Abstract
Objective
To identify the hospital admission data set that best captures the incidence of acute poisoning in rural Sri Lanka.
Methods
Data were collected on all acute poisoning cases admitted to 34 primary and 1 referral hospital in Anuradhapura district from September 2008 to January 2010. Three admission data sets were compared with the “true” incidence of acute poisoning to determine the systematic bias inherent to each data set. “True” incidence was calculated by adding all direct admissions (not transfers) to primary hospitals and to the referral hospital. The three data sets were: (i) all admissions to primary hospitals only; (ii) all admissions to the referral hospital only (direct and referrals), and (iii) all admissions to both primary hospitals and the referral hospital (“all admissions”). The third is the government’s routine statistical method but counts transfers twice, so for the study transferred patients were counted only once through data linkage.
Findings
Of 3813 patients admitted for poisoning, 3111 first presented to a primary hospital and 2287 (73.5%) were later transferred to the referral hospital, where most deaths (161/177) occurred. All data sets were representative demographically and in poisoning type, but referral hospital data yielded a more accurate case-fatality rate than primary hospital data or “all admissions” data. Admissions to primary hospitals only or to the referral hospital only underestimated the incidence of acute poisoning by about 20%, and data on “all admissions” overestimated it by 60%.
Conclusion
Admission data from referral hospitals are easily obtainable and accurately reflect the true poisoning incidence.
Résumé
Objectif
Identifier les données d'admission hospitalière qui identifient au mieux l'incidence des intoxications aiguës dans les régions rurales du Sri Lanka.
Méthodes
Les données ont été recueillies pour tous les cas d'intoxication aiguë admis dans 34 hôpitaux de première ligne et 1 hôpital de référence dans le district d'Anuradhapura de septembre 2008 à janvier 2010. Trois groupes de données d'admission ont été comparés avec l'incidence "réelle" des intoxications aiguës afin de déterminer le biais systématique inhérent à chaque ensemble de données. L'incidence "réelle" a été calculée en cumulant toutes les admissions directes (non-redirigées) dans les hôpitaux de première ligne et dans l'hôpital de référence. Les trois ensembles de données sont les suivants: (i) toutes les admissions dans les hôpitaux de première ligne uniquement, (ii) toutes les admissions à l'hôpital de référence uniquement (directes et redirigées) et (iii) toutes les admissions dans des hôpitaux de première ligne ainsi qu’à l'hôpital de référence ("toutes les admissions"). Le troisième groupe constitue la méthode statistique gouvernementale usuelle mais comptabilise deux fois les cas transférés alors que, dans le cadre de cette étude, les patients référés n'ont été comptés qu'une seule fois par recoupement de données.
Résultats
Sur 3 813 patients admis pour une intoxication, 3 111 se sont initialement présentés à l'hôpital de première ligne et 2 287 (73,5%) ont été ultérieurement transférés vers l'hôpital de référence, où la plupart des décès (161/177) se sont produits. Tous les groupes de données étaient représentatifs tant sur le plan démographique que concernant le type d'intoxication, mais les données de l'hôpital de référence ont abouti à une mesure plus précise du taux de mortalité que les données des hôpitaux de première ligne ou que les données "toutes les admissions". Les admissions dans les hôpitaux de première ligne seuls ou à l'hôpital de référence seul ont sous-estimé l'incidence des intoxications aiguës d'environ 20% et les données sur "toutes les admissions" l'ont surestimée de 60%.
Conclusion
Les données d'admission des hôpitaux de référence sont faciles à obtenir et reflètent fidèlement l'incidence véritable des intoxications.
Resumen
Objetivo
Identificar el conjunto de datos de ingresos hospitalarios que mejor recoja la incidencia de la intoxicación aguda en la Sri Lanka rural.
Métodos
Se recopilaron datos de todos los ingresos por intoxicación aguda en 34 hospitales primarios y un hospital de derivación en el distrito de Anuradhapura, entre septiembre de 2008 y enero de 2010. Se compararon tres conjuntos de datos de ingresos con la incidencia «real» de intoxicación aguda para determinar el sesgo sistemático inherente a cada conjunto de datos. La incidencia «real» se calculó sumando todos los ingresos directos (no remisiones) de los hospitales primarios y del hospital de derivación. Los tres conjuntos de datos fueron: (i) únicamente todos los ingresos en hospitales primarios; (ii) únicamente todos los ingresos en el hospital de derivación (directos y remisiones) y (iii) todos los ingresos tanto en hospitales primarios como en el hospital de derivación («todos los ingresos»). El tercero es el método estadístico rutinario del gobierno, pero en éste las remisiones se cuentan dos veces, así que para el estudio solo se tuvieron en cuenta una vez los pacientes remitidos a través de la interrelación de datos.
Resultados
De los 3813 pacientes ingresados por intoxicación, 3111 acudieron en primer lugar a un hospital primario y 2287 (73,5%) fueron remitidos posteriormente al hospital de derivación, donde se registraron la mayoría de los fallecimientos (161/177). Todos los conjuntos de datos eran representativos demográficamente y por tipo de intoxicación, si bien los datos del hospital de derivación arrojaron una tasa de mortalidad más precisa que los del hospital primario o los de «todos los ingresos». Los conjuntos de datos que contemplaban únicamente los ingresos en los hospitales primarios o únicamente los ingresos en el hospital de derivación subestimaron la incidencia de la intoxicación aguda en aproximadamente un 20% y los datos de «todos los ingresos» la sobreestimaron en un 60%.
Conclusión
Los datos de ingreso de los hospitales de derivación se pueden obtener fácilmente y reflejan de forma precisa la incidencia de intoxicación real.
