Abstract
Purpose
The objective of this study was to evaluate whether changes in the technique for mandibular setback surgery since the introduction of RIF have improved postsurgical stability in Class III correction with setback alone and 2-jaw surgery.
Methods
Cephalometric (skeletal and dental) outcomes for 17 patients with mandibular setback alone were compared to outcomes in 83 patients with 2-jaw surgery for Class III correction. Demographic characteristics in the two groups were similar and the mean amount of setback (−4.7 mm) was the same; but given a mean 4.9 mm maxillary advancement, the 2-jaw patients had a greater total Class III correction.
Results
Eight (47%) of the mandible-only patients, but only one (1%) of the 2-jaw patients, had >4 mm posterior movement of gonion at surgery and a resulting significant change in ramus inclination. Postsurgically, the mean changes for the two groups were similar, with a mean 2.8 mm forward movement of the chin (Pg) in both groups, but the mechanism was different. In the mandible-only patients, the major reason for forward movement of the chin was recovery of ramus inclination. In the 2-jaw group, about half the change in chin position was due to forward movement of gonion—the other half was due to small upward movement of the maxilla that allowed upward-forward rotation of the mandible. In both groups, there was a significant correlation (r = 0.42, p<.0001) between postsurgical change in the position of the chin and gonion.
Conclusion
Despite improvements in surgical techniques for mandibular setback since 1995, postsurgical stability still leaves something to be desired, but there is better control of ramus position when 2-jaw surgery is done.
Keywords: Class III surgery, mandibular setback, Class III long-term stability
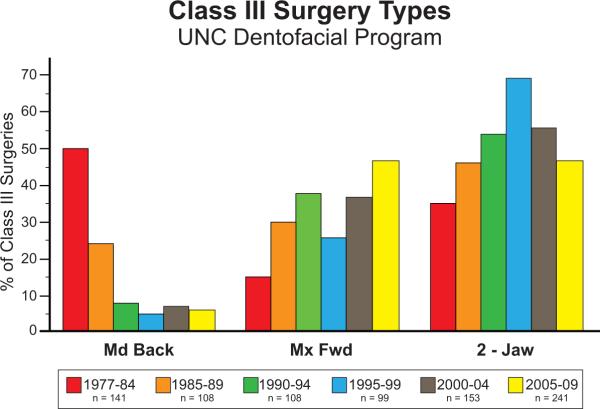
Beginning in the late 1980s, the number of patients with mandibular prognathism as a component of a skeletal Class III problem who were treated with mandibular setback alone decreased remarkably. At the University of North Carolina, the percentage declined from about 50% prior to 1985 to less than 10% in the 1990s, and has remained at that low level (Figure 1).1 The experience elsewhere was similar. The change occurred for three reasons: (1) facial appearance was better if simultaneous maxillary advancement allowed a smaller mandibular setback;2 (2) there were concerns about airway reduction with large setbacks;3,4 and (3) the outcomes of isolated mandibular setback surgery were shown to be less predictable and less stable than desired,5 a report that has been repeatedly confirmed.6,7 For BSSO setback surgery with rigid internal fixation (RIF), part of the problem was posterior rotation of the condylar segment at surgery that produced relapse when the mandible was allowed to function and the musculature repositioned the ramus, and stability seemed to be better with 2-jaw Class III surgery than with isolated mandibular setback.8–11
Figure 1.
Percentage changes for type of surgery for skeletal Class III problems, Univ. of North Carolina. Note the precipitous drop in the percentage of patients with mandibular setback in the early 1980s and the increase in 2-jaw surgery after 1984 that peaked in the 2000–04 period and declined slightly afterward.
The purpose of this study was to directly compare the stability of 2-jaw vs. mandible-only setback procedures performed using modern setback techniques with RIF. This paper reports treatment outcomes in 100 Class III patients who had mandibular setback as part (n=83) or all n=17) of their surgical correction.
