Abstract
Background
Cholecystectomy is associated with increased risks in patients with cirrhosis. The well-established advantages of laparoscopic surgery may be offset by the increased risk for complications relating particularly to portal hypertension and coagulopathy.
Methods
A systematic search was undertaken to identify studies comparing open cholecystectomy (OC) and laparoscopic cholecystectomy (LC) in patients with cirrhosis. A meta-analysis was performed of the available randomized controlled trials (RCTs).
Results
Forty-four studies were analysed. These included a total of 2005 patients with cirrhosis who underwent laparoscopic (n= 1756) or open (n= 249) cholecystectomy, with mortality rates of 0.74% and 2.00%, respectively. A meta-analysis of three RCTs involving a total of 220 patients was conducted. There was a reduction in the overall incidences of postoperative complications and infectious complications and a shorter length of hospital stay in LC. However, frequencies of postoperative hepatic insufficiency did not differ significantly.
Conclusions
There are few RCTs comparing OC and LC in patients with cirrhosis. These studies are small, heterogeneous in design and include almost exclusively patients with Child–Pugh class A and B disease. However, LC appears to be associated with shorter operative time, reduced complication rates and reduced length of hospital stay.
Keywords: cirrhosis < liver, surgery < cholelithiasis, outcomes < gallbladder
Introduction
Prevalences of gallstones in patients with cirrhosis are estimated at 29–46%1,2 and thus are three times as high as those in patients without cirrhosis.3,4 In the non-cirrhotic population, laparoscopic cholecystectomy (LC) appears to have substantial advantages over conventional open cholecystectomy (OC) in terms of hospital stay and convalescence, but not in mortality, complications and operative time.5 However, in the era prior to LC, reported postoperative mortality in patients with cirrhosis undergoing OC was 7.5–25.5%6–9 and patients with the most advanced liver disease were at the greatest risk. Perhaps for this reason, the 1992 National Institutes of Health (NIH) consensus statement on LC confirmed that patients with end-stage cirrhosis of the liver with portal hypertension were not candidates for LC. The first study to specifically report outcomes of LC in the presence of cirrhosis was published in 1993,10 since when many case series and a few case–control studies of this group of patients have emerged. Indeed, a meta-analysis was published in 2003.11 Since then, the literature on the topic has further expanded to include randomized controlled trials (RCTs). This aim of this study was to systematically review the current literature on LC in cirrhosis and to determine whether there is indeed evidence to substantiate the contention that OC should be used preferentially in the presence of cirrhosis.
Materials and methods
Literature search strategy
Searches were conducted of PubMed, the MEDLINE database from 1950 to the 25th week of 2011 and the EMBASE database from January 1980 to the 25th week of 2011. The OVID search engine (Version OvidSP_UI03.02.04.102; Ovid Technologies, Inc., New York, NY, USA) was used. The MESH/EmTree heading ‘liver cirrhosis’ yielded 63 980 hits in MEDLINE and 83 677 hits in EMBASE, and the search term ‘liver cirrhosis’ yielded 81 315 hits in PubMed. The MESH/EmTree heading ‘cholecystectomy’ yielded 22 175 hits in MEDLINE and 28 624 hits in EMBASE, and the search term ‘cholecystectomy’ yielded 27 705 hits in PubMed. The results of these searches were combined in each database to yield 246 articles in MEDLINE, 365 articles in EMBASE and 414 articles in PubMed.
Study selection
Study evaluation was performed by two of the reviewers (JML and PDT). Articles were selected on the basis of three levels of screening12 summarized in Fig. 1. Studies were included regardless of publication status, date of publication and number of participants. Studies published in languages other than English13–15 were translated and the data extracted. Where similar data from the same institution were published on more than one occasion,10,16,17 data from the most relevant publication were analysed. In many of the case series of OC prior to the widespread availability of endoscopic retrograde cholangiopancreatography (ERCP), many patients underwent concomitant open procedures, particularly bile duct exploration and drainage.6,8,18–22 Because the morbidity associated with these additional open procedures might potentially bias comparison with surgery in the laparoscopic era (in which concomitant laparoscopic bile duct exploration was almost never performed), the aforementioned studies were excluded from analysis.
Figure 1.
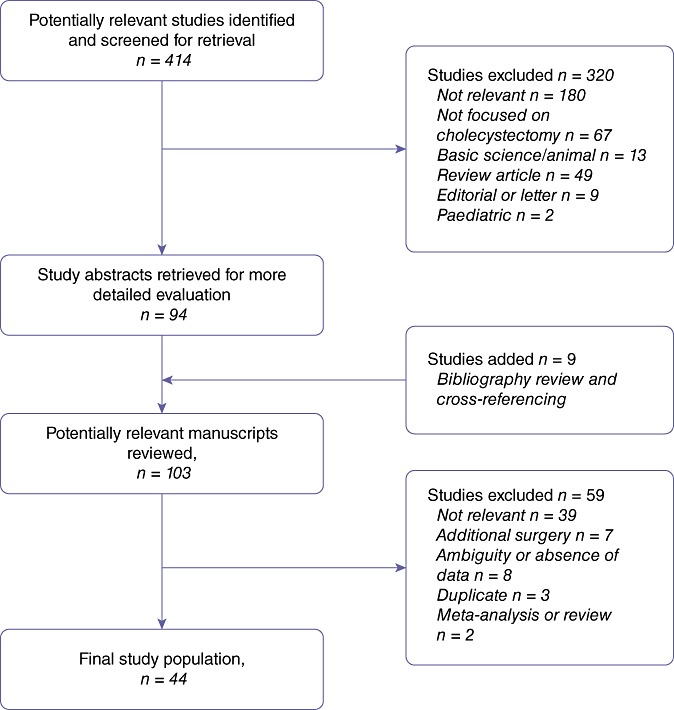
Flow chart showing the search strategy used to identify studies
Data extraction
Each of these 44 articles were independently reviewed by two of the authors (JML and PDT), who separately extracted data on the following categories: dates over which the study was conducted; numbers of patients in the OC and LC groups; age and sex of the patients studied; causes of liver disease; severity of cirrhosis;23 indication(s) for cholecystectomy; mortality; morbidity; rate of conversion to LC; operation times; blood loss; transfusion requirements, and length of hospital stay (LoS). The extracted data were then crosschecked by the two authors to rule out discrepancy. In the event of disagreement, data were extracted by a third reviewer (VWTL).
