Abstract
Objective
To report on remission rates in anxious youth who participated in the Child/Adolescent Anxiety Multimodal Study (CAMS). The CAMS, a multisite clinical trial, randomized 488 children and adolescents (ages 7–17 years; 79% Caucasian; 50% female) with separation, social, and/or generalized anxiety disorder to a 12-week treatment of sertraline (SRT), cognitive behavioral therapy (CBT), their combination (COMB), or clinical management with pill placebo (PBO).
Method
The primary definition of remission was loss of all study-entry anxiety disorder diagnoses; additional definitions of remission were used. All outcomes were rated by independent evaluators blind to treatment assignment. Predictors of remission were also examined.
Results
Remission rates after 12 weeks of treatment ranged from 46% to 68% for COMB, 34% to 46% for SRT, 20% to 46% for CBT, and 15% to 27% for PBO. Rates of remission (i.e., achieving a nearly symptom-free state) were significantly lower than rates of response (i.e., achieving a clinically meaningful improvement relative to baseline) for the entire sample. Youth who received COMB had significantly higher rates of remission compared to all other treatment groups. Both monotherapies had higher remission rates compared to PBO, but rates were not different from each other. Predictors of remission were younger age, nonminority status, lower baseline anxiety severity, absence of other internalizing disorders (e.g., anxiety, depression), and absence of social phobia.
Conclusions
For the majority of children, some symptoms of anxiety persisted, even among those showing improvement after 12 weeks of treatment, suggesting a need to augment or extend current treatments for some children.
Keywords: anxiety, children, adolescents, treatment, remission
An index of outcome in randomized controlled trials (RCTs) for pediatric anxiety disorders (ADs) is the response rate. Response has been defined as a meaningful improvement in symptoms. An important question for clinicians, patients, and families is, what are the chances of becoming nearly symptom free? That is, what is the chance for remission? Although there is no consensus on an operational definition of remission for childhood ADs, it is defined generally as the absence or near absence of symptoms following treatment for a predetermined period of time (Frank et al., 1991). It is considered a more stringent criterion than response. Identifying remission rates in RCTs is thus an important index of treatment outcome.
Reports of remission rates after acute treatment for pediatric ADs are sparse, though initial studies reveal that remission rates are typically lower than response rates. Hudson et al. (2009) reported that posttreatment response rates (defined as the percentage of children no longer meeting criteria for their principal anxiety diagnosis) were 45% after 10 weeks of CBT; the remission rate (percentage no longer meeting criteria for any AD) was 33%. Data on remission rates are similarly sparse for pharmacotherapy trials, although they show a similar pattern. Wagner et al. (2004) reported a 78% response rate (defined as a Clinical Global Impression Improvement Scale [CGI-I] score of 1 [very much improved] or 2 [much improved]) after 16 weeks of paroxetine for youth with social phobia (SOP) and a remission rate (defined as a CGI-I of 1 or a 70% or greater reduction on a social anxiety scale) of 48% and 47%, respectively.
Despite similar patterns of response and remission rates in both pharmacotherapy and cognitive behavioral therapy (CBT) trials for pediatric anxiety, variations in definitions and measurement methods undermine comparisons. The recent Child/Adolescent Anxiety Multimodal Treatment Study (CAMS; Walkup et al., 2008), which compared the efficacy of CBT (Coping Cat; Kendall & Hedtke, 2006), pharmacotherapy (sertraline [SRT]), and their combination (COMB) to pill placebo (PBO) in 488 youth with separation AD (SAD), generalized AD (GAD), and SOP, measured treatment outcome using a variety of methods. Thus, data from this trial are uniquely suited to describe remission rates (i.e., achieving a nearly symptom-free state) conferred by CBT, SRT, and COMB. The initial findings from the CAMS reported only on response rates (Walkup et al., 2008). This study (a) determined multiply defined posttreatment remission rates by treatment condition and (b) assessed predictors of remission.
