Abstract
Objectives
Single-incision laparoscopic cholecystectomy (SILC) may be associated with less pain, shorter hospital stay and better cosmetic results than multiport laparoscopic cholecystectomy (MLC). Advocates suggest that patients prefer SILC, although research directly addressing the question of patient preferences is limited. This study aimed to assess patient preferences using currently available evidence.
Methods
Patients awaiting elective cholecystectomy were shown a series of postoperative images taken after SILC or MLC and asked which procedure this led them to prefer. This was repeated after patients had completed a questionnaire constructed using published objective data comparing patient-reported outcomes of SILC and MLC.
Results
The study was completed by 113 consecutive patients. After their initial viewing of the images, 16% of subjects preferred MLC. Younger age, lower body mass index and female sex were associated with choosing SILC. After completing the questionnaire, 88% of patients preferred MLC (P < 0.001). Patients ranked the level of risk for complications and postoperative pain above cosmetic results in determining their choice of procedure.
Conclusions
Patients' initial preference when presented with cosmetic appearance was for SILC. When contemporary outcome data were included, the majority chose MLC. This underlines the need to fully inform patients during the consent process and indicates that patient views of SILC may differ from the views of those introducing the technology.
Keywords: laparoscopic, cholecystectomy, single-incision laparoscopy, SILC, patient-centred, cosmetic
Introduction
Multiport laparoscopic cholecystectomy (MLC) presented a paradigm shift away from open cholecystectomy as it was associated with enhanced recovery, decreased postoperative pain and no increase in risk for major complications such as bile duct injury.1
Single-incision laparoscopic cholecystectomy (SILC) has the potential to further revolutionize the method by which cholecystectomy is performed. Proponents of SILC consider that patients would prefer the single-port procedure because it facilitates a decrease in postoperative pain and an improved cosmetic outcome, and present observational data supporting this.2,3 It is also argued that the technique is driving development and improvements in the technology of laparoscopic surgery.4 However, few randomized trials comparing SILC with MLC have been conducted.5 Pooled observational data detailing outcomes including pain scores, duration of hospital stay, time between operation and restarting work, and complications including wound infection and bile duct injury have been presented in meta-analyses and case series.6–12 These data give conflicting messages about the benefits of SILC over MLC, and National Institute for Health and Clinical Excellence (NICE) guidelines suggest that the only potential benefit of SILC to the patient is cosmetic,13 despite a current lack of evidence that patients are dissatisfied with cosmetic outcomes following MLC.14
In the absence of a robust comparison of the respective outcomes of SILC and MLC, and evidence suggesting that SILC is associated with higher rates of complications, it is essential to obtain the views of patients upon the potential benefits of SILC. This study used data describing the outcomes of multi- and single-port cholecystectomy to identify the opinions of a cohort of patients scheduled to undergo cholecystectomy.
Materials and methods
This was a prospective study of consecutive patients scheduled to undergo elective laparoscopic cholecystectomy (LC). Study participants were identified over a 3-month period between January and March 2011. Patient age, gender, ethnicity and body mass index (BMI) were recorded. Participants were eligible for inclusion if they had been diagnosed with symptomatic gallstone disease and if they had expressed the wish to undergo LC after participating in discussion of surgical vs. non-operative management strategies. Patients were excluded if they were scheduled for emergency LC because this is not presently widely performed using SILC.15
The study was conducted prior to any discussion with patients of the MLC technique and thus prior to obtaining patient consent. It was explained to participants that cholecystectomy can be performed using either of two laparoscopic techniques (MLC and SILC).
Subjects were first shown postoperative images of patients who had undergone SILC or MLC and asked which procedure this led them to prefer. This was repeated after patients had completed a questionnaire and their preferences after this second round of viewing were compared with their initial responses. The colour photographs of the abdomens of patients who had undergone either SILC or MLC were presented on laminated A4 paper. The images showed two patients who had undergone SILC; the incision in one of these patients was transumbilical and that in the other was supraumbilical. Subjects in the photographs also included a single patient who had undergone MLC conducted using a four-port technique. This patient's abdomen showed 12-mm epigastric and umbilical scars and two right upper quadrant scars from 7-mm ports. All patients were photographed in the early postoperative period and again after 6 weeks. All wounds had healed without complication.