Study outcomes
The main outcomes analysed were the total numbers of patients with cirrhosis undergoing OC and LC and the total number of postoperative deaths in each group. When reported, the patients' Child–Pugh23 status, age, sex and indication for surgery were recorded. Mortality was described with respect to Child–Pugh status when data were provided. All studies, irrespective of design, were included for these outcomes. Total postoperative complication rate, postoperative infectious complication rate, postoperative hepatic insufficiency and LoS were recorded for each study, but a meta-analysis was performed only for the RCTs. The total rate of postoperative complications was a composite outcome measure of complications including pneumonia, wound infection, urinary tract infection, intra-abdominal abscess and peritonitis. The rate of postoperative hepatic insufficiency referred to a composite of the reported incidences of episodes of unspecified liver failure, ascites and encephalopathy. Because not all outcomes were universally reported in each study, when the proportional frequency of an outcome was reported, the denominator was altered according to the number of patients in the studies reporting that outcome (i.e. the population at risk).
Statistical methods
Because of the heterogeneity of the studies selected and the fact that most of them lacked a control group, no meta-analysis could be carried out on the case series and case–control studies. Hence, a descriptive analysis based on the patient pool comprising all of the patients in each of the OC and LC groups was performed. For the RCTs only, meta-analyses were performed using Revman 5.0 (Version 5.0.25 for Mac OS X; Nordic Cochrane Centre, Cochrane Collaboration, Copenhagen, Denmark).24 For dichotomous outcomes, the odds ratio (OR) was calculated with a 95% confidence interval (CI) using the Mantel–Haenszel (M–H) method. For continuous outcomes, the mean difference (MD) and 95% CI were calculated. A random effects model was used. The heterogeneity of study results was assessed using the chi-squared test and the I2 statistic of inconsistency. Statistically significant heterogeneity was defined as a P-value of <0.1 or an I2 statistic >50%.25
Study quality
The studies were assessed using the Oxford Centre for Evidence-Based Medicine Level of Evidence Scale.26 The studies included in the analysis constituted Level 3b or Level 4 evidence, with the exception of the three RCTs, which constituted Level 1b evidence (Table 1).
Table 1.
Summary of studies included in this systematic review
| Author(s) | City of institution | Year | Study design | Participants, n | LC | OC | Level of evidencea |
|---|---|---|---|---|---|---|---|
| Angrisani et al.27 | Naples | 1997 | RCS | 31 | 31 | 0 | 4 |
| Bende & Csiszar13 | Budapest | 1997 | RCS | 27 | 27 | 0 | 4 |
| Bessa et al.28 | Alexandria | 2011 | PCS | 20 | 20 | 0 | 4 |
| Bingener et al.65 | San Antonio, TX | 2008 | RCS | 99 | 99 | 0 | 4 |
| Clark et al.64 | Sydney, NSW | 2001 | RCS | 25 | 25 | 0 | 4 |
| Cobb et al.63 | Charlotte, NC | 2005 | RCS | 22 | 22 | 0 | 4 |
| Cucinotta et al.16 | Messina | 2003 | RCS | 22 | 22 | 0 | 4 |
| Curro et al.62 | Messina | 2005 | RCS | 42 | 42 | 0 | 4 |
| D'Albuquerque et al.61 | São Paulo, SP | 1995 | RCS | 12 | 12 | 0 | 4 |
| da Silveira60 | Stanford, CA | 2006 | RCS | 33 | 24 | 9 | 4 |
| Delis et al.59 | Miami, FL | 2010 | RCS | 220 | 220 | 0 | 4 |
| Dunnington et al.58 | Tucson, AZ | 1987 | RCS | 22 | 0 | 22 | 4 |
| El Nakeeb et al.57 | Mansoura | 2010 | PCS | 60 | 60 | 0 | 4 |
| El-Awadi et al.56 | Mansoura | 2009 | RCT | 110 | 55 | 55 | 1b |
| Fernandes et al.55 | San Antonio, TX | 2000 | RCS | 48 | 48 | 0 | 4 |
| Fontes et al.15 | Porto Alegre, RS | 2002 | RCS | 10 | 10 | 0 | 4 |
| Friel et al.54 | Boston, MA | 1999 | RCS | 30 | 30 | 0 | 4 |
| Garrison et al.7 | Louisville, KY | 1984 | RCS | 29 | 0 | 29 | 4 |
| Gugenheim et al.53 | Nice | 1996 | RCS | 9 | 9 | 0 | 4 |
| Hamad et al.52 | Assiut | 2010 | RCT | 30 | 15 | 15 | 1b |
| Hamid et al.51 | Karachi | 1993 | RCS | 18 | 0 | 18 | 4 |
| Ishikawa et al.50 | Osaka | 1995 | RCS | 4 | 4 | 0 | 4 |
| Jan & Chen49 | Chang Gung | 1997 | RCS | 21 | 21 | 0 | 4 |
| Ji et al.48 | Nanjing | 2004 | RCS | 38 | 38 | 0 | 4 |
| Ji et al.47 | Nanjing | 2005 | RCT | 80 | 42 | 38 | 1b |
| Kogut et al.46 | New York, NY | 1985 | RCS | 27 | 0 | 27 | 4 |
| Lacy et al.45 | Barcelona | 1995 | RCS | 11 | 11 | 0 | 4 |
| Leandros et al.44 | Athens | 2008 | RCS | 34 | 34 | 0 | 4 |
| Leone et al.43 | Turin | 2001 | RCS | 24 | 24 | 0 | 4 |
| Mancero et al.42 | São Paulo, SP | 2008 | RCS | 30 | 30 | 0 | 4 |
| Morino et al.41 | Turin | 2000 | RCS | 33 | 33 | 0 | 4 |
| Nguyen et al.40 | Pittsburgh, PA | 2011 | RCS | 68 | 68 | 0 | 4 |
| Palanivelu et al.39 | Tamilnadu | 2006 | RCS | 265 | 265 | 0 | 4 |
| Pavlidis et al.38 | Thessaloniki | 2009 | RCS | 38 | 38 | 0 | 4 |
| Poggio et al.22 | Rochester, MN | 2000 | RCC | 36 | 24 | 12 | 3b |
| Saeki et al.37 | Fukuoka | 1997 | RCC | 13 | 7 | 6 | 3b |
| Schiff et al.36 | Boston, MA | 2005 | RCS | 31 | 27 | 4 | 4 |
| Shaikh & Muneer35 | Sindh | 2009 | RCS | 20 | 20 | 0 | 4 |
| Sleeman et al.34 | Miami, FL | 1998 | RCS | 25 | 25 | 0 | 4 |
| Tuech et al.33 | Angers | 2002 | RCS | 26 | 26 | 0 | 4 |
| Urban et al.32 | Cleveland, OH | 2001 | RCS | 15 | 15 | 0 | 4 |
| Van Landingham31 | Temple, TX | 1984 | RCS | 7 | ND | 7 | 4 |
| Yeh et al.30 | Taoyuan | 2002 | RCS | 226 | 226 | 0 | 4 |
| Yerdel et al.29 | Ankara | 1997 | PCC | 14 | 7 | 7 | 3b |
Oxford Centre for Evidence-Based Medicine level of evidence scale.
