Abstract
The effects of androgens on cardiovascular disease (CVD) risk in men remain unclear. To better characterize the relationship between androgens and HDL, we investigated the effects of testosterone replacement on HDL protein composition and serum HDL-mediated cholesterol efflux in hypogonadal men. Twenty-three older hypogonadal men (ages 51–83, baseline testosterone < 280 ng/dl) were administered replacement testosterone therapy (1% transdermal gel) with or without the 5α-reductase inhibitor dutasteride. At baseline and after three months of treatment, we determined fasting lipid concentrations, HDL protein composition, and the cholesterol efflux capacity of serum HDL. Testosterone replacement did not affect HDL cholesterol (HDL-C) concentrations but conferred significant increases in HDL-associated paraoxonase 1 (PON1) and fibrinogen α chain (FGA) (P = 0.022 and P = 0.023, respectively) and a decrease in apolipoprotein A-IV (apoA-IV) (P = 0.016). Exogenous testosterone did not affect the cholesterol efflux capacity of serum HDL. No differences were observed between men who received testosterone alone and those who also received dutasteride. Testosterone replacement in older hypogonadal men alters the protein composition of HDL but does not significantly change serum HDL-mediated cholesterol efflux. These effects appear independent of testosterone conversion to dihydrotestosterone. Further research is needed to determine how changes in HDL protein content affect CVD risk in men.
Keywords: cardiovascular disease, lipoproteins, lipids, atherosclerosis, androgens
Men exhibit an increased risk of cardiovascular disease (CVD) relative to premenopausal women (1), and it has been postulated that testosterone contributes to this elevated risk (2). Exogenous testosterone administration can decrease serum concentrations of HDL cholesterol (HDL-C) (2). Because low HDL-C correlates with increased CVD risk, this decrease could contribute to the presumed adverse cardiovascular effects of testosterone. In contrast, recent data demonstrate that low circulating androgen levels in men are associated with increased risk of CVD and mortality (3, 4), challenging the assumption that testosterone adversely impacts cardiovascular health in men.
Part of this apparent discrepancy regarding the impact of androgens on CVD may derive from the historical focus on HDL-C concentration as the sole indicator of HDL-associated CVD risk. Notably, recent intervention trials have failed to demonstrate CVD risk reduction with pharmacologic therapies that raise HDL-C. The cholesterol ester transfer protein (CETP) inhibitor torcetrapib substantially raised HDL-C but was associated with increased incidence of cardiovascular events and mortality (5). Similarly, niacin conferred a significant increase in HDL but failed to reduce cardiovascular event rate, leading to early termination of the Atherothrombosis Intervention in Metabolic syndrome with low HDL/high triglycerides: Impact on Global Health outcomes (AIM-HIGH) trial (6).
Because raising HDL-C does not uniformly appear to reduce CVD risk, recent investigations have focused on alternative methods to assess HDL function and composition, as these may prove more reliable indicators of differential risk or risk modification (7, 8). HDL particles comprise a complex assembly of lipid and protein components. We recently have demonstrated that HDL protein composition differs in populations with and without CVD (9, 10), and these differences in protein cargo likely affect HDL function. HDL particles play a pivotal role in the atheroprotective processes of endothelial repair and reverse cholesterol transport (11–13). Endothelial cells generate the anti-inflammatory and vasodilatory signaling molecule nitric oxide (NO) through eNOS activity, which is stimulated by HDL-associated apolipoprotein A-I (apoA-I) and possibly sphingosine-1 phosphate (S1P) (14). Reverse cholesterol transport describes the process by which HDL transports cholesterol from peripheral tissues to the liver, including removal of cholesterol from foam cells within the artery wall (11). In vitro, efflux of cholesterol from macrophages by serum HDL is lower in individuals with established coronary artery disease (CAD). Importantly, HDL efflux capacity may be a better predictor of CAD than HDL-C alone (7). Thus, assessment of HDL protein composition and function are proving important strategies for enhancing our understanding of the relationship between HDL and CVD risk.
To provide further insights into the effects of testosterone on HDL and atherogenesis in men, we examined the impact of testosterone replacement on HDL function and composition. Previously, we performed a double-blind, randomized intervention trial in older hypogonadal men to evaluate the effects of testosterone replacement, with or without the 5α-reductase inhibitor dutasteride, on the prostate (15). We used a subset of fasting samples from this study to perform a secondary analysis examining the effects of testosterone therapy on HDL cholesterol efflux capacity and protein composition in hypogonadal men.
MATERIALS AND METHODS
Study protocol
Older men (age ≥ 50 years) with low baseline testosterone levels (≤280 ng/dl or ≤300 ng/dl on two separate occasions) were recruited as described previously (15). Exclusion criteria included history of prostate cancer; use of either androgen or anti-androgen therapy within the prior year; severe systemic illness, including diabetes; and weight > 300 lbs. The Institutional Review Board of the University of Washington approved all study procedures, and informed consent was obtained from all subjects.
Subjects were randomized to receive daily 7.5 g transdermal 1% testosterone gel (AndroGel 1%; Abbott Laboratories, Abbott Park, IL) with daily oral placebo (T-only) or 0.5 mg dutasteride (T+D) (Avodart; GlaxoSmithKline, Philadelphia, PA) to selectively decrease serum dihydrotestosterone (DHT). Testosterone dosing was adjusted to achieve physiologic serum concentrations (500–1,000 ng/dl) as described previously (15). Fasting blood for lipid analyses was obtained at baseline and at the three-month study visit. Forty-six subjects completed all study procedures, and 23 subjects (11 T-only, 12 T+D) were included in the present analysis on the basis of i) sufficient sample availability at desired time points, ii) achievement of serum testosterone level > 300 ng/dl at three months, and iii) exclusion of subjects on niacin or fibrate therapy.
