Abstract
The widely‐used Kessler K6 non‐specific distress scale screens for severe mental illness defined as a K6 score ≥ 13, estimated to afflict about 6% of US adults. The K6, as currently used, fails to capture individuals struggling with more moderate mental distress that nonetheless warrants mental health intervention. The current study determined a cutoff criterion on the K6 scale indicative of moderate mental distress based on mental health treatment need and assessed the validity of this criterion by comparing participants with identified moderate and severe mental distress on relevant clinical, impairment, and risk behavior measures. Data were analyzed from 50,880 adult participants in the 2007 California Health Interview Survey. Receiver operating characteristic curve analysis identified K6 ≥ 5 as the optimal lower threshold cut‐point indicative of moderate mental distress. Based on the K6, 8.6% of California adults had serious mental distress and another 27.9% had moderate mental distress. Correlates of moderate and serious mental distress were similar. Respondents with moderate mental distress had rates of mental health care utilization, impairment, substance use and other risks lower than respondents with serious mental distress and greater than respondents with none/low mental distress. The findings support expanded use and analysis of the K6 scale in quantifying and examining correlates of mental distress at a moderate, yet still clinically relevant, level. Copyright © 2012 John Wiley & Sons, Ltd.
Keywords: mental distress, mental health, psychiatric scale, Kessler
Introduction
Mental illness, as well as stress and distress more broadly, place a significant burden on health and productivity (USDHHS, 1999). In economically developed nations like the United States, mental illness accounts for over 15% of the burden of disease, exceeding the disease burden of all cancers, and is the leading cause of disability for ages 15 to 44 (Murray and Lopez, 1996; World Health Organization, 2004). Annually, mental illness costs the United States nearly $200 billion in lost earnings (Kessler et al., 2008). Mental illness also is associated with additional health risks including tobacco use, binge drinking, sedentary behavior, and obesity, increasing the associated health care costs and disease burden (Lasser et al., 2000; Miles et al., 2003; Sanchez‐Villegas et al., 2008). Identification of individuals or population groups with significant mental distress is important for informing clinical interventions and health policy.
Epidemiological studies of the prevalence and correlates of mental illness and distress require brief, validated measures. Standardized clinical diagnostic tests based on the American Psychiatric Association's (1994) Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM‐IV) are time intensive to administer and identify only those individuals meeting criteria for specific disorders.
A measure increasingly used in epidemiological studies is the K6 non‐specific distress scale, a six‐item, psychological screening instrument, developed by Kessler et al. (2002), which takes < 2 minutes to complete and screens at the population level for individuals with possible severe mental illness. Developed for use in the annual US National Health Interview Survey and National Household Survey on Drug Abuse, the K6 has yielded national‐ and state‐level estimates of serious mental illness and informed the funding of block grants for community mental health services (Centers for Disease Control, 2010; Grant et al., 2010; Kessler et al., 2002; Kessler et al., 2003).
The K6 items assess the frequency of non‐specific psychological distress within a particular reference period. The responses range from “none of the time” coded zero to “all of the time” coded four. The six items are summed to yield a number between zero and 24. The scale has demonstrated excellent internal consistency and reliability (Cronbach's alpha = 0.89) (Kessler et al., 2002). Clinical validation studies of the K6 against structured diagnostic interviews have demonstrated the test to have a sensitivity of 0.36, specificity of 0.96, and total classification accuracy of 0.92 at a cut‐point ≥ 13 (Kessler et al., 2003). Its brevity, accuracy, and ability to discriminate DSM‐IV cases from non‐cases make the K6 scale an ideal screening instrument for serious mental illness in population‐based health surveys (Furukawa et al., 2003; Kessler et al., 2003; Veldhuizen et al., 2007).
The K6 cut‐point of 13 was developed to operationalize the definition of serious mental illness, defined as meeting diagnostic criteria for a DSM‐IV disorder in the past 12‐months and experiencing significant impairment, estimated to afflict about 6% of US adults (Kessler et al., 1996). Many more people experiencing significant mental distress possibly will not be detected using this definition. Mental distress that does not meet DSM‐IV diagnostic criteria (i.e. mental distress at a sub‐diagnostic level) can have serious health and economic impacts, particularly at a population‐level (Indig et al., 2007; Katon et al., 2003; Vedsted et al., 2004). Further, the low sensitivity of the K6 scale at the recommended cut‐point of 13 means that some respondents experiencing significant mental distress may go undetected. While the K6 has demonstrated little bias with regard to sex and education (Baillie, 2005), mental illness can manifest in different symptoms in different cultural groups, and some ethnic groups may be less forthcoming in reporting psychological symptoms.
