Abstract
Background
The present study is a meta-analysis of English articles comparing one-stage [laparoscopic common bile duct exploration or intra-operative endoscopic retrograde cholangiopancreatography (ERCP)] vs. two-stage (laparoscopic cholecystectomy preceded or followed by ERCP) management of common bile duct stones.
Methods
MEDLINE/PubMed and Science Citation Index databases (1990–2011) were searched for randomized, controlled trials that met the inclusion criteria for data extraction. Outcomes were calculated as odds ratios (ORs) with 95% confidence intervals (CIs) using RevMan 5.1.
Results
Nine trials with 933 patients were studied. No significant differences was observed between the two groups with regard to bile duct clearance (OR, 0.89; 95% CI, 0.65–1.21), mortality (OR, 1.2; 95% CI, 0.32–4.52), total morbidity (OR, 0.75; 95% CI, 0.53–1.06), major morbidity (OR, 0.95; 95% CI, 0.60–1.52) and the need for additional procedures (OR, 1.58; 95% CI, 0.76–3.30).
Conclusions
Outcomes after one-stage laparoscopic/endoscopic management of bile duct stones are no different to the outcomes after two-stage management.
Keywords: surgery, cholelithiasis, endoscopy, choledocholithiasis, common bile duct stones, ERCP
Introduction
Common bile duct (CBD) stones are present in 3.4–7.2% of patients presenting for a cholecystectomy.1–3
With the increasing availability and use of magnetic resonance cholangio-pancreatography (MRCP) and endoscopic ultrasound (EUS) for the accurate pre-operative prediction of choledocholithiasis, there is no clear consensus regarding the optimal management strategy of CBD stones. The authors previous meta-analysis in 20064 comparing endoscopy and surgery vs. surgery alone for the management of CBD stones concluded that similar outcomes could be achieved with either approach. Since this time, five randomized trials have been published.5–9 Therefore the aim of the present study was to update the previous meta-analysis2 but on this occasion compare one-stage management [laparoscopic cholecystectomy (LC) plus laparoscopic common bile duct exploration (LCBDE) OR intra-operative ERCP) with two-stage management [laparoscopic cholecystectomy preceded or followed by endoscopic retrograde cholangiopancreatography (ERCP)].
Methods
This meta-analysis was conducted according to the recommendations of the PRISMA statement for reporting systematic reviews and meta-analyses.10
Eligibility criteria for study selection
Publications were selected for review if they compared, in a prospective, randomized, controlled way, two-stage laparoscopic/ endoscopic management [ERCP proceeded or followed by LC] vs. one stage management (LCBDE or intra-operative ERCP) of CBD stones in adults. Included are only documents published in English (including one study with an in press status) between 1990 and 2011.
Information sources and search strategy
Relevant studies were identified by searching databases, lists of articles and communication with experts. The electronic search was applied to MEDLINE/PubMed and Science Citation Index databases. Databases were searched from 1990 to 2011 for records in English. The last search was run on 15 June 2011.
A hand-based search of reference lists of published articles and review articles was performed to ensure inclusion of all possible studies and exclude duplicates. Experts were also contacted to acquire information for accepted articles or articles in press.
The following search items were used: common bile duct stones/-calculi; bile duct stones/calculi; ERCP; endoscopic sphincterotomy; and laparoscopic ductal clearance/choledochotomy/bile duct exploration.
Study selection
Eligibility assessment for selecting studies for inclusion in the meta-analysis was performed independently by the two authors. Disagreements were resolved by consensus.
Data extraction and collection
Data were extracted using a standardized electronic form. The primary outcomes used for meta-analysis were: successful duct clearance, mortality, total morbidity (number of patients with at least one complication), major morbidity (sepsis, cholangitis, clinical pancreatitis, pneumonia, bleeding, acute myocardial infarction, stroke, pulmonary embolus, early reoperation and conversion to open surgery in the LCBDE group) and additional procedures (any endoscopy or surgery for failed CBD clearance or management of complications). Data were analysed on an intention-to-treat basis.
