Abstract
The orexin system is a key regulator of sleep and wakefulness. In a multicenter, double-blind, randomized, placebo-controlled, two-way crossover study, 161 primary insomnia patients received either the dual orexin receptor antagonist almorexant, at 400, 200, 100, or 50 mg in consecutive stages, or placebo on treatment nights at 1-week intervals. The primary end point was sleep efficiency (SE) measured by polysomnography; secondary end points were objective latency to persistent sleep (LPS), wake after sleep onset (WASO), safety, and tolerability. Dose-dependent almorexant effects were observed on SE, LPS, and WASO. SE improved significantly after almorexant 400 mg vs. placebo (mean treatment effect 14.4%; P < 0.001). LPS (–18 min (P = 0.02)) and WASO (–54 min (P < 0.001)) decreased significantly at 400 mg vs. placebo. Adverse-event incidence was dose-related. Almorexant consistently and dose-dependently improved sleep variables. The orexin system may offer a new treatment approach for primary insomnia.
The orexin system has been implicated in the regulation of functions such as reward seeking,1 feeding behavior,2 locomotion and physical activity,3,4,5 and arousal from sleep and the sleep–wake cycle.6,7 Orexin-A and orexin-B (also known as hypocretin-1 and hypocretin-2, respectively) are neuropeptides that bind to the G protein–coupled receptors orexin-1 and orexin-2.8,9,10 In rats as well as in humans, orexin levels in cerebrospinal fluid have been shown to fluctuate with the circadian cycle.11,12,13 The levels are highest at the end of the wake-active period and lowest at the end of the sleep period.11,12,13 Orexin deficiency has been linked to narcoleptic symptoms such as sudden sleep attacks and cataplexy, in animals14,15,16 as well as in humans.17,18
Experiments in mice and rats have shown that orexin receptor antagonists have sleep-enabling effects.3,19 The dual orexin receptor antagonist almorexant elicits somnolence without cataplexy in healthy rats, dogs, and humans when given during the active phase of the circadian cycle.20 A phase I study investigating single-dose daytime administration of almorexant in healthy human subjects showed dose-dependent pharmacodynamic effects, with reductions in vigilance, alertness, visuomotor, and motor coordination observed for the 400- and 1,000-mg doses.21 In the same study, pharmacoelectroencephalography profiles showed that almorexant decreases alpha Pz–Oz and increases beta Fz–Cz activities, as well as delta and theta power.21 The increase in delta and theta power may potentially indicate slow-wave sleep. Hence, inhibiting the orexin system with almorexant could represent a novel approach to the treatment of insomnia.
Insomnia is a persistent problem in ~10% of adults,22,23,24 with primary insomnia estimated to be present in ~25% of patients with chronic insomnia.25 Sleep-maintenance problems and nocturnal awakenings are more prevalent than sleep-onset difficulties.26,27 Nonpharmacologic treatments are often preferred;28 however, eventually, most patients either seek pharmacologic treatment or remain untreated.29 Current standard pharmacologic treatments for insomnia include the benzodiazepine receptor agonists, (which potentiate the activity of γ-aminobutyric acid at the ionotropic γ-aminobutyric acid-A receptor), and the melatonin receptor agonist ramelteon. Benzodiazepine receptor agonists include benzodiazepines that decrease sleep latency and increase sleep time,30,31,32 with some agents also improving sleep maintenance.30,32 However, benzodiazepines have been associated with daytime drowsiness, tolerance, dependency, and withdrawal symptoms.33,34,35 Newer benzodiazepine receptor agonists (nonbenzodiazepines) and ramelteon decrease sleep latency,33,36,37 whereas some agents, such as eszopiclone and modified-release zolpidem, increase sleep time and improve sleep maintenance.38,39 The side-effect profiles of nonbenzodiazepines and ramelteon appear to be better than those of benzodiazepines, with fewer next-day effects observed.33,35,36,37,40 New insomnia therapies with different mechanisms of action are currently under investigation with the aim of further improving tolerability and sleep maintenance and specifically targeting sleep–wake architecture.41,42
We performed a two-part clinical study to evaluate the effect of almorexant on sleep in patients with primary insomnia. The primary objective was to determine the minimum dose of almorexant that would have a significant effect on sleep efficiency (SE). In the first part of the study, the effect of almorexant on SE was evaluated at a high dose of 400 mg; thereafter, we conducted the dose-ranging part of the study, which aimed to identify the minimum effective dose. The safety and tolerability of almorexant and its effect on objective and subjective sleep variables were also evaluated.
Results
Between May 2006 and August 2007, 368 patients were screened and 161 were enrolled. Supplementary Figure S1 online shows a summary of study enrollment and the patients treated at each dose level. The main reasons for screening failure were total sleep time (TST) >6 h and/or latency to persistent sleep (LPS) <20 min. Overall, eight patients were excluded from the per-protocol analysis: two of these did not complete the second treatment night because of adverse events (AEs) and six were excluded because of technical difficulties during polysomnography. The per-protocol analysis set therefore consisted of 153 patients. The mean age of all the patients treated was 45.2 years (60% in the age group 41–60 years); 66.5% were women; 98.8% were Caucasian, 0.6% were Hispanic, and 0.6% were Asian. The mean body mass index was 24.2 kg/m2.
Efficacy
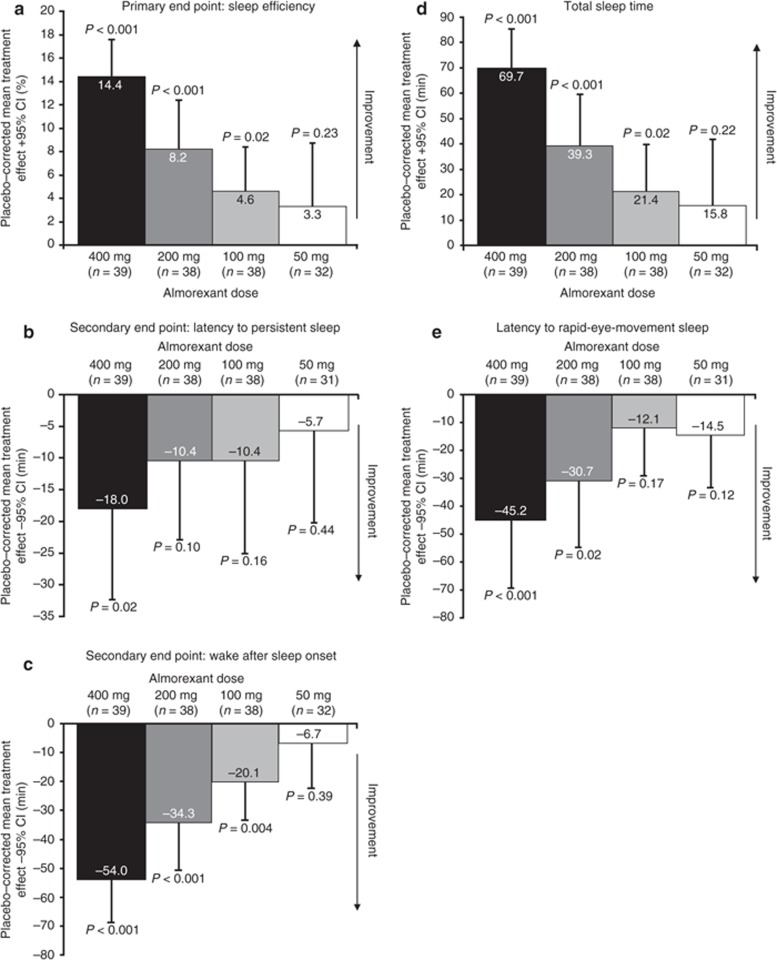
Objective polysomnographic assessments. The mean values for objective sleep variables on the screening/adaptation night and the almorexant and placebo treatment nights for almorexant 400, 200, 100, and 50 mg are reported in Table 1. SE significantly improved after a single 400-mg dose of almorexant, relative to placebo (mean treatment effect 14.4%; P < 0.001), thereby demonstrating the efficacy of almorexant at this dose level (Figure 1a). A dose-related increase in SE was observed with almorexant 100, 200, and 400 mg relative to placebo (Figure 1a). The lowest effective dose was 100 mg (mean treatment effect 4.6%; P = 0.02). No significant treatment effect was observed for a dose of 50 mg (mean treatment effect 3.3%; P = 0.23), and enrollment was stopped in accordance with the study protocol. As a result, only six patients were recruited to the 25-mg dose group, and consequently the efficacy data for this dose group are not reported; however, the data for these patients were included in the safety analysis. The robustness of the main analysis was confirmed by similar findings for the all-treated analysis, which persisted even after adjustment for period and carryover effects (see Supplementary Table S1 online). LPS was significantly reduced after the 400-mg dose of almorexant relative to placebo (mean treatment effect –18 min; P = 0.02; Figure 1b). Wake after sleep onset (WASO) declined significantly in response to the 400-mg dose relative to placebo (mean treatment effect –54 min; P < 0.001), and dose-related, clinically relevant, and nominally significant improvements were observed after almorexant doses of 200 (P < 0.001) and 100 mg (P = 0.004) (Figure 1c).