ملخص
الغرض
تحديد مجموعة بيانات دخول المستشفيات التي ترصد على النحو الأمثل حدوث التسمم الحاد في المناطق الريفية في سري لانكا.
الطريقة
تم جمع البيانات المعنية بجميع حالات التسمم الحاد التي دخلت إلى 34 مستشفى أولية ومستشفى إحالة واحد في مقاطعة آنورادابورا في الفترة من أيلول/سبتمبر 2008 إلى كانون الثاني/يناير 2010. وتمت مقارنة ثلاثة مجموعات بيانات دخول بالحدوث "الحقيقي" للتسمم الحاد لتحديد الانحراف المنهجي المتأصل لكل مجموعة بيانات. وتم حساب الحدوث "الحقيقي" بإضافة جميع حالات الدخول المباشرة (وليس التحويلات) إلى المستشفيات الأولية وإلى مستشفى الإحالة. وتمثلت مجموعات البيانات الثلاثة فيما يلي: (1) جميع حالات الدخول إلى المستشفيات الأولية فقط؛ (2) جميع حالات الدخول إلى مستشفى الإحالة فقط (المباشرة والإحالات)، (3) جميع حالات الدخول إلى كل من المستشفيات الأولية ومستشفى الإحالة ("جميع حالات الدخول"). وتمثل المجموعة الثالثة الأسلوب الإحصائي الروتيني الحكومي غير أنها تقوم بإحصاء التحويلات مرتين، ولذا لأغراض هذه الدراسة، تم إحصاء المرضى المحولين مرة واحدة فقط من خلال ارتباط البيانات.
النتائج
تم أولاً تقديم 3111 مريضًا، من إجمالي 3813 مريضًا دخلوا المستشفيات للعلاج من التسمم، إلى إحدى المستشفيات الأولية/ وتم فيما بعد نقل 2287 (73.5 %) مريضًا إلى مستشفى الإحالة حيث حدثت معظم حالات الوفاة (161/177). وكانت جميع مجموعات البيانات تمثيلية من الناحية الديمغرافية وضمن فئة التسمم، غير أن بيانات مستشفى الإحالة أدت إلى الحصول على معدل إماتة أكثر دقة عن بيانات المستشفى الأولي أو بيانات "جميع حالات الدخول". وقدرت حالات الدخول إلى المستشفيات الأولية فقط أو إلى مستشفى الإحالة فقط حدوث التسمم الحاد بأقل مما ينبغي بنسبة 20 % تقريبًا وقدرت البيانات المعنية "بجميع حالات الدخول" هذا الحدوث بأكثر مما ينبغي بنسبة 60 %.
الاستنتاج
يمكن الحصول بسهولة على بيانات الدخول من مستشفيات الإحالة وهي تعكس بدقة حدوث التسمم الحقيقي.
摘要
目的
识别出能够最好地捕获斯里兰卡农村急性中毒发生率的入院数据集。
方法
收集从2008 年9 月至2010 年1 月在阿努拉德普勒区34 所基层和1 所转诊医院入院的所有急性中毒病例的数据。将三套入院数据集与“真实”的急性中毒发生率进行比较,确定每个数据集固有的系统性偏差。“真实”的发生率通过将基层医院和转诊医院所有直接的入院(非转院)数据相加计算得出。三个数据集是:(i)所有仅在基层医院的入院;(ii)所有仅在转诊医院的入院(直接或转诊);(iii)所有在基层医院和转诊医院的入院(“所有入院”)。第三个是政府常规统计方法,但是将转诊计算了两次,所以研究中通过数据联动仅计算转院的患者一次。
结果
因中毒入院的3813 名患者中,3111 名首先在基层医院就诊,2287 名(73.5%)之后转到转诊医院,其中多数死亡发生在转诊医院(161/177)。所有数据集在人口的中毒类型方面具有代表性,但是转诊医院数据得到比基层医院数据或“所有入院”数据更为准确的病死率。仅基层医院入院或者仅转诊医院入院低估了急性中毒发生率约20%,而“所有入院”数据则高估了约60%。
结论
转诊医院的入院数据容易获得,准确反映了真实的中毒发生率。
Резюме
Цель
Определить набор данных госпитализации, наиболее явно отражающих частоту острых отравлений в сельской местности Шри-Ланки.
Методы
В период с сентября 2008 по январь 2010 гг. были собраны данные обо всех случаях госпитализации при остром отравлении в 34 центрах первичной медицинской помощи и 1 лечебно-диагностическом центре в районе города Анурадхапура. Для установления степени неустранимой систематической погрешности каждого набора данных было проведено сравнение между зарегистрированной частотой случаев острых отравлений согласно 3 наборам данных госпитализации, и фактической частотой таких случаев. Фактическая частота была рассчитана путем подсчета всех случаев госпитализации (не переводов из других медицинских центров) непосредственно в центры первичной медицинской помощи и лечебно-диагностический центр. Эти 3 набора данных включали в себя следующую информацию: (i) все случаи госпитализации только в центры первичной медицинской помощи; (ii) все случаи госпитализации только в лечебно-диагностический центр (непосредственная госпитализация и направления); и (iii) все случаи госпитализации в центры первичной медицинской помощи и лечебно-диагностический центр (общее количество). Треть случаев подсчитана с помощью государственного стандартного статистического метода, но подсчитана дважды. Поэтому в рамках исследования случаи перевода пациентов были подсчитаны один раз, путем сопоставления данных.