LC, laparoscopic cholecystectomy; OC, open cholecystectomy; RCS, retrospective case series; PCC, prospective case–control study; RCC, retrospective case–control study; RCT, randomized controlled trial; PCS, prospective case series; ND, no data.
Results
Description of studies
The studies included in the systematic review are summarized in Table 1. Forty-four studies were included in the analysis.7,13,15,16,22,27–65 These included three RCTs comparing open and laparoscopic surgery in cirrhosis,47,52,56 three case–control studies22,29,37 and 38 case series.7,13,15,16,27,28,30–36,38–46,48–51,53–55,57–65 Two RCTs comparing outcomes of conventional LC and LC performed using the harmonic scalpel in cirrhotic patients were included.28,57 Only the outcomes of conventional LC from these studies were analysed. Main outcome measures are summarized in Table 2.
Table 2.
Summary of outcome measures for laparoscopic and open cholecystectomy in cirrhosis
| Outcome | Laparoscopic cholecystectomy | Open cholecystectomy |
|---|---|---|
| Number of patients | 1756 | 249 |
| Mortality rate, % (deaths/number at risk) | 0.8% (13/1623) | 2.0% (5/249) |
| Stratified mortalitya (A/B/C) | 4/1/1 | ND |
| Mean age ± SE, years | 52.6 ± 1.2 | 50.2 ± 3.2 |
| Sex, male/female | 804/759 | 103/67 |
| Severity of liver diseasea, Child–Pugh class A/B/C | 915/260/19 | 117/50/7 |
| Indication for surgery, % AC (number AC/number at risk) | 19.6% (283/1442) | 28.8% (19/66) |
| Conversion rate, % (conversion/number at risk) | 5.8% (98/1698) | ND |
| Overall complications, % (events/number at risk) | 17.6% (304/1729) | 47.7% (103/216) |
| Infectious complications, % (events/number at risk) | 5.9% (100/1729) | 19.9% (43/216) |
| Postoperative hepatic insufficiency, % (events/number at risk) | 7.7% (133/1729) | 18.1% (39/216) |
Child–Pugh status stratified as A/B/C.
SE, standard error; AC, acute cholecystitis; ND, no data.
Patient characteristics
The systematic review included data pertaining to 2005 patients with cirrhosis undergoing laparoscopic (n= 1756) and open (n= 249) cholecystectomy. Data pertaining to the demographics, severity of chronic liver disease, proportion of patients with acute cholecystitis and conversion rate are summarized in Table 2.
Mortality and complications
Mortality rates in LC and OC were 0.74% and 2.00%, respectively (Table 2). All the deaths in the OC cohort were contributed from a single study,7 which did not report Child–Pugh status. Studies of LC in which mortality was stratified according to Child–Pugh status were analysed, including data pertaining to 1328 patients among whom six deaths were reported. Four of these patients had Child–Pugh class C status and the remaining two had Child–Pugh class A and class B status, respectively. Rates of overall complications, infectious complications and postoperative hepatic insufficiency in the LC and OC groups are summarized in Table 2.
Meta-analysis of RCTs
Outcomes for a total of 220 patients reported in the RCTs were subjected to meta-analysis. No instances of mortality were recorded in any RCT. There were reductions in the overall incidence of postoperative complications (OR 0.25, 95% CI 0.07–0.88) (Fig. 2a) and in the incidence of infectious complications in LC (OR 0.23, 95% CI 0.10–0.56) (Fig. 2b), but the frequency of postoperative hepatic insufficiency did not differ significantly between LC and OC (OR 0.53, 95% CI 0.12–2.32) (Fig. 2c). Length of hospital stay was substantially shorter in patients undergoing LC (MD − 3.31, 95% CI − 4.46 to − 2.16) (Fig. 2d). Statistically significant heterogeneity was observed in the analyses of rates of all postoperative complications (I2= 75%), postoperative hepatic insufficiency (I2= 69%) and LoS (I2= 69%), but not in the infectious complications outcome (I2= 0%). Given the small number of studies, funnel plot analysis could not be used to explore bias.66,67
Figure 2.