Laboratory assessments
Serum sex steroids were measured using liquid chromatography-tandem mass spectrometry (LC-MS/MS), and gonadotropins and sex hormone binding globulin (SHBG) were assessed by immunofluorometric assay (15). Free testosterone was calculated using the Södergard equation (16). Fasting serum lipids were measured at the Northwest Lipid Research Center (Seattle, WA) using standard methods (17). Serum apoA-I levels were determined by nephelometry on a Siemens BN-II automated clinical instrument using a Siemens apoA-I reagent (18).
HDL protein composition
The HDL proteome was determined by LC-MS/MS as previously described (10, 19). Low abundance proteins (mean spectral count < 5 for >50% of subjects) were excluded from the final analysis, yielding a total of 42 HDL-associated proteins.
Serum HDL cholesterol efflux capacity
The cholesterol efflux capacity of apolipoprotein B (apoB)-depleted serum was determined with the method of Khera et al. (7), as previously described (19). The presented values reflect the fraction of total [3H] cholesterol released into the medium after subtraction of values obtained following serum-free incubation. Cholesterol efflux capacity was determined in a single assay from serum collected from all subjects at both time points. All samples were run in duplicate.
Statistical analysis
Comparisons at baseline and three months were made for both treatment groups (T-only, T+D) individually. As our principal aim was to investigate the impact of increased serum testosterone on HDL, we also performed comparisons on the entire study population to increase statistical power. Statistical analyses were performed using Prism 5 (GraphPad, La Jolla, CA). Comparisons between all values at baseline and three months were made using a Wilcoxon sign rank test. Comparisons between treatment groups were made using a Mann-Whitney test. Correlations were determined by calculating Spearman R values.
For analysis of changes in HDL-associated protein abundance, correction for multiple comparisons was performed using a modified Bonferoni method (20) based on Spearman R values and a threshold of 0.8. The adjusted threshold value for significance was P < 0.029. For all other analyses, P < 0.05 was considered statistically significant. To examine the potential interaction between statin use and testosterone replacement, spectral count data were normalized by log transformation, and 2-way ANOVA was performed.
RESULTS
Study participants
Of 53 subjects enrolled in the study, 46 completed all study procedures (15), and 23 were included in the present analysis. Thirty-one subjects had sufficient sample volume; 4 subjects were excluded due to serum testosterone levels < 300 ng/dl at month 3, and 4 were excluded due to concurrent niacin or fibrate therapy. Of the included subjects, 11 (4 T-only and 7 T+D) were not on lipid-lowering therapy, and 12 (7 T-only and 5 T+D) were on statin monotherapy. Selected subjects were representative of the overall study population with regard to age, weight, body mass index (BMI), and sex steroid levels (15) (supplementary Table I). Subjects had a baseline BMI of 32.2 ± 5 kg/m2, and no significant changes in body weight or BMI were evident over the study period. No serious adverse events occurred, and all safety data were reported previously (15).
Sex steroid concentrations
Among subjects in the present analysis, serum testosterone rose significantly, and levels in the physiologic range were achieved uniformly (Table 1). Estradiol levels also were significantly higher at three months compared with baseline. As expected, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) production were suppressed with exogenous testosterone administration. No changes in SHBG or serum DHEA were observed. As anticipated, subjects who received dutasteride had significantly lower DHT levels than subjects who received testosterone alone. At three months, subjects in the T+D group also had higher serum estradiol levels than subjects in the T-only group, but the difference was not statistically significant (P = 0.21). As these differences could contribute to changes in HDL particle composition or function, subgroup and whole-group analyses were performed for all study measures.
TABLE 1.
Hormone concentrations at baseline and after three months of testosterone replacement
| Baseline | Three Months | Baseline | Three Months | Baseline | Three Months | |
| Both groups (n = 23) | T+D (n = 12) | T-only (n = 11) | ||||
| Total testosterone (ng/dl) | 222 ± 81 | 597 ± 307c | 226 ± 81 | 576 ± 254c | 219 ± 85 | 621 ± 368c |
| Free testosterone (ng/dl) | 4.5 ± 1.7 | 14.3 ± 6.2c | 4.9 ± 2.0 | 14.2 ± 6.9c | 4.1 ± 1.3 | 14.4 ± 5.6c |
| Estradiol (pg/ml) | 15.3 ± 9.7 | 25.0 ± 10.9c | 17.0 ± 9.8 | 28.4 ± 11.5b | 13.5 ± 9.8 | 21.3 ± 9.3a |
| DHT (ng/dl) | 24 ± 10 | 95 ± 127a | 25 ± 9 | 13 ± 7b | 24 ± 11 | 184 ± 137c |
| DHEA (ng/ml) | 1.0 ± 0.6 | 1.3 ± 1.2 | 1.2 ± 0.6 | 1.4 ± 1.1 | 0.9 ± 0.5 | 1.2 ± 1.3 |
| SHBG (μg/ml) | 3.2 ± 1.2 | 2.9 ± 1.5 | 2.8 ± 1.3 | 2.9 ± 1.2 | 3.5 ± 1.7 | 3.0 ± 1.8 |
Values expressed as mean ± SD.
P < 0.05.
P < 0.01.
P < 0.001.
Fasting lipid profiles and serum apoA-I
At baseline, fasting lipid levels across study subjects were notable for low HDL-C and mild hypertriglyceridemia (Table 2). No significant differences were found between the T-only and T+D groups at baseline or after three months of testosterone therapy. In both the subgroup and whole-group analyses, no changes in lipid profiles were observed after three months of testosterone therapy. Further, testosterone replacement with or without dutasteride coadministration did not alter serum concentrations of apoA-I.
