Abstract
OBJECTIVE:
The purpose of this study was to evaluate the following: 1) the effects of continuous exercise training and interval exercise training on the end-tidal carbon dioxide pressure (PETCO2) response during a graded exercise test in patients with coronary artery disease; and 2) the effects of exercise training modalities on the association between PETCO2 at the ventilatory anaerobic threshold (VAT) and indicators of ventilatory efficiency and cardiorespiratory fitness in patients with coronary artery disease.
METHODS:
Thirty-seven patients (59.7±1.7 years) with coronary artery disease were randomly divided into two groups: continuous exercise training (n = 20) and interval exercise training (n = 17). All patients performed a graded exercise test with respiratory gas analysis before and after three months of the exercise training program to determine the VAT, respiratory compensation point (RCP) and peak oxygen consumption.
RESULTS:
After the interventions, both groups exhibited increased cardiorespiratory fitness. Indeed, the continuous exercise and interval exercise training groups demonstrated increases in both ventilatory efficiency and PETCO2 values at VAT, RCP, and peak of exercise. Significant associations were observed in both groups: 1) continuous exercise training (PETCO2VAT and cardiorespiratory fitness r = 0.49; PETCO2VAT and ventilatory efficiency r = -0.80) and 2) interval exercise training (PETCO2VAT and cardiorespiratory fitness r = 0.39; PETCO2VAT and ventilatory efficiency r = -0.45).
CONCLUSIONS:
Both exercise training modalities showed similar increases in PETCO2 levels during a graded exercise test in patients with coronary artery disease, which may be associated with an improvement in ventilatory efficiency and cardiorespiratory fitness.
Keywords: Coronary Artery Disease, Exercise, Cardiorespiratory Fitness, Ventilatory Efficiency
INTRODUCTION
End-tidal carbon dioxide pressure (PETCO2) is a noninvasive index that is considered to be a good indicator for evaluating the ventilation/perfusion relationship in patients over a wide range of conditions (1,2). Variations in PETCO2 have been shown to reflect changes in both cardiac output and pulmonary blood flow in animals and humans under constant ventilation (3). For example, previous studies (4,5,6) have demonstrated alterations in the distribution of ventilation and perfusion in the lungs (ventilation-perfusion mismatch) of cardiac patients. This observation has led to an increased ratio of physiologic dead space to tidal volume. In this regard, patients with cardiac disease have been shown to have an abnormally low PETCO2 during exercise, especially those with an impaired response of cardiac output during exercise (5). Moreover, recent investigations have shown that reduced PETCO2 is considered to be a strong predictor of adverse events in cardiac disease (7,8).
Aerobic exercise training has been recommended as a non-pharmacological treatment for patients with coronary artery disease (CAD) (9,10). In this context, continuous exercise training (CET) promotes beneficial cardiorespiratory adaptations in CAD patients (11). Interestingly, previous investigations (12) have also demonstrated the effectiveness of interval exercise training (IET) for improving cardiorespiratory fitness in CAD patients. IET involves alternating brief (2–5 min) higher-intensity (≥75% VO2peak) and moderate-intensity workloads throughout an exercise session. However, little is known regarding the impact of the exercise training modality on the PETCO2 response during a graded exercise test in CAD patients. Thus, the purpose of this study was to evaluate the following: 1) the effects of continuous exercise training and interval exercise training on the PETCO2 response during a graded exercise test in CAD patients; and 2) the effects of exercise modalities on the association between PETCO2 at the ventilatory anaerobic threshold (VAT) and indicators of ventilatory efficiency and cardiorespiratory fitness in CAD patients.
MATERIALS AND METHODS
Population
The patients were admitted to the coronary care unit from the TotalCor Hospital for the diagnosis of coronary artery disease. Forty-five CAD patients (60.0±1.7) were initially enrolled into this study. The inclusion criterion was stable coronary artery disease diagnosed by coronary angiography. The exclusion criteria were unstable angina pectoris, complex ventricular arrhythmias, pulmonary congestion, and orthopedic or neurological limitations to exercise. Thirty-seven patients meeting the inclusion/exclusion criteria were considered for this study. The CAD patients were randomly divided into two groups: CET (n = 20) and IET (n = 17). The patients remained on their standard medication throughout the study, and no changes were reported. The study participants read a detailed description of the protocol and completed a written informed consent (Table 1).