Assessment of methodological quality and risk of bias
Each included trial was assessed for quality using the CONSORT checklist for reporting randomized trials.11 A point was given for each criterion that was met (maximum score is 22).
Statistical analysis
A meta-analysis was performed using Review Manager Version 5.1 (The Nordic Cochrane Centre, Copenhagen, Denmark). For dichotomous variables, odds ratios (OR) with 95% confidence intervals (95% CI) were calculated. Fixed-effect and random-effects models (owing to a number of small studies) were used. In case of discrepancy between the two models, the random effects results are reported; otherwise only the results of the fixed-effect model are reported. The level of significance was set at P < 0.050. Heterogeneity was evaluated using the I2-value. A funnel plot was constructed to determine if there was any publication bias.
Results
The search strategy identified nine randomized trials5–9,12–15 (Fig. 1). Four studies compared ERCP followed by LC against laparoscopic CBD surgery,5,7,8,12 two studies compared LC followed by ERCP against laparoscopic CBD surgery13,14 and two studies compared ERCP+LC against LC plus intra-operative ERCP.6,9
Figure 1.
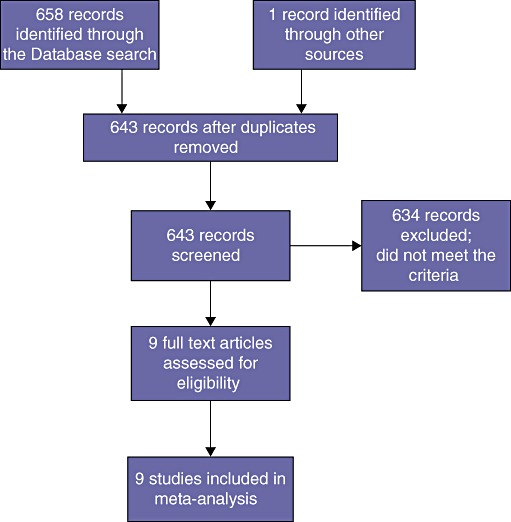
Flow chart of the selection of studies eligible for data extraction and analysis
The median (range) CONSORT score was 20 (17–21).
Outcomes for 933 patients (462 (49.5%) in the one-stage management and 471 (50.5%) in the two-stage management group) were examined (Table 1). Forrest plots (Figs 2–6) were constructed comparing successful duct clearance, mortality, total morbidity, major morbidity and the need for additional procedures for the two-stage vs. the one-stage management group. Heterogeneity between studies was not significant or moderately significant as shown in the individual figures.
Table 1.
Summary of randomized trials comparing two-stage (endoscopic common duct clearance and laparoscopic cholecystectomy) vs. one-stage (laparoscopic surgery alone or combined with intra-operative endoscopy)
| Study | Author | Year | Treatment | n | Duct clearance successful | Mortality | Morbidity (Total) | Morbidity (Major) | Additional procedures required | Length of stay (median, days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Rhodes | 1998 | LC+ERCP | 40 | 37 | 0 | 6 | 4 | 10 | 3.5 |