Table 1. Mean values of objective sleep variables for the screening/adaptation night and the treatment nights.
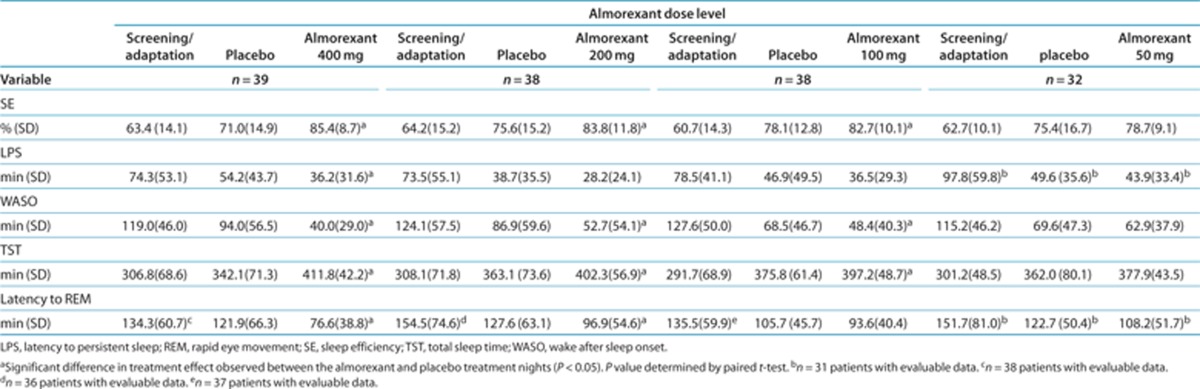
Figure 1.
Treatment effects of almorexant on objective sleep variables. Mean changes relative to placebo with 95% CIs. CI, confidence interval.
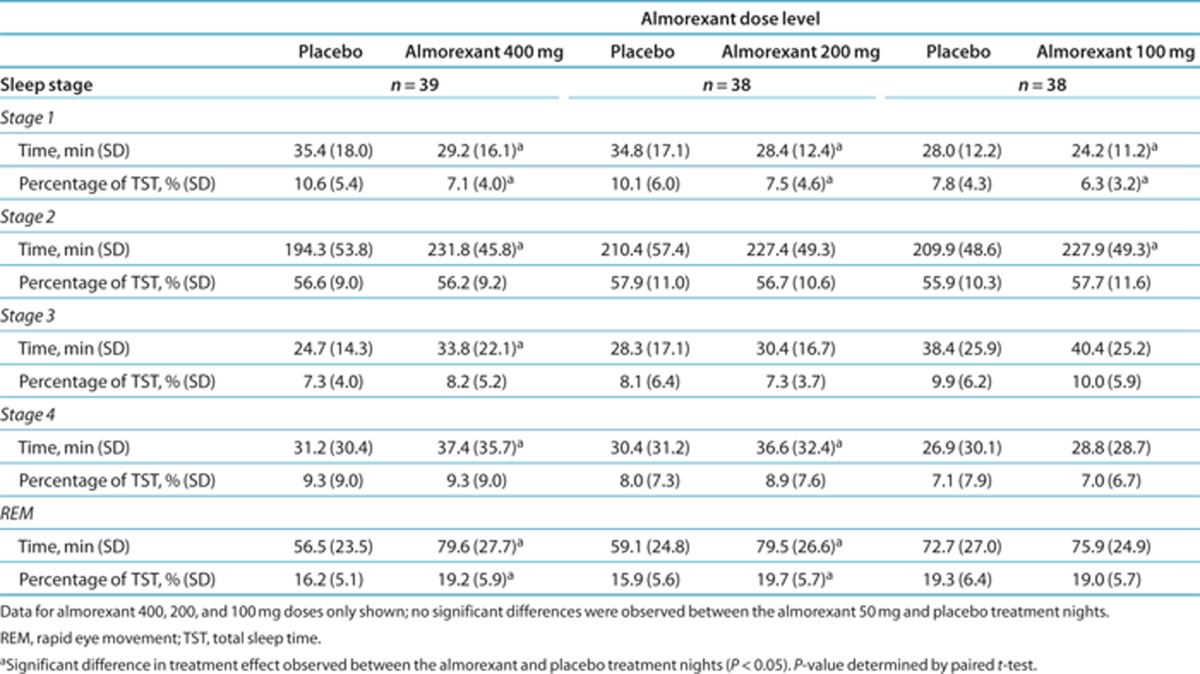
Exploratory polysomnography measurements showed dose-related increases in mean TST for almorexant 400, 200, and 100 mg as compared with placebo (Figure 1d). Almorexant 400 mg was associated with a mean of 411.8 min sleep vs. 342.1 min with placebo. Higher almorexant doses reduced latencies to S1 (400 mg), S2, S3, and S4 sleep stages (200 mg) (data not shown). Latency to rapid eye movement (REM) sleep decreased dose-dependently (Figure 1e). Almorexant 400 mg decreased the time spent in S1 and increased the time spent in S2, S3, S4, and REM sleep stages, as compared with placebo (Table 2). Similar but less pronounced effects were observed after the 200- and 100-mg doses. The percentage of TST spent in S1 decreased dose-dependently and the percentage of TST spent in REM increased dose-dependently after 400 and 200 mg as compared with placebo. The percentages of TST spent in S2, S3, and S4 were similar after placebo and after almorexant, irrespective of the almorexant dose.
Table 2. Mean values of time in sleep stages and percentage of each sleep stage of total sleep time for the treatment nights.