TABLE 2.
Fasting lipid concentrations at baseline and after three months of testosterone replacement
| Baseline | Three Months | Baseline | Three Months | Baseline | Three Months | |
| Both groups (n = 23) | T+D (n = 12) | T-only (n = 11) | ||||
| Total cholesterol (mg/dl) | 187 ± 46 | 181 ± 40 | 187 ± 44 | 189 ± 44 | 186 ± 51 | 171 ± 36 |
| VLDL cholesterol (mg/dl) | 52 ± 40 | 50 ± 39 | 54 ± 44 | 61 ± 49 | 50 ± 38 | 39 ± 21 |
| LDL-C (mg/dl) | 101 ± 41 | 100 ± 36 | 94 ± 32 | 102 ± 41 | 108 ± 50 | 97 ± 33 |
| HDL-C (mg/dl) | 37 ± 11 | 35 ± 11 | 39 ± 11 | 36 ± 12 | 36 ± 11 | 34 ± 11 |
| Triglycerides (mg/dl) | 260 ± 202 | 251 ± 197 | 270 ± 220 | 304 ± 247 | 249 ± 191 | 193 ± 37 |
| ApoA-I (mg/dl) | 164 ± 28 | 157 ± 30 | 168 ± 22 | 165 ± 29 | 160 ± 34 | 150 ± 31 |
Values expressed as mean ± SD.
HDL protein composition
As expected, apoA-I was the most abundant protein identified in HDL at both time points (21) and was unchanged with testosterone replacement (Table 3). In subgroup analysis, no significant differences in HDL-associated protein abundance were evident between the T-only and T+D groups, either at baseline or after three months of testosterone replacement (data not shown). Consequently, all subjects were included in whole-group analysis to increase statistical power. Five HDL-associated proteins changed significantly with testosterone replacement therapy (Table 3). HDL-associated paraoxonase 1 (PON1) and fibrinogen α chain (FGA) increased, whereas apolipoprotein A-IV (apoA-IV), apolipoprotein C-I (apoC-I), and paraoxonase 3 (PON3) decreased after three months of exogenous testosterone. After correction for multiple comparisons, the changes in PON1, apoA-IV, apoC-I, and FGA remained significant.
TABLE 3.
Relative abundance of HDL-associated proteins at baseline and after three months of testosterone therapy
| Protein | Baseline | Three Months | P |
| ApoA-I | 1801 ± 206 | 1862 ± 244 | 0.51 |
| ApoA-II | 682 ± 72 | 672 ± 88 | 0.51 |
| PON1 | 153 ± 35 | 177 ± 45 | 0.022a |
| ApoA-IV | 157 ± 64 | 116 ± 30 | 0.016a |
| SAA4 | 130 ± 19 | 124 ± 22 | 0.07 |
| ApoE | 116 ± 20 | 119 ± 28 | 0.78 |
| ApoC-II | 119 ± 27 | 111 ± 30 | 0.14 |
| ApoC-I | 91 ± 17 | 85 ± 14 | 0.024a |
| ApoD | 66 ± 12 | 68 ± 14 | 0.71 |
| ApoM | 61 ± 13 | 68 ± 15 | 0.09 |
| FGA | 24 ± 19 | 42 ± 23 | 0.023a |
| PON3 | 18 ± 5 | 22 ± 7 | 0.03 |
Values expressed as mean spectral count ± SD. SAA4, serum amyloid A4. Bold font indicates P < 0.05.
P < 0.029.
As lipid-lowering medications have been associated with changes in HDL protein composition (22), further analysis was conducted to determine the potential effects of statin therapy on observed changes in HDL-associated proteins. For the five proteins that changed with testosterone replacement, no significant differences were found in relative protein abundance among subjects on statin therapy and those not on lipid-lowering medications, either at baseline or after three months of testosterone therapy (supplementary Table II). No significant interactions were observed between statin therapy and testosterone replacement (supplementary Table III). Testosterone therapy most robustly contributed to the observed variance in the relative abundance of apoA-IV (17.8%, P = 0.008). Although the effect of statin use on apoC-I relative abundance did not achieve statistical significance (P = 0.08), the degree of variance attributable to statin use was greater than that associated with testosterone therapy (11.3% versus 3.9%, respectively). Statin use did not contribute significantly to the observed variance in PON1, apoA-IV, FGA, or PON3 relative abundance, accounting for <1.0% of the variance in each of these HDL-associated proteins. Thus, the changes in PON1, apoA-IV, and FGA both achieved statistical significance and appeared consequent specifically to testosterone exposure.
For the HDL-associated proteins that changed, no correlations were observed between the magnitude of changes in protein abundance and those in sex steroid levels (data not shown). After three months of testosterone therapy (but not at baseline), a negative correlation was found between total testosterone concentration and apoA-IV abundance (R = −0.48, P = 0.02) (data not shown).
Serum HDL cholesterol efflux
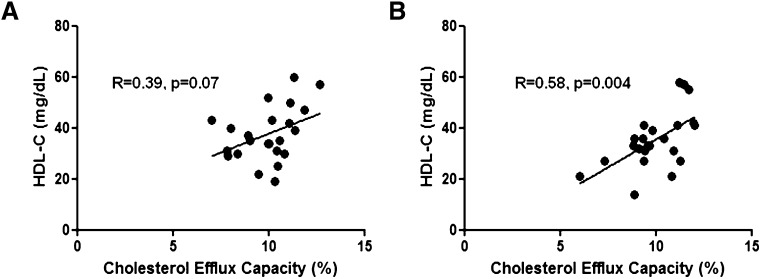
To determine whether changes in HDL protein cargo translated into altered HDL function, cholesterol efflux capacity was quantified by measuring the fraction of radiolabeled cholesterol released from macrophages to serum HDL (apoB-depleted serum). Lower efflux capacity as determined by this assay has been shown to correlate with the presence of CAD (7). No changes in serum HDL-mediated cholesterol efflux were evident after three months of testosterone replacement (baseline mean: 9.9 ± 1.4%, three-month mean: 9.9 ± 1.5%). The absence of change in efflux was apparent in both the subgroup and whole-group analyses. A positive correlation was observed between HDL-C and serum HDL cholesterol efflux as a trend at baseline, and it reached statistical significance after three months of testosterone replacement (Fig. 1A, B). No change in cholesterol efflux capacity was evident after correction for HDL-C (data not shown).