Method
Participants
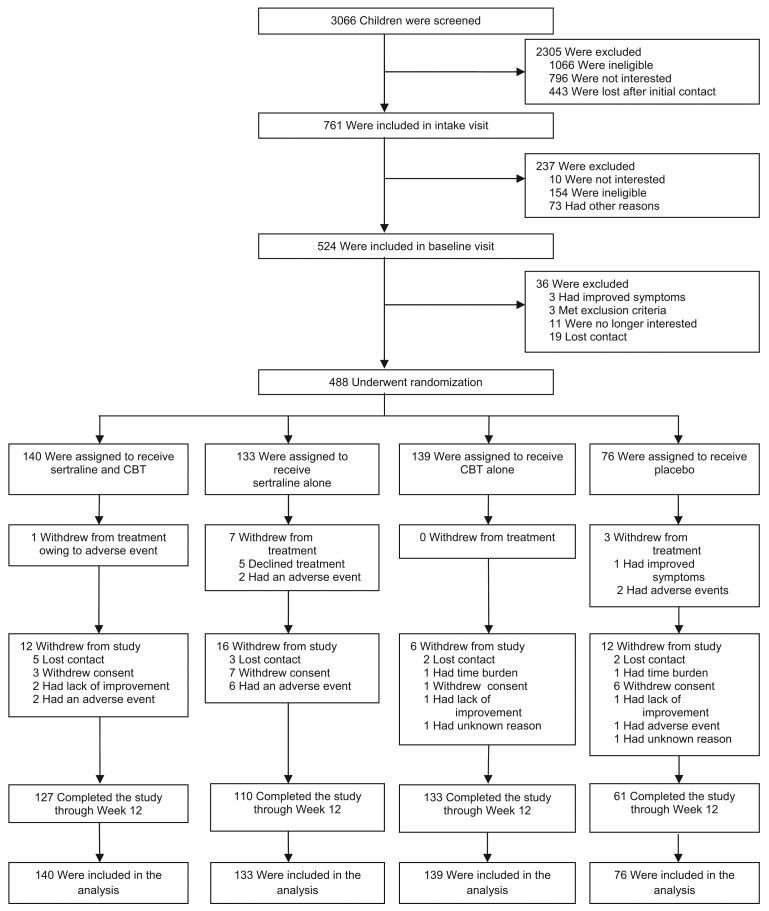
The sample was comprised of 488 children and adolescents (ages 7–17 years) who met Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association, 1994) criteria for GAD, SOP, and/or SAD. Detailed demographic and diagnostic characteristics were described in Kendall et al. (2010) and Walkup et al. (2008). Participants were randomized to treatment conditions as follows: COMB (n = 140), SRT (n = 133), CBT (n = 139), and PBO (n = 76). See Figure 1 for CONSORT diagram.
Figure 1.
Flow diagram of Child/Adolescent Anxiety Multimodal Study. Subjects who are shown as having withdrawn from treatment discontinued their assigned therapy but continued to undergo study assessment. Subjects who are shown as having withdrawn from the study discontinued both therapy and assessment. CBT = cognitive behavioral therapy.
Measures
Outcomes were assessed by an independent evaluator blind to treatment group at the end of 12 weeks of treatment. Measures and definitions of remission were as follows:
Loss of all targeted ADs (i.e., GAD, SOP, SAD) as assessed via the Anxiety Disorders Interview Schedule (ADIS-C/P; Silverman & Albano, 1996). The composite diagnosis (i.e., based on child and parent interviews) was used to determine all diagnoses.
Clinical Global Impression Severity Scale (CGI-S; Guy, 1976) score of 1 or 2. The CGI-S is a global rating of anxiety severity ranging from 1 (not at all ill) to 7 (extremely ill). A score of 1 or 2 reflects no to minimal symptoms.
CGI-I (Guy, 1976) score of 1. The CGI-I is a 7-point Likert-type scale used to indicate improvement relative to baseline severity. A score of 1 refers to very much improved. In the CAMS, response was defined as a CGI-I score of 1 or 2 (Walkup et al., 2008).
Predictor variables included the following measures
Brief Symptom Inventory (BSI; Derogatis, 1993). The total score of the BSI, a widely used 53-item self-report measure, indexed parents' psychiatric symptomatology.
