Abstract
Objective
To assess the effect on out-of-pocket medical spending and physical and mental health of Japan’s reduction in health-care cost sharing from 30% to 10% when people turn 70 years of age.
Methods
Study data came from a 2007 nationally-representative cross-sectional survey of 10 293 adults aged 64 to 75 years. Physical health was assessed using a 16-point scale based on self-reported data on general health, mobility, self-care, activities of daily living and pain. Mental health was assessed using a 24-point scale based on the Kessler-6 instrument for nonspecific psychological distress. The effect of reduced cost sharing was estimated using a regression discontinuity design.
Findings
For adults aged 70 to 75 years whose income made them ineligible for reduced cost sharing, neither out-of-pocket spending nor health outcomes differed from the values expected on the basis of the trend observed in 64- to 69-year-olds. However, for eligible adults aged 70 to 75 years, out-of-pocket spending was significantly lower (P < 0.001) and mental health was significantly better (P < 0.001) than expected. These differences emerged abruptly at the age of 70 years. Moreover, the mental health benefits were similar in individuals who were and were not using health-care services (P = 0.502 for interaction). The improvement in physical health after the age of 70 years in adults eligible for reduced cost-sharing tended to be greater than in non-eligible adults (P = 0.084).
Conclusion
Reduced cost sharing was associated with lower out-of-pocket medical spending and improved mental health in older Japanese adults.
Résumé
Objectif
Évaluer l'incidence sur les dépenses médicales personnelles et la santé physique et mentale de la réduction de 30% à 10% du partage des coûts de soins de santé lorsque les individus atteignent 70 ans.
Méthodes
Les données de l'étude proviennent d'une enquête nationale transversale, effectuée en 2007, sur 10 293 adultes âgés de 64 à 75 ans. Leur santé physique a été évaluée au moyen d'une échelle de 16 points, basée sur des données autodéclarées de santé générale, de mobilité, de soins auto-administrés, d'activités de la vie quotidienne et de douleur. Leur santé mentale a été évaluée au moyen d'une échelle de 24 points sur la base de l'instrument Kessler-6 de détresse psychologique non spécifique. L'effet de la réduction du partage des coûts a été estimé en utilisant une approche de discontinuité de la régression.
Résultats
Pour les individus âgés de 70 à 75 ans inéligibles, en raison de leurs revenus, à une réduction du partage des coûts, ni les dépenses de santé personnelles ni les résultats sanitaires ne différaient des valeurs attendues, sur la base de la tendance observée chez les 64 à 69 ans. Toutefois, pour les individus âgés de 70 à 75 ans ayant droit à cette réduction, les dépenses personnelles étaient significativement plus faibles (P < 0,001) et leur santé mentale significativement meilleure (P < 0,001) que prévu. Ces différences sont apparues brutalement à l'âge de 70 ans. En outre, les avantages en termes de santé mentale étaient similaires chez les individus recourant ou non aux services de santé (P = 0,502 pour l'interaction). L'amélioration de la santé physique après l'âge de 70 ans chez les adultes éligibles à une réduction du partage des coûts avait tendance à être supérieure à celle des adultes inéligibles (P = 0,084).
Conclusion
La réduction du partage des coûts était associée à une baisse des dépenses médicales personnelles et à une amélioration de la santé mentale des personnes âgées japonaises.
Resumen
Objetivo
Evaluar el efecto de la reducción del 30% al 10% de la participación en los gastos de asistencia sanitaria sobre los gastos médicos directos y la salud física y mental en personas mayores de 70 años en Japón.
Métodos
Los datos de estudio se obtuvieron de una encuesta transversal representativa realizada a nivel nacional entre 10.293 adultos con edades comprendidas entre los 64 y los 75 años. La salud física se evaluó por medio de una escala de 16 puntos en función de los datos dados por los encuestados sobre salud general, movilidad, cuidados personales, actividades de la vida diaria y dolor. La salud mental se evaluó por medio de una escala de 24 puntos en función del instrumento Kessler-6 para la angustia psicológica no específica. El efecto de la participación reducida en los gastos se calculó utilizando un diseño de regresiones en discontinuidad.
Resultados
Entre los adultos con edades comprendidas entre los 70 y 75 años, cuyos ingresos no les permitían ser seleccionados para la participación reducida en los gastos, ni los gastos directos ni los costes sanitarios difirieron de los valores esperados en función de la tendencia observada entre los adultos con edades comprendidas entre los 64 y los 60 años. No obstante, los gastos directos fueron significativamente inferiores (P < 0,001) y la salud mental fue significativamente mejor (P < 0,001) de lo esperado entre los adultos elegibles con edades comprendidas entre los 70 y los 75 años. Estas diferencias surgieron de manera repentina a la edad de 70 años. Además, los beneficios sobre la salud mental fueron similares tanto en individuos que utilizaban los servicios de asistencia sanitaria como en aquellos que no lo hacían (P = 0,502 de interacción). La mejora en la salud física a partir de los 70 años en adultos elegibles para la participación reducida en los gastos mostró una tendencia superior que en los adultos no elegibles (P = 0,084).
Conclusión
La participación reducida en los gastos se asoció con la reducción de los gastos médicos directos y mejoró la salud mental de los adultos japoneses de mayor edad.
ملخص
الغرض
تقييم التأثير على الإنفاق الطبي من الأموال الخاصة والصحة البدنية والنفسية الناتج عن خفض اليابان لتقاسم تكاليف الرعاية الصحية من 30 % إلى 10 % عند بلوغ سن الفرد 70 عامًا.
الطريقة
تم استقاء بيانات الدراسة من استقصاء متعدد القطاعات ممثل للواقع على الصعيد الوطني تم إجراؤه في عام 2007 على عينة من 10293 بالغًا تتراوح أعمارهم من 64 إلى 75 عامًا. وخضعت الصحة البدنية للتقييم باستخدام مقياس من 16 نقطة استنادًا إلى البيانات التي يفصح عنها الأشخاص والمعنية بالصحة العمومية والتنقل والرعاية الذاتية وأنشطة المعيشة اليومية والألم. كما خضعت الصحة النفسية للتقييم باستخدام مقياس من 24 نقطة استنادًا إلى أداة كسلر-6 للضائقة النفسية غير المحددة. وتم تقييم تأثير خفض تقاسم التكاليف باستخدام تصميم انقطاع الارتداد.