Based on the accepted cut‐point of K6 ≥ 13 for serious mental illness, this concurrent criterion validity study sought to identify a lower threshold score that characterized moderate levels of mental distress defined as necessitating mental health treatment and causing impairments in functioning. Specifically, the aims of the current study were to: (1) determine a sub‐threshold cutoff criterion score on the widely‐used K6 scale indicative of moderate mental distress; (2) examine invariance of the sub‐threshold cutoff score by four major ethnic/racial groups (i.e. Caucasian, Hispanic, African American, and Asian American); and (3) assess the validity of this criterion by comparing participants meeting the sub‐threshold cutoff to those at the traditional K6 cutoff on mental health care utilization, mental health impairment, substance use (binge drinking and smoking), and other risk factors (sedentary behavior and obesity). For aim three, we hypothesized that respondents with moderate mental health distress would have rates of mental health care utilization, impairment, substance use and other risks that are less than those of respondents with serious mental distress and greater than those of respondents with none or low mental distress.
Methods
Data source
The current study analyzed data from the 2007 California Health Interview Survey (CHIS), a telephone survey of California's non‐institutionalized population. Conducted biennially since 2001, CHIS is the largest state‐level health survey and one of the largest health surveys in the United States (Brown et al., 2005). CHIS uses a multistage stratified random‐digit‐dial sampling design that oversamples racial and ethnic minority groups. Within each sampled household, one adult was randomly selected for an extended interview following the method developed by Rizzo et al. (2004). Briefly, for sampled land‐ and cellular‐lines, if there was only one adult in the household, then that adult was selected. If there were multiple adults in the household, then the computer‐assisted telephone interviewing (CATI) system chose an adult based on a pre‐generated uniform random number and the next birthday method (CHIS, 2009a). Among households screened and determined eligible, the adult sample survey response rate was 52.8% with higher participation among women, older adults, households without children, and households with only one adult (CHIS, 2009b). The telephone interviews were monitored for quality assurance. Proxy interviews were allowed for frail and ill persons over the age of 65. For the current study, we used data from the 2007 CHIS Adult File after excluding proxy interviews (N = 168). The final sample contained 50,880 adults.
Measures
Demographics
Demographic variables included age, gender, race/ethnicity, education level, poverty level, employment status, and marital status.
Kessler K6
The K6 asked respondents to consider the one month in the past 12 months when they were at their worst emotionally and to self report how frequently they experienced the following six symptoms: felt nervous, hopeless, restless or fidgety, worthless, depressed, and felt that everything was an effort (Kessler et al., 2002). For each question, a value of zero, one, two, three, or four was assigned to the answer: “none of the time”, “a little of the time”, “some of the time”, “most of the time”, or “all of the time”, respectively. Responses to the six items were summed to yield a K6 score between zero and 24, with higher scores indicating a greater tendency towards mental illness.
Mental health treatment need items
We used four items in the CHIS that assessed the need for mental health treatment and were asked of all respondents to identify the sub‐threshold moderate mental distress cut‐point for the K6. The four items assessed whether respondents, due to emotional or personal problems in the past 12‐months: (a) took any prescription medications, such as an antidepressant or sedative, almost daily for two weeks or more; (b) saw a primary care physician or general practitioner; (c) saw any other professional, such as a counselor, psychiatrist or social worker; or (d) felt the need to see a professional. Respondents endorsing any one of these four mental health treatment need items received a score of one; respondents who said no to all received a score of zero.
Mental health care utilization items
We used two items in the CHIS that assessed mental health care utilization to check the validity of the identified sub‐threshold moderate mental distress cut‐point by comparing differences in mental health care utilization among three groups – those with serious, moderate, and no or low mental distress (defined later). The first item assessed the number of visits respondents had in the past 12 months to a professional for problems with mental or emotional health or use of alcohol or drugs. The item excluded overnight hospital stays. The second item asked if at the respondents’ last routine medical visit, a doctor provided or arranged treatment for their emotions or moods, such as medications, counseling, or other treatment. Due to a pre‐determined skip pattern on the CHIS, respondents scoring K6 ≤ 5 were not asked this item unless they reported a need to see a professional in the last 12 months for emotional problems. Consequently, we examined differences in provider attention to mental health issues only for the serious and moderate mental distress groups.
Mental health impairment items
We also examined five mental health impairment items and a composite index to check the validity of the identified sub‐threshold moderate mental distress cut‐point. Four items had respondents refer to the month in the past 12 months when they were at their worst emotionally and report how often emotions interfered with their work performance (asked only of employed respondents aged 18 to 70 years), household chores, social life, and family/friend relations. Responses were coded as follows: not at all (zero), some (one), and a lot (two). A composite index averaging the codes of these four items was created. A fifth mental health impairment item assessed the number of days out of the past 365 days that respondents were unable to work or carry out normal activities because they felt nervous, depressed, or emotionally stressed. Due to the pre‐determined skip pattern on the CHIS, all the above impairment items were not asked of respondents scoring K6 ≤ 5, so we examined differences in mental health impairment only for the serious and moderate mental distress groups.