Fig. 1.
A positive correlation between HDL-C and HDL cholesterol efflux capacity was evident as a trend at baseline (A) and achieved significance after three months of testosterone replacement (B).
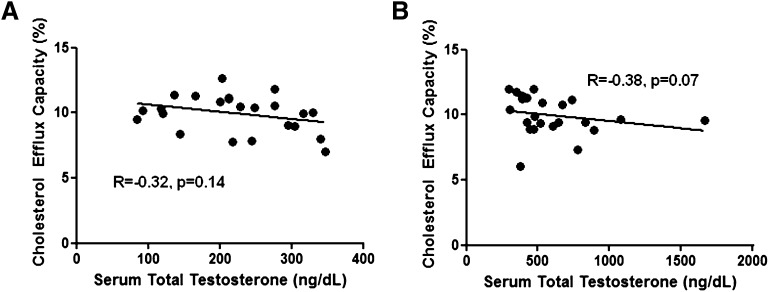
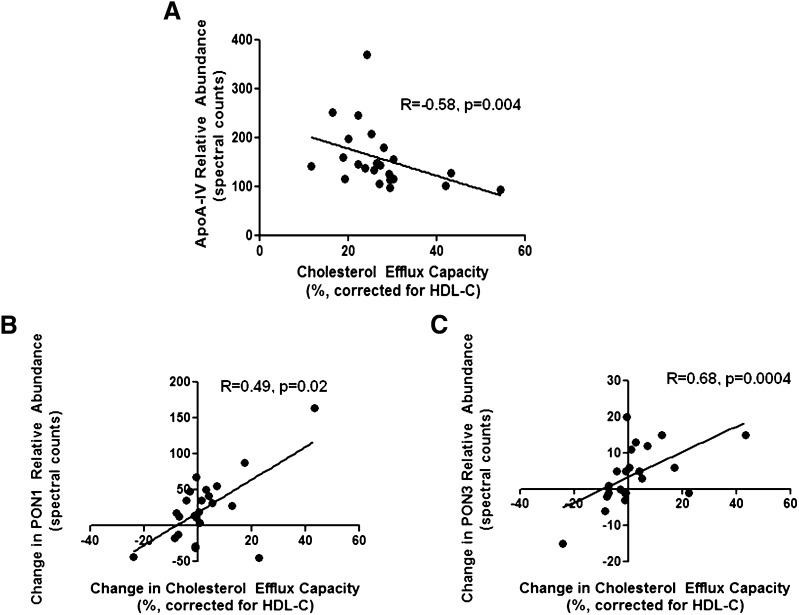
A trend toward a negative correlation between serum total testosterone and cholesterol efflux capacity was evident after three months of testosterone replacement therapy (R = −0.38, P = 0.07) (Fig. 2). At baseline, a negative correlation existed between apoA-IV relative abundance and cholesterol efflux capacity, but only after efflux was corrected for HDL-C (R = −0.58, P = 0.004) (Fig. 3A). The observed changes in both PON1 and PON3 relative abundance exhibited positive correlations with the changes in corrected cholesterol efflux capacity (Fig. 3B, C).
Fig. 2.
No correlation was evident between serum testosterone and efflux capacity at baseline (A), but a negative correlation between efflux capacity and serum testosterone levels existed as a trend after three months of testosterone replacement (B).
Fig. 3.
A negative correlation existed between corrected efflux capacity and apoA-IV relative abundance at baseline (A), and positive correlations were observed between changes in corrected efflux capacity and changes in PON1 (B) and PON3 (C) relative abundance after three months of testosterone replacement.
DISCUSSION
In the current study, we demonstrate that testosterone replacement therapy in older hypogonadal men alters the HDL proteome, supporting a role for sex steroids in determining HDL protein composition. However, this protein remodeling was not associated with a reduction in serum HDL-mediated cholesterol efflux from macrophages. These findings suggest that testosterone replacement in older hypogonadal men may not impair HDL ability to efflux cholesterol from macrophages but may affect other HDL-mediated functions.
Substantial controversy exists regarding the clinical indications for testosterone replacement therapy, particularly in the management of age-related hypogonadism. Reluctance to consider replacement stems in part from concern that testosterone might augment cardiovascular risk in men. Testosterone replacement in older men was associated with an increased incidence of cardiovascular events compared with placebo in a recent trial (1). However, the men in this study had significant mobility limitations and multiple comorbidities, possibly limiting the extension of these findings to healthy, aging men. In frail and healthy older men, testosterone replacement improves strength, physical function, and quality of life, and these benefits have been observed in the absence of an increased cardiovascular event rate (23). Further, epidemiologic data demonstrate increased CVD and mortality risk among men with low circulating testosterone levels (3, 4), and a disproportionately elevated risk of CVD is evident among men who have undergone androgen deprivation therapy for treatment of prostate cancer (24). These observations suggest that maintenance of eugonadal testosterone levels, in at least some populations of men, could exert health-promoting and possibly atheroprotective effects.