النتائج
بالنسبة للبالغين الذين تتراوح أعمارهم من 70 إلى 75 عامًا الذين يحصلون على دخل يجعلهم غير مؤهلين لخفض تقاسم التكاليف، لم يختلف الإنفاق من الأموال الخاصة أو النتائج الصحية عن القيم المتوقعة على أساس الاتجاه الذي لوحظ في الأعمار التي تتراوح من 64 إلى 69 عامًا. إلا أنه بالنسبة للبالغين المؤهلين ممن تتراوح أعمارهم من 70 إلى 75 عامًا، كان الإنفاق من الأموال الخاصة أكثر انخفاضًا بشكل كبير (الاحتمالية > 0.001) وكانت الصحة النفسية أفضل بشكل كبير (الاحتمالية > 0.001) عن المتوقع. علاوة على ذلك، تشابهت فوائد الصحة النفسية لدى الأفراد الذين كانوا يستخدمون ولا يستخدمون خدمات الرعاية الصحية (الاحتمالية = 0.502 للتفاعل). ومال التحسن في الصحة البدنية بعد عمر 70 عامًا لدى البالغين المؤهلين لانخفاض تقاسم التكاليف إلى الزيادة عنه لدى البالغين غير المؤهلين (الاحتمالية = 0.084).
الاستنتاج
ارتبط انخفاض تقاسم التكاليف بانخفاض الإنفاق الطبي من الأموال الخاصة وتحسين الصحة النفسية لدى البالغين اليابانيين الأكبر سنًا.
摘要
目的
评估日本将达到 70 岁的人的医疗保健费用分担从 30 % 减至 10% 对现款医疗费用和身体及心理健康的影响。
方法
研究数据来自 2007 年对 10293 位 64 至 75 岁的成年人的全国代表性横断面调查。基于有关一般健康、活动性、自理、日常生活活动和病痛的自报数据,采用 16 分制评估身体健康状况。基于非特异性心理困扰的 Kessler-6 仪器,采用 24 分制评估心理健康状况。使用回归间断设计估计降低费用分担的影响。
结果
对于其收入水平使其无资格享受降低费用分担政策且年龄在 70 至 75 岁的成年人,无论是现款费用还是健康状况都不同于在基于 64 - 69 岁的人群中观察到的趋势期望值。然而,对于享有资格的 70 至 75 岁的成年人,现款费用显著低于预期(P < 0.001),心理健康状况显著好于预期(P < 0.001)。这些差异突现在 70 岁的人群中。此外,在使用和不使用医疗保健服务的个人当中,心理健康状态的益处相似(交互作用 P = 0.502)。有资格享受降低费用共享政策的 70 岁之后的成年人的身体健康的改善程度有大于无资格的成年人的趋势(P = 0.084)。
结论
降低费用分担与更少的现款医疗费用和更好的日本老年人的心理健康存在关联。
Резюме
Цель
Оценить, как сокращение участия пациентов, достигших 70-летнего возраста, в покрытии затрат на медицинское обслуживание в Японии с 30% до 10% влияет на суммы, выплачиваемые за медицинские услуги, а также на физическое и психическое здоровье.
Методы
Данные для исследования получены из проведенного в 2007 г. национально-репрезентативного перекрестного анкетирования 10293 взрослых пациентов в возрасте от 64 до 75 лет. Состояние физического здоровья оценивалось при помощи теста из 16 пунктов на основании данных, предоставленных участниками, о состоянии здоровья в целом, подвижности, уходе за собой, ежедневной деятельности и болевых ощущениях. Состояние психического здоровья определялось с помощью теста из 24 пунктов, основанного на методе оценки неспецифических психических расстройств Kessler-6. Влияние сокращения участия пациентов в покрытии затрат оценивалось с использованием модели разрывной регрессии.
Результаты
Для взрослых пациентов в возрасте от 70 до 75 лет, чей доход лишал их права на сокращение участия в покрытии затрат, ни оплачиваемые пациентами расходы, ни состояние их здоровья не отличались от значений, полученных на основании тенденций, которые наблюдалась у 64-69-летних. Однако для имеющих такое право взрослых пацентов в возрасте от 70 до 75 лет оплачиваемые пациентами расходы на медицинское обслуживание были значительно ниже (P < 0,001), а психическое здоровье значительно лучше (P < 0,001) ожидаемых. Данные различия начинали резко проявляться в возрасте 70 лет. Более того, польза для психического здоровья пользовавшихся и не пользовавшихся медицинским обслуживанием лиц была сходной (P = 0,502 для взаимосвязи). Улучшение физического здоровья у взрослых старше 70 лет, имеющих право на сокращение участия в покрытии затрат, было более заметным чем у тех, кто такого права не имел (P = 0,084).
Вывод
Сокращение участия в покрытии затрат продемонстрировало уменьшение оплачиваемых пацинтом расходов на медицинское обслуживание, а также лучшее психическое здоровье у японцев пожилого возраста.
Introduction
Asking patients to share the cost of health care is a measure frequently used to reduce demand and control the health-care budget.1–5 Moreover, patient cost sharing can also help finance universal health-care systems by raising additional revenue.6 However, there is still some debate about the level of cost sharing that is best able to control costs while ensuring access to health care, preventing impoverishment from out-of-pocket spending and avoiding adverse health effects.7,8 Several studies have quantified the effects of health insurance coverage and cost sharing on the use of important health services, but few have investigated their influence on health outcomes.9–14 Most studies were conducted in the United States of America, where universal insurance coverage has not been achieved.9,11,12,15–20 The extent to which health outcomes are influenced by cost sharing under national health insurance programmes in other countries is unclear. In this study, we assessed how health outcomes in elderly adults were affected by a change in cost sharing under the universal national health insurance programme in Japan.
Japanese national health insurance provides universal coverage for inpatient, outpatient, dental and pharmaceutical services. There is a fixed cost-sharing rate that varies with age and a general upper limit on monthly out-of-pocket spending for all age groups.21 In 2007, the proportion of Japan’s total national health expenditure that was publicly financed through a tax transfer and social health insurance programme was 81.9%, which ranks among the highest rates for countries in the Organisation for Economic Co-operation and Development’s Asia–Pacific region.22,23 The remainder is private spending by households, which comprises out-of-pocket medical spending for services that may or may not be covered (e.g. non-prescribed over-the-counter medications) by the universal programme.22
Although the exact proportion of patient cost sharing under the public insurance scheme is fixed across services, the level varies by age and income. In particular, in 2001 the Japanese government introduced a system of two different cost-sharing rates: 30% for adults aged less than 70 years and 10% for those aged 70 years or older who had a relatively low income. The rate remained 30% for older individuals with a sufficiently high income.24 We took advantage of this natural experiment to investigate the effect of the change in patient cost sharing at the age of 70 years on physical and mental health.