Substance use and other risk factors
The CHIS assessed binge drinking status defined as those who drank ≥ 5 alcoholic drinks for men or ≥ 4 alcoholic drinks for women in a single episode in the past year. Smoking status was classified as never, current, or former smoker based on having smoked at least 100 cigarettes in one's lifetime and now smoking daily (daily smokers) or some days (non‐daily smokers). Additional risk factors were sedentary behavior defined as no engagement in physical activity or exercise during the past seven days and obesity status defined by body mass index (BMI) ≥ 30 kg/m2.
Statistical analyses
We used receiver operating characteristic (ROC) curve analysis to identify the optimal sub‐threshold K6 cut‐point indicative of moderate mental distress by maximizing the sum of sensitivity and specificity. For our criterion measure, we categorized respondents as needing mental health treatment if they reported either use of prescription medications or seeing a physician or other professional for mental health problems or feeling the need for help with emotional or mental health problems in the past 12‐months. ROC curve analysis is a plot of the true positives (sensitivity) versus the false positives (1 – specificity) for a binary clinical outcome classifier system as its screening test discrimination threshold is varied. We calculated the area under each ROC curve (AUC), which ranges from 0.5 to one with one indicating perfect discrimination. This area can be interpreted as the probability that randomly chosen respondents with or without the clinical outcome of interest would be correctly distinguished based on their screening test scores (Hanley and McNeil, 1982). The clinical outcome in this study was whether or not the respondent reported either use of prescription medications or seeing a physician or other professional for mental health problems or feeling the need for help with emotional or mental health problems in the past 12‐months; the screening test was the K6 scale. We ran ROC curve analysis for the full sample and by race/ethnicity.
Based on the results of the ROC curve analysis, we determined the sub‐threshold K6 cutoff point for distinguishing moderate distress from none or low mental distress. Based on both this cut‐point and the conventional cut‐point of K6 ≥ 13, we classified respondents into three mental distress groups: (1) none or low mental distress, (2) moderate mental distress, and (3) serious mental distress. We ran cross‐tabulations to calculate the prevalence of moderate and serious mental distress by the demographic, substance use, and additional risk factor variables. Next, for validity tests, we examined the associations between the mental distress groups and reports of mental health care utilization and mental health impairment. Lastly, we compared the prevalence of current smoking, binge drinking, sedentary status, and obesity status for the three mental distress groups.
For all multivariate regression analyses, we included all demographic, substance use (binge drinking and smoking status), and additional risk factor variables (sedentary behavior and obesity status) as other covariates. All analyses were performed with SAS software Version 9.2 (SAS Institute Inc., 2009) to derive unbiased estimates and accurate standard errors for the California population, using the Proc Surveyfreq, Surveymeans, Proc Surveylogistic, and Surveyreg procedures, which take into consideration the design effects of complex sample surveys by using the jackknife replication sample weights provided in the CHIS data (CHIS, 2009c). We considered estimates to be statistically significant if the p value from a two‐tailed test was < 0.05.
Results
ROC curve analysis
Of the full sample, 10% reported prescription medication use, 7% contact with a physician, 9% contact with another professional, and 17% feeling the need for help concerning emotional or mental health problems in the past 12‐months. At least one of these four mental health treatment need items was endorsed by 22% of respondents. Individuals reporting one or more mental health treatment need item had significantly (p < 0.0001) greater K6 scores, mean (M) = 9.3, standard error (SE) = 0.10, compared to those who endorsed none of the items, M = 3.2, SE = 0.03.
Using the four items as an indicator of mental health treatment need items as the clinical outcome in ROC curve analysis, we identified the optimal K6 cut‐point for classification of moderate mental distress using ROC curve analysis. The ROC curves for the full sample and four racial/ethnic groups were largely overlapping, indicating little variance (Figure 1). For the full sample and three of the four ethnic groups, the K6 cut‐point that maximized the sum of sensitivity and specificity values (i.e. the optimum threshold) was K6 ≥ 5. For Hispanics, the optimal cut‐point was K6 ≥ 6, though the difference in the sum of sensitivity and specificity values for the cut‐points of five and six was very small (0.012). Based on the consistency in the optimal cut‐point findings for the full sample and different racial/ethnic groups, moderate mental distress was defined as 5 ≤ K6 < 13. Table 1 summarizes the sensitivity, specificity, total classification rate, and AUC values based on the cut‐point of K6 ≥ 5. The AUC values were at least 0.8 for all groups, indicating a high level of accuracy.
Figure 1.
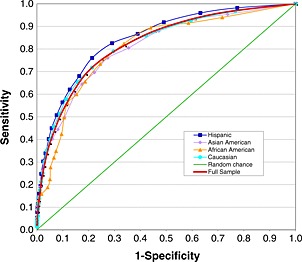
Receive operator characteristic (ROC) curves for all the K6 thresholds predicting moderate mental distress, for the full sample and by four major ethnicity/race groups: Hispanic, Asian American, African American, Caucasian.
Table 1.