Between their first and second viewings of the images, subjects completed a questionnaire constructed using two components. The first component used available data describing patient-reported outcomes or aspects of cholecystectomy. These were presented as statements in the questionnaire comparing MLC with SILC. Data were sourced from articles by Allemann et al.11 and Lee et al.12 and covered cosmetic outcomes, postoperative pain and recovery times, operative variables and complications (described in detail in Tables 1 and 2). Participants were asked to state how ‘acceptable’ they felt each statement was for MLC and SILC, on a scale of 1–5, where 1 = not at all acceptable and 5 = very acceptable. Patients were talked through complications to explain common bile duct injury and wound complications using lay terminology. The same descriptions were given to every patient to avoid any influence of differences on outcome. The second component of the questionnaire explored issues relevant to the introduction of SILC and how acceptable these might be to a patient (i.e. that surgeons are learning a new technique, that the operation is technically more difficult and that SILC is more expensive than MLC). Subjects were then asked to state again which procedure (SILC or MLC) they would prefer.
Table 1.
Acceptability rankings awarded by study participants on data comparing multiport laparoscopic cholecystectomy (MLC) with single-incision laparoscopic cholecystectomy (SILC) (using data obtained from a critical review11 and a randomized controlled trial12)
| Theme | Operation | Statement presented | Median acceptabilitya | IQR | P-valueb |
|---|---|---|---|---|---|
| Cosmetic result | MLC | Two 7-mm and two 12-mm incisionsc | 3.5 | 3–4 | <0.001 |
| SILC | One 14–18-mm umbilical incision16 | 4.0 | 3–5 | ||
| Pain and recovery | MLC | Average pain score: 2.2/1012 | 4.0 | 4–5 | <0.01 |
| SILC | Average pain score: 2.1/1012 | 4.0 | 4–5 | ||
| MLC | Return to work in 5.9 days12 | 4.0 | 3–5 | <0.01 | |
| SILC | Return to work in 5.3 days12 | 4.0 | 4–5 | ||
| Operation and technique | MLC | Average operation duration: 50 min12 | 4.0 | 3–5 | <0.001 |
| SILC | Average operation duration: 70 min12 | 3.0 | 3–3 | ||
| MLC | Established and widely practised technique12 | 4.0 | 4–5 | <0.001 | |
| SILC | New technique, practised in few centres; advancing technology11 | 3.0 | 3–3 | ||
| Complications | MLC | Overall complication rate: less than one in 100 patients11 | 4.0 | 4–5 | <0.001 |
| SILC | Overall complication rate: five in 100 patients11 | 3.0 | 2–3 | ||
| MLC | Common bile duct injuries: two in 1000 patients11 | 4.0 | 4–5 | <0.001 | |
| SILC | Common bile duct injuries: seven in 1000 patients11 | 3.0 | 2–3 | ||
| MLC | Wound complications: five in 1000 patients11 | 4.0 | 4–5 | <0.001 | |
| SILC | Wound complication: two to 10 in 100 patients11 | 2.0 | 1–3 | ||
Acceptability scores: 1 = not at all acceptable; 5 = very acceptable.
Mann–Whitney U-test. P-values are significant at P < 0.01 and P < 0.001.
IQR, interquartile range.
Based on local practice using 2 × 7-mm and 2 × 12-mm Applied Medical (R) ports in MLC.
Table 2.
Acceptability rankings awarded by study participants on independent and more subjective factors linked to multiport laparoscopic cholecystectomy (MLC) or single-incision laparoscopic cholecystectomy (SILC)
| Operation | Statement presented | Median acceptabilitya | IQR |
|---|---|---|---|
| SILC | Surgeons are learning a new technique11 | 4.0 | 3–4 |
| SILC | Technically more difficult17 | 3.0 | 2–3 |
| MLC | Cheaper11 | 4.0 | 3–5 |
Acceptability scores: 1 = not at all acceptable; 5 = very acceptable.
IQR, interquartile range.