Methods
Study population
We obtained data from the 2007 Comprehensive Survey of People's Living Conditions – a nationally-representative, cross-sectional survey administered by the Japanese Ministry of Health, Labour and Welfare.25 In total, 2000 sampling units were randomly selected from all 47 prefectures in Japan. All individuals and households in each unit were asked to complete a self-administered questionnaire in July 2007. We restricted our study population to 10 906 individuals aged between 64 and 75 years (i.e. 70 ± 6 years). We excluded individuals who were hospitalized or institutionalized (n = 408) and those who were eligible for free health care (n = 205). For the remaining 10 293, we performed multiple imputation to address potential bias due to missing data (e.g. data on general health status were missing for 13.3%).
Since 2001, the cost-sharing rate is normally reduced from 30% to 10% in the first month after people turn 70 years of age, provided their annual taxable income is below 12 000 United States dollars (US$), which was equivalent to 1.45 million Japanese yen in July 2007.24 Overall, 83.3% of the study population was eligible for the reduction in 2007.
Study variables
We analysed three dependent variables: out-of-pocket medical spending, physical health and mental health. Out-of-pocket spending included all expenditure on medical services in the month preceding the survey. We used a 16-point summary physical health measure developed for the Comprehensive Survey of People’s Living Conditions.26,27 A summary physical health score was derived for each individual from answers to questions on general health status, mobility, self-care and activities of daily living, and pain, as described in a footnote to Table 1. Mental health status was assessed using a Japanese version of the Kessler-6 24-point scale, which has been validated as a strong predictor of mental disorders, excluding substance use disorder, that can be identified using the Structured Clinical Interview of the Diagnostic and statistical manual of mental disorders, fourth edition and that have a Global Assessment of Functioning score less than 60.28–31 We reversed the original Kessler-6 scale such that 24 was the best score and 0, the worst.
Table 1. Demographic characteristics, medical spending and health status of older adults, 2007 Comprehensive Survey of People’s Living Conditions, Japan.
| Characteristic | Eligiblea for reduced cost sharing at 70 years of age |
Not eligiblea for reduced cost sharing at 70 years of age |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aged 64–69 n = 3 837c |
Aged 70–75 n = 3 769c |
Pb | Aged 64–69 n = 966c |
Aged 70–75 n = 554c |
Pb | ||||||
| Gender | 0.147 | 0.349 | |||||||||
| Male, % | 40.9 | 42.6 | 85.5 | 83.6 | |||||||
| Female, % | 59.1 | 57.4 | 14.5 | 16.4 | |||||||
| Marital status | < 0.001 | 0.005 | |||||||||
| Married, % | 80.7 | 74.9 | 89.1 | 85.0 | |||||||
| Unmarried, % | 2.9 | 2.2 | 1.9 | 3.1 | |||||||
| Widowed, % | 11.9 | 19.3 | 6.0 | 10.1 | |||||||
| Divorced, % | 4.4 | 3.6 | 3.0 | 1.8 | |||||||
| Household size | 0.608 | 0.055 | |||||||||
| Mean, no. of persons | 2.72 | 2.73 | 2.72 | 2.59 | |||||||
| Standard error, no. of persons | 0.023 | 0.026 | 0.042 | 0.059 | |||||||
| Occupational status | < 0.001 | < 0.001 | |||||||||
| Not working, % | 12.9 | 74.5 | 35.6 | 59.0 | |||||||
| Working, % | 86.3 | 25.5 | 64.4 | 41.0 | |||||||
| House ownership | 0.039 | 0.379 | |||||||||
| No, % | 13.7 | 12.1 | 5.9 | 4.7 | |||||||
| Yes, % | 86.3 | 87.9 | 94.1 | 95.3 | |||||||
| Settlement sized | 0.004 | 0.919 | |||||||||
| Metropolitan area, % | 15.9 | 14.1 | 19.6 | 21.1 | |||||||
| Large city (population: > 150 000), % | 26.8 | 25.6 | 30.4 | 31.2 | |||||||
| Medium city (population: 50 000–150 000), % | 27.9 | 28.3 | 27.2 | 26.4 | |||||||
| Small city (population: < 50 000), % | 14.7 | 14.4 | 10.2 | 9.6 | |||||||
| Town or village, % | 14.6 | 17.5 | 12.5 | 11.7 | |||||||
| Reported health-care usee | < 0.001 | < 0.001 | |||||||||
| No, % | 39.2 | 28.6 | 39.1 | 27.8 | |||||||
| Yes, % | 60.8 | 71.4 | 60.9 | 72.2 | |||||||
| Out-of-pocket medical spendingf | < 0.001 | 0.259 | |||||||||
| Mean, US$ | 47.6 | 35.7 | 49.7 | 44.8 | |||||||
| Standard error, US$ | 1.41 | 1.15 | 2.66 | 3.48 | |||||||
| Physical healthg | < 0.001 | < 0.001 | |||||||||
| Mean score | 13.4 | 13.0 | 13.8 | 13.3 | |||||||
| Standard error | 0.044 | 0.053 | 0.063 | 0.106 | |||||||
| Mental healthh | 0.397 | 0.300 | |||||||||
| Mean score | 20.9 | 21.0 | 21.6 | 21.8 | |||||||
| Standard error | 0.077 | 0.083 | 0.117 | 0.147 | |||||||
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for individuals who had an annual taxable income under 12 000 United States dollars (US$).
b χ2 tests were used to compare distributions of categorical variables and t tests were used for continuous variables.
c Because values were missing for some variables, the sample sizes for each two-by-two table were smaller than these numbers. Moreover, the total number of individuals was 9126, which is smaller than the number of the study participants (n = 10 293) because data on income eligibility were missing.
d The size of the settlement where the individual lived at the time of the Comprehensive Survey of People’s Living Conditions.