Table 1.
Patient characteristics.
| All patients | CET | IET | |
| N | 37 | 20 | 17 |
| Age (years) | 59.7±1.7 | 62.5±2.0 | 56.5±3.0 |
| Weight (kg) | 79.8±2.3 | 78.2±3.1 | 81.6±3.7 |
| BMI (kg/m2) | 28.3±0.6 | 28.1±1.0 | 28.5±0.9 |
| Men/women | 28/9 | 15/5 | 14/3 |
| Hypertension | 35 (84%) | 19 (54%) | 16 (46%) |
| Diabetes | 11 (30%) | 4 (36%) | 7 (64%) |
| Myocardial infarction | 17 (46%) | 11 (65%) | 6 (35%) |
| Drugs | |||
| Beta-blockers | 27 (72%) | 16 (59%) | 11 (41%) |
| ACE inhibitors | 24 (65%) | 10 (42%) | 14 (58%) |
Values are means±SE. CET = continuous exercise training; IET = interval exercise training; BMI = body mass index. p>0.01 for all variables between groups.
Graded Exercise Test
A maximal graded exercise test was performed on a programmable treadmill (DigiStress model pulsar, Governador Valadares, MG, Brazil). The gas exchange and ventilatory variables were measured continuously during the gas exchange tests, breath by breath, using an open-circuit spirometry procedure based on an exercise system (SensorMedics - model Vmax 229 Pulmonary Function/Cardiopulmonary Exercise Testing Instrument, Yorba Linda, CA, USA). The following variables were obtained breath by breath and were expressed as 30-s averages: pulmonary oxygen uptake (VO2 ml·kg-1·min-1 STPD), respiratory exchange ratio (RER), pulmonary ventilation (VE l·min-1 BTPS), functional estimate of dead space (VD/VT), ventilatory equivalents for oxygen and carbon dioxide (VE/VO2 and VE/VCO2) and end-tidal pressures for oxygen and carbon dioxide (PETO2 and PETCO2 mmHg). Before each test, the gas analyzers were calibrated using gases of known concentrations of carbon dioxide and oxygen balanced with nitrogen, and the flow meter was calibrated using a 3-L syringe. The heart rate was continuously recorded at rest, during the graded exercise testing and during the recovery period using a 12-lead ECG (HW Systems- HeartWare Ltd.). All tests in this study were performed in the same laboratory at the same room temperature (20-23°C).
The subjects performed a ramp-like progressive exercise test until they were exhausted on the treadmill. The exercise workload (speed and/or slope) was increased every 1 minute; the incremental part of the exercise test was completed between approximately 8 and 12 minutes.
Ventilatory Anaerobic Threshold
The ventilatory anaerobic threshold (VAT) was determined to occur at the break point between the increase in the carbon dioxide output and VO2 (V-Slope) or the point at which the VE/VO2 reached the minimum value and began to rise without a concomitant rise in VE/VCO2 (13).
Respiratory Compensation Point
The respiratory compensation point (RCP) was determined to be the point at which the VE/VCO2 reached its minimum value and began to rise and the highest value of PETCO2 before its progressive fall (14).
Peak Oxygen Consumption
The peak oxygen consumption (VO2peak) was defined as the maximum attained VO2 at the end of the exercise period, when the subject is exhausted (analog scale of the perceived exertion to the Borg scale).
Exercise Training Program
A supervised exercise training program was conducted at the cardiorespiratory rehabilitation center of the TotalCor Hospital. The exercise training program consisted of three 60-minute exercise sessions per week over a 3-month period. Each exercise session consisted of a 5 minute warm-up, 50 minutes of aerobic exercise and 5 minutes of cool-down exercises. The CET was performed on a treadmill with a 50-minute duration and intensity at VAT. The IET consisted of seven sets of 3 minutes at RCP and seven sets of 3 minutes of exercise at moderate intensity corresponding to the VAT totaling 42 minutes. Heart rate was monitored throughout the session to ensure that all patients exercised within the limits of intensity.