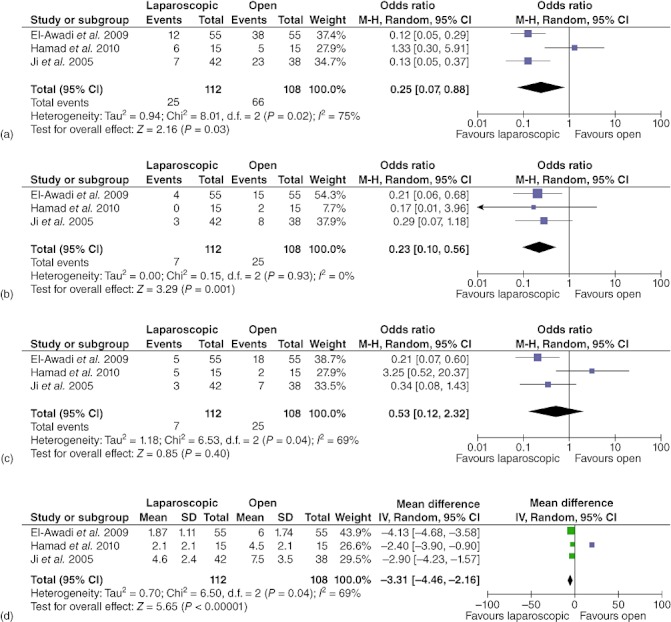
Forest plots illustrating meta-analyses of outcomes in patients with cirrhosis undergoing cholecystectomy by laparoscopic or open surgery. Outcomes analysed were: (a) total postoperative complications, (b) infectious complications, (c) postoperative hepatic insufficiency and (d) length of hospital stay. M–H, Mantel–Haenszel test; 95% CI, 95% confidence interval
Discussion
This systematic review addressed the issue of whether the preferential utilization of OC in cirrhotic patients, as suggested by the 1992 NIH consensus statement,68 has an impact on surgical outcomes. There are few data pertaining to patients with Child–Pugh class C cirrhosis; however, the review and meta-analysis shows that for patients of Child–Pugh class A or B status, LC appears to be associated with reduced complication rates, shorter operative time and reduced LoS. In 1982 Aranha et al. described a 25.5% mortality rate in patients with cirrhosis undergoing cholecystectomy.9 During the dissemination of LC technique, concern about the safety of the procedure in cirrhosis was coloured by such data from the era of open surgery. Certainly, patients with chronic liver disease are at increased risk for mortality when undergoing abdominal surgery.69–71 Cholecystectomy in particular may be more hazardous in cirrhosis because of haemorrhage related to portal hypertension, coagulopathy and thrombocytopenia. In addition, the reduced compliance of the fibrotic liver may make the retraction and exposure of Calot's triangle more difficult laparoscopically.72 It was therefore posited that the benefits of laparoscopic surgery in terms of postoperative recovery5 would be offset by the greater risk for complications associated with the lesser degree of tactile control73 and three-dimensional feedback.74
The quality of the evidence comparing the outcomes of LC and OC is poor. The majority of the data are derived from case series; only three small RCTs have been published. In this systematic review, the data from all studies were pooled as if the combined findings were derived from a single sample, but statistical analyses were not applied. The application of any formal meta-analytic methods, particularly simple pooling, to observational studies is associated with a significant risk for error and for biased conclusions, but it does provide an indication of real-world outcomes.75 Given that combining data by meta-analytic methods is preferable,76 only data from the RCTs were combined. However, it must be acknowledged that the RCTs included in this review each include a small number of patients and, indeed, heterogeneity is evident in meta-analytic statistical measures (I2 statistic). This heterogeneity is probably attributable to differences in the patient samples (such as in the severity of liver disease and the proportion of patients with acute cholecystitis), interventions (use of subtotal cholecystectomy and conversion to OC), outcome assessments and reporting quality. Despite the aforementioned caveats, it appears that LC offers the cirrhotic patient a similar advantage over OC in terms of LoS as it does the non-cirrhotic patient.5 In contradistinction to the non-cirrhotic population undergoing cholecystectomy, this meta-analysis suggests that overall complications and infectious complications may be fewer in LC than in OC in cirrhosis.
Given that conversion to OC is always an option, LC in cirrhosis should be at least as safe as ab initio open surgery provided that the surgeon who starts the procedure laparoscopically has a range of safe options available if problems arise intraoperatively. Commonly discussed options include laparoscopic subtotal39,77–79 and partial80 cholecystectomy, which have been used successfully to circumvent the hazards associated with dissection in the cirrhotic liver bed and around the porta hepatis. Other options include laparoscopic cholecystostomy81 and percutaneous transhepatic cholecystostomy.82,83 Ultimately, conversion to an open procedure remains a fall-back option when safe dissection, visualization of anatomy or control of haemorrhage become impossible laparoscopically. In this review, conversion from LC represented a reasonably frequently used option and occurred in about 5% of procedures. Although an increase in morbidity may be associated with the occasional conversion to open surgery compared with cases completed laparoscopically,84 it seems intuitive that this morbidity will be lower than that caused by a policy of universal OC ab initio, provided that minimal complications arise in the preliminary laparoscopic dissection.
In the current analysis, the mortality rates reported for both LC and OC are substantially lower than those reported for OC in the 1980s. This probably reflects improvements in patient selection and critical care, better treatment of liver failure (particularly liver transplantation), and the availability of a variety of non-surgical options (such as percutaneous cholecystostomy and ERCP) for the high-risk cirrhotic patient. There are relatively few data about the outcome of cholecystectomy in Child–Pugh class C cirrhosis as only 26 patients with this disease class were included in this review, but this group was over-represented amongst the mortalities. Although mortality rates as high as 25% were reported for OC in cirrhosis as recently as the 1980s,9 this analysis of the literature found no reports of death in OC in the cirrhotic population during the era of LC. Clearly, therefore, the dramatic reduction in mortality in cholecystectomy in cirrhosis after LC became commonplace was not associated with the introduction of minimally invasive surgery, but, rather, with other changes in the assessment and management of both chronic liver disease and gallstones. Previously, a considerable proportion of patients with significant jaundice underwent OC and, subsequently, open bile duct exploration and drainage procedures. Often these explorations were not therapeutic as the jaundice was presumably related to the decompensation of chronic liver disease and not obstruction.6,8,18–22 This type of scenario has become uncommon since the accuracy of imaging85,86 and efficacy of endoscopic intervention87,88 have improved and percutaneous biliary interventions have become available.83,89,90 More generally, the death rate from chronic liver disease has changed substantially coincident with the introduction of LC.91,92 Moreover, a significant proportion of the change in mortality in patients with chronic liver disease undergoing surgery is likely to be attributable to the widespread introduction of liver transplantation in the mid-1980s93 and the impact this has had on techniques for managing liver failure and portal hypertension. The greatest danger of mortality in cholecystectomy refers to patients with decompensated liver disease. The most critical factors in avoiding death are, therefore, appropriate diagnosis and treatment of the underlying chronic liver disease, judicious selection of patients for surgery and use of non-surgical temporization measures for patients in whom the level of risk prohibits operative procedures.
Conflicts of interest
None declared.