Methods
The sample for this study, which was approved by the UNC Biomedical IRB, included all 121 patients treated at UNC Memorial Hospital by two oral and maxillofacial surgeons with resident assistants between 1995 and 2007 who had mandibular setback ≥ 2 mm, either alone (n=19), or with maxillary advancement ≥ 2 mm (n=102). Of these, 2 of the mandible-only group and 19 of the 2-jaw group were eliminated because complete records pre-surgery, immediately post-surgery and at one-year recall were not available. The final sample, therefore, was 83 patients who had 2-jaw surgery and 17 who had mandibular setback alone. All the subjects signed an approved informed consent. As Table 1 shows, the demographic characteristics of patients in the two surgery groups were quite similar.
TABLE I.
DEMOGRAPHIC CHARACTERISTICS
| Two Jaw | Mandibular Only | P value | |
|---|---|---|---|
| Sex | |||
| Female | 63.9% | 58.8% | 0.70 |
| Male | 36.1% | 41.2% | |
| Race | |||
| Caucasian | 80.5% | 58.8% | 0.16 |
| African-American | 8.5% | 17.7% | |
| Other | 11.0% | 23.5% | |
| Maxillary Fixation | |||
| Metal Plates/Screws | 54.2% | 100.0% | NA |
| Resorbable Screws | 45.8% | 0.0% | |
| Mandibular Fixation | |||
| Metal Plates/Screws | 54.2% | 58.8% | 0.73 |
| Resorbable Screws | 45.8% | 41.2% |
| Mean | SD | Mean | SD | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Age at Surgery | 20.2 | 6.38 | 21.8 | 7.05 | 0.35 | |||
| Length of Followup | 1.18 | 0.39 | 1.3 | 0.45 | 0.44 |
For all patients, the lateral cephalogram for each time point was digitized using the UNC 140-point model,5 and dimensional changes and changes in landmark locations in the horizontal (x) and vertical (y) planes were calculated. Descriptive statistics and composite cranial base superimpositions were used to describe the changes between the time points. The percentage of patients with clinically significant (>= 2 mm or 2 degrees) or highly clinically significant (>4 mm or 4 degrees) was also recorded.
To evaluate the statistical significance of the treatment outcomes, 21 continuous outcomes (7 for antero-posterior changes, 7 vertical, 7 dimensional) were measured for each subject at three time points (pre-surgery, post-surgery, follow-up). Linear mixed effects models were defined for each outcome separately. The model considered surgery type, gender and time as well as the pairwise interaction between time and surgery type. If the interaction was significant, the interaction model was used; if it was not, the main effect model was used. All analysis was conducted using SAS 9.2. The level of significance was set at 0.05. Pearson correlation coefficients were calculated to evaluate the relationship between postsurgical changes in the position of the chin and ramus inclination or a-p position of gonion.
Results
1. Changes at surgery
Changes immediately after surgery of selected landmark positions and dimensional changes for both groups are shown in Table 2. Note that the adjusted average setback distance (change in the antero-posterior position of Pg) was the same in both groups (−4.7 mm), and in the 2-jaw group the average maxillary advancement (at point A) was 4.9 mm—so the total correction in jaw position for the 2-jaw group was considerably larger. The mean overjet reduction was −8.7 mm for the 2-jaw group, −5.4 mm for the mandible-only group. As expected, no significant changes in maxillary landmarks or dimensions were noted for the mandible-only group. All the maxillary changes for the 2-jaw group were statistically significant (p<.001). For the 2-jaw group, the mandibular changes were statistically significant, except for the mandibular plane angle; for the smaller mandible-only group, mandibular changes were statistically significant (p<.02), except for the mandibular plane angle and the a-p and vertical position of condylion (which had only a small change in both groups).
TABLE 2.