Результаты
Из 3813 пациентов, госпитализированных с отравлениями, 3111 пациентов сначала были госпитализированы в центры первичной медицинской помощи, и 2287 (73,5%) пациентов позже были переведены в лечебно-диагностический центр, где было зарегистрировано большинство случаев летального исхода (161/177). Все наборы данных отражали число пациентов и тип отравления, однако данные лечебно-диагностического центра отражали наиболее точное число случаев госпитализации с летальным исходом, чем данные центров первичной медицинской помощи и данные о госпитализации всех центров в общем. В данных госпитализации только в центры первичной медицинской помощи или только в лечебно-диагностический центр число случаев госпитализации при остром отравлении было занижено на 20%, а общее количество случаев госпитализации при остром отравлении во всех центрах было завышено на 60%.
Вывод
Данные о госпитализации, полученные от лечебно-диагностических центров, являются легкодоступными и точно отражают число случаев отравления.
Introduction
Death from acute poisoning is a major public health issue in many countries. Most deaths are from self-poisoning with highly toxic pesticides, which globally account for the overwhelming majority of poisoning deaths and around one third of all suicides.1 The problem is most widespread in rural areas of developing countries.2,3 This is true of Sri Lanka, where poisoning is among the top five causes of in-hospital deaths in rural areas.4,5 Although acute poisoning can be either intentional or accidental, Sri Lankan hospitals see few accidental poisonings and almost all admissions are due to deliberate self-poisoning.6,7
Continuous surveillance of cases of acute poisoning is important for planning and evaluating public health interventions. However, the methods required for such surveillance are potentially complicated, since the majority of poisoned patients present to small primary hospitals for initial assessment and care and are later transferred to secondary (referral) hospitals.8 To date, most epidemiological studies in Sri Lanka have been performed in these larger referral hospitals,9 as have nearly all hospital studies used to estimate pesticide poisoning rates elsewhere in the world.1 Such studies may be subject to various forms of selection bias. On the other hand, official government statistics are usually a sum of the admission statistics from all hospitals. Since existing surveillance systems rarely allow data linkage to track patients transferred from primary to referral hospitals, transferred patients end up being counted twice. This obviously creates a bias that can result, for example, in an underestimation of the case-fatality rate.8 Hence, it is important, especially in the developing world, to identify a good but uncomplicated strategy for accurately collecting data on acute poisonings and to estimate the magnitude and direction of the systematic bias inherent in various data collection methods. The objective of our study was to explore which of three different data collection methods could deliver the most accurate estimates of the incidence of acute poisoning in a rural district of Sri Lanka.
Methods
For 17 consecutive months we collected data on all admissions of acutely poisoned patients to all hospitals with inpatient beds in Anuradhapura, a large rural district in Sri Lanka’s North Central Province. This included 34 primary hospitals and one referral hospital.
The data were collected as part of a cluster-randomized controlled trial (ISRCTN73983810) that was designed to assess the effect of a brief educational intervention about the management of poisoned patients in primary hospitals. The study established data linkage between the primary and referral hospitals to enable the follow-up of all transferred patients and validate the primary hospital medical record by means of direct interviews with transferred patients.
Anuradhapura district had a total of 820 000 inhabitants, 631 715 of which were above the age of 12 years in mid 2009. The district’s land area represents about 11% of the national territory.10 Demographically and socioeconomically its population is representative of rural Sri Lanka, and so are its health-care services.10,11
All public hospitals with inpatient facilities in the district were included in the study. The 34 primary hospitals are the first point of health system contact for the majority of poisoned patients, many of whom are then transferred to the referral hospital, which has an intensive care unit with specialized staff and better stocks of antidotes and medication. The region has four small private hospitals, all of which were excluded from the study because they indicated that they never provided care for poisoned patients.
We collected data on all patients who were 12 years of age or older and who were admitted into study hospitals for acute poisoning from 1 September 2008 to 30 January 2010. During admission, staff examined any traces of the poison ingested or the product label or bottle and obtained a history from the patient or the patient’s family. They also made note of the clinical symptoms to support the diagnosis, and all details concerning exposure, clinical assessment, case management and clinical outcome were recorded for each patient by the treating medical staff. In primary hospitals these records were kept aside for several weeks for later retrospective extraction of data by trained research assistants using a structured data collection form. All data were entered into an Access (Microsoft, Redmond, United States of America) computer database. Admission log books were checked in each hospital to ensure that all cases were identified and traced. Data entry quality was also validated by comparing the data collected for patients transferred to the referral hospital with the data appearing in the records.
At the referral hospital, all patients who were admitted (either directly or as a transfer from a primary hospital) were examined and interviewed by study physicians during admission. Data on the patients’ demographic profile, poison exposure details, history, clinical assessment, management and outcome were prospectively collected and entered into a study database.
The Sri Lankan health system has no unique patient identifier. We identified patients who were transferred from primary hospitals to the referral hospital by using a data-linkage computer algorithm to search the primary and referral hospitals’ study databases, supplemented by occasional manual checking when the algorithm failed to produce a unique match. Only adult patients are treated in medical wards in referral hospitals; patients less than 12 years of age are referred as paediatric admissions. Since we had no access to paediatric wards and records, we could only identify and link adult patients for this study.
Statistical analysis
We obtained data for each unique patient through the labour-intensive process earlier described, as it was considered to reflect the true incidence of acute poisoning in the study district over the study period. The census population above 12 years of age in 2009 was the denominator used to calculate the incidence of acute poisoning and the population rate of death from acute poisoning. We then compared the incidence “observed” using three different possible admission data sets against the patient admission data set considered to be the most accurate, namely, the sum of all admissions to primary hospitals and to the referral hospital, minus all inter-hospital transfers. The three data sets were:
all admissions to primary hospitals only;
all admissions to the referral hospital only, both direct and referred from a primary hospital;
the sum of all recorded admissions to primary hospitals and to the referral hospital (“all admissions”, routine method used for government statistics, which counts referrals twice).