State-Trait Anxiety Inventory ([STAI] Trait Version; Spielberger, 1983). Parental anxiety was assessed using the total score of the self-report STAI.
Both of these measures were completed primarily (87%) by mothers. The presence of comorbid internalizing (i.e., other anxiety and depressive disorders) and externalizing disorders was assessed using the ADIS-C/P. The CGI-S, study entry AD, and self-reported age, gender, socioeconomic status, and race/ethnicity were also examined as predictors of remission.
Results
Intent-to-treat analyses were conducted including all 488 randomized participants, regardless of study completion and/or compliance. Among them, 439 (90%) had complete Week 12 assessment data. Multiple imputation was used to impute data for the 49 participants who did not provide Week 12 data.
Remission Versus Response Rates
Table 1 presents remission and response rates for each treatment group. McNemar chi-square tests, estimated within a multiple imputation framework, examined whether response and remission rates differed significantly from each other. Results indicated that the sample remission rate was significantly lower than the sample response rate for all definitions of remission, the loss of AD diagnoses (f = 29.11, df = 1, ddf = 100, p < .0001), the CGI-S score of 1 or 2 (f = 19.35, df = 1, ddf = 77, p < .0001), and the CGI-I score of 1 (f = 63.43, df = 1, ddf = 86, p < .0001).
Table 1. Response and Remission Rates (With Confidence Intervals in Brackets) of Child/Adolescent Anxiety Multimodal Study Subjects at Week 12.
| Treatment | CGI-I responsea | No AD remission | CGI-S remission | CGI-I remission |
|---|---|---|---|---|
| COMB (n = 140) | 80.7 | 68.3 [58.7, 76.5] | 64.9 [54.8, 73.8] | 45.6 [36.2, 55.3] |
| SRT (n = 133) | 54.9 | 45.9b | 46.3 [35.9, 57.1] | 33.9 [25.9, 42.9] |
| CBT (n = 139) | 59.7 | 46.2 [37.9, 54.8] | 35.9 [28.3, 44.3] | 20.4 [14.4, 28.0] |
| PBO (n = 76) | 23.7 | 23.7 [15.5, 34.6] | 27.1 [13.0, 48.1] | 15.0 [3.4, 46.4] |
Note. COMB = combination treatment condition; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo; CGI-I = Clinical Global Impression Improvement Scale; CGI-S = Clinical Global Impression Severity Scale; AD = anxiety disorder.
Response rates reported in Walkup et al. (2008) and presented here for ease of comparison.
No variability in this estimate across imputations, thus confidence interval not applicable.
Remission Rates Across Treatment Conditions
To investigate whether remission status varied by treatment condition, we conducted a series of three logistic regression models. Each model also included several covariates: child's age, gender, minority status, socioeconomic status, and treatment site. Six contrasts for each model (comparing each of the four treatment conditions to each other) were conducted. Results for the loss of AD diagnoses indicated that participants in all three active treatments were significantly more likely to remit than participants in the PBO condition (see Table 2). Furthermore, participants in the COMB condition were more likely to remit than participants in the SRT and CBT conditions. SRT and CBT remission rates did not significantly differ from each other.
Table 2. Between-Group Comparisons of Remission Rates Based on Loss of Anxiety Disorder Diagnoses.
| Comparison | Odds ratio | SE | 95% confidence interval | df | t for H0 | p value |
|---|---|---|---|---|---|---|
| COMB vs. PBO | 7.47 | 2.63 | [2.30, 12.64] | 359 | 2.46 | 0.01 |
| SRT vs. PBO | 2.84 | 0.93 | [1.01, 4.67] | 478 | 1.98 | 0.05 |
| CBT vs. PBO | 2.91 | 0.96 | [1.03, 4.79] | 464 | 1.99 | 0.05 |
| COMB vs. CBT | 2.58 | 0.75 | [1.10, 4.06] | 203 | 2.10 | 0.04 |
| COMB vs. SRT | 2.63 | 0.74 | [1.16, 4.11] | 265 | 2.18 | 0.03 |
| SRT vs. CBT | 0.98 | 0.25 | [0.49, 1.47] | 456 | −0.09 | 0.93 |
Note. COMB = combination treatment condition; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo.
