ray, showing consolidation of the left hemithorax, after pneumectomy 58 years earlier. b Chest X-ray performed after cardiac catheterisation. Compared with a preprocedural chest X-ray (Fig. 1b) slight consolidation of the medial, upper region of the right lung was seen (arrow)
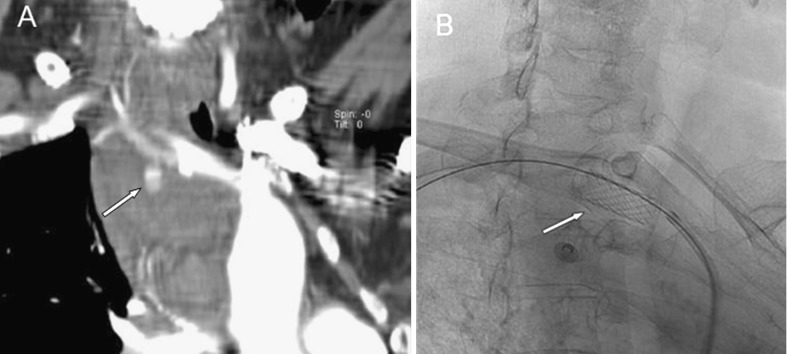
Fig. 2.
a CT angiogram indicating extravasation of contrast from the right subclavian artery (arrow). b Angiogram after placement of covered stent in subclavian artery
Discussion
The radial approach is becoming increasingly popular as vascular access site for cardiac catheterisation [1, 2]. Compared with the femoral approach patients can be mobilised more rapidly and haemostasis is obtained more easily [1, 2]. Although complications seem to be less prevalent, extensive reports are lacking in the literature.
Mediastinal haematomas have been reported in four cases after cardiac catheterisation, via either the transradial or transbrachial approach. The exact site of bleeding was not found in three of those cases. In one case report the site of bleeding was found to be the thymic branch of the right innominate artery. A mediastinal haematoma after cardiac catheterisation may occur from injury of the small vessels near the aortic arch, specially when the transradial approach is used [3–5]. Sanmartin et al. report on their experience in 3369 cardiac catheterisations via the radial approach performed between 2001 and 2003 [6]. In 21 (0.06%) cases vascular complications occurred. Local, mild to moderate, haematomas at the puncture sites were excluded from analysis. In 13 patients a serious haematoma (>6 cm) occurred, five patients presented with perforation of an artery (radial artery in four patients and brachial artery in one patient).
Perforation of the radial and brachial artery could be explained by advancement of the guidewire through an area of tortuosity and/or arterial spasm. All cases were managed conservatively with a local compression bandage for at least 4 h. Other complications were a pseudoaneurysm of the radial artery and arteriovenous fistulas.
Kelly et al. describe the case of a 78-year-old man in whom perforation of the brachial artery occurred during cardiac catheterisation via the radial artery [7]. Probably related to extensive antithrombotic treatment, conservative management failed and a covered stent had to be placed via the femoral artery.
We are the first to describe a perforation of the subclavian artery during cardiac catheterisation via the radial approach and its successful management. Conservative management of a perforation of the subclavian artery is hampered by the fact that application of local pressure is inefficient. Because of multiple side branches (right carotid artery, right vertebral artery and the right internal mammary artery) arising from or in the neighbourhood of the subclavian artery, placing covered stents is challenging. However, surgery is rather invasive and whenever possible placing a covered stent by an experienced interventional radiologist is preferred.
With the advance of the radial approach for cardiac catheterisations, cardiologists should be increasingly aware of the rare complications that can occur during this procedure and its subsequent management.
References
- 1.Agostoni P, Biondi-Zoccai GGL, Benedictis L, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures. Systemic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004;44:349–56. doi: 10.1016/j.jacc.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 2.Eichhöfer J, Horlick E, Ivanov J, et al. Decreased complication rates using the transradial compared to the transfemoral approach in percutaneous coronary intervention in the era of routine stenting and glycoprotein platelet IIb/IIIa inhibitor use: a large single-center experience. Am Heart J. 2008;156:864–70. doi: 10.1016/j.ahj.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 3.Jao YT, Chen Y, Fang CC, et al. Mediastinal and neck hematoma after cardiac catheterization. Catheter Cardiovasc Interv. 2003;58(4):467–72. doi: 10.1002/ccd.10476. [DOI] [PubMed] [Google Scholar]
- 4.Park KW, Chung JW, Chang SA, et al. Two cases of mediastinal hematoma after cardiac catheterization: A rare but real complication of the transradial approach. Int J Cardiol. 2008;130:e89–e92. doi: 10.1016/j.ijcard.2007.05.093. [DOI] [PubMed] [Google Scholar]
- 5.Fransson SG, Nylander E, et al. Vascular injury following cardiac catheterization, coronary angiography, and coronary angioplasty. Eur Heart J. 1994;15:232–5. doi: 10.1093/oxfordjournals.eurheartj.a060481. [DOI] [PubMed] [Google Scholar]
- 6.Sanmartin M, Cuevas D, Goicolea J, et al. Vascular complications associated with radial artery access for cardiac catheterization. Rev Esp Cardiol. 2004;57(6):581–4. doi: 10.1157/13062925. [DOI] [PubMed] [Google Scholar]
- 7.Kelly D, Levy T, Talwar S. Brachial artery perforation repaired with percutaneous transfemoral covered stent deployment in a patient on Abciximab. J Invasive Cardiol. 2008;20(3):e82–3. [PubMed] [Google Scholar]