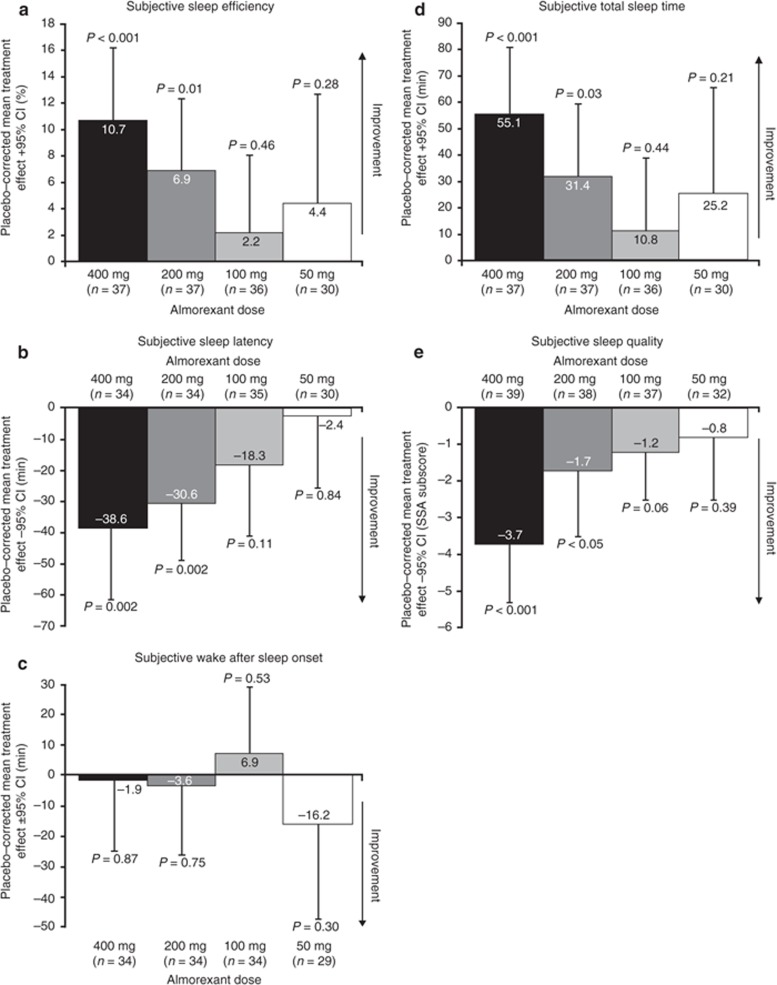
Subjective assessments. The mean values for subjective assessments on the night of the screening/adaptation and on the nights of almorexant (400-, 200-, 100-, and 50-mg doses) and placebo treatments are given in Table 3. Self-reported patient assessments showed dose-related increases in subjective SE (Figure 2a) and decreases in subjective sleep latency after almorexant 400 and 200 mg relative to placebo (Figure 2b). No treatment differences were observed for mean subjective WASO at any almorexant dose relative to placebo (Figure 2c). Subjective TST increased dose-dependently (Figure 2d). Subjective sleep quality improved after almorexant 400 and 200 mg relative to placebo (Figure 2e). Awakening quality and somatic complaint subscores were similar among treatments (data not shown).
Table 3. Mean values of subjective sleep variables and next-day performance for the screening/adaptation night and the treatment nights.
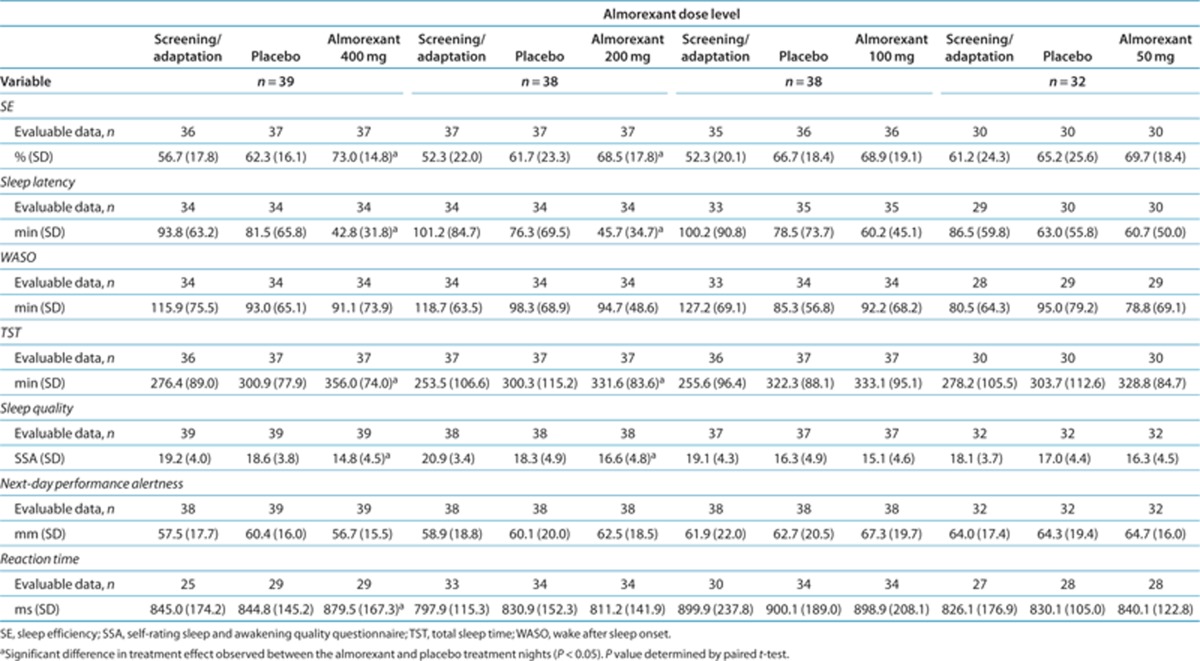
Figure 2.
Treatment effects of almorexant on subjective sleep variables. Mean changes relative to placebo with 95% CIs. CI, confidence interval; SSA, self-rating sleep and awakening quality questionnaire.
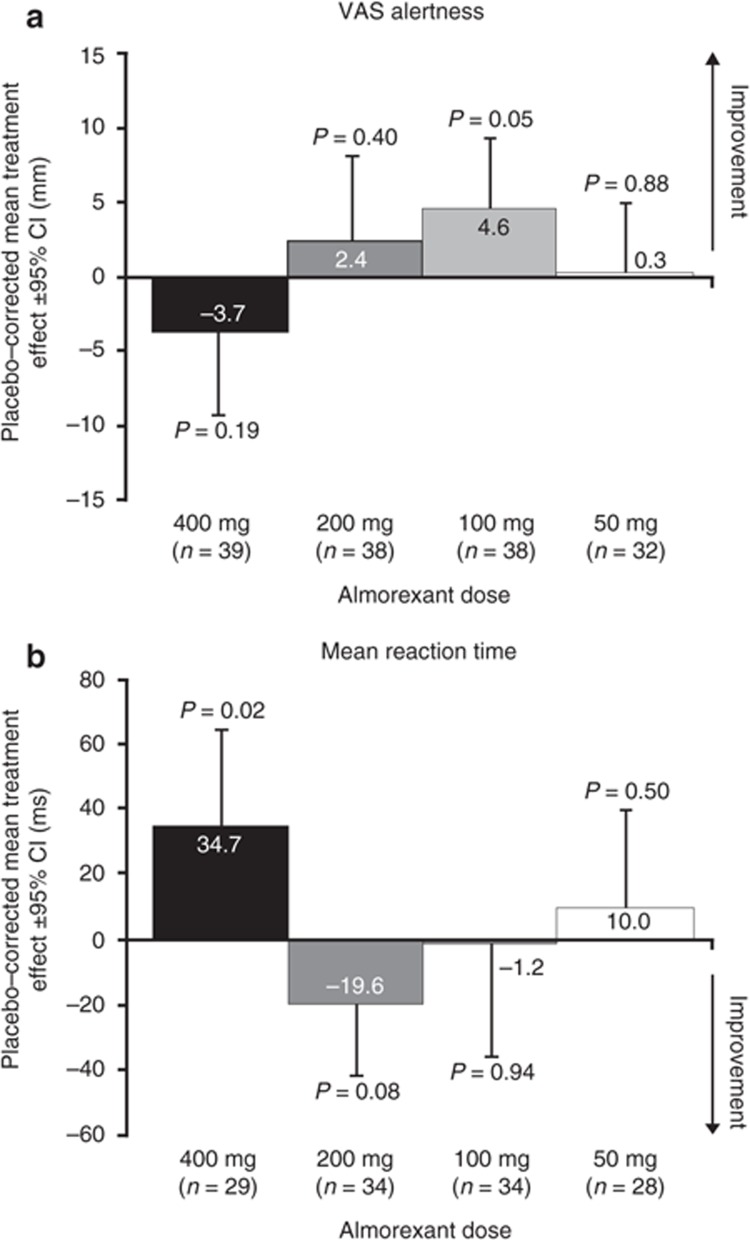
Next-day performance. Overall, no relevant negative residual effects of the previous night's treatment were observed after any of the almorexant doses relative to placebo with respect to subjective alertness levels (Bond and Lader visual analog scale; Figure 3a). With respect to mean reaction time (Figure 3b), there was a small increase after almorexant 400 mg only (mean treatment effect 34.7 ms (95% confidence interval 4.9–64.5 ms)). Almorexant had no effect on the scores in the fine-motor test (data not shown); in the digit span test, a lower forward score was observed for almorexant 200 mg as compared with placebo (mean treatment effect –0.41 (95% confidence interval –0.80 to –0.01)) (data not shown).