In our study, no changes in HDL-C or serum apoA-I were evident with the restoration of physiologic testosterone levels in older hypogonadal men. An HDL-C lowering effect of exogenous testosterone has been observed, although this finding is not universal (25) and is largely limited to studies in younger men and those that administered supraphysiologic or oral testosterone doses (26). The importance of route of administration is underscored by findings from direct comparison of oral and parenteral regimens of anabolic-androgenic steroids in male athletes (27). The absence of changes in HDL-C or serum apoA-I in our study consequently could reflect both the older study population and the use of transdermal administration. In postmenopausal women, oral hormone replacement therapies have been shown to alter HDL-C and serum apoA-I levels, cholesterol efflux capacity, and the abundance of HDL-associated proteins (28–31). Therefore, oral regimens of testosterone replacement therapy could confer substantial changes in lipoprotein-related endpoints not captured in the current study.
Animal models and in vitro data demonstrate that modification of HDL-associated proteins can alter a variety of HDL functions, with associated effects on atherogenesis (32, 33). Further, enrichment of specific HDL-associated proteins has been identified in clinical populations with CVD and CVD risk factors (9, 10, 33, 34). It is therefore of interest that we found changes in three HDL-associated proteins that remained significant after correcting for multiple comparisons and assessing for interaction with concurrent statin use.
Previously, we demonstrated that testosterone deprivation in healthy, eugonadal men increased HDL-associated apoA-IV (19), data consistent with our current findings. The roles of apoA-IV in HDL-mediated cholesterol efflux and CVD remain unclear. In a transgenic mouse model, overexpression of human apoA-IV reduced atherosclerotic lesion area (32), and a common genetic variant of apoA-IV has been shown to exhibit enhanced cholesterol efflux from macrophages (35). ApoA-IV further may attenuate atherogenesis, in part due to its anti-oxidative activity (33). In apparent contrast, HDL-associated apoA-IV was enriched in a clinical population with CAD compared with matched controls (9).
Our data also demonstrate a significant increase in HDL-associated PON1 after testosterone replacement therapy. Recently, HDL particles isolated from patients with CAD were shown to stimulate less NO release from endothelial cells than HDL from healthy controls, a differential effect ascribed to PON1 damage mediated by products of lipid peroxidation (36, 37). PON1 has been proposed to scavenge lipid oxidation products, and apoA-I modified by these products loses its ability to promote cholesterol efflux through the ABCA1 pathway (31, 32); thus, PON1 may be critical for protecting HDL particles from oxidative damage. In future studies, it will be important to verify whether androgens affect PON1 abundance and activity and to determine whether testosterone replacement affects the capacity of HDL to stimulate endothelial cell NO production or scavenge oxidative byproducts. The positive correlations observed between changes in both PON1 and PON3 abundance and HDL-mediated cholesterol efflux further suggest the need for future studies to investigate the relationship between HDL-associated paraoxonase protein levels and HDL efflux capacity.
Finally, we found a significant increase in HDL-associated FGA. To date, no clear role has been identified for FGA in HDL function, atherogenesis, or CVD risk. The observed increase in PON3 relative abundance lost statistical significance after correction for multiple comparisons, and statin use may have played a confounding role in the changes evident in apoC-I abundance. ApoC-I is implicated strongly in triglyceride metabolism, as it can inhibit CETP and may regulate both hepatic lipase and LCAT activity (38–40). VLDL apoC-I content has been positively correlated with fasting triglyceride concentrations and carotid plaque area (41), whereas HDL-mediated apoC-I transport rates were inversely correlated with plasma triglyceride levels (42). The apparent influence of statin therapy on apoC-I abundance in our study is supported by in vitro findings that statin treatment suppressed hepatocyte secretion of apoC-I (43). Nonetheless, subjects who were not on statin therapy also exhibited decreases in HDL-associated apoC-I, and changes in serum apoC-I have been observed consequent to hormone replacement therapy in women (28). Thus, the possible regulation of both apoC-I and PON3 by sex steroids warrants further investigation in larger studies. Finally, our current analytical strategy has limited sensitivity for detecting changes in lower abundance proteins that are known to play pivotal roles in determining HDL composition and function. Such proteins include CETP, which was detected only in two subjects, and will require targeted investigation employing methods of absolute protein quantification. Similarly, as for other HDL-associated enzymes, metrics that assay enzymatic activity in addition to protein levels will be crucial for better delineating the relationship between sex steroids and HDL.
As testosterone is converted to estradiol by aromatization, exogenous testosterone therapy conferred concurrent increases in serum estradiol. Our study therefore cannot discriminate between androgen- and estrogen-mediated effects underlying the observed changes in HDL protein cargo. The absence of differences noted between men who received testosterone alone and those who also received dutasteride indicates that the observed changes were not contingent on circulating levels of DHT. Furthermore, the absence of differences between the two treatment groups suggests that the modestly higher serum estradiol levels evident among men who received dutasteride did not confer substantial effects on HDL protein composition. However, the men who received dutasteride had higher estradiol concentrations at baseline, rendering the net changes in serum estradiol comparable in both treatment groups. This baseline difference likely is consequent to our small sample size and underscores further the need for dedicated investigation of the respective effects of androgens and estrogens on the HDL proteome.