| LC+LCBDE | 40 | 30 | 0 | 7 | 2 | 10 | 1 | |||
| 2 | Cuschieri | 1999 | ERCP+LC | 133 | 82 | 2 | 17 | 9 | 17 | 9 |
| LC+LCBDE | 133 | 92 | 1 | 21 | 9 | 17 | 6 | |||
| 3 | Sgourakis | 2002 | ERCP+LC | 42 | 27 | 1 | 6 | 3 | 5 | 9 |
| LC+LCBDE | 36 | 24 | 1 | 5 | 2 | 4 | 7.4 | |||
| 4 | Nathanson | 2005 | LC+ERCP | 45 | 43 | 0 | 11 | 6 | 3 | 7.7 |
| LC+LCBDE | 41 | 40 | 0 | 12 | 7 | 3 | 6.4 | |||
| 5 | Morino | 2006 | ERCP+LC | 45 | 36 | 0 | 4 | 2 | 15 | 8 |
| LC+ intra-operative ERCP | 46 | 44 | 0 | 5 | 4 | 2 | 4.3 | |||
| 6 | Noble | 2009 | ERCP+LC | 47 | 29 | 1 | 16 | 8 | 18 | 3 (PO stay) |
| LC+LCBDE | 44 | 38 | 0 | 23 | 8 | 0 | 5 (PO stay) | |||
| 7 | Rogers | 2010 | ERCP+LC | 55 | 30 | 0 | 5 | 0 | 1 | 5 |
| LC+LCBDE | 57 | 15 | 0 | 6 | 0 | 2 | 4 | |||
| 8 | Bansal | 2010 | ERCP+LC | 15 | 13 | 0 | 5 | 2 | 2 | 4 |
| LC+LCBDE | 15 | 14 | 0 | 6 | 2 | 1 | 4.2 | |||
| 9 | Tzovaras | 2011 | ERCP+LC | 49 | 45 | 0 | 6 | 5 | 5 | 5.5 |
| LC+ intra-operative ERCP | 50 | 47 | 1 | 7 | 6 | 3 | 4 | |||
| Totals | ||||||||||
| Two stage (endoscopy followed by Surgery) | 471 | 342 (72.6%) | 4 (0.8%) | 76 (16.1%) | 39 (8.3%) | 76 (16.1%) | ||||
| One stage (LCBDE or intra-operative endoscopy) | 462 | 344 (74.4%) | 3 (0.6%) | 92 (19.9%) | 40 (8.6%) | 42 (9%) | ||||
LC, laparoscopic cholecystectomy; ERCP, endoscopic retrograde cholangiopancreatography; LCBDE; laparoscopic common bile duct exploration; PO, post-operative stay.
Figure 2.
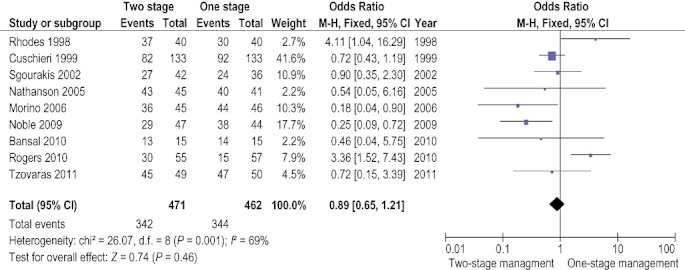
Meta-analysis of successful bile duct clearance (fixed-effects model). Error bars indicate a 95% confidence interval (CI). A summary of effects is shown as a diamond that spans the 95% CI
Figure 6.
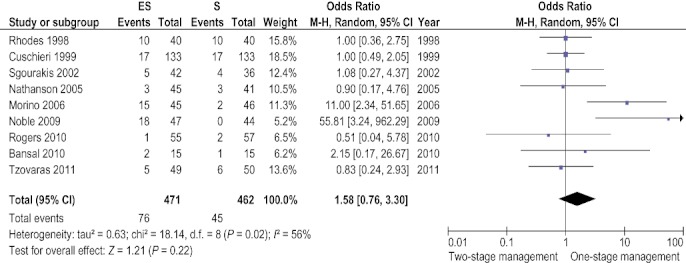
Additional procedures required (Random-effects model). Error bars indicate a 95% confidence interval (CI). A summary of effects is shown as a diamond that spans the 95% CI
Figure 3.
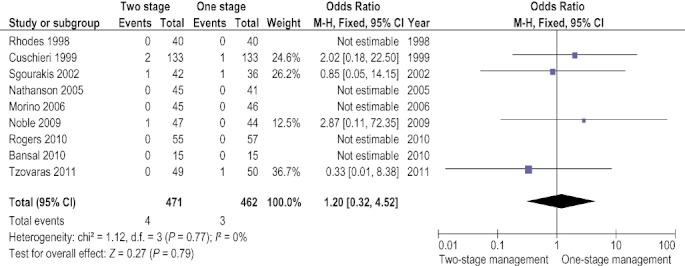
Mortality (fixed-effects model). Error bars indicate a 95% confidence interval (CI). A summary of effects is shown as a diamond that spans the 95% CI
Figure 4.