Figure 3.
Treatment effects of almorexant on next-day alertness and performance (reaction time test). Mean changes relative to placebo with 95% CIs. CI, confidence interval; VAS, visual analog scale.
Safety
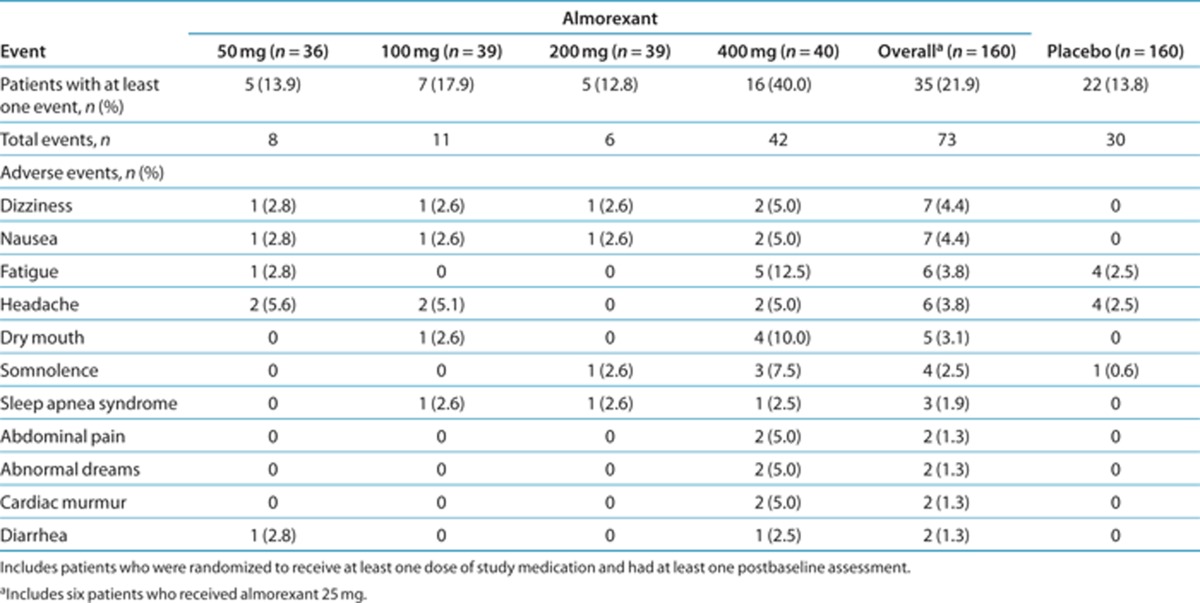
Overall, a larger proportion of patients reported at least one AE after almorexant administration than after placebo (21.9% vs. 13.8%). Dizziness, nausea, fatigue, headache, and dry mouth were the most common AEs reported after almorexant treatment (Table 4). The proportion of patients with one or more AE was highest after almorexant 400 mg (40.0%) but was markedly lower after doses of 200, 100, and 50 mg (12.8, 17.9, and 13.9%, respectively). There was one serious AE (vasovagal syncope after placebo treatment) and no deaths. Other than the serious event, all AEs were of mild or moderate severity. One patient discontinued the study because of a febrile upper respiratory tract infection after receiving almorexant 400 mg (unrelated to study treatment); another discontinued because of the aforementioned serious AE. No treatment-related changes in laboratory parameters, vital signs, or quantitative electrocardiogram variables were observed, nor did any electrocardiogram abnormalities develop. No narcolepsy or cataplexy events were reported, and no trend or dose relationship was detected by the narcoleptic effects questionnaire.
Table 4. Adverse events (safety population) occurring at least once in the overall almorexant group or the placebo group (includes related and unrelated events).
Discussion
This is the first study to suggest that the orexin system may play a role in nocturnal sleep regulation in humans and that orexin receptor antagonism results in sleep-enabling effects in patients with primary insomnia. It extends and confirms previous preclinical and clinical observations.20,21 In this two-part clinical study in patients with primary insomnia, a significant and clinically relevant increase in SE was observed after almorexant 400 mg, and the lowest effective dose was 100 mg. Almorexant 400 mg significantly improved sleep initiation as assessed by LPS, and at doses ≥100 mg almorexant dose-dependently and significantly decreased WASO, a measure of sleep maintenance. Almorexant decreased latency to REM sleep in a dose-dependent manner and decreased latencies to S1–S4 sleep stages at the higher doses, while increasing TST. The drug reduced the time spent in S1 and increased the time spent in REM sleep. At all doses ≥100 mg, it had similar effects on the percentages of TST spent in the S1 and REM sleep stages. The increase in time spent in REM sleep brought the percentage of TST spent in REM to approximately within the normal range, generally 20–25% in normal young adults43 and decreasing with age to 18% in men and 19% in women (age range 61–70 years).44 These results indicate that the administration of an almorexant dose as low as 100 mg caused an increase in the TST during the night, mainly by improving sleep maintenance. This dose level administered in the daytime did not result in detectable impairment of vigilance, alertness, or visuomotor and motor coordination in healthy subjects.21
Consistent effects were generally observed between objective and subjective assessments of sleep variables, particularly with respect to SE, TST, and LPS, although differences were apparent at the lower almorexant doses. The drug had no effect on subjective WASO at any dose, although objective WASO decreased dose-dependently and patients reported improved sleep quality. This absence of an effect on subjective WASO warrants further investigation in future studies using other sleep-diary assessments. With respect to all the objective sleep variables, improvements were observed in the mean values from the night of screening/adaptation to that after placebo treatment. This may be due to an improvement in the patients' comfort with the equipment and sleep laboratory procedures.