e Health-care use reported at the time of the Comprehensive Survey of People’s Living Conditions.
f Spending in Japanese yen was converted into US$ using the rate that applied in July 2007 of approximately 120 Japanese yen per US$.
g Physical health status was evaluated on a scale of 0 to 16 points and was calculated from the sum of four questionnaire health measures: (i) general health status was assessed by asking, “How is your current health status?” (4 if excellent, 3 if very good, 2 if good, 1 if fair and 0 if poor); (ii) mobility was assessed by asking, “How many days have you been in bed (i.e. bed-ridden) because of health-related problems in the previous one month?” (4 if never, 3 if 1 to 3 days, 2 if 4 to 6 days, 1 if 7 to 14 days and 0 if 15 days or more); (iii) self-care and activities of daily living were assessed by asking, “Do you have difficulty with any of the following four areas in your daily life due to your physical health?: daily movements (e.g. getting up, wearing clothes, eating and bathing); staying outdoors; work, housework or studying; and, exercise or sport” (4 if no difficulties, 3 if difficulty in one area, 2 if difficulty in two areas, 1 if difficulty in three areas and 0 if difficulty in all four areas); (iv) pain was assessed by asking, “Do you have pain in the head, stomach, back or extremities?” (4 if no pain, 3 if pain in one location, 2 if pain in two locations, 1 if pain in three locations and 0 if pain in all four locations).
h Mental health status was evaluated on a scale of 0 to 24 points using a reversed version of Japanese Kessler-6 scale, such that 24 was best.
For modelling purposes, we created a dichotomous indicator, designated age ≥ 70dummy: the indicator equalled 1 if the participant was 70 years of age or older and 0 otherwise. A second dichotomous indicator, designated income eligibility, equalled 1 if the participant was eligible for the lower cost-sharing rate because of his or her taxable income, and 0 otherwise.
To adjust for potential confounders, we considered the following covariates in the regression models: gender, marital status, household size, occupational status, house ownership and the size of the settlement where the individual lived. In addition, we carried out separate analyses for participants who did and those who did not report health-care use under the public insurance programme at the time of the survey for at least one chronic illness that had been diagnosed at a clinic or hospital.
Statistical analysis
The effect of the reduction in the cost-sharing rate at the age of 70 years on out-of-pocket medical spending, physical health and mental health was quantified by estimating the discontinuity in the age trend of these outcomes using a regression discontinuity design.17,32 We assumed that out-of-pocket spending and physical and mental health scores would vary smoothly with age in the absence of the rate reduction and attributed any abrupt deviation in the age trend at the age of 70 years to that reduction. Deviations were quantified, first, by estimating the difference between the value of a variable for individuals aged 69 years and 11 months and the value for those in the first month of their 70th year and, second, by determining how much of that difference could not be explained by the trend observed from the age range of 64 to 69 years to the age range of 70 to 74 years.
We fitted the following unadjusted linear model for the three study outcomes:
| (1) |
where E(Y) is the expected value of the dependent variable, age is given in years and age ≥ 70dummy is as described above. Thus, β3 provides a measure of the discontinuity in E(Y) around the age of 70 years and can be interpreted as the effect of the cost-sharing rate reduction. To determine whether the effect observed varied by eligibility for the rate reduction, we fitted separate models for non-eligible and eligible adults.
In secondary analyses, we fitted joint models with interaction terms that compared discontinuities between non-eligible and eligible adults and derived differential discontinuities for eligible adults. These differential discontinuities provided more robust estimates of the effects of cost sharing by controlling for changes in the health of non-eligible adults between the ages of 69 and 70 years. However, our study sample had limited statistical power for estimating these differential effects. In addition, to determine how health-care needs affected outcomes in eligible adults, we fitted separate and joint models for eligible adults who were or were not receiving health care at the time of the survey.
To check a key assumption of the regression discontinuity design, we confirmed that important characteristics of the study participants did not change around the age of 70 years.17,32 Specifically, we used the models described above to look for age discontinuities in sociodemographic factors among eligible adults, such as gender, marital status, household size, occupational status, house ownership, taxable income and the size of the settlement where the individual lived. All P-values for these factors were found to be greater than 0.25, which confirms that the characteristics did not abruptly change at the age of 70 years.
Furthermore, we adjusted the above models for these sociodemographic characteristics and used multiple imputation to address bias that could have been introduced by missing data on outcome variables and covariates, as explained in a footnote to Table 2.33 Therefore, our main results were adjusted for sociodemographic characteristics and multiple imputation.
Table 2. Effect of reduced cost sharing at age 70 yearsa on out-of-pocket medical spending and physical and mental health,b Japan, 2007.
| Characteristic | nc | Unadjusted modeld |
Adjusted modele |
Multiple imputation modelf |
Joint model with interaction after imputationg |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β3 | SE | P | β3 | SE | P | β3 | SE | P | δ6 | SE | P | |||||||||||||
| Out-of-pocket medical spending | n | US$ per monthh | US$ per monthh | US$ per monthh | US$ per monthh | US$ per monthh | US$ per monthh | US$ per monthh | US$ per monthh | |||||||||||||||
| Non-eligiblea adults | 1790 | −3.54 | 8.48 | 0.676 | −4.10 | 8.69 | 0.637 | −3.16 | 8.08 | 0.696 | −21.79 | 8.79 | 0.014 | |||||||||||
| Eligible adultsa | 8503 | −24.93 | 3.61 | < 0.001 | −24.92 | 3.94 | < 0.001 | −25.25 | 3.59 | < 0.001 | ||||||||||||||
| Eligible adultsa with no reported health-care usei | 2968 | −3.40 | 4.19 | 0.417 | −3.73 | 4.27 | 0.382 | −4.19 | 4.58 | 0.361 | −27.68 | 6.43 | < 0.001 | |||||||||||
| Eligible adultsa with reported health-care usei | 5535 | −32.72 | 5.29 | < 0.001 | −32.76 | 5.37 | < 0.001 | −32.44 | 4.61 | < 0.001 | ||||||||||||||
| Physical healthj | n | Score | Score | Score | Score | Score | Score | Score | Score | |||||||||||||||
| Non-eligiblea adults | 1790 | −0.31 | 0.24 | 0.202 | −0.24 | 0.24 | 0.326 | −0.17 | 0.15 | 0.247 | 0.27 | 0.16 | 0.084 | |||||||||||
| Eligible adultsa | 8503 | 0.12 | 0.13 | 0.381 | 0.08 | 0.13 | 0.106 | 0.10 | 0.07 | 0.143 | ||||||||||||||
| Eligible adultsa with no reported health-care usei | 2968 | 0.19 | 0.14 | 0.173 | 0.19 | 0.15 | 0.202 | 0.14 | 0.09 | 0.115 | −0.11 | 0.13 | 0.419 | |||||||||||
| Eligible adultsa with reported health-care usei | 5535 | −0.02 | 0.17 | 0.892 | −0.04 | 0.18 | 0.799 | 0.02 | 0.09 | 0.857 | ||||||||||||||
| Mental healthk | n | Score | Score | Score | Score | Score | Score | Score | Score | |||||||||||||||
| Non-eligiblea adults | 1790 | −0.05 | 0.39 | 0.888 | 0.06 | 0.39 | 0.873 | 0.03 | 0.38 | 0.932 | 0.70 | 0.41 | 0.086 | |||||||||||
| Eligible adultsa | 8503 | 0.58 | 0.20 | 0.004 | 0.56 | 0.20 | 0.007 | 0.66 | 0.18 | < 0.001 | ||||||||||||||
| Eligible adultsa with no reported health-care usei | 2968 | 0.63 | 0.32 | 0.048 | 0.64 | 0.32 | 0.045 | 0.79 | 0.32 | 0.017 | −0.29 | 0.42 | 0.502 | |||||||||||
| Eligible adultsa with reported health-care usei | 5535 | 0.43 | 0.27 | 0.111 | 0.39 | 0.28 | 0.156 | 0.50 | 0.23 | 0.032 | ||||||||||||||
SE, standard error; US$, United States dollars.