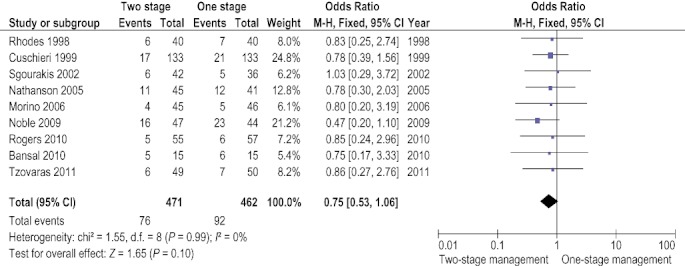
Morbidity (total) (fixed-effects model). Error bars indicate a 95% confidence interval (CI). A summary of effects is shown as a diamond that spans the 95% CI
Figure 5.
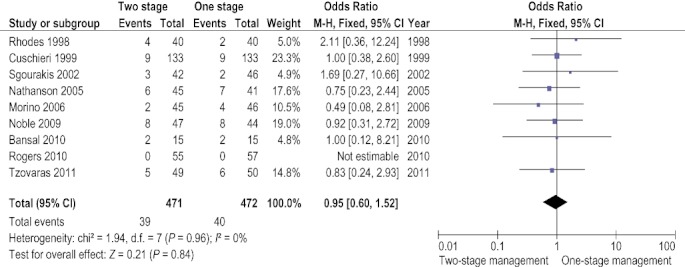
Morbidity (major) (fixed-effects model). Error bars indicate a 95% confidence interval (CI). A summary of effects is shown as a diamond that spans the 95% CI
Successful duct clearance was achieved in 342/471 (72.6%) of patients in the two-stage group and in 344/462 (74.4%) in the one-stage management group. No significant difference between the two groups was observed [OR (fixed) = 0.89 (95% CI = 0.65–1.21), P = 0.46].
Mortality was 4/471 (0.8%) in the two-stage management group and 3/462 (0.6%) in the one-stage management group. No significant difference between the two groups was observed [OR (fixed) = 1.2 (95% CI = 0.32–4.52), P = 0.79].
Total patient morbidity was 76/471 (16.1%) in the two-stage group and 92/462 (19.9%) in the one-stage group. No significant difference between the two groups was observed [OR (fixed) = 0.75 (95%CI = 0.53–1.06), P = 0.10].
Major patient morbidity was 39/471 (8.3%) in the two-stage group and 40/462 (8.6%) in the one-stage group. No significant difference between the two groups was observed [OR (fixed) = 0.95 (95%CI = 0.60–1.52), P = 0.84].
Additional procedures were required in 76/471 (16.1%) in the two-stage group and in 42/462 (9%) in the one-stage management group. No significant difference between the two groups was observed [OR (random) = 1.58 (95% CI = 0.76–3.30), P = 0.22].
Discussion
This meta-analysis shows that both clinical practices (one- vs. two- stage laparoscopic/endoscopic management of CBD stones) have similar clinical outcomes. However, critical review of the studies raised a number of issues.
As previously noted,4 the majority of trials are underpowered. All but two studies8,12 have 50 patients or less in each arm. To detect a 20% (α= 0.05, power = 80%) difference in the rate of bile duct clearance, 100 patients per arm would be required.