Many lines of evidence indicate that HDL mediates pleiotropic effects, suggesting the importance of assessing HDL function in the prediction of CVD risk (44–46). A principal means by which HDL is thought to confer atheroprotection is reverse cholesterol transport, whereby HDL accepts cholesterol from peripheral tissues, including macrophages, and transports it to the liver for excretion (11). This unloading of lipid from macrophages could reduce foam cell formation and thereby attenuate atherogenesis. Notably, Khera et al. (7) have developed an assay of serum HDL-mediated cholesterol efflux from macrophages and demonstrated a significant, negative correlation between efflux capacity and extant CAD in a cross-sectional analysis. In our population of older hypogonadal men, we found no significant change in efflux capacity consequent to testosterone replacement. The absence of change in HDL-C partially may underlie the absence of change in cholesterol efflux capacity, as these have been shown to correlate significantly (7). Alternatively, this negative finding might reflect our limited sample size or the concurrent increases in serum androgen and estrogen concentrations, which could produce differential or offsetting effects on HDL-C and HDL function. Accordingly, further study is required to determine whether the selective restoration of normal physiologic levels of circulating androgens or estrogens affects HDL cholesterol efflux capacity. Notably, cholesterol efflux represents only one of a growing number of functions now recognized for HDL particles (12, 33, 47), and continued research is warranted to determine how testosterone replacement may affect additional HDL-mediated functions.
Our findings indicate that in older hypogonadal men, the restoration of testosterone levels to those found in healthy young men alters HDL protein composition but does not appear to change the cholesterol efflux capacity of serum HDL. Testosterone replacement also conferred significant increases in HDL-associated PON1 and FGA and a decrease in apoA-IV. Given the absence of a functional correlate, the net effects of these changes on HDL function or CVD risk remain unclear. Our findings therefore underscore the need for assessment of additional HDL functions after exogenous testosterone therapy but suggest that sterol efflux to HDL is not impaired by testosterone replacement. Further, our findings indicate the need for continued investigation of both the roles of individual HDL-associated proteins in atherogenesis and the utility of various metrics of HDL function for predicting cardiovascular risk. Such broadened understanding is essential to better interpret the role of sex steroids in cholesterol metabolism and attendant risk of CVD in men.
Footnotes
Abbreviations:
- BMI
- body mass index
- CAD
- coronary artery disease
- CETP
- cholesterol ester transfer protein
- CVD
- cardiovascular disease
- DHEA
- dehydroepiandrosterone
- DHT
- dihydrotestosterone
- FGA
- fibrinogen alpha chain
- FSH
- follicle-stimulating hormone
- HDL-C
- HDL cholesterol
- LH
- luteinizing hormone
- NO
- nitric oxide
- PON1/3
- paraoxonase 1/3
- S1P
- sphingosine-1 phosphate
- SHBG
- sex hormone binding globulin
- T only
- 7.5 g transdermal 1% testosterone gel with daily oral placebo
- T+D
- 7.5 g transdermal 1% testosterone gel with 0.5 mg dutasteride
This work was supported by National Institutes of Health Grants RO1-AG-037603, U54-HD-42454, P50-CA-097186, DK-017047, T32-DK-007247 (K. B. R.), P30-DK-035816 (T. V.), R01-HL-089504 (T. V.), P30-DK-017047, P01-HL-112625 (J. W. H.), R01-HL-086798 (J. W. H.), and P01-HL-092969 (J. W. H.); by the Department of Veterans Affairs Puget Sound Health Care System (A. M. M.); and by American Heart Association Grant 083-0231N (T. V.). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Transdermal placebo and testosterone gels were provided by Abbott Laboratories (formerly Solvay Pharmaceuticals), and dutasteride and oral placebo were provided by GlaxoSmithKline, neither of which had any input into the study design, analyses, or manuscript preparation.
The online version of this article (available at http://www.jlr.org) contains supplementary data in the form of three tables.
REFERENCES
- 1.Basaria S., Coviello A. D., Travison T. G., Storer T. W., Farwell W. R., Jette A. M., Eder R., Tennstedt S., Ulloor J., Zhang A., et al. 2010. Adverse events associated with testosterone administration. N. Engl. J. Med. 363: 109–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu F. C., von Eckardstein A. 2003. Androgens and coronary artery disease. Endocr. Rev. 24: 183–217 [DOI] [PubMed] [Google Scholar]
- 3.Laughlin G. A., Barrett-Connor E., Bergstrom J. 2008. Low serum testosterone and mortality in older men. J. Clin. Endocrinol. Metab. 93: 68–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vikan T., Schirmer H., Njolstad I., Svartberg J. 2009. Endogenous sex hormones and the prospective association with cardiovascular disease and mortality in men: the Tromso Study. Eur. J. Endocrinol. 161: 435–442 [DOI] [PubMed] [Google Scholar]
- 5.Barter P. J., Caulfield M., Eriksson M., Grundy S. M., Kastelein J. J., Komajda M., Lopez-Sendon J., Mosca L., Tardif J. C., Waters D. D., et al. 2007. Effects of torcetrapib in patients at high risk for coronary events. N. Engl. J. Med. 357: 2109–2122 [DOI] [PubMed] [Google Scholar]