For each data set we calculated the incidence of poisonings and case-fatality rates, both overall and for selected subgroups based on demographics and poison type. We calculated exact 95% confidence intervals (CIs) for estimated proportions. We compared the “true” data with each of the three admission data sets by examining the difference in patient numbers and the ratio of estimated proportions and by determining if the “true” value was included in the CIs. All analyses were conducted in Stata version 11.0 (StataCorp. LP, College Station, United States of America) and graphs were produced using GraphPad Prism version 5.0 software (GraphPad Software, La Jolla, USA).
Ethical clearance
This study protocol was approved by the Human Research Ethics Committee of the University of Sydney, Australia (Ref Number: 12083) and the Ethics Review Committee of the University of Peradeniya, Sri Lanka.
Results
Incidence of poisoning
In total, 3813 poisoned patients (above 12 years of age) were admitted to the hospitals in Anuradhapura district during the 17-month data collection period. The overall annual population incidence among people above 12 years of age was 426 per 100 000, while the annual population incidence in females was slightly higher than in males (450 versus 408 per 100 000, respectively). In-hospital deaths totalled 177, and the annual population mortality rate for acute poisoning was 19.8 per 100 000 for the population above 12 years of age.
Most poisoning admissions (97%) were deliberate self-poisonings; only 3% (119/3813) were accidental poisonings. These occurred mainly while spraying or preparing pesticides, as accidental ingestions, or as a result of medication dosing errors or food poisoning. No deaths were recorded in this group.
Of the 3813 patients admitted for acute poisoning, 3111 (81.6%) were initially admitted to primary hospitals, and 2287 (73.5%) were subsequently transferred to the referral hospital. Direct admissions to the referral hospital totalled 702 (18.4%). Thus, a data set composed of all hospital admissions resulted in the double counting of more than half the patients, whereas each of the two other admission data sets underestimated the incidence by about 20% (Table 1).
Table 1. “True” acute poisoning admissions, by age and sex, and systematic bias observed in estimates obtained through three possible hospital admission data sets, Anuradhapura district, Sri Lanka, September 2008 to January 2010.
| Group | No. of “true” total admissionsa | All admissions to primary hospitals onlyb |
All admissions to referral hospital onlyc |
All admissionsd |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Absolute difference | Per cent difference (bias) | No. | Absolute difference | Per cent difference (bias) | No. | Absolute difference | Per cent difference (bias) | |||||||||||
|
Age (years)e |
|||||||||||||||||||
| 12−14 |
120 |
97 |
23 |
19.2 |
94 |
26 |
21.7 |
191 |
71 |
59.2 |
|||||||||
| 15−19 |
980 |
811 |
169 |
17.2 |
739 |
241 |
24.6 |
1550 |
570 |
58.3 |
|||||||||
| 20−29 |
1364 |
1081 |
283 |
20.7 |
1098 |
266 |
19.5 |
2179 |
815 |
59.8 |
|||||||||
| 30−39 |
607 |
489 |
118 |
19.4 |
496 |
111 |
18.3 |
985 |
378 |
62.3 |
|||||||||
| 40−49 |
416 |
351 |
65 |
15.6 |
325 |
91 |
21.9 |
676 |
260 |
62.5 |
|||||||||
| 50−59 |
210 |
182 |
28 |
13.3 |
152 |
58 |
27.6 |
334 |
124 |
59.0 |
|||||||||
| ≥ 60 |
95 |
79 |
16 |
16.8 |
71 |
24 |
25.3 |
150 |
55 |
58.0 |
|||||||||
| Total | 3792 | 3090 | 702 | 18.5 | 2976 | 816 | 21.7 | 6066 | 2274 | 60.0 | |||||||||
| Sex | |||||||||||||||||||
| Females | 1952 | 1578 | 374 | 19.2 | 1512 | 440 | 22.5 | 3090 | 1138 | 58.3 | |||||||||
| Males | 1861 | 1533 | 328 | 17.6 | 1477 | 384 | 20.6 | 3010 | 1149 | 61.7 | |||||||||
|
Poisoning type |
|||||||||||||||||||
| All pesticides |
1573 |
1352 |
221 |
14.0 |
1293 |
280 |
17.8 |
2989 |
1416 |
90.0 |
|||||||||
| Medicine overdose |
789 |
561 |
228 |
28.9 |
627 |
162 |
20.5 |
1188 |
399 |
50.6 |
|||||||||
| Other poison |
1451 |
1198 |
253 |
17.4 |
1060 |
391 |
26.9 |
2258 |
807 |
55.6 |
|||||||||
| Total | 3813 | 3111 | 702 | 18.5 | 2974 | 817 | 21.6 | 6063 | 2272 | 59.9 | |||||||||
a Sum of all direct acute poisoning admissions to the district’s primary hospitals and its referral hospital (i.e. all admissions minus transfers).
b All admissions to primary hospitals only (all are direct admissions, not referrals).
c All admissions (both direct and transfers) to the referral hospital.
d Raw total of all admissions to all hospitals in the district (routine method used for government statistics, which double counts patients transferred to referral hospitals).
e No age was recorded for 21 patients.
Poisoned patients ranged in age from 12 to 86 years (median age: 24 years; inter-quartile range [IQR]: 19–35), and 1952 (51.1%) were female. No age was recorded for 21 patients – 8 females and 13 males. These patients were not included in age-group comparisons.
Observed age, sex and poison
Despite the double-counting or under-counting of admissions, all admission data sets were approximately similar in sex and age distribution (Table 2, available at: http://www.who.int/bulletin/volumes/90/6/11-092114). Minor errors were noted (all less than 20%) in the estimated proportion of different types of poisoning (Table 2).
