Abstract
Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA), also known as Herlyn-Werner-Wunderlich syndrome, is a rare syndrome with only a few hundred reported cases described since 1922. Only a handful of these cases have been associated with pyocolpos. Mullerian duct anomalies have an incidence of 2–3%. While OHVIRA constitutes 0.16–10% of these Mullerian duct anomalies. Symptoms usually present shortly after menarche when hematocolpos develops during menstruation resulting in dysmenorrhea and a pelvic mass. The pelvic mass is the collection of blood products within the obstructed hemivagina. The first study in the diagnostic work-up is usually ultrasonography, which typically demonstrates a pelvic fluid collection which can simulate other disease processes thus confounding the diagnosis. MRI findings of the pelvis reveal a didelphic uterus. Imaging of the abdomen reveals agenesis of the ipsilateral kidney. MRI is beneficial in characterizing the didelphic uterus and vaginal septum for pre-operative planning. Understanding the imaging findings, in conjunction with the clinical presentation, is critical for early diagnosis in attempting to prevent complications such as endometriosis or adhesions from chronic infections with subsequent infertility.
Keywords: Herlyn-Werner-Wunderlich syndrome, OHVIRA, Mullerian duct anomalies, didelphic uterus
CASE REPORT
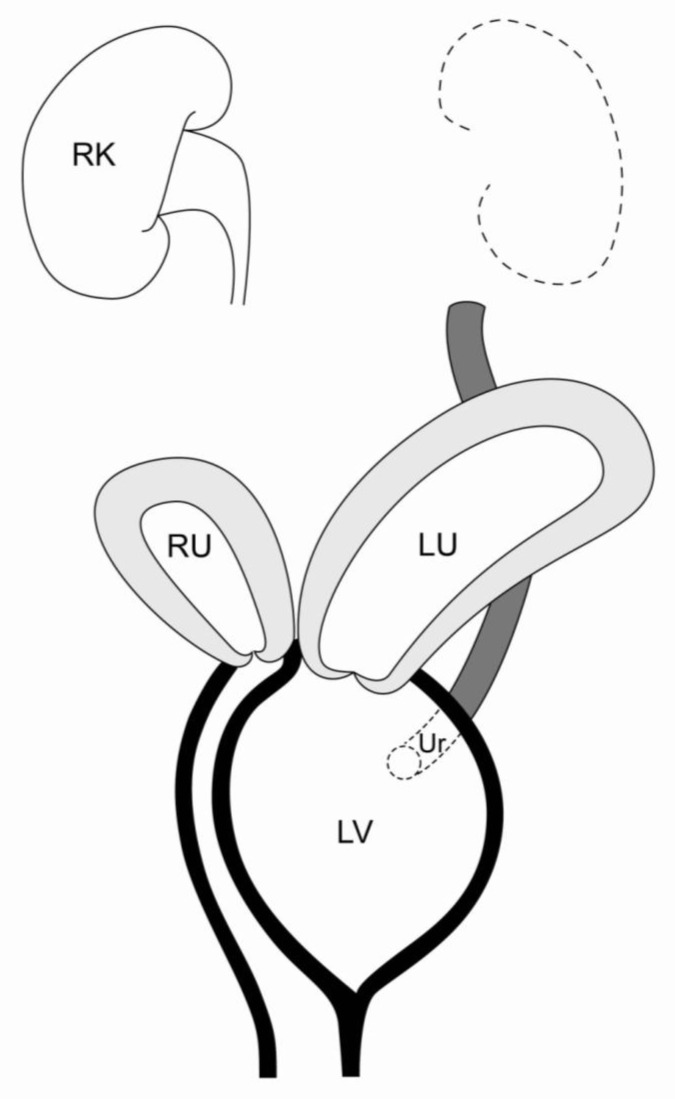
We present an unusual case of a didelphic uterus with pyocolpos in an obstructed hemivagina and ipsilateral renal anomaly (figure 1).
Figure 1.
Diagram depicting OHVIRA. Didelphic uterus with left hemivaginal obstruction (LV), hydrometrocolpos of the left uterine horn (LU) and ipsilateral renal agensis. Occasional ectopic ureter (Ur) insertion into the obstructed hemivagina can occur.