References
- 1.Bouchier IA. Postmortem study of the frequency of gallstones in patients with cirrhosis of the liver. Gut. 1969;10:705–710. doi: 10.1136/gut.10.9.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iber FL, Caruso G, Polepalle C, Kuchipudi V, Chinoy M. Increasing prevalence of gallstones in male veterans with alcoholic cirrhosis. Am J Gastroenterol. 1990;85:1593–1596. [PubMed] [Google Scholar]
- 3.Conte D, Fraquelli M, Fornari F, Lodi L, Bodini P, Buscarini L. Close relation between cirrhosis and gallstones: cross-sectional and longitudinal survey. Arch Intern Med. 1999;159:49–52. doi: 10.1001/archinte.159.1.49. [DOI] [PubMed] [Google Scholar]
- 4.Maggi A, Solenghi D, Panzeri A, Borroni G, Cazzaniga M, Sangiovanni A, et al. Prevalence and incidence of cholelithiasis in patients with liver cirrhosis. Ital J Gastroenterol Hepatol. 1997;29:330–335. [PubMed] [Google Scholar]
- 5.Keus F, Gooszen HG, van Laarhoven CJ. Open, small-incision, or laparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato-Biliary Group reviews. Cochrane Database Syst Rev. 2010;(1):CD008318. doi: 10.1002/14651858.CD008318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bloch RS, Allaben RD, Walt AJ. Cholecystectomy in patients with cirrhosis. A surgical challenge. Arch Surg. 1985;120:669–672. doi: 10.1001/archsurg.1985.01390300019003. [DOI] [PubMed] [Google Scholar]
- 7.Garrison RN, Cryer HM, Howard DA, Polk HC., Jr Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann Surg. 1984;199:648–655. doi: 10.1097/00000658-198406000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castaing D, Houssin D, Lemoine J, Bismuth H. Surgical management of gallstones in cirrhotic patients. Am J Surg. 1983;146:310–313. doi: 10.1016/0002-9610(83)90403-8. [DOI] [PubMed] [Google Scholar]
- 9.Aranha GV, Sontag SJ, Greenlee HB. Cholecystectomy in cirrhotic patients: a formidable operation. Am J Surg. 1982;143:55–60. doi: 10.1016/0002-9610(82)90129-5. [DOI] [PubMed] [Google Scholar]
- 10.Yerdel MA, Tsuge H, Mimura H, Sakagami K, Mori M, Orita K. Laparoscopic cholecystectomy in cirrhotic patients: expanding indications. Surg Laparosc Endosc. 1993;3:180–183. [PubMed] [Google Scholar]
- 11.Puggioni A, Wong LL. A meta-analysis of laparoscopic cholecystectomy in patients with cirrhosis. J Am Coll Surg. 2003;197:921–926. doi: 10.1016/j.jamcollsurg.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 12.de Meijer VE, Kalish BT, Puder M, Ijzermans JN. Systematic review and meta-analysis of steatosis as a risk factor in major hepatic resection. Br J Surg. 2010;97:1331–1339. doi: 10.1002/bjs.7194. [DOI] [PubMed] [Google Scholar]
- 13.Bende J, Csiszar M. [Laparoscopic cholecystectomy in patients with liver cirrhosis. Orv Hetil. 1997;138:481–482. [PubMed] [Google Scholar]
- 14.Eramishantsev AK, Gordeev PS, Akhmetzhanov KK. [Diagnosis and therapy of acute cholecystitis in liver cirrhosis.] Khirurgiia (Mosk) 1992;1:15–17. [PubMed] [Google Scholar]
- 15.Fontes PR, de Mattos AA, Eilers RJ, Nectoux M, Pinheiro JO. [Laparoscopic cholecystectomy in patients with liver cirrhosis. Arq Gastroenterol. 2002;39:212–216. doi: 10.1590/s0004-28032002000400002. [DOI] [PubMed] [Google Scholar]
- 16.Cucinotta E, Lazzara S, Melita G. Laparoscopic cholecystectomy in cirrhotic patients. Surg Endosc. 2003;17:1958–1960. doi: 10.1007/s00464-002-8852-4. [DOI] [PubMed] [Google Scholar]
- 17.Curro G, Baccarani U, Adani G, Cucinotta E. Laparoscopic cholecystectomy in patients with mild cirrhosis and symptomatic cholelithiasis. Transplant Proc. 2007;39:1471–1473. doi: 10.1016/j.transproceed.2007.01.086. [DOI] [PubMed] [Google Scholar]
- 18.Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122:730–735. doi: 10.1016/s0039-6060(97)90080-5. discussion 735–736. [DOI] [PubMed] [Google Scholar]
- 19.Isozaki H, Okajima K, Morita S, Ishibashi T, Tanimura M, Hara H, et al. Surgery for cholelithiasis in cirrhotic patients. Surg Today. 1993;23:504–508. doi: 10.1007/BF00730625. [DOI] [PubMed] [Google Scholar]
- 20.Sirinek KR, Burk RR, Brown M, Levine BA. Improving survival in patients with cirrhosis undergoing major abdominal operations. Arch Surg. 1987;122:271–273. doi: 10.1001/archsurg.1987.01400150025003. [DOI] [PubMed] [Google Scholar]
- 21.Cryer HM, Howard DA, Garrison RN. Liver cirrhosis and biliary surgery: assessment of risk. South Med J. 1985;78:138–141. doi: 10.1097/00007611-198502000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Poggio JL, Rowland CM, Gores GJ, Nagorney DM, Donohue JH. A comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease. Surgery. 2000;127:405–411. doi: 10.1067/msy.2000.104114. [DOI] [PubMed] [Google Scholar]
- 23.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JPT, Green S. 2009. Cochrane Handbook for Systematic Reviews of Interventions Version 5.02. http://www.cochrane-handbook.org. [Accessed 20 December 2010]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips B, Ball C, Sacket D, Bendoch D, Straus S, Haynes B, et al. 2011. Oxford Centre for Evidence-Based Medicine Level of Evidence. http://www.cebm.net/index.aspx?o=1025. [Accessed 20 December 2011.