Table 2. “True” acute poisoning admissions and number of admissions that would be obtained with three possible hospital admission data sets, by age, sex and poisoning type, Anuradhapura district, Sri Lanka, September 2008 to January 2010.
| Group | “True” total admissionsa |
All admissions to primary hospitals onlyb |
All admissions to referral hospital onlyc |
All admissionsd |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % (95% CI) | Proportions ratio | No. | % (95% CI) | Proportions ratio | No. | % (95% CI) | Proportions ratio | ||||||||||
| Males (by age in years)e | ||||||||||||||||||||
| 12–14 | 36 | 2 | 27 | 1.8 (1.2–2.6) | 0.91 | 30 | 2 (1.4–2.9) | 1.05 | 57 | 1.9 (1.4–2.5) | 0.98 | |||||||||
| 15–19 | 282 | 15.3 | 231 | 15.2 (13.4–17.1) | 1.00 | 220 | 15 (13.2–16.9) | 0.98 | 451 | 15.1 (13.8–16.4) | 0.99 | |||||||||
| 20–29 | 626 | 33.9 | 511 | 33.6 (31.2–36.1) | 0.99 | 507 | 34.5 (32.1–37.0) | 1.02 | 1018 | 34.1 (32.4–35.8) | 1.00 | |||||||||
| 30–39 | 357 | 19.3 | 292 | 19.2 17.3–21.3) | 1.00 | 288 | 19.6 (17.6–21.7) | 1.02 | 580 | 19.4 (18.0–20.9) | 1.01 | |||||||||
| 40–49 | 306 | 16.6 | 254 | 16.7 (14.9–18.7) | 1.01 | 246 | 16.7 (14.9–18.8) | 1.01 | 500 | 16.7 (15.4–18.1) | 1.01 | |||||||||
| 50–59 | 169 | 9.1 | 145 | 9.5 (8.1–11.1) | 1.05 | 124 | 8.4 (7.1–10.0) | 0.93 | 269 | 9 (8.0–10.1) | 0.99 | |||||||||
| ≥ 60 | 73 | 4.0 | 60 | 3.9 (3.0–5.1) | 0.99 | 54 | 3.7 (2.8–4.8) | 0.92 | 114 | 3.8 (3.2–4.6) | 0.95 | |||||||||
| Total | 1849 | 48.8 | 1520 | 49.2 (47.4–51.0) | 1.01 | 1469 | 49.1 (47.3–51.0) | 1.01 | 2989 | 49.3 (48.0–50.6) | 1.01 | |||||||||
| Females (by age in years)e | ||||||||||||||||||||
| 12–14 | 84 | 4.3 | 70 | 4.5 (3.5–5.6) | 1.03 | 64 | 4.1 (3.2–5.3) | 0.95 | 134 | 4.3 (3.6–5.1) | 0.99 | |||||||||
| 15–19 | 698 | 35.9 | 580 | 37 (34.6–39.4) | 1.03 | 520 | 34.6 (32.1–37.0) | 0.96 | 1100 | 35.8 (34.1–37.5) | 1.00 | |||||||||
| 20–29 | 738 | 38 | 570 | 36.3 (33.9–38.8) | 0.96 | 591 | 39.3 (36.8–41.8) | 1.03 | 1161 | 37.8 (36.0–39.5) | 0.99 | |||||||||
| 30–39 | 250 | 12.9 | 197 | 12.6 (11.0–14.3) | 0.98 | 208 | 13.8 (12.1–15.7) | 1.07 | 405 | 13.2 (12.0–14.4) | 1.02 | |||||||||
| 40–49 | 110 | 5.7 | 97 | 6.2 (5.0–7.5) | 1.09 | 79 | 5.2 (4.2–6.5) | 0.93 | 176 | 5.7 (4.9–6.6) | 1.01 | |||||||||
| 50–59 | 41 | 2.1 | 37 | 2.4 (1.7–3.2) | 1.12 | 28 | 1.9 (1.2–2.7) | 0.88 | 65 | 2.1 (1.6–2.7) | 1.00 | |||||||||
| ≥ 60 | 22 | 1.1 | 19 | 1.2 (0.7–1.9) | 1.07 | 17 | 1.1 (0.7–1.8) | 1.00 | 36 | 1.2 (0.8–1.6) | 1.03 | |||||||||
| Total | 1943 | 51.2 | 1570 | 50.8 (49.0–52.6) | 0.99 | 1507 | 50.4 (48.5–52.2) | 0.98 | 3075 | 50.7 (49.4–52.0) | 0.99 | |||||||||
| Poisoning type | ||||||||||||||||||||
| Organophosphates and carbamate | 706 | 18.5 | 603 | 19.4 (18.0–20.8) | 1.05 | 601 | 20.1 (18.7–21.6) | 1.09 | 1204 | 19.7 (18.7–20.8) | 1.07 | |||||||||
| Paraquat | 77 | 2.0 | 55 | 1.8 (1.3–2.3) | 0.88 | 71 | 2.4 (1.9–3.0) | 1.18 | 126 | 2.1 (1.7–2.5) | 1.02 | |||||||||
| Other pesticide | 790 | 20.7 | 694 | 22.3 (20.9–23.8) | 1.08 | 621 | 20.8 (19.3–22.3) | 1.00 | 1315 | 21.6 (20.5–22.6) | 1.04 | |||||||||
| Medicine overdose | 789 | 20.7 | 561 | 18 (16.7–19.4) | 1.15 | 627 | 21.0 (19.5–22.5) | 1.01 | 1188 | 19.5 (18.5–20.5) | 0.94 | |||||||||
| Oleander | 393 | 10.3 | 299 | 9.6 (8.6–10.7) | 1.07 | 363 | 12.1 (11.9–13.4) | 1.18 | 662 | 10.9 (10.1–11.7) | 1.05 | |||||||||
| Other | 1058 | 27.7 | 899 | 28.9 (27.3–30.5) | 1.04 | 706 | 23.6 (22.1–25.2) | 0.85 | 1605 | 26.3 (25.2– 27.4) | 0.95 | |||||||||
| Total | 3813 | 100.0 | 3111 | 100 | – | 2989 | 100 | – | 6100 | 100 | – | |||||||||
CI, confidence interval.