The final component of the study was the presentation of a set of eight factors that we believe to be important when considering a surgical procedure; these were ranked by the study participants in order of importance. These factors were: complications; cosmetic result; cost of the procedure to the National Health Service (NHS); whether the surgeon was in the process of learning or consolidating the procedure; operation duration; novelty of the procedure (i.e. whether it is important to the patient that he or she undergoes a newer, potentially high-profile technique); number of surgical incisions, and postoperative pain. In order to avoid any bias imposed by the personal opinion of the researcher administering the questionnaire, the researcher did not offer any opinion on the merits or disadvantages of either technique to the patient if asked.
Statistical analysis
The study hypothesis was that patients would prefer SILC over MLC. It was assumed that cosmetic result and postoperative pain would strongly influence patient perspectives.
Data were analysed using the Mann–Whitney U-test, the chi-squared test, repeated measures analysis of variance (anova) test and correlation coefficients as appropriate. spss Version 18 (SPSS, Inc., Chicago, IL, USA) was used to perform statistical analysis.
Results
Over the period of 3 months, 113 patients were approached and all participated in the study. The median age of the cohort was 50 years (range: 19–86 years). The cohort included 85 (75%) women. The median BMI was 28 kg/m2 (range: 19–47 kg/m2). Eighty-six patients (76%) were White.
Patient preferences
On their initial inspection of the images of patients who had previously undergone SILC or MLC, 57% of study participants preferred the option of SILC, 27% had no preference and 16% preferred MLC. After completing the questionnaire, 10% of patients stated they would prefer SILC, 2% had no preference and 88% said they would select MLC (repeated measures anova, P < 0.001).
Women were more likely than men to select SILC after their initial inspection of the images. At their first inspection, 61%, 19% and 20% of women stated preferences for SILC, MLC and no preference, respectively, compared with 38%, 17% and 45%, respectively, of men (chi-squared test, P = 0.018).
Younger age and low BMI were also associated with an initial choice of SILC (R = 0.58 and R = 0.96, respectively). Older age was associated with a tendency for no preference (R = 0.78).
All the patients (n = 13) who stated a preference for SILC after completing the questionnaire had chosen SILC initially. The median age of this group was 36 years (range: 21–68 years). Their median BMI was 27 kg/m2 (range: 19–35 kg/m2). Ten of the 13 subjects were female.
Comparison of SILC with MLC: patient-reported outcomes and operative variables
After reviewing objective data comparing SILC with MLC, study participants gave higher acceptability scores to SILC compared with MLC with respect to pain (P < 0.01), duration of time off work (P < 0.01) and number of incisions (P < 0.001). Acceptability scores were higher for MLC than SILC with regard to operation duration, that MLC is an established procedure as opposed to a new technique being introduced, overall complication rate, risk for bile duct injury and risk for wound infection (all P < 0.001) (Table 1).
Patient perspectives on the introduction of SILC
Subjects appeared receptive to the introduction of new technology. The median score for acceptability of the fact that surgeons are learning a new technique was 4 [interquartile range (IQR): 3–4]. Most patients were not concerned that the technique is technically more difficult than MLC (median acceptability score = 3; IQR: 2–3). However, subjects generally favoured conventional MLC over SILC in terms of cost-effectiveness (to the NHS) (median score = 4; IQR: 3–5) (Table 2).
Factors influencing choice of operation
Subjects ranked the risk for complications (median ranking = 1; IQR: 1–2) and pain (median ranking = 2; IQR: 1–2) as more important than the number of incisions (median ranking = 3; IQR: 3–5) and cosmetic outcome (median ranking = 5; IQR: 4–7) in their choice of operation. Cosmesis was given median rankings of 5 by women and 6 by men (P < 0.005). Subjects did not appear to be concerned that the surgeon might be on a ‘learning curve’ for the procedure (median ranking = 6; IQR: 5–6). The least important variable presented to subjects was novelty of the procedure (median ranking = 8; IQR: 7–8) (Fig. 1).
Figure 1.