Statistical Analysis
The statistical procedures were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL). The normality of the distribution was checked for all variables using the Kolmogorov-Smirnov test. A two-way analysis of variance (ANOVA) with repeated measures was performed to evaluate possible within-group and between-group differences for physical characteristics, cardiorespiratory fitness, ventilatory efficiency and PETCO2 response during GET in the CAD patients subjected to CET and IET. When significance was identified, a Tukey's post hoc comparison was performed.
For both groups, the relative difference (Δ%) was calculated for PETCO2 in the intervals from rest to VAT, rest to RCP, and rest to peak of exercise.
The Pearson-product moment correlation was performed to examine the association between PETCO2 at VAT and the cardiorespiratory fitness and ventilatory efficiency after the interventions. The data are presented as means±SE. A p-value of <0.05 was considered statistically significant.
RESULTS
Effects of interventions
Baseline measurements
Before the interventions, no differences in the physical characteristics between the groups studied were noted (Table 2). In addition, both groups exhibited similar levels of cardiorespiratory fitness and ventilatory efficiency (Table 2).
Table 2.
Physical and cardiorespiratory measurements in the CAD patients subjected to continuous exercise training and interval exercise training.
| CET | IET | |||
| Pre | Post | Pre | Post | |
| Physical measurements | ||||
| Age (years) | 62.5±2.1 | 62.6±2.1 | 56.5±2.7 | 56.8±2.6 |
| Weight (kg) | 78.2±3.3 | 78.1±3.3 | 81.6±3.3 | 81.9±3.0 |
| BMI (kg/m2) | 28.1±1.0 | 28.1±1.0 | 28.5±0.7 | 28.5±0.7 |
| Cardiorespiratory measurements | ||||
| VO2peak mL/kg/min | 18.0±1.2 | 22.2±1.3* | 17.9±1.0 | 22.3±1.1* |
| VO2 (VAT) mL/kg/min | 12.5±0.7 | 15.0±0.7* | 12.3±0.6 | 14.0±0.7* |
| VEVCO2 (VAT) | 33.0±0.8 | 29.7±0.6* | 31.8±0.4 | 29.1±0.6* |
| VD/VT (VAT) | 0.20±0.0 | 0.16±0.0*† | 0.20±0.0 | 0.18±0.0* |
| PETCO2 (VAT) mmHg | 37.5±0.6 | 41.0±0.4*† | 38.0±0.6 | 40.2±0.3* |
Values are means+SE. Pre, pre-intervention; Post, post-intervention; CET, continuous exercise training; IET, interval exercise training; BMI, body mass index; VAT, ventilatory anaerobic threshold. *p<0.05 vs. pre-intervention; †p<0.01 vs. pre-intervention.
Physical characteristics
After the interventions, neither the CET nor IET showed a significant reduction in body weight (Table 2).
Cardiorespiratory response
After the interventions, both the CET and IET showed an increase in the VO2peak. A comparison between the groups revealed a similar increase in the cardiorespiratory fitness (Table 2).
The ventilatory efficiency was analyzed at the VAT. After the exercise training program, the CAD patients subjected to either CET or IET showed significantly lower values for VEVCO2 and VD/VT. In addition, both exercise training modalities demonstrated an increase in the PETCO2 at VAT (Table 2). A comparison between the groups revealed a similar increase in the ventilatory efficiency (Table 2).
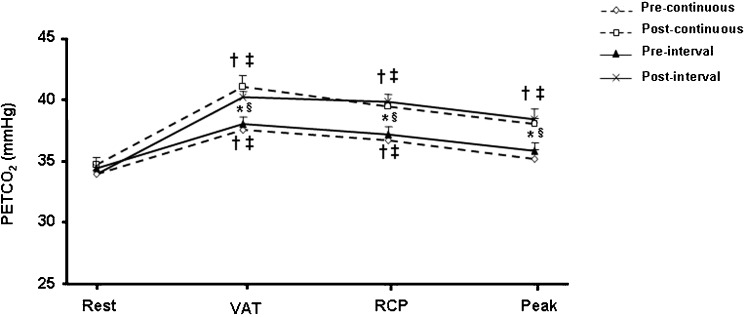
After the interventions, both the CET and IET showed values significantly greater for the PETCO2 during the GET (Figure 1).