Receiver operator characteristic (ROC) curve analysis statistics for the full sample and by race/ethnicity at a cut‐point of K6 ≤ 5
| Full sample | Caucasian | Hispanic | Asian American | African American | |
|---|---|---|---|---|---|
| N | 50,880 | 33,193 | 9,067 | 4,332 | 2,391 |
| Sensitivity | 0.76 | 0.72 | 0.83 | 0.76 | 0.73 |
| Specificity | 0.75 | 0.79 | 0.71 | 0.73 | 0.76 |
| Total classification accuracy | 0.74 | 0.72 | 0.75 | 0.77 | 0.73 |
| Area under the curve (AUC) | 0.82 | 0.82 | 0.84 | 0.81 | 0.80 |
Prevalence of moderate and serious mental distress
In 2007, 8.6% of California adults met criteria for serious mental distress and another 27.9% met criteria for moderate mental distress based on the cut‐points of K6 ≥ 13, and 5 ≤ K6 < 13, respectively. Table 2 shows the prevalence of moderate (5 ≤ K6 < 13) and serious (K6 ≥ 13) mental distress by demographic characteristics and risk behaviors. Controlling for other covariates, moderate mental distress was significantly more likely among adults aged 18–34; women; those who identified their race/ethnicity as other; the less educated; those below the federal poverty level; those who were unemployed, looking for work; those who were not married; binge drinkers; current and former smokers; those who were not regularly physically active; and those who were obese. The prevalence of serious mental distress varied similarly by demographic and risk behavior groups.
Table 2.
Prevalencea of moderate (5 ≤ K6 < 13) and serious mental distress (K6 ≥ 13)
| Characteristics | Prevalence of mental distress | Multinomial logistic model AOR (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| N | Moderate | Serious | Moderate | Serious | |||
| Full sample | 50,880 | 27.9 | 8.5 | ||||
| Age in years | |||||||
| 18–25 (reference) | 3181 | 35.9 | 13.6 | ||||
| 26–34 | 4632 | 33.4 | 9.7 | 0.9 (0.8, 1.0) | 0.8 (0.6, 0.9) | * | |
| 35–49 | 12,801 | 28.0 | 8.4 | 0.7 (0.6, 0.9) | * | 0.7 (0.5, 0.9) | * |
| 50+ | 30,266 | 22.0 | 6.0 | 0.5 (0.4, 0.6) | * | 0.3 (0.3, 0.4) | * |
| Gender | |||||||
| Men (reference) | 20,410 | 25.8 | 6.6 | ||||
| Women | 30,470 | 29.9 | 10.4 | 1.4 (1.3, 1.6) | * | 2.0 (1.8, 2.4) | * |
| Race/ethnicity | |||||||
| Caucasian (reference) | 33,193 | 26.3 | 8.2 | ||||
| Hispanic | 9067 | 30.2 | 9.3 | 0.9 (0.8, 1.0) | 0.8 (0.7, 0.9) | * | |
| Asian American | 4332 | 27.6 | 6.0 | 0.9 (0.8, 1.1) | 0.7 (0.5, 0.9) | * | |
| African American | 2391 | 25.2 | 10.3 | 0.7 (0.6, 0.9) | * | 0.7 (0.5, 0.9) | * |
| Other | 1897 | 34.5 | 13.8 | 1.4 (1.2, 1.7) | * | 1.5 (1.2, 2.0) | * |
| Education status | |||||||
| < High school degree (reference) | 4924 | 31.0 | 11.1 | ||||
| High school graduate | 11,333 | 28.6 | 9.5 | 0.8 (0.7, 0.9) | * | 0.8 (0.6, 1.0) | |
| Some college | 14,415 | 28.1 | 10.1 | 0.9 (0.8, 1.0) | 0.9 (0.7, 1.2) | ||
| College or more | 20,208 | 25.5 | 5.3 | 0.9 (0.8, 1.0) | 0.8 (0.6, 0.9) | * | |
| Poverty level | |||||||
| < 100% FPL (reference) | 7094 | 33.6 | 13.7 | ||||
| 100 − 199% FPL | 8307 | 31.1 | 10.4 | 0.9 (0.8, 1.0) | 0.8 (0.7, 0.9) | * | |
| 200 − 399% FPL | 12,640 | 27.6 | 8.7 | 0.8 (0.7, 0.9) | * | 0.7 (0.6, 0.9) | * |
| ≥ 400% FPL | 22,839 | 24.3 | 5.5 | 0.7 (0.6, 0.8) | * | 0.5 (0.4, 0.7) | * |
| Employment level | |||||||
| Full‐time (reference) | 25,446 | 27.6 | 7.0 | ||||
| Part‐time | 3950 | 29.9 | 8.9 | 1.0 (0.9, 1.2) | 1.1 (0.9, 1.4) | ||
| Employed but not working | 169 | 30.2 | 15.7 | 1.2 (0.7, 2.2) | 2.3 (0.7, 7.9) | ||
| Unemployed, looking for work | 1232 | 38.9 | 17.3 | 1.6 (1.3, 2.0) | * | 2.4 (1.7, 3.2) | * |
| Unemployed, not looking for work | 20,083 | 26.3 | 10.4 | 1.1 (0.9, 1.2) | 1.7 (1.4, 2.0) | * | |
| Marital status | |||||||
| Married (reference) | 26,088 | 24.3 | 5.5 | ||||
| Not married | 24,792 | 32.2 | 12.2 | 1.3 (1.2, 1.4) | * | 1.8 (1.6, 2.1) | * |
| Binge drinking status | |||||||
| No (reference) | 39,010 | 26.3 | 7.8 | ||||
| Yes | 11,870 | 31.5 | 10.2 | 1.2 (1.1, 1.3) | * | 1.3 (1.1, 1.6) | * |
| Smoking status | |||||||