Two residual effects on next-day performance, namely, increased mean reaction time and a lower forward score on the digit span test, were detected in association with the higher almorexant doses (400 and 200 mg, respectively). Given that the major goal for insomnia therapies is to improve sleep maintenance without affecting next-day performance, further investigation of any potential next-day effects after almorexant treatment at the therapeutic dose would be valuable. Of the current standard pharmacologic treatments used for sleep maintenance indications, benzodiazepines are associated with next-day effects; however, nonbenzodiazepine agents such as eszopiclone and controlled-release zolpidem cause minimal or no residual daytime effects.35,39,40,45
The safety profile of almorexant was similar to that of placebo for the lower doses, and an increase in the incidence of AEs was evident only for the 400-mg dose. There was no evidence of narcolepsy or cataplexy as seen from AE reporting and the narcoleptic effects questionnaire. The decrease in latencies to REM after almorexant administration deserves further attention and should be studied in larger trials at the therapeutic doses. Shortened REM latency could potentially point to narcolepsy-like changes in sleep architecture or potential direct effects of dual orexin receptor antagonists on sleep; alternatively, it could indicate REM rebound in individuals susceptible to chronic partial REM deprivation.
The strengths of this study include the trial design, which involved the initial administration of a high dose of almorexant followed by decreasing doses in subsequent stages. This design allowed the efficacy of almorexant at a high dose to be established first before determining the lowest effective dose. Limitations of the study include the shortness of the treatment duration from which to assess the efficacy, safety, and tolerability of almorexant. The sleep-enabling and -maintaining effects and long-term safety and tolerability of dual orexin receptor antagonist treatment need to be assessed in large, long-term, randomized trials. This step is essential for new insomnia therapies because long-term use of current pharmacologic treatments can be associated with the development of tolerance and dependence, and with rebound insomnia on their withdrawal.22,46,47 The clinical development of almorexant was discontinued in January 2011 for reasons not related to any of the observations in our study.48
In conclusion, in this study, a single dose of the dual orexin receptor antagonist almorexant enabled initiation and maintenance of sleep in patients with primary insomnia. Almorexant treatment was associated with a dose-dependent improvement in SE, strongly suggesting that the endogenous orexin system plays an important role in the sleep–wake cycle. Consistent improvements were observed in sleep time, initiation, and maintenance, and in the patients' perception of sleep. Small effects on next-day performance were observed only after the higher almorexant doses. No safety concerns were revealed. Overall, dual orexin receptor antagonism may offer a potential new treatment approach for primary insomnia.
Methods
Study design. This was a prospective, multicenter, multistage, double-blind, randomized, placebo-controlled, two-way crossover, single-dose study involving almorexant in patients with primary insomnia. The study was conducted at 20 centers across Europe and Israel (6 in Germany; 3 in Austria; 2 each in Finland, Sweden, and Switzerland; and 1 each in Denmark, Israel, the Netherlands, Spain, and the United Kingdom). The study design incorporated two parts: a first part to determine the efficacy of almorexant at a high dose followed by a second part with dose-descending stages to establish the minimum effective dose. In the first part of the study, the patients received a single dose of 400 mg oral almorexant and a placebo on different treatment nights 1 week apart, in a crossover design. The patients were allocated in a 1:1 ratio to the two treatment sequences (placebo/almorexant and almorexant/placebo) on the first treatment night, using a computer-generated randomization list. The study treatments were indistinguishable with respect to packaging, appearance, and number of capsules administered. The duration of the washout period and the timing of study drug administration were based on pharmacodynamic and pharmacokinetic data from a previous ascending single-dose study of almorexant in healthy subjects. Almorexant was rapidly absorbed, with a median time to maximum concentration ranging from 0.7 to 2.3 h and rapid decreases to ~20% of peak plasma concentrations over the course of 8 h after time to maximum concentration.21 The pharmacodynamics of the drug correlated well with the concentration levels and, in general, the onset of pharmacodynamic effects was observed within 1 h after the dose.21
If the primary end point treatment effect was found to be significant (P < 0.05), the study continued with the next lower dose (200, 100, 50, or 25 mg) in new patients sequentially until the treatment effect was no longer statistically significant. When the number of patients successfully screened reached the target sample size for a dose level, subsequent patients were assigned to the next dose level. Therefore some patients entered the next dose level before the outcome for the previous dose was known. After study enrollment was completed, all the patients were scheduled to complete all periods and assessments. If the primary end point was not significant at 400 mg, 1,000 mg was to be tested against placebo in new patients. For each dose level, patients underwent a screening period (up to 4 weeks), first treatment night, 1-week washout period, second treatment night, and 28-day post-treatment follow-up. Patients were required to complete a daily sleep log for at least 1 week before the screening/adaptation night, 1 week before the first treatment night, and during the 1-week washout period before the second treatment night. The sleep log consisted of a “day questionnaire” and the self-rating sleep and awakening quality questionnaire (SSA).49 The “day questionnaire” assessed the patient's daily habits regarding meals, caffeine-containing beverages, alcoholic drinks, smoking, nonstudy medication, and naps. In addition, information on the patient's well-being, physical and emotional stress, and expected stressful events was collected. The investigator reviewed the sleep log and assessed the patient's well-being and compliance before each polysomnography recording. Polysomnography was performed for 8 h overnight during the screening/adaptation night and each treatment night. The purpose of the screening/adaptation night was to objectively confirm the subjectively patient-reported pattern of sleep disturbances relating to TST and sleep onset latency. The screening/adaptation night also served to accustom the patient to the sleep laboratory, the polysomnography equipment, and the psychometric tests. All polysomnography results were analyzed in accordance with the rules of Rechtschaffen and Kales, using the validated Somnolyzer 24 × 7 scoring tool50,51,52 and including a structured expert review. Sleep was scored in 30-s epochs. During treatment nights, a single dose of almorexant or placebo was administered 30 min before the start of the polysomnography. The patients were required to remain at the center the morning following the polysomnography until they were free of symptoms possibly related to sleep-enabling medication, as judged by the physician responsible.
Patients. Male and female patients 18–65 years of age were eligible for inclusion if they had primary insomnia (by the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition—Text Revision) and a history (≥3 months) of subjectively reported usual TST of 3–6 h, usual sleep disturbance with a subjective sleep onset latency of >30 min, and daytime complaints associated with poor sleep. Other inclusion criteria were polysomnographic confirmation of TST of <6 h and LPS ≥20 min during the screening/adaptation night; a body mass index of 18–30 kg/m2; no clinically relevant abnormalities as shown by a 12-lead electrocardiogram and by hematology/biochemistry test results; willingness to refrain from central nervous system-active drugs for five half-lives of the drug (at least 1 week); and a negative urine test for barbiturates, cannabinoids, amphetamines, and cocaine. Psychotropic drugs were not permitted, except hypnotics with a short half-life of ≤10 h taken ≥48 h before each treatment night; other stable medications were allowed. Cytochrome P450 isoenzyme 3A4 inhibitors were not permitted within 1 week before screening. Key exclusion criteria included major depressive disorder, severe psychosis, or significant anxiety disorder; a score >2 on the symptom assessment questionnaire for diagnosis of apnea,53 a raw score ≥50 on the Zung Self-Rating Depression or Anxiety Scale;54,55 and restless legs syndrome or insomnia associated with or caused by sleep apnea or periodic limb movement disorder, as assessed by polysomnography during the screening night (defined as apnea/hypopnea index >10/h or periodic limb movement arousal index >10/h, respectively). Caffeine consumption of >7 U/ day was not permitted on a regular basis (one unit of caffeine was defined as one cup of coffee or two cups of tea). Pregnancy and lactation were also exclusion criteria. Women with childbearing potential were administered urine pregnancy tests at predefined time points during the study and were required to use a reliable method of contraception during the entire study duration and for at least 3 months after intake of the study drug.