Results from the models for CGI-S and CGI-I remission revealed only one significant difference (see Tables 3 and 4). Using these definitions for remission, participants in the COMB treatment condition were more likely to remit than participants in the CBT condition. Despite this, neither COMB, CBT, nor SRT participants exhibited significantly different CGI-I or CGI-S remission rates from participants in the PBO condition.
Table 3. Between-Group Comparisons of Remission Rates Based on Clinical Global Impression Severity Scale Score of 1 or 2.
| Comparison | Odds ratio | SE | 95% confidence interval | df | t for H0 | p value |
|---|---|---|---|---|---|---|
| COMB vs. PBO | 5.59 | 3.22 | [0, 12.07] | 43 | 1.43 | 0.16 |
| SRT vs. PBO | 2.55 | 1.45 | [0, 5.48] | 43 | 1.07 | 0.29 |
| CBT vs. PBO | 1.65 | 0.94 | [0, 3.53] | 44 | 0.69 | 0.49 |
| COMB vs. CBT | 3.39 | 0.95 | [1.51, 5.27] | 253 | 2.51 | 0.01 |
| COMB vs. SRT | 2.22 | 0.68 | [0.86, 3.57] | 124 | 1.77 | 0.08 |
| SRT vs. CBT | 1.56 | 0.46 | [0.64, 2.47] | 148 | 1.20 | 0.23 |
Note. COMB = combination treatment condition; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo.
Table 4. Between-Group Comparisons of Remission Rates Based on Clinical Global Impression Improvement Scale Score of 1.
| Comparison | Odds ratio | SE | 95% confidence interval | df | t for H0 | p value |
|---|---|---|---|---|---|---|
| COMB vs. PBO | 5.97 | 4.88 | [0, 15.82] | 43 | 1.02 | 0.31 |
| SRT vs. PBO | 3.56 | 2.96 | [0, 9.53] | 43 | 0.86 | 0.39 |
| CBT vs. PBO | 1.77 | 1.49 | [0, 4.78] | 44 | 0.52 | 0.61 |
| COMB vs. CBT | 3.42 | 1.03 | [1.39, 5.46] | 253 | 2.34 | 0.02 |
| COMB vs. SRT | 1.71 | 0.49 | [0.74, 2.67] | 208 | 1.45 | 0.15 |
| SRT vs. CBT | 2.01 | 0.59 | [0.86, 3.17] | 402 | 1.72 | 0.09 |
Note. COMB = combination treatment; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo.
Predictors of Remission
In a second set of analyses, we conducted a series of single-predictor logistic regressions, within a multiple imputation framework, in which each of 10 potential variables was examined as predictors of remission. Four demographic variables (i.e., child's age, gender, minority status, and socioeconomic status), four baseline child clinical variables (i.e., anxiety severity as measured by the CGI-S, primary AD diagnosis, presence of a comorbid internalizing disorder [i.e., anxiety or depressive disorder] other than the primary three [i.e., GAD, SAD, and SOP] treated as part of this study, presence of a comorbid externalizing disorder), and two baseline measures of parental psychopathology (BSI Global scale and STAI total score) were examined. In a last step, we combined significant predictors together in one model to examine which uniquely contributed to predicting remission rates.
Demographic Variables
Age (measured in year increments) significantly predicted remission status on the ADIS-C/P, b = −0.007, t(464) = −2.65, p = .01, odds ratio (OR) = 0.92, 95% confidence interval (CI) [0.86, 0.98], and CGI-S, b = −0.006, t(443) = −2.11, p = .04, OR = 0.54, 95% CI [0.42, 0.71], such that older children were less likely to enter remission (see Table 5). Minority status also predicted remission on the ADIS-C/P, b = −0.73, t(331) = −2.97, p = .003, OR = 2.07, 95% CI [1.94, 2.21], such that minority children were less likely to enter remission (see Table 6). Neither gender nor socioeconomic status significantly predicted remission status for any definition of remission. None of the demographic variables significantly predicted CGI-I remission status.