- 6.AIM-HIGH Investigators 2011. The role of niacin in raising high-density lipoprotein cholesterol to reduce cardiovascular events in patients with atherosclerotic cardiovascular disease and optimally treated low-density lipoprotein cholesterol: baseline characteristics of study participants. The Atherothrombosis Intervention in Metabolic syndrome with low HDL/high triglycerides: impact on Global Health outcomes (AIM-HIGH) trial. Am. Heart J. 161: 538–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khera A. V., Cuchel M., de la Llera-Moya M., Rodrigues A., Burke M. F., Jafri K., French B. C., Phillips J. A., Mucksavage M. L., Wilensky R. L., et al. 2011. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N. Engl. J. Med. 364: 127–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heinecke J. 2011. HDL and cardiovascular-disease risk--time for a new approach? N. Engl. J. Med. 364: 170–171 [DOI] [PubMed] [Google Scholar]
- 9.Vaisar T., Mayer P., Nilsson E., Zhao X. Q., Knopp R., Prazen B. J. 2010. HDL in humans with cardiovascular disease exhibits a proteomic signature. Clin. Chim. Acta. 411: 972–979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaisar T., Pennathur S., Green P. S., Gharib S. A., Hoofnagle A. N., Cheung M. C., Byun J., Vuletic S., Kassim S., Singh P., et al. 2007. Shotgun proteomics implicates protease inhibition and complement activation in the antiinflammatory properties of HDL. J. Clin. Invest. 117: 746–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rader D. J., Alexander E. T., Weibel G. L., Billheimer J., Rothblat G. H. 2009. The role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis. J. Lipid Res. 50(Suppl.): S189–S194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon S. M., Hofmann S., Askew D. S., Davidson W. S. 2011. High density lipoprotein: it's not just about lipid transport anymore. Trends Endocrinol. Metab. 22: 9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Movva R., Rader D. J. 2008. Laboratory assessment of HDL heterogeneity and function. Clin. Chem. 54: 788–800 [DOI] [PubMed] [Google Scholar]
- 14.Mineo C., Shaul P. W. 2011. PON-dering differences in HDL function in coronary artery disease. J. Clin. Invest. 121: 2545–2548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page S. T., Hirano L., Gilchriest J., Dighe M., Amory J. K., Marck B. T., Matsumoto A. M. 2011. Dutasteride reduces prostate size and prostate specific antigen in older hypogonadal men with benign prostatic hyperplasia undergoing testosterone replacement therapy. J. Urol. 186: 191–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vermeulen A., Verdonck L., Kaufman J. M. 1999. A critical evaluation of simple methods for the estimation of free testosterone in serum. J. Clin. Endocrinol. Metab. 84: 3666–3672 [DOI] [PubMed] [Google Scholar]
- 17.Guy J., Ogden L., Wadwa R. P., Hamman R. F., Mayer-Davis E. J., Liese A. D., D'Agostino R., Jr, Marcovina S., Dabelea D. 2009. Lipid and lipoprotein profiles in youth with and without type 1 diabetes: the SEARCH for Diabetes in Youth case-control study. Diabetes Care. 32: 416–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agger S. A., Marney L. C., Hoofnagle A. N. 2010. Simultaneous quantification of apolipoprotein A-I and apolipoprotein B by liquid-chromatography-multiple- reaction-monitoring mass spectrometry. Clin. Chem. 56: 1804–1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubinow K. B., Tang C., Hoofnagle A. N., Snyder C. N., Amory J. K., Heinecke J. W., Page S. T. 2012. Acute sex steroid withdrawal increases cholesterol efflux capacity and HDL-associated clusterin in men. Steroids. 77: 454–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tukey J. W., Ciminera J. L., Heyse J. F. 1985. Testing the statistical certainty of a response to increasing doses of a drug. Biometrics. 41: 295–301 [PubMed] [Google Scholar]
- 21.Karlsson H., Leanderson P., Tagesson C., Lindahl M. 2005. Lipoproteomics II: mapping of proteins in high-density lipoprotein using two-dimensional gel electrophoresis and mass spectrometry. Proteomics. 5: 1431–1445 [DOI] [PubMed] [Google Scholar]
- 22.Green P. S., Vaisar T., Pennathur S., Kulstad J. J., Moore A. B., Marcovina S., Brunzell J., Knopp R. H., Zhao X. Q., Heinecke J. W. 2008. Combined statin and niacin therapy remodels the high-density lipoprotein proteome. Circulation. 118: 1259–1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Srinivas-Shankar U., Roberts S. A., Connolly M. J., O'Connell M. D., Adams J. E., Oldham J. A., Wu F. C. 2010. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J. Clin. Endocrinol. Metab. 95: 639–650 [DOI] [PubMed] [Google Scholar]
- 24.Keating N. L., O'Malley A. J., Freedland S. J., Smith M. R. 2010. Diabetes and cardiovascular disease during androgen deprivation therapy: observational study of veterans with prostate cancer. J. Natl. Cancer Inst. 102: 39–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ozata M., Yildirimkaya M., Bulur M., Yilmaz K., Bolu E., Corakci A., Gundogan M. A. 1996. Effects of gonadotropin and testosterone treatments on Lipoprotein(a), high density lipoprotein particles, and other lipoprotein levels in male hypogonadism. J. Clin. Endocrinol. Metab. 81: 3372–3378 [DOI] [PubMed] [Google Scholar]
- 26.Shabsigh R., Katz M., Yan G., Makhsida N. 2005. Cardiovascular issues in hypogonadism and testosterone therapy. Am. J. Cardiol. 96: 67M–72M [DOI] [PubMed] [Google Scholar]
- 27.Hartgens F., Rietjens G., Keizer H. A., Kuipers H., Wolffenbuttel B. H. 2004. Effects of androgenic-anabolic steroids on apolipoproteins and lipoprotein (a). Br. J. Sports Med. 38: 253–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chiuve S. E., Martin L. A., Campos H., Sacks F. M. 2004. Effect of the combination of methyltestosterone and esterified estrogens compared with esterified estrogens alone on apolipoprotein CIII and other apolipoproteins in very low density, low density, and high density lipoproteins in surgically postmenopausal women. J. Clin. Endocrinol. Metab. 89: 2207–2213 [DOI] [PubMed] [Google Scholar]