- 27.Angrisani L, Lorenzo M, Corcione F, Vincenti R. Gallstones in cirrhotics revisited by a laparoscopic view. J Laparoendosc Adv Surg Tech A. 1997;7:213–220. doi: 10.1089/lap.1997.7.213. [DOI] [PubMed] [Google Scholar]
- 28.Bessa SS, Abdel-Razek AH, Sharaan MA, Bassiouni AE, El-Khishen MA, El-Kayal el SA. Laparoscopic cholecystectomy in cirrhotics: a prospective randomized study comparing the conventional diathermy and the harmonic scalpel for gallbladder dissection. J Laparoendosc Adv Surg Tech A. 2011;21:1–5. doi: 10.1089/lap.2010.0255. [DOI] [PubMed] [Google Scholar]
- 29.Yerdel MA, Koksoy C, Aras N, Orita K. Laparoscopic versus open cholecystectomy in cirrhotic patients: a prospective study. Surg Laparosc Endosc. 1997;7:483–486. [PubMed] [Google Scholar]
- 30.Yeh CN, Chen MF, Jan YY. Laparoscopic cholecystectomy in 226 cirrhotic patients. Experience of a single centre in Taiwan. Surg Endosc. 2002;16:1583–1587. doi: 10.1007/s00464-002-9026-0. [DOI] [PubMed] [Google Scholar]
- 31.Van Landingham SB. Cholecystectomy in cirrhotic patients. South Med J. 1984;77:38–40. doi: 10.1097/00007611-198401000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Urban L, Eason GA, ReMine S, Bogard B, Magisano J, Raj P, et al. Laparoscopic cholecystectomy in patients with early cirrhosis. Curr Surg. 2001;58:312–315. doi: 10.1016/s0149-7944(00)00477-3. [DOI] [PubMed] [Google Scholar]
- 33.Tuech JJ, Pessaux P, Regenet N, Rouge C, Bergamaschi R, Arnaud JP. Laparoscopic cholecystectomy in cirrhotic patients. Surg Laparosc Endosc Percutan Tech. 2002;12:227–231. doi: 10.1097/00129689-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Sleeman D, Namias N, Levi D, Ward FC, Vozenilek J, Silva R, et al. Laparoscopic cholecystectomy in cirrhotic patients. J Am Coll Surg. 1998;187:400–403. doi: 10.1016/s1072-7515(98)00210-5. [DOI] [PubMed] [Google Scholar]
- 35.Shaikh AR, Muneer A. Laparoscopic cholecystectomy in cirrhotic patients. JSLS. 2009;13:592–596. doi: 10.4293/108680809X12589999537959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schiff J, Misra M, Rendon G, Rothschild J, Schwaitzberg S. Laparoscopic cholecystectomy in cirrhotic patients. Surg Endosc. 2005;19:1278–1281. doi: 10.1007/s00464-004-8823-z. [DOI] [PubMed] [Google Scholar]
- 37.Saeki H, Korenaga D, Yamaga H, Mawatari K, Orita H, Itasaka H, et al. A comparison of open and laparoscopic cholecystectomy for patients with cirrhosis. Surg Today. 1997;27:411–413. doi: 10.1007/BF02385703. [DOI] [PubMed] [Google Scholar]
- 38.Pavlidis TE, Symeonidis NG, Psarras K, Skouras C, Kontoulis TM, Ballas K, et al. Laparoscopic cholecystectomy in patients with cirrhosis of the liver and symptomatic cholelithiasis. JSLS. 2009;13:342–345. [PMC free article] [PubMed] [Google Scholar]
- 39.Palanivelu C, Rajan PS, Jani K, Shetty AR, Sendhilkumar K, Senthilnathan P, et al. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203:145–151. doi: 10.1016/j.jamcollsurg.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 40.Nguyen KT, Kitisin K, Steel J, Jeyabalan G, Aggarwal S, Geller DA, et al. Cirrhosis is not a contraindication to laparoscopic cholecystectomy: results and practical recommendations. HPB (Oxford) 2011;13:192–197. doi: 10.1111/j.1477-2574.2010.00270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morino M, Cavuoti G, Miglietta C, Giraudo G, Simone P. Laparoscopic cholecystectomy in cirrhosis: contraindication or privileged indication? Surg Laparosc Endosc Percutan Tech. 2000;10:360–363. [PubMed] [Google Scholar]
- 42.Mancero JM, D'Albuquerque LA, Gonzalez AM, Larrea FI, de Oliveira e Silva A. Laparoscopic cholecystectomy in cirrhotic patients with symptomatic cholelithiasis: a case–control study. World J Surg. 2008;32:267–270. doi: 10.1007/s00268-007-9314-x. [DOI] [PubMed] [Google Scholar]
- 43.Leone N, Garino M, De Paolis P, Pellicano R, Fronda GR, Rizzetto M. Laparoscopic cholecystectomy in cirrhotic patients. Dig Surg. 2001;18:449–452. doi: 10.1159/000050192. [DOI] [PubMed] [Google Scholar]
- 44.Leandros E, Albanopoulos K, Tsigris C, Archontovasilis F, Panoussopoulos SG, Skalistira M, et al. Laparoscopic cholecystectomy in cirrhotic patients with symptomatic gallstone disease. ANZ J Surg. 2008;78:363–365. doi: 10.1111/j.1445-2197.2008.04478.x. [DOI] [PubMed] [Google Scholar]
- 45.Lacy AM, Balaguer C, Andrade E, Garcia-Valdecasas JC, Grande L, Fuster J, et al. Laparoscopic cholecystectomy in cirrhotic patients. Indication or contradiction? Surg Endosc. 1995;9:407–408. doi: 10.1007/BF00187160. [DOI] [PubMed] [Google Scholar]
- 46.Kogut K, Aragoni T, Ackerman NB. Cholecystectomy in patients with mild cirrhosis. A more favourable situation. Arch Surg. 1985;120:1310–1311. doi: 10.1001/archsurg.1985.01390350090019. [DOI] [PubMed] [Google Scholar]
- 47.Ji W, Li LT, Wang ZM, Quan ZF, Chen XR, Li JS. A randomized controlled trial of laparoscopic versus open cholecystectomy in patients with cirrhotic portal hypertension. World J Gastroenterol. 2005;11:2513–2517. doi: 10.3748/wjg.v11.i16.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ji W, Li LT, Chen XR, Li JS. Application of laparoscopic cholecystectomy in patients with cirrhotic portal hypertension. Hepatobiliary Pancreat Dis Int. 2004;3:270–274. [PubMed] [Google Scholar]