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for individuals who had an annual taxable income under 12 000 United States dollars (US$).
b The effect of reduced cost sharing was evaluated using a regression discontinuity design and a generalized estimating equation method.
c The sample sizes include individuals with missing values, all of whom were included in the imputation model.
d We calculated β coefficients for the model: E(Y) = β0 + β1(age) + β2(age)2 + β3(age ≥ 70 dummy), where E(Y) is the expected value of the dependent variable, namely out-of-pocket medical spending, physical health or mental health, age is given in years and age ≥ 70dummy is a dichotomous indicator that equalled 1 if the participant was 70 years or older and 0 otherwise. No other control variables were used in the unadjusted model.
e The adjusted model included the control variables: gender, marital status, household size, occupational status, house ownership and the size of the settlement where the individual lived at the time of the Comprehensive Survey of People’s Living Conditions. Income was not included as it was used to determine whether an individual was eligible for reduced cost sharing. However, including income in the models did not substantially change the results.
f For multiple imputation, we used all the variables described in the methods section and an importance-resampling expectation-maximization algorithm with the assumption that values were missing at random. Five data sets generated from the multiple imputation were mobilized and pooled for point estimation. The same control variables included in the adjusted model were used in the multiple imputation and subsequent regression analyses. Since missing values were estimated and filled in, the standard errors in the imputation model should smaller than those in unadjusted or adjusted model.
g We calculated δ coefficients for the model: E(Y) = δ1(age) + δ2(age)2 + δ3(age ≥ 70dummy) + δ4(age) × (income eligibility or reported health-care use) + δ5(age)2 × (income eligibility or reported health-care use) + δ6(age ≥ 70dummy) × (income eligibility or reported health-care use) + Σδ(control variables), where E(Y) is the expected value of the dependent variable, namely out-of-pocket medical spending, physical health or mental health, age is given in years and age ≥ 70dummy is a dichotomous indicator that equalled 1 if the participant was 70 years or older and 0 otherwise. Coefficients were calculated between adults who were or were not eligible for reduced cost sharing and between eligible adults who did or did not report health-care use at the time of the survey. The main effect was measured by δ6.
h Spending in Japanese yen was converted into US$ using the rate that applied in July 2007 of approximately 120 Japanese yen per US$.
i Health-care use reported at the time of the Comprehensive Survey of People’s Living Conditions.
j Physical health status was evaluated on a scale of 0 to 16 points and was calculated as described in a footnote to Table 1
k Mental health status was evaluated on a scale of 0 to 24 points using a reversed version of Japanese Kessler-6 scale, such that 24 was best.
To understand the clinical significance of the average change in mental health status associated with reduced cost sharing, we used logistic regression to estimate the associated change in the prevalence of mild mental illness. We used a validated threshold for the diagnosis of mental illness (i.e. any mood or anxiety disorder in the Diagnostic and statistical manual of mental disorders, fourth edition) in Japan: a score of 19 or less on our reversed Kessler-6 scale.30
We carried out several sensitivity analyses. First, we progressively narrowed the age cohort to individuals aged between 67 and 72 years and then to those between 69 and 70 years. Second, we estimated discontinuities across 11 different dichotomous indicators for age thresholds ranging from 65 to 75 years. We used generalized estimating equations to account for correlated observations within households when estimating standard errors and conducting two-sided tests.34,35 Analyses were performed using Stata version 12.0 (StataCorp. LP, College Station, USA) and R version 2.13.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
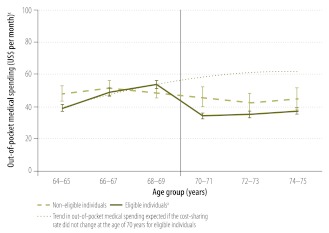
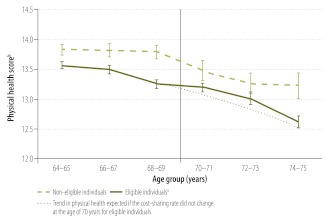
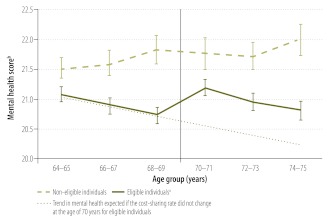
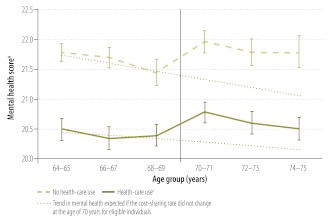
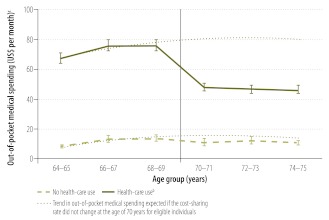
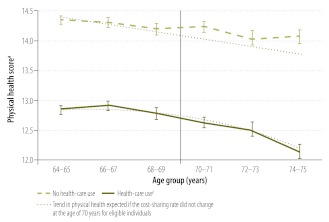
Significant differences in sociodemographic characteristics and health-care needs were found between participants aged from 64 to 69 years and those aged from 70 to 75 years (Table 1). Table 2 shows that adjustment for sociodemographic covariates and multiple imputation to address bias due to missing data did not substantially alter the results of the analysis. Although out-of-pocket medical spending by adults who were not eligible for lower cost sharing did not change significantly at the age of 70 years (β3 = −3.16 US$/month; P = 0.696; Table 2, multiple imputation model), spending by eligible adults decreased significantly and abruptly (β3 = −25.25 US$/month; P < 0.001), as shown in Fig. 1. There was no significant discontinuity in physical health score at the age of 70 years in either group (Fig. 2, available at: http://www.who.int/bulletin/volumes/90/6/11-095380, and Table 2). However, the differential discontinuity in physical health score for eligible adults (δ6 = +0.27; P = 0.084, joint model with interaction after imputation) showed a relative improvement that approached statistical significance (Table 2). On the other hand, there was a significant improvement in mental health status in the eligible group at the age of 70 years (β3 = 0.66; P < 0.001; Table 2, multiple imputation model) but not in the non-eligible group (β3 = 0.03; P = 0.932), as shown in Fig. 3. This improvement was significant even among participants who reported no health-care use at the time of the survey (β3 = 0.79; P = 0.017), as shown in Fig. 4.