Table 5. Remission Rates by Age.
| Treatment | % no AD | % CGI-S (1, 2) | % CGI-I (1) | |||
|---|---|---|---|---|---|---|
| 7–11 | 12–17 | 7–11 | 12–17 | 7–11 | 12–17 | |
| COMB | 73.2 | 58.8 | 70.4 | 54.4 | 48.0 | 41.0 |
| SRT | 51.1 | 34.9 | 50.7 | 37.0 | 39.6 | 21.9 |
| CBT | 51.7 | 36.1 | 37.2 | 33.6 | 20.2 | 20.7 |
| PBO | 26.0 | 19.4 | 30.0 | 21.3 | 15.5 | 14.1 |
Note. Percentages reported represent the proportion of participants in that cell (i.e., in that treatment condition and age group) who remitted. COMB = combination treatment; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo; AD = anxiety disorder; CGI-I = Clinical Global Impression Improvement Scale; CGI-S = Clinical Global Impression Severity Scale.
Table 6. Remission Rates by Treatment Condition and Minority Status.
| Treatment | % no AD | % CGI-S (1, 2) | % CGI-I (1) | |||
|---|---|---|---|---|---|---|
| Racial minority | Caucasian | Racial minority | Caucasian | Racial minority | Caucasian | |
| COMB | 45.1 | 73.0 | 52.1 | 67.5 | 40.1 | 46.7 |
| SRT | 36.7 | 48.5 | 41.2 | 47.8 | 27.8 | 35.7 |
| CBT | 33.7 | 50.1 | 26.0 | 39.0 | 21.9 | 19.9 |
| PBO | 18.8 | 25.1 | 30.4 | 26.1 | 20.7 | 13.4 |
Note. Percentages reported represent the proportion of participants in that cell (i.e., in that treatment condition and category with regard to minority status) who remitted. COMB = combination treatment; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo; AD = anxiety disorder; CGI-I = Clinical Global Impression Improvement Scale; CGI-S = Clinical Global Impression Severity Scale.
Baseline Child Clinical Variables
Higher anxiety on the CGI-S significantly predicted reduced likelihood of remitting for all definitions of remission, loss of AD diagnoses on the ADIS-C/P: b = −0.61, t(437) = −4.51, p = .0001, OR = 0.54, 95% CI [0.42, 0.71]; CGI-S: b = −0.64, t(387) = −4.62, p = .0001, OR = 0.64, 95% CI [0.48, 0.84]; CGI-I: b = −0.45, t(461) = −3.16, p = .002, OR = 0.52, 95% CI [0.40, 0.69].
Diagnoses
Binary variables coded to denote the presence or absence of a diagnosis at baseline for GAD, SAD, and SOP were entered together in models for each definition of remission. There were no significant interactions among diagnoses for any definition of remission; thus, interaction terms were not included in the models. Results revealed that participants with baseline SOP were significantly less likely to achieve remission than those participants without SOP on the ADIS-C/P, b = −0.91, t(473) = −3.65, p = .003, OR = 0.40, 95% CI [0.24, 0.66], and the CGI-S, b = −0.65, t(415) = −2.64, p = .01, OR = 0.52, 95% CI [0.32, 0.85], at Week 12 but not on the CGI-I score of 1, b = −0.36, t(461) = −1.43, p = .15 (see Table 7). No significant differences were found for participants with or without GAD and SAD.
Table 7. Remission Rates by Treatment Condition for Participants With and Without Social Phobia.
| Treatment | % no AD | % CGI-S (1, 2) | % CGI-I (1) | |||
|---|---|---|---|---|---|---|
| No SOP | SOP | No SOP | SOP | No SOP | SOP | |
| COMB | 88.0 | 64.0 | 84.0 | 60.7 | 52.0 | 44.2 |
| SRT | 52.0 | 44.4 | 47.6 | 46.0 | 40.6 | 32.3 |
| CBT | 72.0 | 40.6 | 52.0 | 32.4 | 28.0 | 18.7 |
| PBO | 46.1 | 19.1 | 45.9 | 23.1 | 17.3 | 14.5 |
Note. Percentages reported represent the proportion of participants in that cell (i.e., in that treatment condition and category with regard to SOP) who remitted. COMB = combination treatment; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo; AD = anxiety disorder; CGI-I = Clinical Global Impression Improvement Scale; CGI-S = Clinical Global Impression Severity Scale; SOP = social phobia.
