The role of cytokines and growth factors in diverse forms of neurodegeneration is now widely recognized. Several proinflammatory cytokines, notably tumor necrosis factor (TNF) α and IL-1, have been shown to mediate diverse forms of experimental neurodegeneration (1, 2), although in several cases both neurotoxic and neuroprotective actions have been reported. Similarly numerous growth factors, including insulin-like growth factor (IGF), fibroblast growth factor, transforming growth factor β, ciliary neurotrophic factor, vascular endothelial growth factor, glia-derived neurotrophic factor, brain-derived neurotrophic factor, nerve growth factor, and several neurotrophins have neuroprotective and/or neurotrophic actions in vivo and in vitro (e.g., refs. 3 and 4). The mechanisms of action of such cytokines and growth factors and their interactions between these molecules are largely unknown but are major questions in neurobiology and are of direct relevance in the search for potential treatments for neurodegenerative disease.
In this issue of the Proceedings, Venters et al. (5) describe the mechanism of interaction between TNFα and IGF-1 in the death of cerebellar granule cells in vitro, which may explain the observed contribution of TNFα to neurodegeneration. They first showed that cell death, induced in primary cultures of rodent cerebellar granule cells by serum withdrawal and low potassium, is markedly inhibited by addition of recombinant IGF-1 in a dose-dependent manner. This protection by IGF-1 was paralleled by an increase in activity of the enzyme phosphatidylinositol 3′-kinase (PI3-kinase), which is known to be essential for neuroprotective effects of IGF-1 (6). As shown previously (7), TNFα alone did not influence survival of cerebellar granule neurons, even at high concentrations (5). However, very low concentrations (less than 1 pM) of TNFα inhibited the protective effects of IGF-1. TNFα suppressed IGF-1-induced phosphorylation of the insulin receptor substrate-2 (IRS-2) docking molecule and IRS-2-precipitable PI3-kinase activity, thus causing cell death. Crosstalk between TNFα and IGF-1 and insulin signaling has been reported previously in the periphery (e.g., ref. 8) but not in the brain, so this work suggests that TNFα may contribute to cell death in cerebellar granule cells by inducing resistance to the protective effects of IGF-1 through blocking its signaling pathway.
The major questions arising from this work are whether the same or similar mechanisms of interaction between intracellular signaling pathways can explain cell death in other neurones in response to other insults, whether these mechanisms apply in vivo, and whether they are applicable to the actions of other cytokines and growth factors.
The evidence that TNFα contributes to neurodegeneration is considerable but controversial. Expression of TNFα is rapidly increased in response to experimental injury induced by cerebral ischemic, excitotoxic, and traumatic injury (see ref. 9). TNFα immunoreactivity has been reported on neurones, astrocytes, microglia, and endothelial cells, and is present within perivascular spaces (10). Although TNFα does not cause cell death when infused into a normal rodent brain, there is considerable evidence that TNFα mediates neuronal death in an injured brain (e.g., ref. 9). Administration of exogenous TNFα markedly exacerbates ischemic injury in vivo (7) and, most importantly, acute inhibition of TNFα action, by administration of TNF soluble receptor (which prevents its action) (7, 11) or a neutralizing antibody to TNFα (e.g., refs. 7 and 12) markedly attenuates ischemic brain damage in rat and mouse.
In contrast, studies in mice lacking TNFα receptor suggest that TNFα may also have neuroprotective actions, mediated by the p55 receptor (13, 14). Ischemic and excitotoxic injury is greater in animals that lack either the p55 receptor or both TNF receptors, compared with wild-type animals or those lacking the p75 receptor (13, 14). This apparent anomaly between the studies described above, in which protection was observed when TNFα was inhibited acutely, and mice lacking TNFα receptors that show greater neuronal injury remains to be explained. The discrepancy could reflect differences between acute and chronic modification of TNFα, changes and adaptations associated with gene knockout—for example, developmental alterations and/or variations in growth factor expression, or the presence of other ligands for the TNF receptors.
IGFs are multifunctional peptides essential for normal growth and development (15). There is now considerable evidence to suggest that IGFs are also important in adulthood, particularly during neurodegenerative conditions. Injury to the brain results in increased expression of IGFs, their receptors, and binding proteins (e.g., ref. 16). This response is presumably protective, because exogenous IGF-1 protects the brain from hypoxic (e.g., ref. 17) and ischemic (e.g., ref. 18) injury in vivo. In vitro, IGF-1 protects hypothalamic, hippocampal, septal, and cerebellar granule neurones from diverse forms of injury (19–22).