| Never smoker (reference) | 28,835 | 26.9 | 7.1 | ||||
| Former smoker | 15,434 | 26.2 | 7.3 | 1.2 (1.1, 1.3) | * | 1.4 (1.2, 1.7) | * |
| Current (daily smoker) | 4756 | 33.6 | 18.1 | 1.7 (1.5, 2.0) | * | 3.3 (2.7, 4.0) | * |
| Current (non‐daily smoker) | 1855 | 37.2 | 14.4 | 1.8 (1.5, 2.2) | * | 2.7 (2.0, 3.6) | * |
| Sedentary behavior | |||||||
| No physical activity | 7301 | 30.6 | 11.7 | 1.4 (1.2, 1.5) | * | 1.7 (1.5, 2.1) | * |
| Some physical activity | 24,625 | 28.3 | 8.5 | 1.2 (1.1, 1.3) | * | 1.3 (1.1, 1.4) | * |
| Regular physical activity (reference) | 18,954 | 26.2 | 7.4 | ||||
| Body weight status (BMI, in kg/m2) | |||||||
| Underweight (BMI < 18.5) | 1229 | 33.5 | 9.9 | 1.1 (0.9, 1.5) | 1.0 (0.7, 1.5) | ||
| Normal (18.5 ≤ BMI < 25) (reference) | 20,331 | 28.3 | 7.9 | ||||
| Overweight (25 ≤ BMI < 30) | 18,040 | 25.8 | 7.7 | 0.9 (0.9, 1.1) | 1.1 (0.9, 1.3) | ||
| Obese (BMI ≥ 30) | 11,280 | 29.7 | 10.8 | 1.2 (1.1, 1.4) | * | 1.6 (1.4, 1.8) | * |
Note: AOR, adjusted odds ratio, controlling for all other variables in the table; CI, confidence interval; FPL, federal poverty level based on household composition and self‐reported household annual income; BMI, body mass index.
Estimation was based on weighted analyses accounting for complex survey design.
Statistically significant at p < 0.05, two‐tailed test.
Mental health care utilization by mental distress group
The three mental distress groups differed significantly on the number of visits to a professional in the past 12 months for problems with mental or emotional health or use of alcohol or drugs: serious mental distress [M = 6.9, 95% confidence interval (CI) = 5.5–8.3]; moderate mental distress (M = 1.8, 95% CI = 1.6–2.0); and none or low mental distress (M = 0.4, 95% CI = 0.3–0.5). In multivariate linear regression analyses controlling for other covariates, the serious mental distress group had 6.1 additional visits (p < 0.0001) than the none or low mental distress group, and 4.9 additional visits (p < 0.0001) than the moderate mental distress group, while the moderate mental distress group had 1.3 additional visits (p < 0.0001) than the none or low mental distress group.
The likelihood that a doctor provided or arranged treatment for one's emotions or moods, such as medications, counseling, or other treatment was 30.2% (95% CI = 28.0–32.5) among participants identified with serious mental distress versus 11.6% (95% CI = 10.7–12.5) among those with moderate mental distress. Of note, less than one in three adults with serious mental distress received treatment or a referral from a doctor for their emotions or moods.
Mental health impairment by mental distress group
The moderate and serious mental distress groups differed significantly on each of the four impairment items assessing work performance, household chores, social life, and family/friend relations (see Figure 2). Respondents with moderate mental distress had a greater proportion reporting some impairment, while those with serious mental distress had a greater proportion reporting a lot of impairment. The mean values on the impairment index were 0.79 (95% CI = 0.78–0.81) for moderate and 1.37 (95% CI = 1.34–1.40) for serious mental distress. In a multivariate linear regression controlling for other covariates, the serious mental distress group had a significantly greater impairment index value than the moderate group by 0.56 (p < 0.0001). The moderate and serious mental distress groups also differed significantly on the item assessing the number of impairment days. On average, adults with serious mental distress reported 66 days (95% CI = 59.5–72.7; SE = 3.3) of impairment compared to 12 days (95% CI = 10.8–13.1; SE = 0.6) reported by adults with moderate mental distress. In a multivariate linear regression controlling for other covariates, the serious mental distress group had significantly more number of impairment days than the moderate group by 48.2 days (p < 0.0001).
Figure 2.