- 49.Jan YY, Chen MF. Laparoscopic cholecystectomy in cirrhotic patients. Hepatogastroenterology. 1997;44:1584–1587. [PubMed] [Google Scholar]
- 50.Ishikawa T, Sowa M, Nagayama M, Nishiguchi Y. Laparoscopic cholecystectomy for cholelithiasis in patients with liver cirrhosis. Diagn Ther Endosc. 1995;1:147–152. doi: 10.1155/DTE.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamid S, Siddiqui M, Jafri W, Shah H, Khan H, Ahmed M. Outcome of biliary tract surgery in unknown cirrhotics: a case–control study. Ann R Coll Surg Engl. 1993;75:434–436. [PMC free article] [PubMed] [Google Scholar]
- 52.Hamad MA, Thabet M, Badawy A, Mourad F, Abdel-Salam M, Abdel-Rahman Mel T, et al. Laparoscopic versus open cholecystectomy in patients with liver cirrhosis: a prospective, randomized study. J Laparoendosc Adv Surg Tech A. 2010;20:405–409. doi: 10.1089/lap.2009.0476. [DOI] [PubMed] [Google Scholar]
- 53.Gugenheim J, Casaccia M, Mazza D, Toouli J, Laura V, Fabiani P, et al. Laparoscopic cholecystectomy in cirrhotic patient. HPB Surg. 1996;10:79–82. doi: 10.1155/1996/67964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Friel CM, Stack J, Forse A, Babineau TJ. Laparoscopic cholecystectomy in patients with hepatic cirrhosis: a five-year experience. J Gastrointest Surg. 1999;3:286–291. doi: 10.1016/s1091-255x(99)80070-5. [DOI] [PubMed] [Google Scholar]
- 55.Fernandes NF, Schwesinger WH, Hilsenbeck SG, Gross GW, Bay MK, Sirinek KR, et al. Laparoscopic cholecystectomy and cirrhosis: a case–control study of outcomes. Liver Transpl. 2000;6:340–344. doi: 10.1053/lv.2000.6353. [DOI] [PubMed] [Google Scholar]
- 56.El-Awadi S, El-Nakeeb A, Youssef T, Fikry A, Abd El-Hamed TM, Ghazy H, et al. Laparoscopic versus open cholecystectomy in cirrhotic patients: a prospective randomized study. Int J Surg. 2009;7:66–69. doi: 10.1016/j.ijsu.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 57.El Nakeeb A, Askar W, El Lithy R, Farid M. Clipless laparoscopic cholecystectomy using the harmonic scalpel for cirrhotic patients: a prospective randomized study. Surg Endosc. 2010;24:2536–2541. doi: 10.1007/s00464-010-0999-9. [DOI] [PubMed] [Google Scholar]
- 58.Dunnington G, Alfrey E, Sampliner R, Kogan F, Putnam C. Natural history of cholelithiasis in patients with alcoholic cirrhosis (cholelithiasis in cirrhotic patients) Ann Surg. 1987;205:226–229. doi: 10.1097/00000658-198703000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Delis S, Bakoyiannis A, Madariaga J, Bramis J, Tassopoulos N, Dervenis C. Laparoscopic cholecystectomy in cirrhotic patients: the value of MELD score and Child–Pugh classification in predicting outcome. Surg Endosc. 2010;24:407–412. doi: 10.1007/s00464-009-0588-y. [DOI] [PubMed] [Google Scholar]
- 60.da Silveira EB. Outcome of cirrhotic patients undergoing cholecystectomy: applying Bayesian analysis in gastroenterology. J Gastroenterol Hepatol. 2006;21:958–962. doi: 10.1111/j.1440-1746.2006.04227.x. [DOI] [PubMed] [Google Scholar]
- 61.D'Albuquerque LA, de Miranda MP, Genzini T, Copstein JL, de Oliveira e Silva A. Laparoscopic cholecystectomy in cirrhotic patients. Surg Laparosc Endosc. 1995;5:272–276. [PubMed] [Google Scholar]
- 62.Curro G, Iapichino G, Melita G, Lorenzini C, Cucinotta E. Laparoscopic cholecystectomy in Child–Pugh class C cirrhotic patients. JSLS. 2005;9:311–315. [PMC free article] [PubMed] [Google Scholar]
- 63.Cobb WS, Heniford BT, Burns JM, Carbonell AM, Matthews BD, Kercher KW. Cirrhosis is not a contraindication to laparoscopic surgery. Surg Endosc. 2005;19:418–423. doi: 10.1007/s00464-004-8722-3. [DOI] [PubMed] [Google Scholar]
- 64.Clark JR, Wills VL, Hunt DR. Cirrhosis and laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11:165–169. [PubMed] [Google Scholar]
- 65.Bingener J, Cox D, Michalek J, Mejia A. Can the MELD score predict perioperative morbidity for patients with liver cirrhosis undergoing laparoscopic cholecystectomy? Am Surg. 2008;74:156–159. [PubMed] [Google Scholar]
- 66.Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20:641–654. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 67.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.National Institutes of Health. National Institutes of Health consensus development conference statement on gallstones and laparoscopic cholecystectomy. Am J Surg. 1993;165:390–398. doi: 10.1016/s0002-9610(05)80929-8. [DOI] [PubMed] [Google Scholar]
- 69.Teh SH, Nagorney DM, Stevens SR, Offord KP, Therneau TM, Plevak DJ, et al. Risk factors for mortality after surgery in patients with cirrhosis. Gastroenterology. 2007;132:1261–1269. doi: 10.1053/j.gastro.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 70.Befeler AS, Palmer DE, Hoffman M, Longo W, Solomon H, Di Bisceglie AM. The safety of intra-abdominal surgery in patients with cirrhosis: Model for End-stage Liver Disease score is superior to Child–Turcotte–Pugh classification in predicting outcome. Arch Surg. 2005;140:650–654. doi: 10.1001/archsurg.140.7.650. discussion 655. [DOI] [PubMed] [Google Scholar]