Study end points. The primary end point was SE as determined by polysomnography, where SE (%) = (TST in minutes/total time in bed in minutes (fixed to 480 min)) × 100. Secondary end points, determined by polysomnography, were LPS (the time in minutes from the start of recording to the beginning of the first 20 nonwake epochs) and WASO (the time in minutes spent awake after sleep onset until the end of the recording, where sleep onset is the time of the first occurrence of three consecutive epochs in S1 or first occurrence of S2). Exploratory end points measured by polysomnography included TST (the amount of actual sleep time in minutes in the total sleep period), latency to sleep stages (the time in minutes from the start of the polysomnography recording to the first occurrence of the respective sleep stage) including REM sleep (the time in minutes from sleep onset to the first occurrence of REM), and time spent (in minutes) and percentage of TST for each of the sleep stages; and subjective measures of SE, sleep latency, WASO, TST, and sleep quality, assessed using the SSA. Next-day performance and alertness after treatment nights were assessed using the Bond and Lader visual analog scale, which assesses 16 subjective feelings;56 fine-motor testing, reaction time testing;57,58 and both forward and backward digit span testing.59
Safety assessments. AEs and serious AEs occurring within 36 h of administration of study treatment were recorded, irrespective of whether they were considered to be related to the study treatment. Any AE that continued for 24 h after the last drug intake was monitored for up to 28 days. Clinical laboratory tests, vital signs, 12-lead electrocardiogram, and a subjective narcoleptic effects questionnaire were assessed the morning after study drug administration. The narcoleptic effects questionnaire was specifically designed for this study; it evaluated symptoms of cataplexy and sleep paralysis seen in narcolepsy with a series of yes/no questions on muscle relaxation/weakness and dreams.
Statistical analysis. This dose-ranging study was powered to detect a placebo-corrected mean difference in SE of 6.5%. SE was assumed to be normally distributed, with a standard deviation of 9.8%; no period or carryover effects were expected. The desired power for each dose level (1,000, 400, 200, 100, 50, and 25 mg) was 98%, 98%, 96%, 94%, 94%, and 94%, requiring 39, 39, 34, 31, 31, and 31 patients, respectively. This approach was used to maximize the power for the first dose tested (400 mg) and to have ≥80% actual power at the 50 mg dose level. By this calculation, a minimum of 78 patients (400 and 1,000 mg dose levels) and a maximum of 166 patients (400, 200, 100, 50, and 25 mg dose levels) were required for the study. The null hypothesis of no difference between each dose and placebo was tested using a two-sided paired t-test on the per-protocol analysis set, and rejected when P < 0.05. If the null hypothesis was rejected, secondary end points were to be sequentially tested (i.e., first LPS, then WASO) using a two-sided paired t-test. Robustness analyses of the primary and secondary end points included the Wilcoxon signed-rank test, and analysis of the all-treated set using all available data. For the primary end point, carryover and period effects were investigated using mixed modeling. If the carryover effect was significant (at the α = 0.10 level), statistical analysis of only the first period was carried out. Exploratory end points were analyzed in the same manner as the main analysis of the primary end point, but any statistical inferences had no confirmatory value. Statistical analyses were performed using SAS software version 8.2 (SAS Institute, Cary, NC). Safety end points were analyzed descriptively.
Study oversight. All materials were reviewed and approved by the appropriate independent ethics committees before the study began. The study was conducted in accordance with the Declaration of Helsinki, followed the International Conference on Harmonization Guidelines for Good Clinical Practice, and was registered at ClinicalTrials.gov (NCT00640848). Written informed consent was obtained from each patient before any study procedure and after adequate explanation of the aims, methods, objectives, and potential hazards of the study. It was made clear to each patient that he or she was completely free to refuse to enter the study or to withdraw from it at any time for any reason. Data were collected by the investigators and analyzed by the sponsor. The authors had access to the data, and they vouch for the accuracy and completeness of the data.
Author Contributions
P.H. wrote the manuscript, designed research, and analyzed data. G.D. wrote the manuscript, designed research, analyzed data, and contributed new reagents/analytical tools. H. Beneš. performed research. T.P. performed research. H.D.-H. wrote the manuscript, performed research, and contributed new reagents/analytical tools. M.J.B. wrote the manuscript and performed research. G.P. performed research and analyzed data. B.S. designed and performed research. O.P. performed research and analyzed data. D.K. wrote the manuscript and performed research. J.Z. wrote the manuscript and performed research. S.B. performed research. M.P. wrote the manuscript and performed research. C.L.B. performed research. B.H. wrote the manuscript and performed research. I.O.E. performed research. E.H.-T. performed research. H. Bengtsson performed research. Y.P. performed research. U.-M.H. performed research. E.C. designed and performed research, and analyzed data. G.H. designed and performed research, and analyzed data. J.D. wrote the manuscript, designed research, and analyzed data.
Acknowledgments
This study was sponsored by Actelion Pharmaceuticals Ltd, Switzerland. The sponsor supplied the study treatment capsules and analyzed the data. Actelion Pharmaceuticals provided payments to investigators or their institutions to perform the study and paid for travel and/or accommodation expenses for investigators to attend meetings related to the study. The authors received medical writing support from Gail Rickard (Medi Cine International, UK), sponsored by Actelion Pharmaceuticals. Data from this study were previously presented in poster and oral presentations at the 5th World Sleep Congress in 2007.60
P.H., E.C., and J.D. were full-time employees of, and own stock options in, Actelion Pharmaceuticals Ltd. All the other authors were investigators of the study, and payments were received either by them or by their institutions from Actelion Pharmaceuticals for performing the study and for travel and/or accommodation expenses for investigator meetings related to the study. The Siesta Group Schlafanalyse, Vienna, Austria, was paid by Actelion Pharmaceuticals for data analysis. The following authors report disclosures for activities unrelated to the submitted work: G.D. is the chief executive officer of the Siesta Group Schlafanalyse and is also employed by Philips Respironics; he owns stock options in the Siesta Group and has been paid for his expert testimony by the Gerson Lehrmann Group. G.D.'s institution has received grants from Philips Respironics, and the Siesta Group provides analysis services to several pharmaceutical companies. H. Beneš. has received honoraria from GSK, Boehringer Ingelheim, Cephalon, and UCB for educational lectures and advisory board meetings. T.P. has received financial support from several pharmaceutical companies for attending conferences and advisory board meetings, and his institution has received grants from the European Union and German National Funds. H.D.