a Sum of all direct acute poisoning admissions to the district’s primary hospitals and its referral hospital (i.e. all admissions minus transfers).
b All admissions to primary hospitals (all are direct admissions, not referrals).
c All admissions (both direct and transfers) to the referral hospital.
d Raw total of all admissions to all hospitals in the district (routine method used for government statistics, which double counts patients transferred to referral hospitals).
e No age was recorded for 21 patients (includes males and females).
Variation in mortality and case-fatality
The case-fatality rate among patients admitted to primary hospitals and not transferred was low (1.9%); the case-fatality rate among transferred patients was comparable to the rate observed in patients directly admitted to the referral hospital. This suggests that primary hospitals correctly identify nearly all high-risk patients and transferred them appropriately (Table 3). The best estimate of the actual number of deaths was provided by the “all admissions” data set, but most deaths (161/177) were found in the data set of admissions to the referral hospital exclusively (Table 3). Only two patients died during the transfer to the referral hospital.
Table 3. “True” case-fatality rate (CFR) for various poison types and CFRs that would be obtained with three possible hospital admission data sets, Anuradhapura district, Sri Lanka, September 2008 to January 2010.
| Poisoning type | “True” totala |
Primary hospitalsb |
Referral hospitalc |
All admissionsd |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. admitted | CFR | No. admitted | Deaths | CFR (95% CI) | No. admitted | Deaths | CFRe (95% CI) | No. admitted | Deaths | CFR (95% CI) | |||||||
| Directly | Transferred | In cases admitted directly | In transfers | ||||||||||||||
| Organophosphates and carbamate |
706 |
5.8 |
603 |
6 |
1.0 (0.4–2.2) |
103 |
498 |
6 |
29 |
5.8 (4.1–8.0) |
1204 |
41 |
3.4 (2.5–4.6) |
||||
| Paraquat |
77 |
22.1 |
55 |
0 |
0.0 (0.0–6.5) |
22 |
49 |
8 |
9 |
23.9 (14.6–35.5) |
126 |
17 |
13.5 (8.1–20.7) |
||||
| Other pesticide |
790 |
4.8 |
694 |
4 |
0.6 (0.2–1.5) |
95 |
526 |
0 |
34 |
5.5 (3.8–7.6) |
1315 |
38 |
2.9 (2.1–3.9) |
||||
| Medicine overdose |
789 |
0.6 |
561 |
0 |
0.0 (0.0–0.7) |
228 |
399 |
0 |
5 |
0.8 (0.3–1.9) |
1188 |
5 |
0.4 (0.1–1.0) |
||||
| Oleander |
393 |
4.1 |
299 |
1 |
0.3 (0.01–1.8) |
94 |
269 |
2 |
13 |
4.1 (2.3–6.7) |
662 |
16 |
2.4 (1.4–3.9) |
||||
| Other |
1058 |
5.7 |
899 |
5 |
0.6 (0.2–1.3) |
106 |
546 |
6 |
49 |
7.8 (5.9–10.0) |
1605 |
60 |
3.7 (2.9–4.8) |
||||
| Total | 3813 | 4.6 | 3111 | 16 | 0.5 (0.3–0.8) | 702 | 2287 | 22 | 139 | 5.4 (4.6–6.3) | 6091 | 177 | 2.9 (2.5–3.4) | ||||
CI, confidence interval.
a Sum of all direct acute poisoning admissions to the district’s primary hospitals and its referral hospital (i.e. all admissions minus transfers).
b All admissions to primary hospitals (all are direct admissions, no referrals).
c All admissions (both direct and transfers) to the referral hospital.
d Raw total of all admissions to all hospitals in the district (routine method used for government statistics, which double counts patients transferred to referral hospitals).
e CFR is based on the sum of deaths among transferred patients and patients directly admitted.
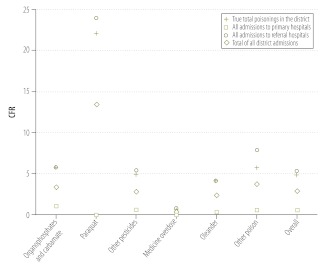
Admission data sets for the primary hospital only and the “all admissions” data set substantially underestimated overall case-fatality. The best case-fatality estimate was provided by referral hospital admissions data (Fig. 1 and Table 3). This was also true for the case-fatality rates pertaining to specific types of poisoning (Fig. 1). The “true” case-fatality rate falls within the CI of the case-fatality rate derived from referral hospital data (Table 3).
Fig. 1.