Figure 1.
PETCO2 response during a graded exercise test in patients with coronary artery disease subjected to either continuous exercise training or interval exercise training. VAT = ventilatory anaerobic threshold; RCP = respiratory compensation point. † p<0.05 vs. rest (pre- and post-continuous); ‡ p<0.05 vs. rest (pre- and post-interval); * p<0.05 vs. post-continuous; § p<0.05 vs. post-interval.
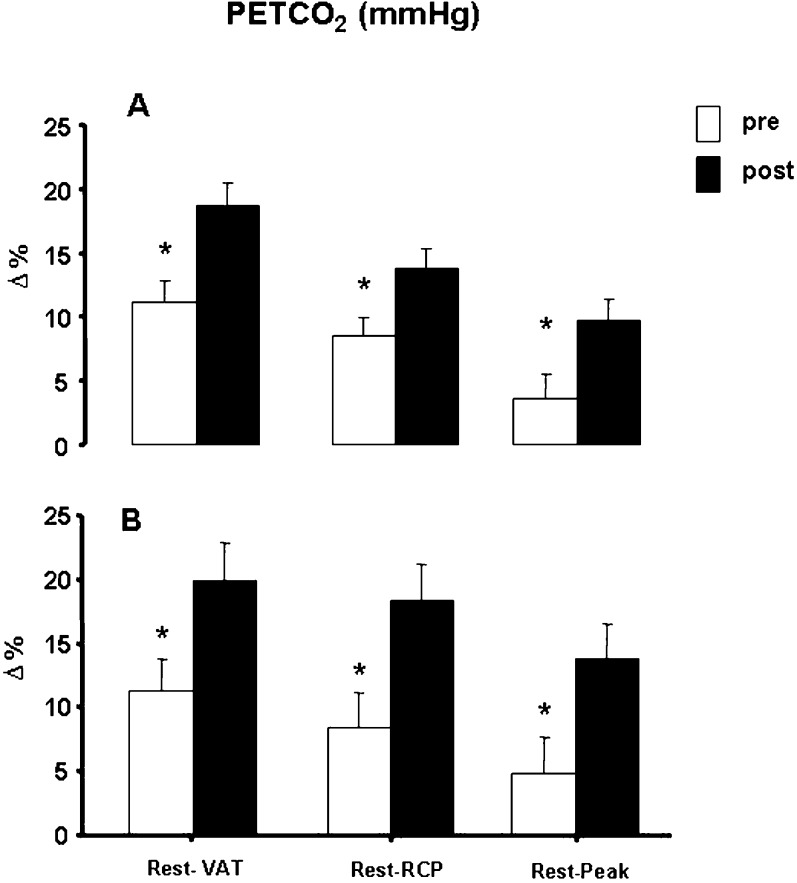
The changes in the PETCO2 response from rest to VAT, rest to RCP, and rest to peak of exercise are shown in Figure 2. The statistical analysis determined that the relative difference of the PETCO2 in all intervals analyzed were significantly higher after the interventions.
Figure 2.
Percentage difference from rest to ventilatory anaerobic threshold (rest/VAT), rest to respiratory compensation point (rest/RCP) and rest to peak of exercise (rest/Peak) in patients with coronary artery disease subjected to continuous exercise training (panel A) and interval exercise training (panel B). VAT = ventilatory anaerobic threshold; RCP = respiratory compensation point. * p<0.05 vs. post-intervention.
The results of the correlation analysis between PETCO2 at VAT and the cardiorespiratory parameters after either CET or IET are shown in Table 3.
Table 3.