At baseline, 44% of the sample (n = 215) met criteria for one or more of the following internalizing disorders, in addition to the child's target diagnosis/diagnoses of GAD, SAD, and/or SOP: selective mutism, obsessive-compulsive disorder, panic disorder, agoraphobia, specific phobia, major depressive disorder, major depressive disorder not otherwise specified, and dysthymic disorder. Eighteen percent (n = 90) met criteria for one or more of the following externalizing disorders: attention-deficit/hyperactivity disorder, attention-deficit/hyperactivity disorder not otherwise specified, conduct disorder, and oppositional defiant disorder (see Kendall et al., 2010, for a full description of comorbidities in the CAMS sample). The presence of a comorbid internalizing disorder was associated with a reduced likelihood of achieving remission in Week 12 as assessed by the ADIS-C/P, b = −0.38, t(459) = −2.04, p = .04, but was not statistically associated with the CGI-S, b = −0.36, t(306) = −1.84, p = .07, or CGI-I, t(437) = −0.89,p = .37, remission status (see Table 8). Comorbid externalizing disorder did not significantly predict remission status for any definition of remission, ADIS-C/P: t(396) = −0.81, p = .42; CGI-I: t(322) = 0.04, p = .89; and CGI-S: t(261) = −0.81, p = .42.
Table 8. Remission Rates by Treatment Condition for Participants With and Without Additional Internalizing Comorbidity.
| Treatment | % no AD | % CGI-S (1, 2) | % CGI-I (1) | |||
|---|---|---|---|---|---|---|
| No AIC | AIC | No AIC | AIC | No AIC | AIC | |
| COMB | 73.9 | 62.6 | 68.6 | 61.2 | 52.9 | 38.3 |
| SRT | 52.6 | 36.4 | 51.9 | 38.4 | 36.5 | 30.2 |
| CBT | 49.1 | 42.1 | 40.1 | 29.8 | 18.7 | 22.8 |
| PBO | 27.9 | 18.3 | 32.8 | 19.6 | 15.4 | 14.3 |
Note. Percentages reported represent the proportion of participants in that cell (i.e., in that treatment condition and category with regard to AIC) who remitted. COMB = combination treatment; SRT = sertraline; CBT = cognitive behavioral therapy; PBO = placebo; AD = anxiety disorder; CGI-I = Clinical Global Impression Improvement Scale; CGI-S = Clinical Global Impression Severity Scale; AIC = additional internalizing comorbidity.
Parental Psychopathology
Parent Global BSI scores did not significantly predict Week 12 remission status on the ADIS-C/P, t(381) = −0.07, p = .94; the CGI-I, t(418) = −0.12, p = .90; or the CGI-S, t(254) = 0.29, p = .77. Similarly, parental trait anxiety did not predict Week 12 remission status, ADIS-C/P: t(439) = 0.69, p = .49; CGI-I: t(411) = −0.13, p = .90; and CGI-S: t(392) = 1.01, p = .31.
Combined Predictors of Remission
In this last step in these analyses, we tested models in which baseline CGI-S score, the presence of SOP, and internalizing comorbidity, together with age and minority status, predicted remission status for each different definition of remission. Results indicated that baseline CGI-S score, b = −0.53, t(432) = −3.80, p = .0002; SOP, b = −0.77, t(467) = −2.93, p = .004; and minority status, b = −0.68, t(321) = −2.69, p = .001, all significantly predicted ADIS-C/P remission status when included in the same model. Internalizing comorbidity, b = −0.37, t(452) = −1.88, p = .06, and age, b = −0.05, t(456) = −1.77, p = .08, were not predictors of ADIS-C/P remission in this model. In contrast, only baseline CGI-S score, b = −0.64, t(384) = −4.20, p < .0001, and SOP, b = −0.51, t(403) = −1.98, p = .05, significantly predicted CGI-S remission status when included, together with comorbid internalizing, age, and minority status, in the same model. Last, only baseline CGI-S significantly predicted CGI-I remission status, b = −0.42, t(460) = −2.87, p = .004, when all significant predictors were included in the same model.