A 17-year-old Caucasian female presented to our institution with progressive painful distention of the lower abdomen. It was not until recently that she began complaining of yellowish vaginal discharge. She denied fevers, chills, nausea, vomiting or diarrhea. However, she reported an ultrasound performed in a small military medical clinic in Samoa, prior to her arrival, revealed absence of her left kidney.
The patient had reported overall good health. She denied sexual activity or exposure to sexually transmitted diseases. She also denied any gynecological problems except for the recent cyclic abdominal pain and enlarging abdominal mass. The patient reported normal menstruation beginning at 12–13 years of age. She denied any prior surgeries, use of medications or allergies. Family history was relevant for a paternal aunt with ovarian and cervical cancer and a mother with questionable cervical cancer.
Physical exam was remarkable only for a palpable left pelvic mass, which measured 4.5 × 3.5 cm on bedside ultrasound. Speculum exam revealed a fluctuant intravaginal mass. A normal appearing right sided cervix was identified with yellowish vaginal discharge. The external genitalia was normal. Furthermore, a urinalysis later demonstrated a urinary tract infection, which was subsequently treated with antibiotics.
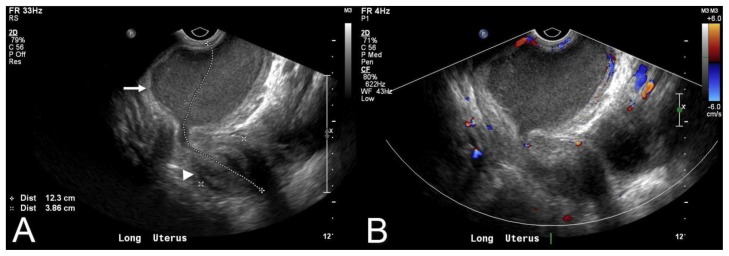
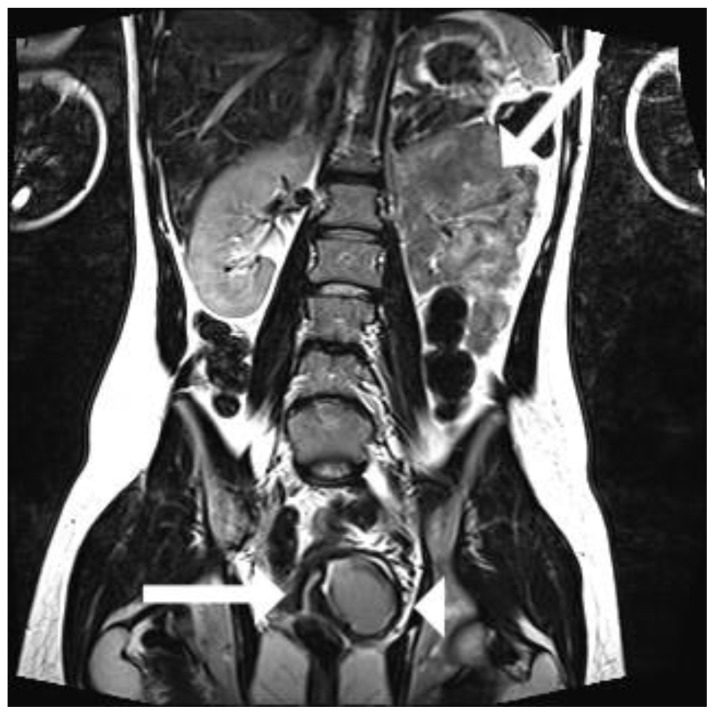
The patient was sent to radiology for further characterization. A pelvic ultrasound was performed revealing a 7 cm fluid collection with diffuse low level internal echoes, which appeared contiguous with the endocervix (figure 2). Subsequently, a MRI was performed to better characterize the pelvic anatomy and better identify the anatomic location of this pelvic fluid collection. A didelphic uterus was demonstrated. The right endometrial cavity appeared normal along with the right cervix. The left endometrial cavity was moderately distended and contiguous with the obstructed hemivagina. The fluid in the obstructed left hemivagina measured 6.7 × 7.4 × 8.2 cm (figure 3). The high T2 signal characteristics in conjunction with low level internal echoes seen on the comparison ultrasound were consistent with hematometrocolpos vs pyocolpos (figure 2, 3). Imaging of both renal fossae confirmed the ultrasound findings of left renal agenesis (figure 4).