“True” case-fatality rate (CFR) in patients admitted to hospital for acute poisoning and CFRs based on three possible hospital admission data sets, Anuradhapura district, Sri Lanka, September 2008 to January 2010
Discussion
The developing world bears a disproportionate share of the global burden of suicide by poisoning. This is largely because the agents commonly ingested in cases of self-poisoning in these countries, such as pesticides, tend to have higher toxicity.1 However, the types of poisons used in deliberate self-poisoning and their lethality vary substantially in the developing world. Epidemiological data are important because they provide information used to plan and evaluate public health responses. In this paper, we have demonstrated that in a rural district in Sri Lanka the simplest approach is to use data on admissions to the referral hospital, which is not only reasonably representative of poisonings in the entire district but also more accurate than any other hospital admission data set that does not track transferred patients. The public health structure and referral patterns in most of rural Sri Lanka are similar. Thus, we believe that our findings apply to all rural districts in Sri Lanka. The use of referral hospitals for toxicovigilance is more convenient, less expensive and better suited to detailed prospective data collection than other methods. Our findings also help to validate the results of previous studies in rural Sri Lanka based on the use of data for acute poisoning admissions to referral hospitals.8
The potential limitations of the suggested method of toxicovigilance need to be considered. In this study primary hospital data were collected retrospectively from patient records by research assistants within 3 weeks of admission using a structured form. We verified the completeness of case-finding by comparing the data thus collected with the data in each hospital’s admissions book. We also validated the quality of data entry by comparing the data collected for the 75% of patients who were transferred to the referral hospital with the data appearing in the books.
In the referral hospital, data were prospectively collected by junior research physicians who provided 24-hour coverage. This data collection included all data elements collected for referred patients in the primary hospital. Validation confirmed the accuracy of data extraction in primary hospitals. The referral hospital tended to identify the specific poison ingested, whereas primary hospitals tended to list only the chemical class. This is important because agents belonging to the same chemical class vary substantially in their toxicity. Poisoning exposure data that aggregates exposures by chemical groups is seldom useful for developing effective public health response measures, including regulatory restriction of specific compounds.9
In the study district the transfer rate from primary hospitals to the referral hospital was very high. In Sri Lanka, transfers are initiated by physicians in primary hospitals; there are few barriers and no fixed protocol. As previously noted, the resultant double-counting of transferred cases in official statistics leads to large underestimates of the mean case-fatality rates for all poisonings.8
During the study period, deaths from acute poisoning totalled 177 in all hospitals in the study district. Previous studies in the district showed that 96% of deaths from pesticide ingestion occur in public hospitals. This probably reflects easy access to the public health system and the fact that the most toxic pesticides that can cause a rapid death are banned.12,13
Data on “all admissions”, used by the government to derive the population incidence, overestimated the incidence of self-poisoning by about 60%. In 2007, 5118 cases of acute poisoning occurred in Anuradhapura district, for an official incidence of 639 per 100 000.14 In our study, the observed “true” population incidence of acute poisoning in 2008–2010 was 461 per 100 000 (2962 annual cases on average). A casual reader might assume that incidence of acute poisoning has changed dramatically, whereas the difference can be entirely explained by the double counting. In contrast, in our study the estimated average true annual incidence of death from acute poisoning was almost identical to the rate derived from “all admissions”, used for government statistics: 14.1 per 100 000 (113 deaths per year on average)15 from government statistics versus 15.2 per 100 000 (125 deaths per year on average) in our study.
Our “gold standard” study, intended to identify the most accurate hospital admission data set required to calculate the incidence of acute poisoning, required a large team of research assistants and auditors and labour-intensive data linkage to avoid undercounting or double counting cases. Such complicated surveillance is unlikely to be practical in a broader, non-research public health setting. This study suggests that referral hospital admissions data can yield incidence and case-fatality estimates very close to the “true” or “gold standard” figures in many respects and are therefore the best hospital data set for this purpose. Collecting data from larger referral hospitals only, has other advantages over collecting it from dozens of small primary hospitals. The large number of patients justifies prospective data collection by a small team, which makes it much easier to ensure good data quality and to collect the data more quickly and efficiently. Data can easily be expanded to include more details on exposure or on the circumstances surrounding the poisoning, the specific chemical used and the clinical management required. Such data can facilitate public health education, research and interventions.
In Sri Lanka, most hospital admissions for acute poisoning are deliberate self-poisonings. Surprisingly, the small, primary hospitals provided little data regarding the less serious occupational and other accidental exposures. Although our study showed minor differences in the type of acute poisoning cases presenting to primary hospitals, referral hospital data captured most of these patients and was generally a better source of data for calculating incidence and case-fatality than primary hospital admissions data. Current government statistics have the additional problem of being based largely on coded data from all hospitals, and as a result they only contain data for the poison’s chemical class (four broad categories) and for patient age and sex. The lack of details on specific types of poison limits the use of government statistics for targeting regulatory responses and assessing interventional studies. In our study relatively few deaths occurred in primary hospitals, and this further confirms that such hospitals correctly identify and transfer nearly all high-risk patients.15,16 However, transferred cases rarely died of medication poisoning, which suggests that few such patients need to be transferred for more intensive treatment. Reducing these transfers may save health resources.
Our results may be applicable to rural districts in developing countries at large, particularly if their health systems and referral patterns are comparable to those of Sri Lanka. In this country’s rural provinces, most patients live within 30 minutes (by motorized vehicle transport) of a primary hospital, and primary hospitals are typically at a distance of 1 to 4 hours from the referral hospital by vehicle transport. Public health care is free; the private sector is relatively underdeveloped and poisonings very rarely present to private hospitals. The toxicity of the poisons ingested in Sri Lanka is such that poisoned patients usually reach the hospital alive and seldom die during transfer or have a worse outcome than patients who present directly to referral hospitals.9 However, poisons with very rapid onset of toxicity and death may be subject to a different sampling bias. For example, in Sri Lanka’s Southern Province we have reported on the high toxicity of a cleaning agent that quickly causes death.17 When using any sentinel data source, it is important to know the time-course of common poisonings to understand whether the representativeness of the data is threatened by the inclusion of cases of poisoning with certain compounds. Our method of conducting toxicovigilance requires an understanding of both patient transfer patterns and the degree of toxicity of common poisons to know what adjustments should be made in interpreting the data.