CEPHALOMETRIC CHANGES, CLASS III SURGERY
| A-P landmark changes (mm, + = forward) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Changes at Surgery | Changes Post-Surg to One Year | |||||||
| 2-Jaw n = 83 | Adj* | Mand Back n = 17 | Adj* | 2-Jaw n = 83 | Adj* | Mand Back n = 17 | Adj* | |
| Mean (SD) | Mean | Mean (SD) | Mean | Mean(SD) | Mean | Mean(SD) | Mean | |
| point A | 5.1 (3.2) | 4.9 | −0.2 (0.5) | 0.1 | −0.8 (2.1) | −0.8 | 0.3 (0.9) | 0.3 |
| point B | −5.8 (4.5) | −5.7 | −5.2(2.5) | −5.7 | 2.7 (2.6) | 2.7 | 2.9 (2.7) | 2.7 |
| pogonion (Pg) | −4.9 (6.1) | −4.7 | −3.7 (2.7) | −4.7 | 2.8 (3.0) | 2.8 | 2.8 (3.2) | 2.8 |
| gonion (Go) | −2.7 (3.4) | −2.8 | −3.0 (2.7) | −2.8 | 2.9 (3.0) | 3.0 | 3.3 (3.5) | 3.0 |
| condylion (Co) | 0.1 (2.1) | −0.04 | 0.2 (1.8) | −0.04 | 0.4 (1.8) | −0.4 | 0.6 (1.9) | −0.4 |
| mx incisor | 3.3 (3.1) | 3.3 | −0.2 (1.0) | −0.2 | 1.0 (2.0) | 1.0 | 1.2 (2.4) | 1.2 |
| mn incisor | −5.3 (3.9) | −5.5 | −6.3 (2.4) | −5.5 | 2.1 (2.2) | 2.2 | 2.6 (1.8) | 2.2 |
| Vertical landmark changes (mm, + = up) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Changes at Surgery | Changes Post-Surg to One Year | |||||||
| 2-Jaw n = 83 | Adj | Mand Back n = 17 | Adj | 2-Jaw n = 83 | Adj | Mand Back n = 17 | Adj | |
| Mean (SD) | Mean | Mean (SD) | Mean | Mean(SD) | Mean | Mean(SD) | Mean | |
| point A | 1.6 (3.1) | 1.6 | −0.2 (0.8) | −0.2 | −1.2(2.0) | −1.2 | −0.4 (1.5) | −0.4 |
| point B | 1.2 (4.6) | 1.0 | −0.1 (2.7) | 1.0 | 2.9 (2.9) | −2.7 | −1.6 (2.5) | −2.7 |
| pogonion (Pg) | 0.9 (5.4) | 0.6 | −0.8 (3.6) | 0.6 | −2.5(2.9) | −2.3 | −1.3 (2.4) | −2.3 |
| gonion (Go) | 0.7 (2.8) | 0.6 | 0.2 (3.0) | 0.6 | −1.7(2.7) | −1.7 | −1.6 (3.2) | −1.7 |
| condylion (Co) | 0.2 | −1.1 | −0.2 | 0.2 | ||||
| mx incisor | 2.3 (3.1) | 2.3 | 0.2 (1.7) | 0.1 | −1.1(2.9) | −1.1 | −0.7 (1.5) | −0.7 |
| mn incisor | 1.4 (4.7) | 1.2 | −0.2 (2.2) | 1.2 | −2.9(2.5) | −2.7 | −1.7 (2.5) | −2.7 |
| Dimensional landmark changes (mm, + = more) (degrees, + = larger) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Changes at Surgery | Changes Post-Surg to One Year | |||||||
| 2-Jaw n = 83 | Adj | Mand Back n = 17 | Adj | 2-Jaw n = 83 | Adj | Mand Back n = 17 | Adj | |
| overjet | 8.7 (3.3) | 8.7 | 5.4 (2.1) | 5.4 | −0.7 (1.7) | −0.7 | −1.3 (1.5) | −1.3 |
| overbite | 0.7 (3.0) | 0.6 | 0.2 (2.4) | 0.6 | 1.7 (1.6) | 1.6 | 1.1 (1.7) | 1.6 |
| Co-Pg | −3.1 (3.8) | −3.0 | −2.3 (3.2) | −3.0 | 0.5 (2.3) | 0.6 | 1.0 (1.9) | 0.6 |
| ANB° | 6.4 (4.9) | 6.3 | 1.1 (3.0) | 1.1 | −2.0 (1.8) | −2.0 | −1.1 (1.4) | −1.1 |
| mand plane angle ° | 0.7 (4.8) | 0.5 | −0.6 (2.8) | 0.5 | −0.7 (2.3) | −0.4 | 0.5 (3.0) | −0.4 |
| palatal plane angle° | 3.0 (3.6) | 3.0 | −0.1 (0.6) | −0.1 | −2.0 (1.8) | −1.0 | 0.1 (0.8) | 0.6 |
| SN-ArGo° | 2.7 (3.7) | 2.8 | 3.2 (4.2) | 2.8 | −3.5 (3.1) | −3.6 | −3.9 (4.1) | −3.6 |