Correlations between PETCO2 at ventilatory anaerobic threshold and the cardiorespiratory measurements in CAD patients after continuous exercise training and interval exercise training.
| CET | IET | |||
| r | p-value | r | p-value | |
| VO2peak mL/kg/min | 0.49 | 0.01 | 0.39 | 0.01 |
| VO2 (VAT) mL/kg/min | 0.49 | 0.01 | 0.33 | 0.05 |
| VEVCO2 (VAT) | -0.80 | 0.01 | -0.45 | 0.01 |
| VD/VT (VAT) | -0.57 | 0.01 | -0.42 | 0.01 |
CET, continuous exercise training; IET, interval exercise training. r = Pearson's product moment correlation coefficient.
Positive associations were observed in both groups for cardiorespiratory fitness: 1) CET (PetCO2VAT and VO2peak r = 0.49; PetCO2VAT and VO2VAT r = 0.49; p<0.05) and 2) IET (PetCO2VAT and VO2peak r = 0.39; PetCO2VAT and VO2VAT r = 0.33; p<0.05). However, negative associations were observed in both groups for ventilatory efficiency: 1) CET (PetCO2VAT and VEVCO2VAT r = -0.80; PetCO2VAT and VD/VT VAT r = -0.57; p<0.05) and 2) IET (PetCO2VAT and VEVCO2VAT r = -0.45; PetCO2VAT and VD/VT VAT r = -0.42; p<0.05).
DISCUSSION
The main findings of this investigation were the following: 1) continuous exercise training and interval exercise training improved the PETCO2 response during a graded exercise test in CAD patients; 2) both exercise modalities resulted in similar increases in the values of PETCO2; and 3) after exercise training, the improvements in ventilatory efficiency and cardiorespiratory fitness in patients with CAD were associated with increased values of PETCO2.
The elucidation of the mechanisms involved in the improvement observed in the PETCO2 response after exercise training in the CAD patients are beyond the scope of this study. However, we suggest that factors related to the improvement of the ventilation-perfusion (V/Q) mismatch may be responsible for the increase in the PETCO2 during a graded exercise test (11).
In this regard, previous investigations have shown that the failure of pulmonary blood flow (cardiac output) to increase appropriately during exercise and increased physiological dead space are the main factors leading to a decrease in PETCO2 in cardiac patients (1,15). For example, Matsumoto et al. (5) reported a positive association between cardiac output and PETCO2 during a graded exercise test in cardiac patients. In addition, ETO et al. (11) observed a close relationship between increased PETCO2 and cardiac output after aerobic exercise training in cardiac patients. In contrast, previous studies (1,5,15) reported an association between low levels of PETCO2 during exercise with ventilatory inefficiency. Accordingly, our findings suggest that factors related to the increase in both ventilatory efficiency and cardiorespiratory fitness were mainly responsible for the increase in PETCO2 during the graded exercise test. In fact, after 12 weeks of either CET or interval exercise training, the CAD patients had lower values for VEVCO2 and VD/VT at VAT. Moreover, the CAD patients subjected to both exercise training modalities demonstrated increases in VO2peak. After the interventions, we observed a positive association between PETCO2 at VAT and VO2peak and a negative association between PETCO2 at VAT and VEVCO2 at VAT. These findings suggest that the improvement in the V/Q mismatch after exercise training may be associated with an increase in the PETCO2 at VAT. Another possible explanation for the increased PETCO2 after exercise training would be raising the set point of PaCO2 modulation by peripheral chemoreceptors and/or hypoventilation (11,16).
With regard to cardiorespiratory fitness, the CAD patients subjected to either CET or IET exhibited similar increases in VO2peak. In this context, our findings are in agreement with previous studies that demonstrated the same effectiveness of both exercise training modalities to increase the cardiorespiratory fitness in CAD patients (12,17. However, other investigations 18,19,20) observed greater responsiveness to interval exercise training compared with continuous exercise training.
For example, Rogmo et al. (18) observed a superior increase in VO2peak in CAD patients subjected to IET, in which 4 minutes at a higher intensity (80-90% VO2peak) and 3 minutes at a moderate intensity (50-60% VO2peak) were alternated throughout the exercise session. In the same study (18), the CAD patients subjected to CET performed 41 minutes at a moderate intensity (50-60% VO2peak) over 10 weeks. In the same context, Ciolac et al. (20) observed that interval exercise training (80% of reserve heart rate) in hypertensive patients increased cardiorespiratory fitness to a higher degree than continuous exercise training (60% of reserve heart rate).