Discussion
Using diagnostic status as a rigorous definition of remission (i.e., no longer meeting criteria for any of the three primary ADs treated in this study), children randomized to the COMB condition had significantly higher remission rates than did children in any of the other treatment conditions. Children treated with either monotherapy had similar remission rates but higher remission rates than those in the PBO treatment. This pattern was similar to that found for response rates in the CAMS (Walkup et al., 2008). Findings also indicated that remission rates for the entire sample were significantly lower than response rates. The pattern and magnitude of remission rates found in the current study were fairly consistent with published CBT and SSRI medication trials for pediatric anxiety (Hudson et al., 2009; Wagner et al., 2004). Importantly, despite the use of varying definitions and measures used to assess remission in published CBT and medication trials, comparable remission rates were found across these definitions and measures used in this study (i.e., the CGI-I has been used most often in medication trials and the loss of AD used most often in CBT trials).
Findings from this study also revealed that remission rates varied based on the definition and measure used. This highlights the importance of developing a consensus definition of remission for ADs, as has been done for depression. Valid measures capturing this definition are also needed. For instance, the use of single-item measures such as the CGI-I, although used in published studies, may not be reliable and reflects a measure of improvement rather than remission.
Several baseline variables predicted remission status. Specifically, out of 10 predictors (four demographic, four child clinical, and two parent), five emerged as significant: younger age, nonminority race/ethnicity, lower severity of anxiety, absence of a comorbid internalizing (i.e., anxiety or depressive) disorder, and absence of SOP. When combined into a single model to assess their relative importance in predicting outcomes, lower baseline anxiety severity, absence of SOP and nonminority status all significantly predicted remission based on the ADIS-C/P. Taken together, each of these variables has been examined in previous CBT and medication pediatric anxiety trials with respect to treatment response or absence of primary disorder; however, findings across these studies have been inconsistent (e.g., Berman, Weems, Silverman, & Kurtines, 2000). Previous trials examining predictors of response have been hampered by small sample sizes, which may explain the inconsistent findings. Alternatively, predictors of remission may differ from those of response. Given the relatively large sample size of the CAMS, these results help clarify important and clinically relevant predictors of remission. The current findings suggest that the most consistent baseline predictors of remission (i.e., across more than one definition) were younger age, lower anxiety, and the absence of SOP. Taken together, refinements of treatment, augmentation, and/or increased dosage or duration of treatment may be needed for older and non-Caucasian youth and those with higher anxiety severity, SOP (as in Crawley, Beidas, Benjamin, Martin, & Kendall, 2008), and additional comorbid internalizing disorders.
Limitations
Findings from the current study should be interpreted in the context of several limitations. First, although we examined three definitions of remission, alternate definitions may yield different results, and future studies are needed to explore which definition is superior. Second, we examined a limited number of predictors. Future studies may identify additional predictors (as well as moderators or mediators) such as age of onset or duration of illness. Related to this, we did not examine whether the predictors differed for different treatment condition. Third, the sample was comprised of volunteers and excluded youth meeting criteria for major depressive disorder, limiting the representativeness of the sample. Fourth, RCTs such as the CAMS are powered to detect response, not remission, which may explain the absence of consistent statistical differences using the CGI-S and CGI-I remission criteria. Fifth, definitions of response and remission do not explicitly measure the degree to which intervention addresses associated functional impairment, an important index of outcome. Sixth, the current study addressed the end of acute treatment (i.e., 12 weeks of treatment) and not the long-term impact of residual anxiety symptoms. The availability of follow-up data will eventually enable tests to examine whether a particular remission definition possesses greater prognostic significance.