Severe complications after ERCP in specialized centres are reported as low as 0.8%16 and was 2.6% in a multi-centre French study.17 The severe complication rate of the two-stage group in the present analysis was 8%. In addition, the ERCP success rate was 87% in the French study17 vs. 73% in the two-stage group of this meta-analysis. This underscores the importance of having an expert ERCP service when dealing with these patients.18
Laparoscopic common bile duct exploration has not found widespread favour amongst the surgical community. It has remained a procedure limited to experienced and/or enthusiastic laparoscopic surgeons. Findings from these randomized trials may not apply to the surgical community at large. A recent survey of >16 000 cholecystectomies in Germany showed that two-stage management was the preferred method in 99% of patients with suspected CBD stones and there was a conversion rate of 43% in patients with an attempted LCBDE.19 In contrast, a survey in the UK among upper gastrointestinal surgeons showed that 61% perform laparoscopic CBD exploration, 25% advise post-operative ERCP and 13% perform either LCBDE or ERCP when they encounter CBD stones.20
Two of the included studies reported cost analysis.6,8 Both found that the two-stage approach had significantly higher costs (1319 USD difference in the USA study and 1005 Euro in the Italian study). A non-randomized trial from Belgium reported that total hospital costs were significantly less after one-stage management (2636 vs. 4608 Euro in the two-stage arm).21 A US analysis of five treatment strategies found that the most cost-effective treatment of CBD stones was LC + intra-operative cholangiography + postoperative ERCP.22 However, cost comparisons are very difficult to make, not only between countries but also between hospitals within a specific country.
The patient population in this meta-analysis is variable. There were differences in the CBD stone diagnosis; some studies used MRC before any intervention,5,6 whereas others used ERC or intra-operative cholangiography.8,12,13 Some studies included patients with acute cholangitis12,13 and others excluded these patients.6,8 It should be noted that patients with cholecysto/choledocholithiasis who undergone CBD stone clearance must undergo a cholecystectomy (unless medically unfit) because of the high risk of recurrent biliary events.23
In conclusion, this meta-analysis shows that the clinical outcome after one-stage laparoscopic/endoscopic management of bile duct stones is no different to the outcome after two-stage management. Strategies can be based on a combination of local expertise and availability of therapeutic resources.
Conflicts of interest
None declared.
References
- 1.Alkhaffaf B, Parkin E, Flook D. Endoscopic retrograde cholangiopancreatography prior to laparoscopic cholecystectomy: a common and potentially hazardous technique that can be avoided. Arch Surg. 2011;146:329–333. doi: 10.1001/archsurg.2011.30. [DOI] [PubMed] [Google Scholar]
- 2.Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan G. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy. Ann Surg. 2004;239:28–33. doi: 10.1097/01.sla.0000103069.00170.9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz D, Nikfarjam M, Sfakiotaki A, Christophi C. Selective endoscopic cholangiography for the detection of common bile duct stones in patients with cholelithiasis. Endoscopy. 2004;36:1045–1049. doi: 10.1055/s-2004-825955. [DOI] [PubMed] [Google Scholar]
- 4.Clayton E, Connor S, Alexakis N, Leandros E. Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg. 2006;93:1185–1191. doi: 10.1002/bjs.5568. [DOI] [PubMed] [Google Scholar]
- 5.Bansal V, Misra M, Garg P, Prabhu M. A prospective randomized trial comparing two-stage versus single-stage management of patients with gallstone disease and common bile duct stones. Surg Endosc. 2010;14:1986–1989. doi: 10.1007/s00464-010-0891-7. [DOI] [PubMed] [Google Scholar]
- 6.Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A. Preoperative endoscopic sphincterotomy versus laparoendoscopic randevous in patients with gallblader and bile duct stones. Ann Surg. 2006;244:889–896. doi: 10.1097/01.sla.0000246913.74870.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noble H, Tranter S, Chesworth T, Norton S, Thompson M. A randomized clinical trial to compare endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy with primary laparoscopic bile duct exploration during cholecystectomy in higher risk patients with choledocholithiasis. J. Laparoendosc Adv Surg Tech. 2009;19:713–720. doi: 10.1089/lap.2008.0428. [DOI] [PubMed] [Google Scholar]