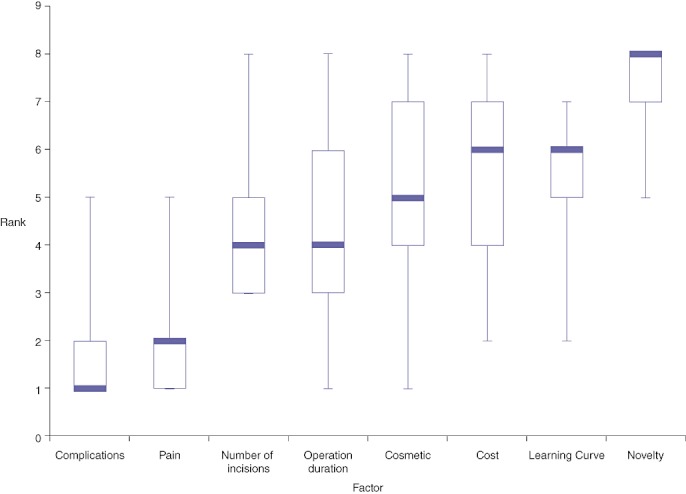
Study subjects' rankings of eight variables relevant in the consideration of an operation. 1 = most important, 8 = least important. Data are expressed as the median ranking (bold line), first and third interquartile ranges (lower and upper limits of the box) and minimum and maximum scores (lowest and highest limits) for each factor
Discussion
Recent developments in laparoscopic surgery have led to the introduction of SILC, although its use is currently limited to a few centres. Technical hurdles for surgeons and the probable increase in cost associated with SILC may partly explain why the procedure has failed to become widely adopted.11 Given the potential advantages of decreased postoperative pain and improved cosmetic outcome, the use of SILC might be expected to be driven by patient choice. To the authors' knowledge, this opinion has been neglected to date; this study therefore aimed to identify patient preferences in the choice between MLC and SILC. The study was undertaken using a series of postoperative photographs of subjects who had undergone SILC or MLC and a questionnaire compiled using objective published data.
The study found that the majority of subjects scheduled for elective cholecystectomy would prefer SILC over MLC based on postoperative cosmetic appearance alone. However, when various outcomes including recovery times and cosmetic scores (favouring SILC) and complications (favouring MLC) were considered, subjects preferred MLC. Furthermore, subjects ranked the risk for complications and pain as more important than the number of incisions and cosmetic outcome. This indicates that in order for SILC to become widely accepted, improved wound infection rates and a risk for bile duct injury equivalent to that in MLC need to be demonstrated. It may be that the rate of bile duct injury will fall as surgeons become more familiar with SILC in the same way that it did in MLC when the latter succeeded open cholecystectomy. Patients are also receptive towards the idea that it is necessary for surgeons to embark on a learning curve in surgery, as shown by the high acceptability of the fact that surgeons performing SILC are learning a new technique.
Subjects who initially selected SILC were more likely to be female, younger and to have a lower BMI. These characteristics may define a potential target group for the wider introduction of this operation.
It was interesting to observe that number of incisions was ranked as more important than cosmetic result. This suggests that patients do see the value of fewer incisions, but not necessarily on the grounds of cosmetic reasoning.
Limitations of the study include its use of a non-validated questionnaire. A validated questionnaire for this type of research does not exist and the design of the present study required that specific aspects of patient perspectives be explored using contemporary data. To avoid bias, the authors used objective data available at the time of study design. Furthermore, the researchers did not offer their personal opinions to the study subjects.
As new data describing the outcomes of SILC become available, the results of this work should be reviewed. Given the lack of randomized trials of SILC vs. MLC, patients' views should be sought prior to selection for SILC or MLC. It appears that patients prefer a good cosmetic result, but not at the expense of higher rates of postoperative complications. If newer studies were to show lower complication rates in SILC, patients' final choices of which operation they would prefer might well alter. The present study therefore highlights the need for clearer and more robust evidence relating to complication rates, and in direct comparison with MLC. This remains an important factor in patient choice and one which will affect the ability of SILC as a technique to break into wider use. The value of the patient's opinion should not be underestimated.