- 29.Ulloa N., Arteaga E., Bustos P., Duran-Sandoval D., Schulze K., Castro G., Jauhiainen M., Fruchart J. C., Calvo C. 2002. Sequential estrogen-progestin replacement therapy in healthy postmenopausal women: effects on cholesterol efflux capacity and key proteins regulating high-density lipoprotein levels. Metabolism. 51: 1410–1417 [DOI] [PubMed] [Google Scholar]
- 30.von Eckardstein A., Crook D., Elbers J., Ragoobir J., Ezeh B., Helmond F., Miller N., Dieplinger H., Bennink H. C., Assmann G. 2003. Tibolone lowers high density lipoprotein cholesterol by increasing hepatic lipase activity but does not impair cholesterol efflux. Clin. Endocrinol. (Oxf.). 58: 49–58 [DOI] [PubMed] [Google Scholar]
- 31.Hughes T. A., Pace D. T., Ke R. W., Tolley E. A., Qureshi N., Stentz F. 2004. Lipoprotein compositional changes with combination hormone therapy (conjugated estrogen and medroxyprogesterone) in African American women. Endocr. Pract. 10: 179–186 [DOI] [PubMed] [Google Scholar]
- 32.Duverger N., Tremp G., Caillaud J. M., Emmanuel F., Castro G., Fruchart J. C., Steinmetz A., Denefle P. 1996. Protection against atherogenesis in mice mediated by human apolipoprotein A-IV. Science. 273: 966–968 [DOI] [PubMed] [Google Scholar]
- 33.Kontush A., Chapman M. J. 2006. Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis. Pharmacol. Rev. 58: 342–374 [DOI] [PubMed] [Google Scholar]
- 34.Hoofnagle A. N., Wu M., Gosmanova A. K., Becker J. O., Wijsman E. M., Brunzell J. D., Kahn S. E., Knopp R. H., Lyons T. J., Heinecke J. W. 2010. Low clusterin levels in high-density lipoprotein associate with insulin resistance, obesity, and dyslipoproteinemia. Arterioscler. Thromb. Vasc. Biol. 30: 2528–2534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gomaraschi M., Putt W. E., Pozzi S., Iametti S., Barbiroli A., Bonomi F., Favari E., Bernini F., Franceschini G., Talmud P. J., et al. 2010. Structure and function of the apoA-IV T347S and Q360H common variants. Biochem. Biophys. Res. Commun. 393: 126–130 [DOI] [PubMed] [Google Scholar]
- 36.Besler C., Heinrich K., Rohrer L., Doerries C., Riwanto M., Shih D. M., Chroni A., Yonekawa K., Stein S., Schaefer N., et al. 2011. Mechanisms underlying adverse effects of HDL on eNOS-activating pathways in patients with coronary artery disease. J. Clin. Invest. 121: 2693–2708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shao B., Pennathur S., Pagani I., Oda M. N., Witztum J. L., Oram J. F., Heinecke J. W. 2010. Modifying apolipoprotein A-I by malondialdehyde, but not by an array of other reactive carbonyls, blocks cholesterol efflux by the ABCA1 pathway. J. Biol. Chem. 285: 18473–18484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rouhani N., Young E., Chatterjee C., Sparks D. L. 2008. HDL composition regulates displacement of cell surface-bound hepatic lipase. Lipids. 43: 793–804 [DOI] [PubMed] [Google Scholar]
- 39.Conde-Knape K., Bensadoun A., Sobel J. H., Cohn J. S., Shachter N. S. 2002. Overexpression of apoC-I in apoE-null mice: severe hypertriglyceridemia due to inhibition of hepatic lipase. J. Lipid Res. 43: 2136–2145 [DOI] [PubMed] [Google Scholar]
- 40.Meyers N. L., Wang L., Small D. M. 2012. Apolipoprotein C–I binds more strongly to phospholipid/triolein/water than triolein/water interfaces: a possible model for inhibiting cholesterol ester transfer protein activity and triacylglycerol-rich lipoprotein uptake. Biochemistry. 51: 1238–1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hansen J. B., Fernandez J. A., Noto A. T., Deguchi H., Bjorkegren J., Mathiesen E. B. 2011. The apolipoprotein C-I content of very-low-density lipoproteins is associated with fasting triglycerides, postprandial lipemia, and carotid atherosclerosis. J. Lipids. 2011: 271062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohn J. S., Batal R., Tremblay M., Jacques H., Veilleux L., Rodriguez C., Mamer O., Davignon J. 2003. Plasma turnover of HDL apoC-I, apoC-III, and apoE in humans: in vivo evidence for a link between HDL apoC-III and apoA-I metabolism. J. Lipid Res. 44: 1976–1983 [DOI] [PubMed] [Google Scholar]
- 43.Bouchard C., Dubuc G., Davignon J., Bernier L., Cohn J. S. 2005. Post-transcriptional regulation of apoC-I synthesis and secretion in human HepG2 cells. Atherosclerosis. 178: 257–264 [DOI] [PubMed] [Google Scholar]
- 44.Shao B., Oda M. N., Oram J. F., Heinecke J. W. 2010. Myeloperoxidase: an oxidative pathway for generating dysfunctional high-density lipoprotein. Chem. Res. Toxicol. 23: 447–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barter P. J., Nicholls S., Rye K. A., Anantharamaiah G. M., Navab M., Fogelman A. M. 2004. Antiinflammatory properties of HDL. Circ. Res. 95: 764–772 [DOI] [PubMed] [Google Scholar]
- 46.Yvan-Charvet L., Wang N., Tall A. R. 2010. Role of HDL, ABCA1, and ABCG1 transporters in cholesterol efflux and immune responses. Arterioscler. Thromb. Vasc. Biol. 30: 139–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suzuki M., Pritchard D. K., Becker L., Hoofnagle A. N., Tanimura N., Bammler T. K., Beyer R. P., Bumgarner R., Vaisar T., de Beer M. C., et al. 2010. High-density lipoprotein suppresses the type I interferon response, a family of potent antiviral immunoregulators, in macrophages challenged with lipopolysaccharide. Circulation. 122: 1919–1927 [DOI] [PMC free article] [PubMed] [Google Scholar]