- 8.Rogers S, Cello J, Horn J, Siperstein A, Schecter W, Campbell A, et al. Prospective randomized trial of LC+LCBDE vs ERCP+LC for common bile duct stone disease. Arch Surg. 2010;145:28–33. doi: 10.1001/archsurg.2009.226. [DOI] [PubMed] [Google Scholar]
- 9.Tzovaras G, Baloyiannis I, Zachari E, Symeonidis D, Zacharoulis D, Kapsoritakis A, et al. Laparo-endoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: Interim analysis of a controlled randomized trial. Ann Surg. 2012 doi: 10.1097/SLA.0b013e3182456ec0. (in press) [DOI] [PubMed] [Google Scholar]
- 10.Liberati A, Altman D, Tetzlaff J, Mulrow C, Gotzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Schulz K, Altman D. The consort statement revised recommendation for improving quality of reporting of parallel group randomised controlled trials. JAMA. 2001;285:1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- 12.Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, et al. EAES multi-center prospective randomized trial comparing two stage vs single stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13:952–957. doi: 10.1007/s004649901145. [DOI] [PubMed] [Google Scholar]
- 13.Nathanson L, O'Rourke N, Martin I, Fielding G, Cowen A, Roberts R, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg. 2005;242:188–192. doi: 10.1097/01.sla.0000171035.57236.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhodes M, Sussman L, Cohen L, Lewis M. Randomized trial of laparoscopic exploration of common bile duct versus postoperative ERCP for common bile duct stones. Lancet. 1998;351:159–161. doi: 10.1016/s0140-6736(97)09175-7. [DOI] [PubMed] [Google Scholar]
- 15.Sgourakis G, Karaliotas K. Laparoscopic common bile duct exploration and cholecystectomy versus endoscopic stone extraction and laparoscopic cholecystectomy for choledocholithiasis. A prospective randomized study. Minerva Chir. 2002;57:467–474. [PubMed] [Google Scholar]
- 16.Salminen P, Laine S, Gullichsen R. Severe and fatal complications after ERCP: analysis of 2555 procedures in a single experienced center. Surg Endosc. 2008;22:1965–1970. doi: 10.1007/s00464-007-9711-0. [DOI] [PubMed] [Google Scholar]
- 17.Vitte R, Morfoisse J. Evaluation of endoscopic retrograde cholangiopancreatography procedures performed in general hospitals in France. Gastroenterol Clin Biol. 2007;31:740–749. doi: 10.1016/s0399-8320(07)91936-3. [DOI] [PubMed] [Google Scholar]
- 18.Williams E, Taylor S, Fairclough P, Hamlyn A, Logan R, Martin D, et al. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56:821–829. doi: 10.1136/gut.2006.097543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spelsberg F, Nusser F, Huttl T, Obeidat F, Lang R, Jauch K, et al. [Management of cholecysto- and choledocholithiasis – survey and analysis of 16 615 cholecystectomies and common bile duct explorations in bavaria] Zentralbl Chir. 2009;134:120–126. doi: 10.1055/s-0028-1098879. (in German) [DOI] [PubMed] [Google Scholar]
- 20.Sanjay P, Kulli C, Polignano F, Tait I. Optimal surgical technique, use of intra-operative cholangiography (IOC), and management of acute gallbladder disease: the results of a nation-wide survey in the UK and Ireland. Ann R Coll Surg Engl. 2010;92:302–306. doi: 10.1308/003588410X12628812458617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Topal B, Vromman K, Aerts R, Verslype C, Van Steenbergen W, Penninckx F. Hospital cost categories of one-stage versus two-stage management of common bile duct stones. Surg Endosc. 2010;24:413–416. doi: 10.1007/s00464-009-0594-0. [DOI] [PubMed] [Google Scholar]
- 22.Brown L, Rogers S, Cello J, Brasel K, Inadomi J. Cost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stones. J Am Coll Surg. 2011;212:1049–1060. doi: 10.1016/j.jamcollsurg.2011.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boerma D, Rauws A, Keulemans Y, Janssen I, Bolwerk C, Timmer R, et al. Wait- and- see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile duct stones: a randomized trial. Lancet. 2002;360:761–765. doi: 10.1016/S0140-6736(02)09896-3. [DOI] [PubMed] [Google Scholar]