Conclusions
This study highlights the importance of giving full information to a patient who is in the process of choosing between intervention options and subsequently giving consent. In the present study, when patients were naïve of available factual data, they preferred the cosmetic outcome of SILC over MLC. However, when they were able to consider fuller data comparing SILC with MLC, the majority chose MLC. More rigorous studies are needed to establish the potential benefits of SILC and quantify the relative risks associated with the procedure. Decisions on whether to implement SILC on a wider scale must take patient perspectives into account and, where SILC is offered, patients should be adequately informed of its potential benefits and complications.
Conflicts of interest
None declared.
References
- 1.Keus F, Gooszen HG, Van Laarhoven CJHM. Systematic review: open, small-incision or laparoscopic cholecystectomy for symptomatic cholecystolithiasis. Aliment Pharmacol Ther. 2008;29:359–378. doi: 10.1111/j.1365-2036.2008.03894.x. [DOI] [PubMed] [Google Scholar]
- 2.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009;23:1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 3.Gumbs AA, Milone L, Sinha P, Bessler M. Totally transumbilical laparoscopic cholecystectomy. J Gastrointest Surg. 2009;13:533–534. doi: 10.1007/s11605-008-0614-8. [DOI] [PubMed] [Google Scholar]
- 4.Kommu SS, Rané A. Devices for laparoendoscopic single-site surgery in urology. Expert Rev Med Devices. 2009;6:95–103. doi: 10.1586/17434440.6.1.95. [DOI] [PubMed] [Google Scholar]
- 5.Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010;24:1842–1848. doi: 10.1007/s00464-010-0887-3. [DOI] [PubMed] [Google Scholar]
- 6.Phillip SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009;209:632–637. doi: 10.1016/j.jamcollsurg.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009;75:681–685. [PubMed] [Google Scholar]
- 8.Rao PP, Bhagwat SM, Rane A, Rao PP. The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB. 2008;10:336–340. doi: 10.1080/13651820802276622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech. 2009;19:495–499. doi: 10.1089/lap.2008.0424. [DOI] [PubMed] [Google Scholar]
- 10.Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Praveenraj P. Transumbilical flexible endoscopic cholecystectomy in humans: first feasibility study using a hybrid technique. Endoscopy. 2008;40:428–431. doi: 10.1055/s-2007-995742. [DOI] [PubMed] [Google Scholar]
- 11.Allemann P, Schafer M, Demartines N. Critical appraisal of single port access cholecystectomy. Br J Surg. 2010;97:1476–1480. doi: 10.1002/bjs.7189. [DOI] [PubMed] [Google Scholar]
- 12.Lee P-C, Lo C, Lai P-S, Chang J-J, Huang S-J, Lin M-T, et al. Randomized clinical trial of single-incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg. 2010;97:1007–1012. doi: 10.1002/bjs.7087. [DOI] [PubMed] [Google Scholar]
- 13.National Institute for Health and Clinical Evidence. 2010. Single-incision laparoscopic cholecystectomy: guidance. IPG346. http://www.nice.org.uk/nicemedia/live/12237/48780/48780.pdf. [Accessed 17 June 2011]
- 14.Rhodes M. Critical appraisal of single port access cholecystectomy. Br J Surg. 2010;97:1476–1480. doi: 10.1002/bjs.7190. [DOI] [PubMed] [Google Scholar]
- 15.Antoniou SA, Pointner R, Granderath FA. Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc. 2011;25:367–377. doi: 10.1007/s00464-010-1217-5. [DOI] [PubMed] [Google Scholar]
- 16.Bhandarkar D, Mittal G, Shah R, Katara A, Udwadia TE. Single-incision laparoscopic cholecystectomy: how I do it. J Min Access Surg. 2011;7:17–23. doi: 10.4103/0972-9941.72367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rawlings A, Hodgett SE, Matthews BD, Strasberg SM, Quasebarth M, Brunt LM. Single-incision laparoscopic cholecystectomy: initial experience with critical view of safety dissection and routine intraoperative cholangiography. J Am Coll Surg. 2010;211:1–7. doi: 10.1016/j.jamcollsurg.2010.02.038. [DOI] [PubMed] [Google Scholar]