Figure 2.
17 year old female with OHVIRA and pyocolpos. Endovaginal longitudinal view of the uterus (8 MHz EV transducer, Phillips iU22) demonstrating an obstructed left hemivagina (arrow) with retained echogenic fluid. Uterus is also visualized in this image (arrowhead). Color Doppler demonstrates no flow in the collection.
Figure 3.
17 year old female with OHVIRA and pyocolpos. Initial noncontrast coronal T2 FSE weighted sequence (3T Siemens, 5mm slice thickness, TR 3,800, TE 120) demonstrates a didelphic uterus with obstructed left uterine horn (large arrow) and left hemivagina (arrowhead). Note the right uterine horn (small arrow).
Figure 4.
17 year old female with OHVIRA and pyocolpos. Coronal follow-up non-contrast enhanced T2 fat saturated MRI (3T Siemens, 5mm slice thickness, TR 3,822.8, TE 154) through the abdomen demonstrating absence of the left kidney (arrow) with reacumulation of fluid in the obstructed hemivagina status post IR drainage (arrowhead). Note the right uterine horn (small arrow).
The patient was subsequently sent to interventional radiology for drainage of the obstructed left hemivagina to alleviate her pain before surgical resection of the vaginal septum. A pigtail catheter was placed under ultrasound guidance. Purulent fluid was drained and sent to the lab for further evaluation. Aerobic cultures grew out staphylococcus aureus and agalactiae, while the anaerobic cultures grew out lactobacillus and prevotella bivia. The pigtail catheter was left in place for 4 days at which time it was removed in the locked position in an attempt to prevent reaccumulation of fluid by lacerating the wall of the hemivagina (Figure 5). This was done in an attempt to forgo the need for vaginoplasty. However, follow-up MRI 2 days after drain removal demonstrated re-accumulation of fluid in the left hemivagina (Figure 4). The patient subsequently underwent successful surgical resection of the vaginal septum.
Figure 5.
17 year old female with OHVIRA and pyocolpos. AP fluoroscopic image (Siemens Artis Zee, kvp 70, mA 47) of post transvaginal drainage catheter placement into the infected hemivaginal fluid collection.
DISCUSSION
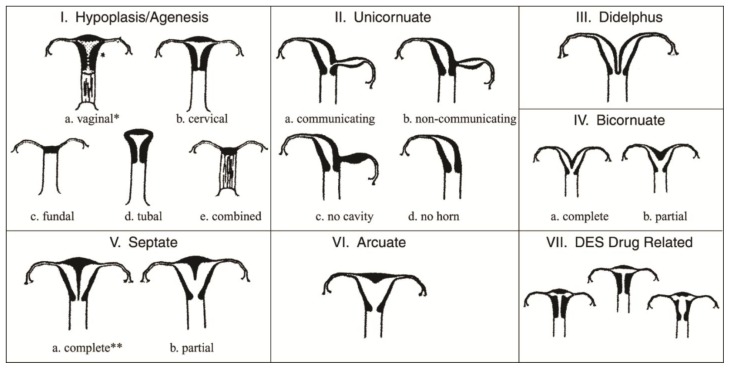
There is a spectrum of uterine fusion anomalies that can occur during early development. Lateral fusion defects are the most common type of Mullerian duct abnormalities ranging from symmetric or asymmetric to obstructed or non-obstructed fusion anomalies. This has ultimately lead to the classification scheme developed by the American Fertility Society, which describes the appearance of the uterus given the various fusion anomalies that can occur (figure 6).
Figure 6.
The American Fertility Society Classification Of Mullerian Anomalies: The spectrum of fusion anomalies. Reprinted with permission.
A didelphic uterus with an obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) is a rare congenital anomaly constituting 0.16–10% of all Mullerian duct abnormalities [1]. Patients present with pelvic pain, worsening dysmenorrhea, and an associated pelvic mass [2]. There have only been a few case reports to date discussing the rare complication of pyocolpos in this entity. As in our case, most cases report a history of normal regular menstral periods up until there is an obstruction of the hemivagina resulting in abdominal distention and pelvic pain. Some patients occasionally present with urgency, frequency or vaginal discharge [3].