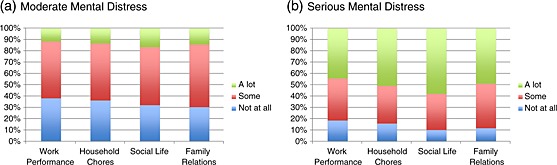
Reported impairment in the worst month emotionally in the past 12‐months for participants meeting criteria for (a) moderate mental distress versus (b) serious mental distress.
Substance use and additional risk factors by mental distress group
Table 3 shows that prevalence of substance use and other risk factors significantly differed by mental distress group. The prevalence of current daily and non‐daily smoking, sedentary behavior, and obesity all were greatest among adults with serious mental distress, followed by adults with moderate mental distress, and lowest among adults with no mental distress. Adults with serious and moderate mental distress did not differ from each other in prevalence of binge drinking, while both groups had binge drinking prevalence that was significantly greater than adults without mental illness.
Table 3.
Prevalence of substance use and additional risk factors by mental distress group
| Risk behavior | None or low mental distress | Moderate mental distress | Serious mental distress | ||
|---|---|---|---|---|---|
| Current daily smoking (%) | 11.7 | 20.5 | |||
| AOR (95% CI) | 7.4 | 1.7 (1.5, 1.9) | A | 3.3 (2.8, 4.0) | BC |
| Current non‐daily smoking (%) | 6.4 | 8.0 | |||
| AOR (95% CI) | 3.6 | 1.8 (1.5, 2.2) | A | 2.7 (2.0, 3.5) | BC |
| Binge drinking (%) | 33.6 | 35.7 | |||
| AOR (95% CI) | 27.3 | 1.2 (1.1, 1.3) | A | 1.3 (1.1, 1.5) | B |
| Sedentary behavior (%) | 15.9 | 19.1 | |||
| AOR (95% CI) | 12.6 | 1.2 (1.1, 1.4) | A | 1.5 (1.3, 1.8) | BC |
| Obesity (%) | 24.0 | 28.5 | |||
| AOR (95% CI) | 21.1 | 1.2 (1.1, 1.4) | A | 1.5 (1.3, 1.8) | BC |
Note: AOR, adjusted odds ratio, controlling for age, gender, race/ethnicity, education, poverty level, employment status, marital status, as well as all other substance use and risk factors; CI, confidence interval; subscripts indicate significant group differences at p < 0.05 between (A) none or low and moderate mental distress groups, (B) none or low and serious mental distress groups, and (C) moderate and serious mental distress groups.
Discussion
The K6 was developed with the goal of being sensitive to the upper 90th to 99th percentile range of the population distribution of mental distress (Kessler et al., 2002). It is estimated that about 6% of the US population meets criteria for serious mental illness, defined as meeting DSM‐IV diagnostic criteria for at least one psychiatric disorder in the past 12 months, that has resulted in serious impairment, not counting a substance use disorder (Kessler et al., 1996). In this California sample, the prevalence of serious mental illness as detected with a K6 scale score ≥ 13 was 8.5%.
The current study examined the utility of the K6 scale for identifying mental distress at a moderate level that nevertheless impacts functioning and necessitates treatment. ROC curve analysis identified a K6 scale score ≥ 5 as optimal in identifying respondents with mental health treatment needs. The cut‐point provided a balance between sensitivity (0.76) and specificity (0.75) with an overall classification accuracy of 0.74 and little variance by ethnic/racial group. Further, the AUC value of 0.82 was comparable to that reported for the K6 cut‐point of ≥ 13 when predicting serious mental illness (AUC = 0.865) (Kessler et al., 2003).
Using the identified cut‐point of 5 ≤ K6 < 13, an additional 27.9% of respondents identified themselves as experiencing mental distress at a moderate level that impacted functioning across a number of impairment domains (work, household, social, family/friends, disability) and was associated with increased utilization of mental health treatment. Correlates of mental distress were similar at both serious and moderate levels with a greater likelihood among younger adults, women, those below the poverty level, and those who identified their race/ethnicity as other. These ethnic, gender, and socio‐economic patterns with mental distress parallel those reported nationally in the 1993–2001 Behavioral Risk Factor Surveillance System Surveys (Zahran et al., 2004). The current study also found that mental distress was more prevalent among the less educated, those who were unemployed and looking for work, those who were not married, binge drinkers, current and former smokers, those who were not regularly physically active, and those who were obese.
Prior research has demonstrated that individuals with mental illness are at greater risk for engagement in multiple risk behaviors such as smoking, alcohol misuse, sedentary behavior, and obesity (Lasser et al., 2000; Miles et al., 2003; Sanchez‐Villegas et al., 2008). In the current study, adults with moderate mental distress had profiles comparable to adults with serious mental distress in increased risk for substance use and additional risk behaviors. For current tobacco use, sedentary behavior, and obesity, a linear relationship was demonstrated with adults with serious mental distress being at the highest risk and adults with no or low mental distress being at the lowest risk.