Venters et al. (5) suggest that TNFα and IGF-1 are expressed in close proximity after insults in vivo, suggesting a potential relationship. However, although both peptides have been described in perivascular spaces (10, 16), no studies have determined whether they are coexpressed by the same cells. Venters et al. (5) report data on primary culture cerebellar granule cells. Although these cells represent a very useful experimental system of relatively pure neurones, they do not normally degenerate in clinical conditions and are slightly unusual in that they require depolarizing conditions for survival. Given that IGF-1 and TNFα are known to influence survival of other neuronal cell types in vitro and in vivo, it seems reasonable to suppose that the relationship described by Venters et al. (5) may also be relevant to other cell types and may occur in vivo, but this remains to be tested.
The mechanisms described by Venters et al. (5) may also be relevant to the actions of other cytokines in neurodegeneration. IL-1, like TNFα, is induced by experimental and clinical brain insults and exacerbates ischemic brain damage. Inhibiting exogenous IL-1 action, by administration of IL-1 receptor antagonist, significantly limits damage induced by focal or global ischemia, excitotoxins, or traumatic brain injury in rodents (see refs. 1 and 23). Indeed, there is some evidence that IL-1 can influence expression of the IGF family (e.g., ref. 24) and inhibit IGF-1 activity, possibly by interfering with IGF-1 receptor phosphorylation (e.g., ref. 25).
The work of Venters et al. (5) may also help to resolve a number of major anomalies in observations on the involvement of cytokines in neurodegeneration. For example, TNFα and IL-1 clearly contribute to and enhance experimental neurodegeneration, yet even at very high doses fail to cause cell death in healthy brain. This failure to induce death directly may be because these molecules are not neurotoxic per se, but influence survival by inhibiting the protective effect of an endogenous growth factor that is produced in the injured brain. The fact that TNFα and IL-1 contribute to but do not cause cell death is an important issue because both of these and other proinflammatory cytokines are produced in the central nervous system in response to systemic insults such as infection or inflammation (26) and act as mediators of an array of host defense responses, including fever, appetite suppression, and neuroendocrine changes (27). Clearly such cytokine production does not lead to overt neurodegeneration. Interestingly, though, there is evidence that systemic infections worsen clinical neurological conditions such as stroke and multiple sclerosis. Thus, in otherwise healthy brain, cytokine production may have no deleterious effect, but when neuronal damage is present, its expression may worsen neurodegeneration.
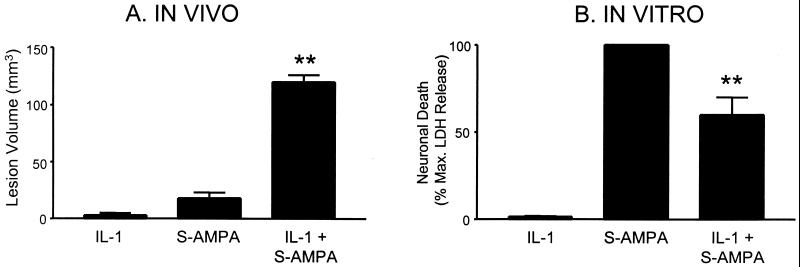
Secondly, there are significant discrepancies between in vitro studies, particularly on primary neuronal cultures, and in vivo experiments on cytokines. There are several reports that, in contrast to animal studies, in neuronal cultures, TNFα (28) and IL-1 (29) not only fail to exacerbate injury but actually reduce cell death (see Fig. 1).
Figure 1.
Effect of IL-1 on excitotoxic damage. (A) Coinfusion of recombinant IL-1β (10 ng) with the excitotoxin S-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (S-AMPA) markedly exacerbates brain damage (adapted from ref. 30) determined histologically 48 h later. (B) In contrast, in primary cultures of cortical rat neurones cell death (assessed by lactic dehydrogenase release) induced by S-AMPA is significantly inhibited by IL-1β (500 ng/ml) (adapted from ref. 29). ∗∗, P < 0.01 vs. respective S-AMPA group.