A didelphic uterus is suggestive of an embryologic arrest occurring during the 8th week of gestation which ultimately affects the Mullerian and Metanephric ducts [4]. The exact cause of this developmental defect is not known. However, if one of the Wolffian ducts is absent, the kidney and ureter on the ipsilateral side will fail to fuse at midline. This process may occur completely or incompletely. If the failure to fuse is complete, then a uterus didelphys is formed. The Mullerian duct, on the side lacking the Wolffian duct, displaces itself laterally and cannot come into contact with the urogenital sinus in the center resulting in a blind sac, imperforate or obstructed vagina. However, the distal part of the vagina, originating from the urogenital sinus is not affected [4]. Each ureteric bud develops from the Wolffian duct which is ultimately responsible for the development of the kidney. Occasionally an ectopically obstructed ureter inserts into the obstructed hemivagina on the side of the congenitally absent ipsilateral kidney (figure 1) [3]. The ureteric bud grows dorsocranially into the metanephric blastema inducing differentiation of the metanephric nephrons. If the ureteric bud fails to either form or make contact with the metanephric blastema, the kidney on that side will fail to develop [4].
US and MRI are the modalities of choice for the diagnosis and surgical planning of OHVIRA. Although US can be used to diagnose this condition, MRI plays an important role in further characterizing the didelphic uterus, obstructed hemivagina, and ipsilateral renal agenesis. Furthermore, MRI is superior to ultrasound by allowing for better characterization of anatomic relationships given its multiplanar capabilities and wider field of view, important for surgical planning.
Delays in diagnosis have been attributed to lack of understanding of this condition by radiologists, gynecologists, and pediatricians. Furthermore, regular menstruation in the context of an incomplete vaginal outlet obstruction and slow extension of hematocolpos have also been described as culprits to delayed diagnosis [3]. Delayed diagnosis can lead to complications that include endometriosis, adhesions, infertility and infectious complications arising from chronic cryptomenorrhoea [1].
The diagnosis of OHVIRA should be suspected in cases of women presenting with pelvic pain and a pelvic mass with ipsilateral renal agenesis. Systematic analysis of the literature suggests management of these cases to consist mainly of vaginoplasty with excision of the vaginal septum in order to prevent the long term complication of recurrent pyocolpos and infertility from chronic cryptomenorrhoea. In a case review series of 15 patients, those patients who desired pregnancy following vaginoplasty and/or hemihysterectomy demonstrated successful pregnancy rates similar to females with didelphic uteri [5]. Those cases where an ectopic ureter inserts into the obstructed hemivagina, laproscopic surgical ligation vs surgical removal is advocated to prevent recurrent fluid accumulation in the obstructed hemivagina [3]. It could be argued that surgical excision might be better as there have been reported cases of malignant transformation occurring in the ectopic ureter [3].
TEACHING POINT
OHVIRA (obstructed hemivagina with ipsilateral renal agenesis) with pyocolpos is a rare clinical presentation. Ultrasound and MRI findings can collectively delineate uterine morphology, absence of the ipsilateral kidney, and the nature of the fluid content in the obstructed hemivagina. Understanding the imaging findings is critical for early diagnosis in attempt to prevent complications such as endometriosis or adhesions from chronic infections with subsequent infertility.
Table 1.
Summary table of obstructed hemivagina with ipsilateral renal agenesis (OHVIRA)
| Etiology | The pathogenesis is not well understood, but is believed to be related to Mullerian duct fusion anomaly which results in failed development of the Wolffian duct on the side of the obstructed hemivagina causing ipsilateral renal agenesis. |
|
| |
| Incidence | .16–10% of all Mullerian duct anomalies |
|
| |
| Age predilection | Mean age 14 years. |
|
| |
| Risk factors | No known risk factors |
|
| |
| Treatment | Hemihysterectomy with excision of the vaginal septum in order to prevent the long term complication of recurrent pyocolpos or hematometrocolpos. |
|
| |
| Prognosis | Excellent with generally no effect on reproduction after treatment. |
|
| |
| Imaging findings | |
| US | Didelphic uterus with a fluid collection which may be anechoic or demonstrate diffuse low level swirling echogenicities. Absent ipsilateral kidney. |
| CT | Fluid density mass in the pelvis with absent ipsilateral kidney. |
| MR | Didelphic uterus with iso/hypointense T1 and increased T2 signal pelvic fluid collection; ipsilateral renal agenesis |
Table 2.