The K6 scale has demonstrated utility for providing aggregate estimates of serious mental illness prevalence and correlates (Kessler et al., 2010). To date, it has largely been used by the nation and states to identify the most at‐risk individuals to demonstrate the need for community intervention. The K6 also has been suggested as a useful screening scale in health risk appraisal surveys and primary care screening batteries (Kessler et al., 2002). The findings from the current study demonstrate the utility of examining a fuller range of K6 scale scores to identify populations experiencing mental distress at a moderate or sub‐threshold level that still may warrant clinical attention and health policy interventions.
Strengths of the current study include analysis of data from a large, population‐based survey and examination of the sub‐threshold cut‐point across major ethnic/racial groups. Consistent with prior investigations demonstrating little bias in the K6 scale with regard to gender and education (Baillie, 2005), the current study found high consistency by race/ethnicity in selection of the optimal cut‐point on the K6 for moderate mental illness. The study data were limited to the state of California, and it is unknown how findings may generalize. A limitation of the data collection was that several mental health utilization and impairment items were not asked of respondents scoring K6 ≤ 5. The decision rule was intended to capture 15% to 20% of the California adult population with the highest level of mental health symptoms based on examination of past‐30‐day K6 data from the 2005 CHIS. The current findings suggest that future CHIS surveys should assess mental health impairments and treatment utilization with individuals who score as low as five on the K6 scale.
This study concurrently determined a sub‐threshold cutoff criteria on the K6 scale indicative of moderate mental distress and assessed the validity of this criterion by comparing participants meeting the sub‐threshold cutoff to serious mental distress participants meeting the traditional K6 cutoff on mental health care utilization, mental health impairment, substance use as well as additional risk behaviors. The choice of criterion for establishment of the sub‐threshold cut‐point was based on the inference that individuals in treatment or perceiving the need for treatment are experiencing clinically relevant mental health symptoms. Future studies should examine the new cut‐point in relation to other established mental health symptomatology or diagnostic measures.
The current findings, including the consistency in the optimal cut‐point results from the ROC curve analysis across diverse ethnic/racial groups, support expanded use and analysis of the K6 scale in quantifying and examining correlates of mental distress at a moderate, yet still clinically relevant, level. Further, the elevated risks for tobacco and heavy alcohol use, sedentary behavior, and obesity among respondents with identified serious and moderate mental distress underscore the need for comprehensive interventions that address the multiple risks with which these groups present.
Declaration of interest statement
The authors have no competing interests.
Acknowledgments
This study was supported by funding from the Tobacco‐related Disease Research Program of the University of California (#18XT‐0092 and #13KT‐0152), the National Institute on Drug Abuse (#K23 DA018691 and #P50 DA09253), and the National Institute of Mental Health (#P30 MH082760).
References
- American Psychiatric Association . (1994) Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition, Washington, DC, American Psychiatric Association. [Google Scholar]
- Baillie A.J. (2005) Predictive gender and education bias in Kessler's psychological distress scale (K10). Social Psychiatry and Psychiatric Epidemiology, 40, 743–748, DOI: 10.1007/s00127-005-0935-9 [DOI] [PubMed] [Google Scholar]
- Brown E.R., Holtby S., Zahnd E., Abbott G.B. (2005) Community‐based participatory research in the California Health Interview Survey. Preventing Chronic Disease, 2(4), A03. [PMC free article] [PubMed] [Google Scholar]
- California Health Interview Survey . (2009a) CHIS 2007 Methodology Series: Report 1 – Sample Design, pp. 4‐1–4‐2, Los Angeles, CA, UCLA Center for Health Policy Research. http://www.chis.ucla.edu/pdf/CHIS2007_method1.pdf [2 April 2011].