It is possible that these effects in cell culture reflect the fact that endogenous growth factors (many of which are produced by glia) are not present. Interestingly, IL-1 and TNFα have been reported to exacerbate neuronal death on mixed cultures of neurones and glia (31, 32). It has been assumed that this may reflect release of neurotoxins from glia, but instead it may be caused by cytokine inhibition of endogenous growth factors such as IGF-1 produced by glia in the culture, which are inhibiting neuronal cell death. Further elucidation of the role of endogenous cytokines and growth factors and their mechanisms of interaction may require studies on mixed populations of neurones and glia. The primary source of TNFα and IL-1 after injury is microglia, but astrocytes, oligodendrocytes, neurones, and vascular endothelial cells may also produce cytokines (26), further adding to the potential complexity of this cascade of interactions.
Venters et al. (5) report that serum withdrawal combined with low KCl in cerebellar granule cells leads to cell death associated with features of apoptosis. There is considerable debate about the functional importance of apoptosis in neurodegeneration in the adult nervous system (33). Thus, it will be important to determine whether similar crosstalk between TNFα and IGF-1 contributes to cell death induced by stimuli that induce cell death, which appears to be largely necrotic, and whether similar mechanisms apply to other neuronal cell types.
The major questions that remain to be addressed are whether cytokine inhibition of growth factor protection is a common mechanism of neurodegeneration, and what are the downstream signaling pathways by which growth factors and cytokines modify cell death.
Acknowledgments
N.J.R. is supported by a Medical Research Council Research Chair and S.L. is supported by a Royal Society fellowship.
ABBREVIATIONS
- TNFα
tumor necrosis factor α
- IGF
insulin-like growth factor
Footnotes
A commentary on this article begins on page 9879.
References
- 1.Rothwell N J. J Physiol (London) 1999;514:3–17. doi: 10.1111/j.1469-7793.1999.003af.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feuerstein G Z, Wang X, Barone F C. NeuroImmunoModulation. 1998;5:143–159. doi: 10.1159/000026331. [DOI] [PubMed] [Google Scholar]
- 3.Connor B, Dragunow M. Brain Res Rev. 1998;27:1–39. doi: 10.1016/s0165-0173(98)00004-6. [DOI] [PubMed] [Google Scholar]
- 4.Dore S, Kar S, Quirion R. Trends Neurosci. 1997;20:326–331. doi: 10.1016/s0166-2236(96)01036-3. [DOI] [PubMed] [Google Scholar]
- 5.Venters H D, Tang Q, Liu Q, VanHoy R W, Dantzer R, Kelley K W. Proc Natl Acad Sci USA. 1999;96:9879–9884. doi: 10.1073/pnas.96.17.9879. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Zhang F X, Rubin R, Rooney T A. J Neurochem. 1998;71:196–204. doi: 10.1046/j.1471-4159.1998.71010196.x. [DOI] [PubMed] [Google Scholar]
- 7.Barone F C, Arvin B, White R F, Miller A, Webb C L, Willette R N, Lysko P G, Feuerstein G Z. Stroke (Dallas) 1997;28:1233–1244. doi: 10.1161/01.str.28.6.1233. [DOI] [PubMed] [Google Scholar]
- 8.Peraldi P, Hotamisligil G S, Buurman W A, White M F, Spiegelman B M. J Biol Chem. 1996;271:13018–13022. doi: 10.1074/jbc.271.22.13018. [DOI] [PubMed] [Google Scholar]
- 9.Feuerstein G Z, Liu T, Barone F C. Cerebrovasc Brain Metab Rev. 1995;6:341–360. [PubMed] [Google Scholar]
- 10.Botchkina G I, Meistrell M E, Botchkina I L, Tracey K J. Mol Med. 1997;3:765–781. [PMC free article] [PubMed] [Google Scholar]