Fig. 1.
Effect of reduced cost sharing at age 70 yearsa on out-of-pocket medical spending,b Japan, 2007
US$, United States dollars.
The vertical bars represent standard errors.
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
b Out-of-pocket medical spending includes expenditure both on items covered by public health-care insurance and items that are not covered, such as over-the-counter medicines.
c Spending in Japanese yen was converted into US$ using the rate that applied in July 2007 of approximately 120 Japanese yen per US$.
Fig. 2.
Effect of reduced cost sharing at age 70 yearsa on physical health,b Japan, 2007
The vertical bars represent standard errors.
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
b Physical health status was evaluated on a scale of 0 to 16 points and was calculated as described in a footnote to Table 1.
Fig. 3.
Effect of reduced cost sharing at age 70 yearsa on mental health,b Japan, 2007
The vertical bars represent standard errors.
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
b Mental health was evaluated on a scale of 0 to 24 points using a reversed version of Japanese Kessler-6 scale, such that 24 was best.
Fig. 4.
Effect of reduced cost sharing at age 70 years on the mental healtha of eligible individualsb using and not using health-care,c Japan, 2007
The vertical bars represent standard errors.
a Mental health was evaluated on a scale of 0 to 24 points using a reversed version of Japanese Kessler-6 scale, such that 24 was best.
b The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
c Health-care use reported at the time of the 2007 Comprehensive Survey of People’s Living Conditions.
When eligible participants were divided into two subgroups with different health-care needs, the decrease in out-of-pocket spending at the age of 70 years was found to be greater among adults who reported health-care use at the time of the survey than in those who did not (P < 0.001 for interaction, Table 2), as shown in Fig. 5. In contrast, the effect of reduced cost sharing on mental health status was similar in the two subgroups (P = 0.502 for interaction), as was the effect on physical health status (P = 0.419 for interaction), as shown in Fig. 6 (available at: http://www.who.int/bulletin/volumes/90/6/11-095380).
Fig. 5.
Effect of reduced cost sharing at age 70 years on out-of-pocket medical spending of eligible individualsa using and not using health-care,b Japan, 2007
US$, United States dollars.
The vertical bars represent standard errors.
a The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
b Health-care use reported at the time of the 2007 Comprehensive Survey of People’s Living Conditions.
c Spending in Japanese yen was converted into US$ using the rate that applied in July 2007 of approximately 120 Japanese yen per US$.
Fig. 6.
Effect of reduced cost sharing at age 70 years on the physical healtha of eligible individualsb using and not using health-care,c Japan, 2007
The vertical bars represent standard errors.
a Physical health status was evaluated on a scale of 0 to 16 points and was calculated as described in a footnote to Table 1.
b The cost-sharing rate decreased from 30% to 10% at the age of 70 years for eligible individuals, who had an annual taxable income under 12 000 United States dollars (US$).
c Health-care use reported at the time of the 2007 Comprehensive Survey of People’s Living Conditions.
Logistic regression analysis showed that the prevalence of mild mental illness decreased significantly at the age of 70 years among eligible participants (odds ratio, OR: 0.718; P = 0.009), but not among non-eligible participants (OR: 0.984; P = 0.960). When we incrementally narrowed the age range of participants included in the analysis from the initial 64 to 75 years, the estimated effect of reduced cost sharing on mental health became progressively larger: β3 was 0.66 (P < 0.001) for the age range 64 to 75 years, 0.69 (P = 0.022) for the range from 67 to 72 years and 1.19 (P = 0.047) for the range from 69 to 70 years. Finally, of the 11 dichotomous indicators for the different age thresholds investigated, only that for a threshold of 70 years was associated with a significant discontinuity in mental health scores.
Discussion
In this nationally representative study, we found that a reduction in health-care cost sharing from 30% to 10% at the age of 70 years was associated with a significant decrease in out-of-pocket medical spending and a significant improvement in mental health in Japanese adults. There was also a relative improvement in physical health in those eligible for the reduction by comparison with those who were not eligible, but it was not significant. Nevertheless, the relative improvement in physical health was similar to that observed in a larger longitudinal study,18 which suggests that our study was not adequately powered to detect this effect. Furthermore, the sharp regression discontinuity design captured only the immediate effect of the cost sharing reduction and may have missed improvements that become manifest over time.