In this investigation, the CAD patients subjected to IET performed 3 minutes at RCP (80-90% VO2peak) and 3 minutes at moderate intensity corresponding to the VAT. In contrast, the patients subjected to CET performed 50 minutes at VAT (70-80% VO2peak) over 12 weeks.
These results conflict with previous studies (18,20) and may be associated with a greater relative intensity and higher training volume in the CET group of our study.
In fact, evidence has suggested that stroke volume is the main factor that limits cardiorespiratory fitness (20). Moreover, higher intensities of aerobic exercise promote an increase in central O2 delivery (cardiac output), thereby contributing to the training-induced improvements in VO2peak (20).
These findings demonstrate the need for a greater number of randomized trials to investigate the mode of aerobic exercise training that is more responsive in terms of increased cardiorespiratory fitness for patients with coronary artery disease.
Interestingly, after an exercise training program, the CAD patients did not display any reduction in body weight. Recent studies (21,22) have indicated that exercise-related caloric expenditure for patients enrolled in cardiac rehabilitation programs was only modest.
In both exercise training modalities, we observed energy expenditures of approximately 230 kcal/session. For example, Savage et al. (2000) reported that a caloric expenditure of 270 kcal/session during three months of a cardiac rehabilitation program had little impact on measures of obesity.
This study has limitations, such as the lack of evaluations of cardiac output and arterial blood gases during the graded exercise test.
In summary, these findings suggest that both continuous exercise training and interval exercise training promote an improved PETCO2 response during a graded exercise test in patients with coronary artery disease. Taken together, these results demonstrate that the application of different modalities of aerobic exercise training may be important in improving cardiorespiratory efficiency in patients with coronary artery disease.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Tanabe Y, Hosaka Y, Ito M, Ito E, Suzuki K. Significance of end-tidal P(CO(2)) response to exercise and its relation to functional capacity in patients with chronic heart failure. Chest. 2001;119(3):811–7. doi: 10.1378/chest.119.3.811. [DOI] [PubMed] [Google Scholar]
- 2.Hansen JE, Ulubay G, Chow BF, Sun XG, Wasserman K. Mixed-expired and end-tidal CO2 distinguish between ventilation and perfusion defects during exercise testing in patients with lung and heart diseases. Chest. 2007;132(3):977–83. doi: 10.1378/chest.07-0619. [DOI] [PubMed] [Google Scholar]
- 3.Idris AH, Staples ED, O'Brien DJ, Melker RJ, Rush WJ, Del Duca KD, et al. End-tidal carbon dioxide during extremely low cardiac output. Annals of emergency medicine. 1994;23(3):568–72. doi: 10.1016/s0196-0644(94)70080-x. [DOI] [PubMed] [Google Scholar]
- 4.Wasserman K, Zhang YY, Gitt A, Belardinelli R, Koike A, Lubarsky L, et al. Lung function and exercise gas exchange in chronic heart failure. Circulation. 1997;96(7):2221–7. doi: 10.1161/01.cir.96.7.2221. [DOI] [PubMed] [Google Scholar]
- 5.Matsumoto A, Itoh H, Eto Y, Kobayashi T, Kato M, Omata M, et al. End-tidal CO2 pressure decreases during exercise in cardiac patients: association with severity of heart failure and cardiac output reserve. Journal of the American College of Cardiology. 2000;36(1):242–9. doi: 10.1016/s0735-1097(00)00702-6. [DOI] [PubMed] [Google Scholar]