Clinical Implications and Future Directions
Achieving remission, rather than response or symptomatic improvement, is a preferred goal when treating youth with ADs. Although combined treatment had the highest remission rates relative to other treatment arms, clinicians need to be mindful that approximately 30%–50% of youth receiving 12 weeks of high-quality combined treatment will continue to experience some residual symptoms—even among those who show meaningful improvement. Treatments may need to be augmented or prolonged to buttress outcomes by targeting residual symptoms and the specific predictors of poor remission. Universal or unified protocols that target comorbid symptoms, adding social skills training for youth with SOP and enhancing parental involvement, may augment treatment response. Finally, identifying the mechanisms of change in CBT and in SRT and working toward optimizing these change strategies early in treatment may prove fruitful in maximizing the potential for remission. Given that the treatment providers in the CAMS were highly trained and continuously supervised, the need to improve current treatments for anxious youth may be even greater for clinical practice in community settings.
Acknowledgments
This study was supported by National Institute of Mental Health (NIMH) Grants MH64089, MH64107, MH64003, MH63747, MH064092, and MH64088.
Footnotes
Views expressed within this article represent those of the authors and are not intended to represent the position of the NIMH, National Institutes of Health, or Department of Health and Human Services.
Contributor Information
Golda S. Ginsburg, Division of Child and Adolescent Psychiatry, The Johns Hopkins University School of Medicine
Dara Sakolsky, Department of Psychiatry, University of Pittsburgh, and Western Psychiatric Institute & Clinic, University of Pittsburgh Medical Center.
John Piacentini, Division of Child and Adolescent Psychiatry, UCLA Semel Institute for Neuroscience and Human Behavior.
John T. Walkup, Department of Psychiatry, Weill Cornell Medical College, and Division of Child and Adolescent Psychiatry, New York-Presbyterian Hospital
Kimberly A. Coffey, Department of Psychiatry, Duke University Medical Center
Courtney P. Keeton, Division of Child and Adolescent Psychiatry, The Johns Hopkins University School of Medicine
Satish Iyengar, Departments of Statistics and Psychiatry, University of Pittsburgh.
Philip C. Kendall, Department of Psychology, Temple University
Scott N. Compton, Department of Psychiatry, Duke University Medical Center
Anne Marie Albano, Department of Psychiatry, New York State Psychiatric Institute–Columbia University Medical Center.
Joel Sherrill, Division of Services and Intervention Research, National Institute of Mental Health.
Moira A. Rynn, Department of Psychiatry, New York State Psychiatric Institute–Columbia University Medical Center
James T. McCracken, Division of Child and Adolescent Psychiatry, UCLA Semel Institute for Neuroscience and Human Behavior
Lindsey Bergman, Division of Child and Adolescent Psychiatry, UCLA Semel Institute for Neuroscience and Human Behavior.
Boris Birmaher, Department of Psychiatry, University of Pittsburgh, and Western Psychiatric Institute & Clinic, University of Pittsburgh Medical Center.
John March, Department of Psychiatry, Duke University Medical Center.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Berman SL, Weems CF, Silverman WK, Kurtines WM. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000;31:713–731. doi: 10.1016/S0005-7894(00)80040-4. [DOI] [Google Scholar]
- Crawley S, Beidas R, Benjamin C, Martin E, Kendall PC. Treating socially phobic youth with CBT: Differential outcomes and treatment considerations. Behavioural and Cognitive Psychotherapy. 2008;36:379–389. doi: 10.1017/S1352465808004542. [DOI] [Google Scholar]
- Derogatis LR. The Brief Symptom Inventory (BSI): Administration, scoring and procedures manual. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Frank E, Prien RF, Jarret RB, Keller MB, Kupfer DJ, Lavori PW, Weissman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Guy W. Clinical global impressions ECDEU assessment manual for psychopharmacology. Rockville, MD: National Institute for Mental Health; 1976. [Google Scholar]
- Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48:533–544. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, Piacentini J. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24:360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Hedtke K. Coping Cat workbook. 2nd. Ardmore, PA: Workbook Publishing; 2006. [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children for DSM-IV (Child and Parent Versions) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Wagner KD, Berard R, Stein MB, Wetherhold E, Carpenter DJ, Perera P, Machin A. A multicenter, randomized, double-blind, placebo-controlled trial of paroxetine in children and adolescents with social anxiety disorder. Archives of General Psychiatry. 2004;61:1153–1162. doi: 10.1001/archpsyc.61.11.1153. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]