- 11.Nawashiro H, Martin D, Hallenbeck J M. J Cereb Blood Flow Metab. 1997;17:229–232. doi: 10.1097/00004647-199702000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Lavine S D, Hofman F M, Zlokovic B V. J Cereb Blood Flow Metab. 1998;18(1):52–58. doi: 10.1097/00004647-199801000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Bruce A J, Boling W, Kindy M S, Peschon J, Kraemer P J, Carpenter M K, Holtsberg F W, Mattson M P. Nat Med. 1996;2:788–794. doi: 10.1038/nm0796-788. [DOI] [PubMed] [Google Scholar]
- 14.Gary D S, Bruce-Keller A J, Kindy M S, Mattson M P. J Cereb Blood Flow Metab. 1998;18:1283–1287. doi: 10.1097/00004647-199812000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Jones J I, Clemmons D R. Endocr Rev. 1995;16:3–34. doi: 10.1210/edrv-16-1-3. [DOI] [PubMed] [Google Scholar]
- 16.Beilharz E J, Russo V C, Butler G, Baker N L, Connor B, Sirimanne E S, Dragunow M, Werther G A, Gluckman P D, Williams C E, et al. Brain Res Mol Brain Res. 1998;59:119–134. doi: 10.1016/s0169-328x(98)00122-3. [DOI] [PubMed] [Google Scholar]
- 17.Gluckman P D, Guan J, Williams C, Scheepens A, Zhang R, Bennet L, Gunn A. Mol Cell Endocrinol. 1998;140:95–99. doi: 10.1016/s0303-7207(98)00035-5. [DOI] [PubMed] [Google Scholar]
- 18.Loddick S A, Liu X-J, Lu Z-X, Liu C, Behan D P, Chalmers D C, Foster A C, Vale W W, Ling N, De Souza E B. Proc Natl Acad Sci USA. 1998;95:1894–1898. doi: 10.1073/pnas.95.4.1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng B, Mattson M P. J Neurosci. 1992;12:1558–1566. doi: 10.1523/JNEUROSCI.12-04-01558.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dore S, Kar S, Quirion R. Proc Natl Acad Sci USA. 1997;94:4772–4777. doi: 10.1073/pnas.94.9.4772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galli C, Meucci O, Scorziello A, Werge T M, Calissano P, Schettini G. J Neurosci. 1995;15:1172–1179. doi: 10.1523/JNEUROSCI.15-02-01172.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sortino M A, Canonico P L. Endocrinology. 1996;137:1418–1422. doi: 10.1210/endo.137.4.8625919. [DOI] [PubMed] [Google Scholar]
- 23.Rothwell N, Allan S, Toulmond S. J Clin Invest. 1997;100:2648–2652. doi: 10.1172/JCI119808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fan J, Wojnar M M, Theodorakis M, Lang C H. Am J Physiol. 1996;270:R621–R629. doi: 10.1152/ajpregu.1996.270.3.R621. [DOI] [PubMed] [Google Scholar]
- 25.Costantino A, Vinci C, Mineo R, Frasca F, Pandini G, Milazzo G, Vigneri R, Belfiore A. Endocrinology. 1996;137:4100–4107. doi: 10.1210/endo.137.10.8828463. [DOI] [PubMed] [Google Scholar]
- 26.Hopkins S J, Rothwell N J. Trends Neurosci. 1995;18:83–88. [PubMed] [Google Scholar]
- 27.Rothwell N J, Hopkins S J. Trends Neurosci. 1995;18:130–136. doi: 10.1016/0166-2236(95)93890-a. [DOI] [PubMed] [Google Scholar]
- 28.Mattson M P, Goodman Y, Luo H, Fu W, Furukawa K. J Neurosci Res. 1997;49:681–697. doi: 10.1002/(SICI)1097-4547(19970915)49:6<681::AID-JNR3>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 29.Strijbos P J L M, Rothwell N J. J Neurosci. 1995;15:3468–3474. doi: 10.1523/JNEUROSCI.15-05-03468.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lawrence C B, Allan S M, Rothwell N J. Eur J Neurosci. 1998;10:1188–1195. doi: 10.1046/j.1460-9568.1998.00136.x. [DOI] [PubMed] [Google Scholar]
- 31.Chao C C, Hu S, Ehrlich L, Peterson P K. Brain Behav Immun. 1995;9:355–365. doi: 10.1006/brbi.1995.1033. [DOI] [PubMed] [Google Scholar]
- 32.Jeohn G H, Kong L Y, Wilson B, Hudson P, Hong J S. J Neuroimmunol. 1998;85:1–10. doi: 10.1016/s0165-5728(97)00204-x. [DOI] [PubMed] [Google Scholar]
- 33.Nicotera P, Leist M, Manzo L. Trends Pharmacol Sci. 1999;20:46–51. doi: 10.1016/s0165-6147(99)01304-8. [DOI] [PubMed] [Google Scholar]