Conclusion
In Sri Lanka, acute poisoning cases admitted to primary and referral hospitals differ in terms of the poisons ingested, case severity and case-fatality. However, because most patients are subsequently transferred to referral hospitals, admission data from referral hospitals only can be used with reasonable accuracy to represent the true incidence of acute poisoning within an entire province. Studies in other countries should be conducted to try to validate this approach.18
Acknowledgements
We thank W Attapattu, Provincial Director of Health Services, North Central Province, Palitha Bandara (Regional Director of Health Services – Anuradhapura), Dhammika de Silva (MO Planning – North Central Province), Director of the Teaching Hospital in Anuradhapura and all physicians and other hospital staff members in Anuradhapura district. We also thank Indika Gawarammana, Fahim Mohamed, Aruna Kumara and other research assistants, and the office staff of the South Asian Clinical Toxicology Research Collaboration, as well as HR Dias, Deputy Director of the Population Census and Demography Division of Sri Lanka’s Department of Census and Statistics.
Funding:
The South Asian Clinical Toxicology Research Collaboration funded this study (Wellcome Trust/National Health and Medical Research Council International Collaborative Research Grant GR071669MA and NHMRC GNT0630650). Lalith Senarathna was supported by the Australian Endeavour Postgraduate Award. None of the funding sources had any role in study design, in data collection, analysis or interpretation, or in the preparation or publication of this paper.
Competing interests:
None declared.
References
- 1.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van der Hoek W, Konradsen F, Athukorala K, Wanigadewa T. Pesticide poisoning: a major health problem in Sri Lanka. Soc Sci Med. 1998;46:495–504. doi: 10.1016/S0277-9536(97)00193-7. [DOI] [PubMed] [Google Scholar]
- 3.Bertolote JM, Fleischmann A, Eddleston M, Gunnell D. Deaths from pesticide poisoning: a global response. Br J Psychiatry. 2006;189:201–3. doi: 10.1192/bjp.bp.105.020834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Provincial Health Bulletin – 2006 Anuradhapura: Provincial Department of Health Services; 2006.
- 5.Annual Heath Bulletin – 2003 Colombo: Ministry of Health, Sri Lanka; 2003.
- 6.Eddleston M, Gunnell D, Karunaratne A, de Silva D, Sheriff MHR, Buckley NA. Epidemiology of intentional self-poisoning in rural Sri Lanka. Br J Psychiatry. 2005;187:583–4. doi: 10.1192/bjp.187.6.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Senanayake N, Karalliedde L. Pattern of acute poisoning in a medical unit in central Sri Lanka. Forensic Sci Int. 1988;36:101–4. doi: 10.1016/0379-0738(88)90221-6. [DOI] [PubMed] [Google Scholar]
- 8.Eddleston M, Sudarshan K, Senthilkumaran M, Reginald K, Karalliedde L, Senarathna L, et al. Patterns of hospital transfer for self-poisoned patients in rural Sri Lanka: implications for estimating the incidence of self-poisoning in the developing world. Bull World Health Organ. 2006;84:276–82. doi: 10.2471/BLT.05.025379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dawson AH, Eddleston M, Senarathna L, Mohamed F, Gawarammana I, Bowe SJ, et al. Acute human lethal toxicity of agricultural pesticides: a prospective cohort study. PLoS Med. 2010;7:e1000357. doi: 10.1371/journal.pmed.1000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Statistics handbook of Anuradhapura district Colombo: Department of Census and Statistics of Sri Lanka; 2010. [Google Scholar]
- 11.Life tables for Sri Lanka and districts, 2000–2002. Colombo: Department of Census and Statistics of Sri Lanka; 2008.
- 12.Eddleston M, Udayakumara N, Adhikari S, de Silva D, Rezvi Sheriff MH, Waidyaratne DL. The importance of poisoning vs. road traffic injuries as a cause of death in rural Sri Lanka. PLoS ONE. 2007;2:e-599. doi: 10.1371/journal.pone.0000599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts DM, Karunarathna A, Buckley NA, Manuweera G, Sheriff MHR, Eddleston M. Influence of pesticide regulation on acute poisoning deaths in Sri Lanka. Bull World Health Organ. 2003;81:789–98. [PMC free article] [PubMed] [Google Scholar]
- 14.Annual health statistics, Sri Lanka 2007 Colombo: Ministry of Health, Sri Lanka; 2007. [Google Scholar]
- 15.Senarathna DLP. How the level of resources and hospital staff attitude in primary care hospitals in rural Sri Lanka affect poisoning patient outcome. [Minor thesis]. Newcastle: University of Newcastle; 2006. [Google Scholar]
- 16.Senarathna L, Adams J, De Silva D, Buckley NA, Dawson AH. Personal and professional challenges in the management of deliberate self-poisoning patients in rural Sri Lanka: a qualitative study of rural hospital doctors' experiences and perceptions. BMC Public Health. 2008;8:373. doi: 10.1186/1471-2458-8-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gawarammana IB, Ariyananda PL, Palangasinghe C, De Silva NGL, Fernando K, Vidanapathirana M, et al. Emerging epidemic of fatal human self-poisoning with a washing powder in Southern Sri Lanka: a prospective observational study. Clin Toxico (Phila) 2009;47:407–11. doi: 10.1080/15563650902915320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller M, Bhalla K. An urgent need to restrict access to pesticides based on human lethality. PLoS Med. 2010;7:e1000358. doi: 10.1371/journal.pmed.1000358. [DOI] [PMC free article] [PubMed] [Google Scholar]