Our findings are largely consistent with previous studies of the effect that providing Medicare coverage in the United States after the age of 65 years has on health-care utilization and health outcomes: coverage was associated with an abrupt increase in health-care utilization and improvements in physical and mental health, mortality and disparities in disease control.9,14–19 In addition, higher cost sharing among insured adults has been linked to less use of clinical services and adverse effects on health outcomes.8,9,14–20,36
Our findings on out-of-pocket medical spending are consistent with the results of the RAND Health Insurance Experiment,12 which reported that reduced cost sharing substantially increased both total health-care utilization and total health-care spending. Although we could not measure total health-care spending directly, we were able to estimate it in the following way. Data from a separate nationally representative survey indicate that out-of-pocket spending on services included in Japan’s universal insurance coverage programme constitutes 70% of all out-of-pocket medical spending by elderly Japanese adults whose health care is covered by the programme, while spending on services that are not covered (e.g. over-the-counter medications) accounts for the remaining 30%.37 If total health-care spending is unchanged by reduced cost sharing, out-of-pocket spending by eligible adults should decrease to one third (i.e. from 30% to 10%). However, the observed value of out-of-pocket medical spending by eligible adults aged between 70 and 71 years was 29% higher than expected, which suggests that both total health-care spending and utilization had increased substantially and that this may have influenced mental and physical health.
The mental health gains we observed suggest that reduced cost sharing helped alleviate depression and anxiety, which are known to be the largest contributors to disability globally.38 Surprisingly, the improvement in mental health was even observed in individuals who were not using health-care services, which suggests that reduced cost sharing may have affected mental health in several ways. Individuals may have benefited from increased use of health-care services or from the greater sense of security provided by more affordable insurance coverage.
Policy implications
One topic for debate is whether, from a societal or governmental perspective, the gain in mental health linked to reduced cost sharing is worth the associated increase in health-care spending.39–41 Fostering a sense of security is one of the core functions of universal health insurance coverage and our findings suggest that the Japanese government has ameliorated the burden of mental illness among the elderly by reducing their cost-sharing rate.2,42,43 However, because of fiscal constraints, in April 2008 the Japanese government decided to raise the cost-sharing rate from 10% to 20% after the age of 70 years, perhaps in 2012 or 2013.24,44 This decision is likely to become a major issue in the next national election. Closer follow-up of the effect of this policy change on population health and medical expenditure would provide the information policy-makers in medium- to high-income countries need to design a system of universal health insurance coverage that incorporates the optimum cost-sharing rate for elderly populations.
Limitations
A lack of survey data on chronic conditions prevented us from being able to identify individuals with treatable chronic conditions, such as cardiovascular disease and diabetes, whose health status may have been particularly affected by reduced cost sharing.14,15,18
In addition, because our study used a cross-sectional rather than a longitudinal design, the results may have been affected by selection bias. For example, in general, individuals who were not using health care between the ages of 64 and 69 years were more likely to use health care after the age of 70 years following the cost sharing reduction.12 However, those who did not start using health care after the age of 70 years were likely to be healthier than those who did. The effect would be an abrupt change in the composition of cross-sectional comparison group samples, which would probably lead to an underestimate of the mental and physical health benefits for the group using health care and an overestimate of the benefits for those not using health care. Thus, although strong conclusions can be drawn from our analysis about changes in mental health for the entire study sample, the results obtained by stratifying participants by use of health care should be interpreted with caution.
Finally, the fact that our study did not have a randomized experimental design makes it impossible to infer a cause and effect relationship when interpreting the findings. In particular, because eligibility for the cost-sharing reduction was determined by income, it was not possible to match the income distribution in eligible and non-eligible groups. Nevertheless, we used a strong regression discontinuity design to control for all observed and unobserved characteristics that trended smoothly with age in our study sample.32,45,46 Furthermore, our analysis included difference-in-difference comparisons that adjusted the effect of cost sharing on eligible adults for changes in physical and mental health observed in the non-eligible, or control, group.
In summary, a reduction in health-care cost sharing at the age of 70 years was associated with lower out-of-pocket medical spending and improved mental health in Japanese adults. This finding suggests that governments in medium- and high-income countries with universal health insurance coverage can reduce the burden of depression and anxiety by modifying cost sharing. The proposed increase in patient cost sharing currently under consideration by the Japanese government deserves close scrutiny because it may have an adverse effect on the mental, and possibly physical, health of older adults.
Acknowledegments
Akihiro Nishi is supported by the Nakajima Foundation. We thank Gary King at Harvard University, John Z Ayanian and Sae Takada at Harvard Medical School and Keiko Sakurai at the University of Tokyo.
Funding:
We were funded by the Japanese Ministry of Health, Labour and Welfare (H22-Policy-033), the Bill & Melinda Gates Foundation, the China Medical Board, the Beeson Career Development Award Program (NIA K08 AG038354) and the American Federation for Aging Research.
Competing interests:
None declared.
References
- 1.Newhouse JP. Medical care costs: how much welfare loss? J Econ Perspect. 1992;6:3–21. doi: 10.1257/jep.6.3.3. [DOI] [PubMed] [Google Scholar]
- 2.Resolution WHA58.33. Sustainable health financing, universal coverage and social health insurance. In: Fifty-eighth World Health Assembly, Geneva, 16–25 May 2005. Volume 1: Resolutions and decisions, and list of participants Geneva: World Health Organization; 2005 (WHA58/2005/REC/1). Available from: http://apps.who.int/gb/or/e/e_wha58r1.html [accessed 23 February 2012].