- 6.Myers JN, Gujja P, Neelagaru S, Hsu L, Burkhoff D. Noninvasive measurement of cardiac performance in recovery from exercise in heart failure patients. Clinics (Sao Paulo) 2011;66(4):649–56. doi: 10.1590/S1807-59322011000400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arena R, Peberdy MA, Myers J, Guazzi M, Tevald M. Prognostic value of resting end-tidal carbon dioxide in patients with heart failure. Int J Cardiol. 2006;109(3):351–8. doi: 10.1016/j.ijcard.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 8.Arena R, Guazzi M, Myers J. Prognostic value of end-tidal carbon dioxide during exercise testing in heart failure. Int J Cardiol. 2007;117(1):103–8. doi: 10.1016/j.ijcard.2006.04.058. [DOI] [PubMed] [Google Scholar]
- 9.Hagberg JM. Physiologic adaptations to prolonged high-intensity exercise training in patients with coronary artery disease. Medicine and science in sports and exercise. 1991;23(6):661–7. [PubMed] [Google Scholar]
- 10.Kendziorra K, Walther C, Foerster M, Mobius-Winkler S, Conradi K, Schuler G, et al. Changes in myocardial perfusion due to physical exercise in patients with stable coronary artery disease. Eur J Nucl Med Mol I. 2005;32(7):813–9. doi: 10.1007/s00259-005-1768-1. [DOI] [PubMed] [Google Scholar]
- 11.Eto Y, Koike A, Matsumoto A, Momomura S, Tajima A, Aizawa T, et al. Early aerobic training increases end-tidal CO2 pressure during exercise in patients after acute myocardial infarction. Circ J. 2004;68(8):778–83. doi: 10.1253/circj.68.778. [DOI] [PubMed] [Google Scholar]
- 12.Moholdt TT, Amundsen BH, Rustad LA, Wahba A, Lovo KT, Gullikstad LR, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: A randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;158(6):1031–7. doi: 10.1016/j.ahj.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Wasserma.K, Whipp BJ, Koyal SN, Beaver WL. Anaerobic Threshold and Respiratory Gas-Exchange during Exercise. J Appl Physiol. 1973;35(2):236–43. doi: 10.1152/jappl.1973.35.2.236. [DOI] [PubMed] [Google Scholar]
- 14. Braga A, Nunes N, In: ed Negrão CE, Barreto ACP, editors. Avaliação Cardiopulmonar Cardiologia do Exercício: do Atleta ao Cardiopata. Manole; 2005. p. 128–47 [Google Scholar]
- 15.Myers J, Gujja P, Neelagaru S, Hsu L, Vittorio T, Jackson-Nelson T, et al. End-tidal CO2 pressure and cardiac performance during exercise in heart failure. Medicine and science in sports and exercise. 2009;41(1):19–25. doi: 10.1249/MSS.0b013e318184c945. [DOI] [PubMed] [Google Scholar]
- 16.Tomita T, Takaki H, Hara Y, Sakamaki F, Satoh T, Takagi S, et al. Attenuation of hypercapnic carbon dioxide chemosensitivity after postinfarction exercise training: possible contribution to the improvement in exercise hyperventilation. Heart. 2003;89(4):404–10. doi: 10.1136/heart.89.4.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mifkova L, Siegelova J, Vymazalova L, Svacinova H, Vank P, Panovsky R, et al. [Interval and continuous training in cardiovascular rehabilitation] Vnitrni lekarstvi. 2006;52(1):44–50. [PubMed] [Google Scholar]
- 18.Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiov Prev R. 2004;11:216–222. doi: 10.1097/01.hjr.0000131677.96762.0c. [DOI] [PubMed] [Google Scholar]
- 19.Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients - A randomized study. Circulation. 2007;115(24):3086–94. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 20.Ciolac EG, Guimaraes GV, D'Avila VM, Bortolotto LA, Doria EL, Bocchi EA. Acute effects of continuous and interval aerobic exercise on 24-h ambulatory blood pressure in long-term treated hypertensive patients. Int J Cardiol. 2009;133(3):381–7. doi: 10.1016/j.ijcard.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Schairer JR, Kostelnik T, Proffitt SM, Faitel KI, Windeler S, Rickman LB, et al. Caloric expenditure during cardiac rehabilitation. J Cardiopulm Rehabil. 1998;18(4):290–4. doi: 10.1097/00008483-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Savage PD, Brochu M, Scott P, Ades PA. Low caloric expenditure in cardiac rehabilitation. Am Heart J. 2000;140(3):527–33. doi: 10.1067/mhj.2000.109219. [DOI] [PubMed] [Google Scholar]