- 71.Neeff H, Mariaskin D, Spangenberg HC, Hopt UT, Makowiec F. Perioperative mortality after non-hepatic general surgery in patients with liver cirrhosis: an analysis of 138 operations in the 2000s using Child and MELD scores. J Gastrointest Surg. 2011;15:1–11. doi: 10.1007/s11605-010-1366-9. [DOI] [PubMed] [Google Scholar]
- 72.Lucidi V, Buggenhout A, Donckier V. Cholecystectomy in cirrhotic patients: pitfalls and reasonable recommendations. Acta Chir Belg. 2009;109:477–480. doi: 10.1080/00015458.2009.11680463. [DOI] [PubMed] [Google Scholar]
- 73.Salkini MW, Doarn CR, Kiehl N, Broderick TJ, Donovan JF, Gaitonde K. The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol. 2010;24:99–102. doi: 10.1089/end.2009.0307. [DOI] [PubMed] [Google Scholar]
- 74.Votanopoulos K, Brunicardi FC, Thornby J, Bellows CF. Impact of three-dimensional vision in laparoscopic training. World J Surg. 2008;32:110–118. doi: 10.1007/s00268-007-9253-6. [DOI] [PubMed] [Google Scholar]
- 75.Blettner M, Sauerbrei W, Schlehofer B, Scheuchenpflug T, Friedenreich C. Traditional reviews, meta-analyses and pooled analyses in epidemiology. Int J Epidemiol. 1999;28:1–9. doi: 10.1093/ije/28.1.1. [DOI] [PubMed] [Google Scholar]
- 76.Bravata DM, Olkin I. Simple pooling versus combining in meta-analysis. Eval Health Prof. 2001;24:218–230. doi: 10.1177/01632780122034885. [DOI] [PubMed] [Google Scholar]
- 77.Singhal T, Balakrishnan S, Hussain A, Nicholls J, Grandy-Smith S, El-Hasani S. Laparoscopic subtotal cholecystectomy: initial experience with laparoscopic management of difficult cholecystitis. Surgeon. 2009;7:263–268. doi: 10.1016/s1479-666x(09)80002-4. [DOI] [PubMed] [Google Scholar]
- 78.Philips JA, Lawes DA, Cook AJ, Arulampalam TH, Zaborsky A, Menzies D, et al. The use of laparoscopic subtotal cholecystectomy for complicated cholelithiasis. Surg Endosc. 2008;22:1697–1700. doi: 10.1007/s00464-007-9699-5. [DOI] [PubMed] [Google Scholar]
- 79.Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 2006;5:584–589. [PubMed] [Google Scholar]
- 80.Soleimani M, Mehrabi A, Mood ZA, Fonouni H, Kashfi A, Buchler MW, et al. Partial cholecystectomy as a safe and viable option in the emergency treatment of complex acute cholecystitis: a case series and review of the literature. Am Surg. 2007;73:498–507. [PubMed] [Google Scholar]
- 81.Chowbey PK, Venkatasubramanian R, Bagchi N, Sharma A, Khullar R, Soni V, et al. Laparoscopic cholecystostomy is a safe and effective alternative in critically ill patients with acute cholecystitis: two cases. J Laparoendosc Adv Surg Tech A. 2007;17:43–46. doi: 10.1089/lap.2006.05078. [DOI] [PubMed] [Google Scholar]
- 82.Klimberg S, Hawkins I, Vogel SB. Percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Am J Surg. 1987;153:125–129. doi: 10.1016/0002-9610(87)90212-1. [DOI] [PubMed] [Google Scholar]
- 83.Berman M, Nudelman IL, Fuko Z, Madhala O, Neuman-Levin M, Lelcuk S. Percutaneous transhepatic cholecystostomy: effective treatment of acute cholecystitis in high risk patients. Isr Med Assoc J. 2002;4:331–333. [PubMed] [Google Scholar]
- 84.Tang B, Cuschieri A. Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg. 2006;10:1081–1091. doi: 10.1016/j.gassur.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 85.O'Regan D, Tait P. Imaging of the jaundiced patient. Hosp Med. 2005;66:17–22. doi: 10.12968/hmed.2005.66.1.17530. [DOI] [PubMed] [Google Scholar]
- 86.Foley WD, Quiroz FA. The role of sonography in imaging of the biliary tract. Ultrasound Q. 2007;23:123–135. doi: 10.1097/01.ruq.0000263851.53549.a5. [DOI] [PubMed] [Google Scholar]
- 87.Itoi T, Wang HP. Endoscopic management of bile duct stones. Dig Endosc. 2010;22(Suppl. 1):69–75. doi: 10.1111/j.1443-1661.2010.00953.x. [DOI] [PubMed] [Google Scholar]
- 88.Artifon EL, et al. Management of common bile duct stones in cirrhotic patients with coagulopathy: a comparison of supra-papillary puncture and standard cannulation technique. Dig Dis Sci. 2011;56:1904–1911. doi: 10.1007/s10620-011-1593-2. [DOI] [PubMed] [Google Scholar]
- 89.Sugiyama M, Atomi Y, Kuroda A, Muto T. Treatment of choledocholithiasis in patients with liver cirrhosis. Surgical treatment or endoscopic sphincterotomy? Ann Surg. 1993;218:68–73. doi: 10.1097/00000658-199307000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aranha GV, Kruss D, Greenlee HB. Therapeutic options for biliary tract disease in advanced cirrhosis. Am J Surg. 1988;155:374–377. doi: 10.1016/s0002-9610(88)80085-0. [DOI] [PubMed] [Google Scholar]
- 91.Hurwitz ES, Holman RC, Strine TW, Chorba TL. Chronic liver disease mortality in the United States, 1979 through 1989. Am J Public Health. 1995;85:1256–1260. doi: 10.2105/ajph.85.9.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Singh GK, Hoyert DL. Social epidemiology of chronic liver disease and cirrhosis mortality in the United States, 1935–1997: trends and differentials by ethnicity, socioeconomic status, and alcohol consumption. Hum Biol. 2000;72:801–820. [PubMed] [Google Scholar]
- 93.Evans RW. Liver transplants and the decline in deaths from liver disease. Am J Public Health. 1997;87:868–869. doi: 10.2105/ajph.87.5.868. [DOI] [PMC free article] [PubMed] [Google Scholar]