Differential table of obstructed hemivagina with ipsilateral renal agenesis (OHVIRA)
| X-ray | Pelvic US | CT | MRI | Contrast enhancement | |
|---|---|---|---|---|---|
| OHVIRA | Absent renal outline suggesting diagnosis | Pelvic fluid collection contiguous with the endocervix | Hypo/hyper dense pelvic fluid collection, absent ipsilateral kidney | Iso/low T1, high T2 signal pelvic fluid collection contiguous with the endocervix; didelphic uterus; Ipsilateral renal agenesis. | None unless infected |
| Cystic ovarian Malignancy | NA | Multiseptated pelvic mass with internal flow | Fluid/soft tissue density septated pelvic mass | Multiloculated low/high T1, areas of high T2 signal. | Enhancing soft tissue components |
| Pelvic abscess | NA | Heterogeneous echogenic pelvic mass with peripheral flow | Fluid density pelvic mass, kidneys present | Low T1, high T2 signal pelvic mass with with/without loculations | Peripheral enhancement |
| Ovarian cyst | NA | Anechoic fluid verses fluid with low level echoes, consistent with/hemorrhage | Fluid density pelvic mass, kidneys are present | Iso/low T1, high T2 signal pelvic mass | None |
| Pyosalpinx | NA | Tubular hyperechoic pelvic mass | Tubular fluid density pelvic mass, kidneys present | Iso/low T1, high T2 signal tubular pelvic mass; kidneys present | None to mild peripheral enhancement |
| Hydrosalpinx | NA | Tubular hypoechoic pelvic mass | Tubular hypodense pelvic mass, kidneys present | Tubular low T1, high T2 signal pelvic mass. Kidneys are present | None |
ABBREVIATIONS
- OHVIRA
Obstructed hemivagina and ipsilateral renal anomaly
- MRI
Magnetic resonance imaging
REFERENCES
- 1.Adair L, II, Georgiades M, Osborne R, Ng T. Uterus didelphys with unilateral distal vaginal agenesis and ipsilateral renal agenesis: Common presentation of an unusual variation. [Accessed February 13, 2012];Journal of Radiology Case Reports. 2011 5:1–8. doi: 10.3941/jrcr.v5i1.572. http// www.radiologycases.com/index.php/radiologycases/article/view/572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoeffel C, Olivier M, Scheffler C, et al. Uterus didelphys, obstructed hemivagina and ipsilateral renal agenesis. European Journal of Radiology. 1997;25:246–248. doi: 10.1016/s0720-048x(96)01149-7. [DOI] [PubMed] [Google Scholar]
- 3.Boram H, Herndon C, Rosen M, et al. Uterine didelphys associated with obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: Radiology Case Reports. 2010. [Accessed November 2, 2011]. http://radiology.casereports.net/index.php/rcr/article/viewFile/327/702. [DOI] [PMC free article] [PubMed]
- 4.Vercellini P, Daguati R, Somigliana E, et al. Asymmetric lateral distribution of obstructed hemivagina and renal agenesis in women with uterus didelphys: institutional case series and a systematic literature review. Fertility Sterility. 2007;87:719–24. doi: 10.1016/j.fertnstert.2007.01.173. [DOI] [PubMed] [Google Scholar]
- 5.Phupong V, Pruksananonda K, Taneepanichskul S, et al. Double Uterus with Unilaterally Obstructed Hemivagina and Ipsilateral Renal Agenesis: A Variety Presentation and a 10-Year Review of the Literature. Journal Medical Thai. 2000;83:569–574. [PubMed] [Google Scholar]
- 6.Orazi C, Lucchetti M, Schingo P, et al. Herlyn-Werner-Wunderlich syndrome: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis: Sonographic and MR findings in 11 cases. Pediatric Radiology. 2007;37:657–665. doi: 10.1007/s00247-007-0497-y. [DOI] [PubMed] [Google Scholar]