- 3.Social health protection: an ILO strategy towards universal access to health care Geneva: International Labour Organization; 2008. [Google Scholar]
- 4.Garrett L, Chowdhury AMR, Pablos-Méndez A. All for universal health coverage. Lancet. 2009;374:1294–9. doi: 10.1016/S0140-6736(09)61503-8. [DOI] [PubMed] [Google Scholar]
- 5.Hsiao WC. Why is a systemic view of health financing necessary? Health Aff (Millwood) 2007;26:950–61. doi: 10.1377/hlthaff.26.4.950. [DOI] [PubMed] [Google Scholar]
- 6.Akin J, Birdsall N, de Ferranti D. Financing health services in developing countries: an agenda for reform Washington: World Bank; 1987. [Google Scholar]
- 7.Yates R. Universal health care and the removal of user fees. Lancet. 2009;373:2078–81. doi: 10.1016/S0140-6736(09)60258-0. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358:375–83. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 9.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443–94. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masuhara H.Roujin Hoken Seido to Gairai Jushin [Health care system for older people and their physician visit] Kikan Shakai Hosho Kenkyu 200440266–76.Japanese [Google Scholar]
- 11.Levy H, Meltzer D. The Impact of health insurance on health. Annu Rev Public Health. 2008;29:399–409. doi: 10.1146/annurev.publhealth.28.021406.144042. [DOI] [PubMed] [Google Scholar]
- 12.Newhouse JP, Rand Corporation Insurance Experiment Group. Free for all?: lessons from the Rand Health Insurance Experiment Cambridge: Harvard University Press; 1993. [Google Scholar]
- 13.Lostao L, Regidor E, Geyer S, Aïach P. Patient cost sharing and social inequalities in access to health care in three western European countries. Soc Sci Med. 2007;65:367–76. doi: 10.1016/j.socscimed.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 14.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med. 2009;150:505–15. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 15.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Medicare spending for previously uninsured adults. Ann Intern Med. 2009;151:757–66. doi: 10.7326/0003-4819-151-11-200912010-00149. [DOI] [PubMed] [Google Scholar]
- 16.McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Impact of Medicare coverage on basic clinical services for previously uninsured adults. JAMA. 2003;290:757–64. doi: 10.1001/jama.290.6.757. [DOI] [PubMed] [Google Scholar]
- 17.Card D, Dobkin C, Maestas N. Does Medicare save lives? Q J Econ. 2009;124:597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McWilliams JM, Meara E, Zaslavsky A, Ayanian J. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298:2886. doi: 10.1001/jama.298.24.2886. [DOI] [PubMed] [Google Scholar]
- 19.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357:143–53. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 20.Decker SL, Rapaport C. Medicare and inequalities in health outcomes: the case of breast cancer. Contemp Econ Policy. 2002;20:1–11. doi: 10.1093/cep/20.1.1. [DOI] [Google Scholar]
- 21.Fukawa T. Public health insurance in Japan Washington: World Bank Institute; 2002. [Google Scholar]
- 22.OECD health data 2010: statistics and indicators. Paris: Organisation for Economic Co-operation and Development; 2010. [Google Scholar]
- 23.Wagstaff A. Health systems in East Asia: What can developing countries learn from Japan and the Asian Tigers? Washington: World Bank; 2005 (World Bank Policy Research Working Paper 3790). [DOI] [PubMed]
- 24.70 saidai zenhan no hihokensha nado ni kakaru ichibu hutan kin nado no keigen tokurei sochi jisshi youkou” no ichibu kaisei ni tsuite [Notice on the partial amendment of the implementation guidance of the special procedure of lowering the out-of-pocket expenditure among insured people aged 70-74]. Tokyo: Ministry of Health, Labour, and Welfare; 2010. Available from: http://wwwhourei.mhlw.go.jp/cgi-bin/t_docframe.cgi?MODE=tsuchi&DMODE=CONTENTS&SMODE=NORMAL&KEYWORD=&EFSNO=15154 [accessed 12 January 2012]. Japanese.
- 25.Kokumin seikatsu kiso chosa [Comprehensive survey of the living conditions of people on health and welfare] Tokyo: Ministry of Health, Labour, and Welfare; 2007. Japanese. [Google Scholar]
- 26.Noguchi H.Shakai keizai teki youin to kenko tono ingasei ni taisuru kousaru [Causal inference between socio-economic factors and health]. Quart Soc Security Res 2011466Japanese [Google Scholar]
- 27.Nishi A, Noguchi H, Hashimoto H, Tamiya N. Scale development of health status for secondary data analysis using a nationally representative survey. Environ Health Prev Med 2011. Forthcoming. [DOI] [PMC free article] [PubMed]
- 28.Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. 2008;17:152–8. doi: 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakurai K, Nishi A, Kondo K, Yanagida K, Kawakami N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci. 2011;65:434–41. doi: 10.1111/j.1440-1819.2011.02236.x. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–9. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 32.Imbens G, Lemieux T. Regression discontinuity designs: a guide to practice. J Econometrics. 2008;142:615–35. doi: 10.1016/j.jeconom.2007.05.001. [DOI] [Google Scholar]
- 33.King G, Honaker J, Joseph A, Scheve K. Analyzing incomplete political science data: an alternative algorithm for multiple imputation. Am Polit Sci Rev. 2001;95:49–69. [Google Scholar]
- 34.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- 35.Imai K, King G, Lau O. Zelig: everyone’s statistical software [Internet]. Cambridge: Harvard University, 2007. Available from: http://gking.harvard.edu/zelighttp://[accessed 12 January 2012].
- 36.Trivedi AN, Moloo H, Mor V. Increased ambulatory care copayments and hospitalizations among the elderly. N Engl J Med. 2010;362:320–8. doi: 10.1056/NEJMsa0904533. [DOI] [PubMed] [Google Scholar]
- 37.Zenkoku Shohi Jittai Chosa [Family Income and Expenditure Survey]. Tokyo: Ministry of Internal Affairs and Communications-Statistics Bureau; 2004. Japanese. [Google Scholar]
- 38.Global health risks; mortality and burden of disease attributable to selected major risks Geneva: World Health Organization; 2009. Available from: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdfhttp://[accessed 12 January 2012].
- 39.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddard GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005. [Google Scholar]
- 40.Tsuchiya A. QALYs and ageism: philosophical theories and age weighting. Health Econ. 2000;9:57–68. doi: 10.1002/(SICI)1099-1050(200001)9:1<57::AID-HEC484>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 41.Carrin G, Mathauer I, Xu K, Evans DB. Universal coverage of health services: tailoring its implementation. Bull World Health Organ. 2008;86:857–63. doi: 10.2471/BLT.07.049387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–83. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 43.Frenk J. Strengthening health systems to promote security. Lancet. 2009;373:2181–2. doi: 10.1016/S0140-6736(09)60002-7. [DOI] [PubMed] [Google Scholar]
- 44.CBnews [Internet]. Government policy on copayment of people age 70–74 for next year. Tokyo: Career Brain; 2011. Japanese. Available from: http://news.cabrain.net/article/newsId/36222.html;jsessionid=B5302A6CCDB7A2E6A29B5DF3BB050275http://[accessed 12 January 2012].
- 45.Serumaga B, Ross-Degnan D, Avery AJ, Elliott RA, Majumdar SR, Zhang F, et al. Effect of pay for performance on the management and outcomes of hypertension in the United Kingdom: interrupted time series study. BMJ. 2011;342:d108. doi: 10.1136/bmj.d108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]