-H. has received consultancy fees from PAREXEL International and refund of travel expenses incurred for activities supported by GSK, MSD, Sanofi-Synthelabo, and UCB; her institution has received grants from Actelion Pharmaceuticals, GSK, MSD, Bioprojet, and PAREXEL International. G.P. has received payments from Actelion Pharmaceuticals for expenses relating to his position as a steering committee member of a separate study. B.S. has received research support from Abiogen Pharma, Actelion Pharmaceuticals, AstraZeneca, Cephalon, GlaxoSmithKline, Sanofi-Aventis, Schwarz Pharma, Servier, and Takeda. He has received honoraria (not exceeding US$10,000/year) for serving on scientific advisory boards of Nycomed, Servier, Takeda, UCB, and Sanofi-Aventis; for being a consultant for Merck and Xenoport; and for being a speaker for AstraZeneca, Cephalon, Ixico, Janssen, and Lundbeck. He is a shareholder of the Siesta Group Schlafanalyse. O.P. has received consultancy fees from Orion Pharma, MSD, Pfizer, and Actelion Pharmaceuticals, and payment from Boehringer Ingelheim, Pfizer, GSK, AstraZeneca, and Maribo Medical for lectures; he owns stocks in Unesta, which provides services for several pharmaceutical companies. M.P. has received consultancy fees from Cephalon, Leiras-Nycomed, Sanofi-Aventis, Servier, and UCB, and payment from Boehringer Ingelheim, GSK, Leiras, Servier, and UCB for lectures; his institution has received grants from the Academy of Finland and the Parkinson Foundation. C.L.B. has received payments from UCB, Pfizer, Boehringer Ingelheim, Bioprojet, Lundbeck, and Actelion Pharmaceuticals for advisory board membership, and from UCB, Pfizer, Lundbeck, Bioprojet, Boehringer Ingelheim, and Novartis for lectures; his institution has received grants from UCB, Pfizer, ResMed, and Respironics, and payment from Pfizer for the development of educational presentations. B.H. has received consultancy fees from UCB, Boehringer Ingelheim, GSK, Pfizer, and Jazz Pharmaceuticals; payments from UCB, Boehringer Ingelheim, GSK, Cephalon, and Sanofi for lectures; and royalties from CUP. Her institution has received grants from UCB. Y.P. has received payments from ResMed, Roche, and AstraZeneca for lectures, and his institution has received grants from the Swedish Heart and Lung Foundation and other national and local foundations as well as from ResMed, ResMed Foundation, Pfizer, Boehringer Ingelheim, and Actelion Pharmaceuticals. U.-M.H. has received payment for serving on advisory boards of Eli Lilly, Bristol-Myers Squibb, and Pfizer. G.H. has received consultancy fees, payments for advisory board membership and participation in speaker boards, and research funding from Actelion Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Cephalon, Daimler Benz, Eli Lilly, EuMeCom, Essex Pharma, Gerson Lerman Group Council of Healthcare Advisors, GSK, Janssen-Cilag, Lundbeck, McKinsey, MedaCorp, Merck, Network of Advisors, Novartis, Organon, Pfizer, Sanofi-Aventis, Schering-Plough, Sepracor, Takeda, Transcept Pharmaceuticals, UCB, Volkswagen, Weinmann, and Wyeth. D.K., J.Z., S.B., I.O.E., E.H.-T., and H. Bengtsson have no financial disclosures or potential conflicts of interest to report. M.J.B. is deceased and therefore no disclosures are reported for this author.
Footnotes
SUPPLEMENTARY MATERIAL is linked to the online version of the paper at http://www.nature.com/cpt
Supplementary Material
References
- Harris G.C., Wimmer M., &, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature. 2005;437:556–559. doi: 10.1038/nature04071. [DOI] [PubMed] [Google Scholar]
- Sakurai T. Roles of orexins and orexin receptors in central regulation of feeding behavior and energy homeostasis. CNS Neurol. Disord. Drug Targets. 2006;5:313–325. doi: 10.2174/187152706777452218. [DOI] [PubMed] [Google Scholar]
- Anaclet C.et al. Orexin/hypocretin and histamine: distinct roles in the control of wakefulness demonstrated using knock-out mouse models J. Neurosci 2914423–14438.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotz C.M.et al. Orexin A mediation of time spent moving in rats: neural mechanisms Neuroscience 14229–36.2006 [DOI] [PubMed] [Google Scholar]
- Siegel J.M. Hypocretin (orexin): role in normal behavior and neuropathology. Annu. Rev. Psychol. 2004;55:125–148. doi: 10.1146/annurev.psych.55.090902.141545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan J.J.et al. Orexin A activates locus coeruleus cell firing and increases arousal in the rat Proc. Natl. Acad. Sci. USA 9610911–10916.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai T. The neural circuit of orexin (hypocretin): maintaining sleep and wakefulness. Nat. Rev. Neurosci. 2007;8:171–181. doi: 10.1038/nrn2092. [DOI] [PubMed] [Google Scholar]
- de Lecea L.et al. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity Proc. Natl. Acad. Sci. USA 95322–327.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mignot E.et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias Arch. Neurol 591553–1562.2002 [DOI] [PubMed] [Google Scholar]
- Sakurai T.et al. Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior Cell 92573–585.1998 [DOI] [PubMed] [Google Scholar]
- Kiyashchenko L.I.et al. Release of hypocretin (orexin) during waking and sleep states J. Neurosci 225282–5286.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M.G., Hassani O.K., &, Jones B.E. Discharge of identified orexin/hypocretin neurons across the sleep-waking cycle. J. Neurosci. 2005;25:6716–6720. doi: 10.1523/JNEUROSCI.1887-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon R.M.et al. Diurnal variation of cerebrospinal fluid hypocretin-1 (Orexin-A) levels in control and depressed subjects Biol. Psychiatry 5496–104.2003 [DOI] [PubMed] [Google Scholar]
- Chemelli R.M.et al. Narcolepsy in orexin knockout mice: molecular genetics of sleep regulation Cell 98437–451.1999 [DOI] [PubMed] [Google Scholar]
- Lin L.et al. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene Cell 98365–376.1999 [DOI] [PubMed] [Google Scholar]
- Mieda M., Willie J.T., Hara J., Sinton C.M., Sakurai T., &, Yanagisawa M. Orexin peptides prevent cataplexy and improve wakefulness in an orexin neuron-ablated model of narcolepsy in mice. Proc. Natl. Acad. Sci. USA. 2004;101:4649–4654. doi: 10.1073/pnas.0400590101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann C.R., &, Bassetti C.L. Hypocretins (orexins) and sleep-wake disorders. Lancet Neurol. 2005;4:673–682. doi: 10.1016/S1474-4422(05)70196-4. [DOI] [PubMed] [Google Scholar]
- Peyron C.et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains Nat. Med 6991–997.2000 [DOI] [PubMed] [Google Scholar]
- Dugovic C.et al. Blockade of orexin-1 receptors attenuates orexin-2 receptor antagonism-induced sleep promotion in the rat J. Pharmacol. Exp. Ther 330142–151.2009 [DOI] [PubMed] [Google Scholar]
- Brisbare-Roch C.et al. Promotion of sleep by targeting the orexin system in rats, dogs and humans Nat. Med 13150–155.2007 [DOI] [PubMed] [Google Scholar]
- Hoever P.et al. Orexin receptor antagonism, a new sleep-promoting paradigm: an ascending single-dose study with almorexant Clin. Pharmacol. Ther 87593–600.2010 [DOI] [PubMed] [Google Scholar]
- Hilty D., Young J.S., Bourgeois J.A., Klein S., &, Hardin K.A. Algorithms for the assessment and management of insomnia in primary care. Patient Prefer. Adherence. 2009;3:9–20. doi: 10.2147/ppa.s2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health NIH State of the Science Conference statement on manifestations and management of chronic insomnia in adults. Sleep. 2005;28:1049–1057. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- Partinen M, Hublin C.Epidemiology of sleep disorders Principles and Practice of Sleep Medicineeds. Kryger M.H., and, Dement W.626–647.Elsevier, New York; 2005 [Google Scholar]