- California Health Interview Survey . (2009b) CHIS 2007 Methodology Series: Report 4 – Response Rates, Los Angeles, CA, UCLA Center for Health Policy Research. http://www.chis.ucla.edu/pdf/CHIS2007_method4.pdf [2 April 2011]
- California Health Interview Survey . (2009c) CHIS 2007 Methodology Series: Report 5 – Weighting and Variance Estimation, Los Angeles, CA, UCLA Center for Health Policy Research. http://www.chis.ucla.edu/pdf/CHIS2007_method5.pdf [2 April 2011]
- Centers for Disease Control . (2010) QuickStats: percentage of adults aged ≥ 18 years who experienced serious psychological distress during the preceding 30 days,* by sex and age group – National Health Interview Survey, 2009. Morbidity and Mortality Weekly Report, 59(49), 1621. [Google Scholar]
- Furukawa T.A., Kessler R.C., Slade T., Andrews G. (2003) The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well‐Being. Psychological Medicine, 33(2), 357–362. [DOI] [PubMed] [Google Scholar]
- Grant D.R., Kravitz‐Wirtz N., Aguilar‐Gaxiola S., Sribney W.M., Aydin M., Brown E.R. (2010) Mental Health Status and Use of Mental Health Services by California Adults, Los Angeles, CA, UCLA Center for Health Policy Research. [PubMed] [Google Scholar]
- Hanley J.A., McNeil B.J. (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology, 143(1), 29–36. [DOI] [PubMed] [Google Scholar]
- Indig D., Eyeson‐Annan M., Copeland J., Conigrave K.M. (2007) The effects of alcohol consumption, psychological distress and smoking status on emergency department presentations in New South Wales, Australia. BMC Public Health, 7, 46, DOI: 10.1186/1471-2458-7-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W.J., Lin E., Russo J., Unutzer J. (2003) Increased medical costs of a population‐based sample of depressed elderly patients. Archives of General Psychiatry, 60(9), 897–903. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., Walters E.E., Zaslavsky A.M. (2002) Short screening scales to monitor population prevalences and trends in non‐specific psychological distress. Psychological Medicine, 32, 959–976, DOI: 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.L., Manderscheid R.W., Walters E.E., Zaslavsky A.M. (2003) Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P.A., Zhao S., Leaf P.J., Kouzis A.C., Bruce M.L., Friedman R.M., Grossier R.C., Kennedy C., Narrow W.E., Kuehnel T.G., Laska E.M., Manderscheid R.W., Rosenheck R.A., Santoni T.W., Schneier M. (1996) The 12‐month prevalence and correlates of serious mental illness In Mental Health, United States, 1996, Manderscheid R.W., Sonnenschein M.A. (eds) pp. 59–70, Washington, DC, US Government Printing Office. [Google Scholar]
- Kessler R.C., Green J.G., Gruber M.J., Sampson N.A., Bromet E., Cuitan M., Furukawa T.A., Gureje O., Hinkov H., Hu C.Y., Lara C., Lee S., Mneimneh Z., Myer L., Oakley‐Browne M., Posada‐Villa J., Sagar R., Viana M.C., Zaslavsky A.M. (2010) Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19(Suppl 1), 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Heeringa S., Lakoma M.D., Petukhova M., Rupp A.E., Schoenbaum M., Wang P.S., Zaslavsky A.M. (2008) Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. The American Journal of Psychiatry, 165, 703–711, DOI: 10.1176/appi.ajp.2008.08010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasser K., Boyd J.W., Woolhandler S., Himmelstein D.U., McCormick D., Bor D.H. (2000) Smoking and mental illness: a population‐based prevalence study. Journal of the American Medical Association, 284, 2606–2610, DOI: 10.1001/jama.284.20.2606 [DOI] [PubMed] [Google Scholar]
- Miles H., Johnson S., Amponsah‐Afuwape S., Finch E., Leese M., Thornicroft G. (2003) Characteristics of subgroups of individuals with psychotic illness and a comorbid substance use disorder. Psychiatric Services, 54(4), 554–561. [DOI] [PubMed] [Google Scholar]
- Murray C.J.L, Lopez A.D. (1996) The Global Burden of Disease, Geneva, World Health Organization, Harvard School of Public Health, World Bank. [Google Scholar]
- Rizzo L., Brick J.M., Park I. (2004) A minimally intrusive method for sampling persons in Random Digit Dialing Surveys. Public Opinion Quarterly, 68, 267–274, DOI: 10.1093/poq/nfh014 [DOI] [Google Scholar]
- Sanchez‐Villegas A., Ara I., Guillen‐Grima F, Bes‐Rastrollo M., Varo‐Cenarruzabeitia J.J., Martínez‐González M.A. (2008) Physical activity, sedentary index, and mental disorders in the SUN cohort study. Medicine & Science in Sports & Exercise, 40, 827–834, DOI: 10.1249/MSS.0b013e31816348b9 [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc . (2009) SAS/STAT ® 9.2 User's Guide, second edition, Cary, NC, SAS Institute Inc. [Google Scholar]
- USDHHS . (1999) Mental Health: A Report of the Surgeon General, Washington, DC, Department of Health and Human Services. [Google Scholar]
- Vedsted P., Fink P., Sorensen H.T., Olesen F. (2004) Physical, mental and social factors associated with frequent attendance in Danish general practice. A population‐based cross‐sectional study. Social Science & Medicine, 59, 813–823, DOI: 10.1016/j.socscimed.2003.11.027 [DOI] [PubMed] [Google Scholar]
- Veldhuizen S., Cairney J., Kurdyak P., Streiner D.L. (2007) The sensitivity of the K6 as a screen for any disorder in community mental health surveys: a cautionary note. Canadian Journal of Psychiatry, 52(4), 256–259. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2004) The World Health Report 2004: Changing History, Annex Table 3: Burden of Disease in DALYs by Cause, Sex, and Mortality Stratum in WHO Regions, Estimates for 2002, Geneva, World Health Organization. [Google Scholar]
- Zahran H.S., Kobau R., Moriarty D.G., Zack M.M., Giles W.H. (2004). Self‐reported frequent mental distress among adults – United States, 1993–2001. Morbidity and Mortality Weekly Report, 53(41), 963–966. [PubMed] [Google Scholar]