- Roth T., &, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin. Cornerstone. 2003;5:5–15. doi: 10.1016/s1098-3597(03)90031-7. [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. 2002 Sleep in America Poll < < http://www.sleepfoundation.org/sites/default/files/2002SleepInAmericaPoll.pdf > ( 2002
- Ohayon M.M. Nocturnal awakenings and comorbid disorders in the American general population. J. Psychiatr. Res. 2008;43:48–54. doi: 10.1016/j.jpsychires.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Schutte-Rodin S., Broch L., Buysse D., Dorsey C., &, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J. Clin. Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- Roth T. Prevalence, associated risks, and treatment patterns of insomnia. J. Clin. Psychiatry. 2005;66 (suppl. 9:10–13; quiz 42. [PubMed] [Google Scholar]
- Allen R.P., Mendels J., Nevins D.B., Chernik D.A., &, Hoddes E. Efficacy without tolerance or rebound insomnia for midazolam and temazepam after use for one to three months. J. Clin. Pharmacol. 1987;27:768–775. doi: 10.1002/j.1552-4604.1987.tb02994.x. [DOI] [PubMed] [Google Scholar]
- Holbrook A., Crowther R., Lotter A., &, Endeshaw Y. The role of benzodiazepines in the treatment of insomnia: meta-analysis of benzodiazepine use in the treatment of insomnia. J. Am. Geriatr. Soc. 2001;49:824–826. doi: 10.1046/j.1532-5415.2001.49161.x. [DOI] [PubMed] [Google Scholar]
- Scharf M.B., Roth P.B., Dominguez R.A., &, Ware J.C. Estazolam and flurazepam: a multicenter, placebo-controlled comparative study in outpatients with insomnia. J. Clin. Pharmacol. 1990;30:461–467. doi: 10.1002/j.1552-4604.1990.tb03486.x. [DOI] [PubMed] [Google Scholar]
- Dündar Y., Dodd S., Strobl J., Boland A., Dickson R., &, Walley T. Comparative efficacy of newer hypnotic drugs for the short-term management of insomnia: a systematic review and meta-analysis. Hum. Psychopharmacol. 2004;19:305–322. doi: 10.1002/hup.594. [DOI] [PubMed] [Google Scholar]
- Hajak G.et al. Rebound insomnia after hypnotic withdrawal in insomniac outpatients Eur. Arch. Psychiatry Clin. Neurosci 248148–156.1998 [DOI] [PubMed] [Google Scholar]
- Lieberman J.A. Update on the safety considerations in the management of insomnia with hypnotics: incorporating modified-release formulations into primary care. Prim. Care Companion J. Clin. Psychiatry. 2007;9:25–31. doi: 10.4088/pcc.v09n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscemi N.et al. The efficacy and safety of drug treatments for chronic insomnia in adults: a meta-analysis of RCTs J. Gen. Intern. Med 221335–1350.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit G., Erman M., Wang-Weigand S., Sainati S., Zhang J., &, Roth T. Evaluation of the efficacy and safety of ramelteon in subjects with chronic insomnia. J. Clin. Sleep Med. 2007;3:495–504. [PMC free article] [PubMed] [Google Scholar]
- Erman M.K.et al. A polysomnographic placebo-controlled evaluation of the efficacy and safety of eszopiclone relative to placebo and zolpidem in the treatment of primary insomnia J. Clin. Sleep Med 4229–234.2008 [PMC free article] [PubMed] [Google Scholar]
- Roth T., Soubrane C., Titeux L., &, Walsh J.K., Zoladult Study Group Efficacy and safety of zolpidem-MR: a double-blind, placebo-controlled study in adults with primary insomnia. Sleep Med. 2006;7:397–406. doi: 10.1016/j.sleep.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Zammit G. Comparative tolerability of newer agents for insomnia. Drug Saf. 2009;32:735–748. doi: 10.2165/11312920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Eriksson K.S., Sergeeva O.A., Haas H.L., &, Selbach O. Orexins/hypocretins and aminergic systems. Acta Physiol. (Oxf) 2010;198:263–275. doi: 10.1111/j.1748-1716.2009.02015.x. [DOI] [PubMed] [Google Scholar]
- Rosenberg R.P. Sleep maintenance insomnia: strengths and weaknesses of current pharmacologic therapies. Ann. Clin. Psychiatry. 2006;18:49–56. doi: 10.1080/10401230500464711. [DOI] [PubMed] [Google Scholar]
- Carskadon M, Dement W.Normal Human Sleep: An Overview4th edn. (ElsevierSaunders, Philadelphia, PA; 2005 [Google Scholar]
- Redline S., Kirchner H.L., Quan S.F., Gottlieb D.J., Kapur V., &, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch. Intern. Med. 2004;164:406–418. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- Zammit G.K., McNabb L.J., Caron J., Amato D.A., &, Roth T. Efficacy and safety of eszopiclone across 6-weeks of treatment for primary insomnia. Curr. Med. Res. Opin. 2004;20:1979–1991. doi: 10.1185/174234304x15174. [DOI] [PubMed] [Google Scholar]
- Griffiths R.R., &, Johnson M.W. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J. Clin. Psychiatry. 2005;66 (suppl. 9:31–41. [PubMed] [Google Scholar]
- Soldatos C.R., Dikeos D.G., &, Whitehead A. Tolerance and rebound insomnia with rapidly eliminated hypnotics: a meta-analysis of sleep laboratory studies. Int. Clin. Psychopharmacol. 1999;14:287–303. [PubMed] [Google Scholar]
- Actelion/GlaxoSmithKline. Actelion and GSK Discontinue Clinical Development of Almorexant < < http://www.actelion.com/en/investors/ media-releases/index.page?newsId=1483135 >. Accessed 28 January 2011.
- Saletu B., Kindshofer G., Anderer P., &, Grünberger J. Short-term sleep laboratory studies with cinolazepam in situational insomnia induced by traffic noise. Int. J. Clin. Pharmacol. Res. 1987;7:407–418. [PubMed] [Google Scholar]
- Anderer P.et al. An E-health solution for automatic sleep classification according to Rechtschaffen and Kales: validation study of the Somnolyzer 24 x 7 utilizing the Siesta database Neuropsychobiology 51115–133.2005 [DOI] [PubMed] [Google Scholar]
- Penzel T.et al. Digital analysis and technical specifications J. Clin. Sleep Med 3109–120.2007 [PubMed] [Google Scholar]
- Svetnik V.et al. Evaluation of automated and semi-automated scoring of polysomnographic recordings from a clinical trial using zolpidem in the treatment of insomnia Sleep 301562–1574.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ploch T., Kemeny C., Gilbert G., Cassel W., &, Peter J.H. Significance of a screening questionnaire for diagnosis of sleep apnea] Pneumologie. 1993;47 (suppl. 1:108–111. [PubMed] [Google Scholar]
- Zung W.W. A self-rating depression scale. Arch. Gen. Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- Zung W.W. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- Bond A, Lader M. The use of analogue scales in rating subjective feelings. Br. J. Med. Psychol. 1974;47:211–218. [Google Scholar]
- Gruenberger J. Maudrich, Vienna, Austria; 1977. Psychodiagnostik des Alkoholkranken. Ein methodischer Beitrag zur Bestimmung der Organizitaet in der Psychiatrie. [Google Scholar]
- Grünberger J., Linzmayer L., Dietzel M., &, Saletu B. The effect of biologically-active light on the noo- and thymopsyche and on psychophysiological variables in healthy volunteers. Int. J. Psychophysiol. 1993;15:27–37. doi: 10.1016/0167-8760(93)90092-4. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Psychological, New York; 1995. Manual for the Wechsler Adult Intelligence Scale. [Google Scholar]
- Dingemanse J.et al. Proof-of-concept study in primary insomnia patients with ACT-078573, a dual orexin receptor antagonist Sleep Biol. Rhythms 5suppl. s1), A194 (2007 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.