Adjusted mean value for each type of surgery after controlling for gender
For both surgery groups, the data show a tendency to push the ramus segment back at surgery (posterior movement of gonion, increase in SN-NGo angle), but there was considerable variation in this change and it occurred more frequently in the mandible-only patients. Gonion moved posteriorly >4 mm in 8 (47%) of the mandible-only patients, but in only one (1%) of the 2-jaw patients; all but one (94%) of the mandible-only patients had >2° increase in the inclination of the ramus and 53% had >4° degree increase vs. 68% and 43%, respectively, of the 2-jaw patients. The average changes in the a-p position of gonion and the SN-ArGo angle were statistically significantly different in both groups (mand only, p = 0.01; 2-jaw, p=0.009). Vertical changes occurred in both groups, with nearly equal percentages of increase and decrease in the mandibular plane angle and the y-coordinate of menton and gonion. The mandible was shortened more in the 2-jaw patients (Co-Pg decrease of 3.1 vs. 2.3 mm), but this was not statistically significant.
2. Changes from immediately post-surgery to one-year recall
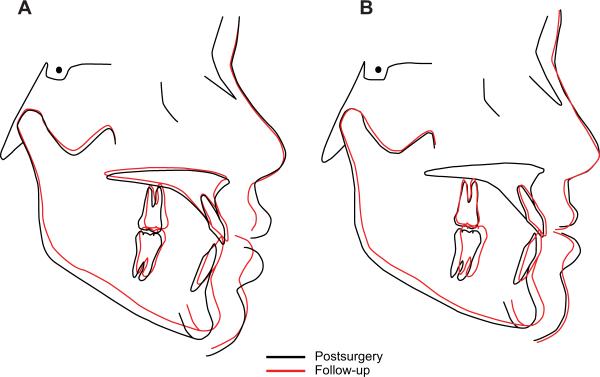
Changes post-surgery also are shown in Table 2 and the mean changes can be compared in superimposed composite tracings in Figures 2A and 2B. In the post-surgery timeframe, statistically significant changes for maxillary dimensions/landmarks were seen only in the 2-jaw group. In the mandible, changes in vertical position of the condyle and the mandibular plane angle were not statistically significant in either group. Note in Table 2 that forward movement of the chin post-surgically (x coordinate of Pg) was similar in the two groups and surprisingly large: an average change of 2.8 mm in both groups. As Figure 2 shows, however, the mechanism by which the chin came forward was not the same in the two groups. In the 2-jaw group, much of the forward movement of the chin was due to upward-forward rotation of the mandible on removal of the surgical splint and/or upward movement of the maxilla; in the mandible-only group some rotation of the mandible also occurred, but it was smaller and due to splint removal. The mean change in the inclination of the ramus was similar and not significantly different between the two surgery types. Despite the larger decrease in the Co-Pg distance in the 2-jaw patients, they had a lower average postsurgical change (mean change of 0.5 vs. 1.0 mm), but this difference was not statistically significant.
Figure 2.
Post-surgery to one year, composite tracings for (A) mand-only and (B) 2-jaw patients.
Most of the skeletal change was not reflected in the overjet, which showed an average decrease of 0.7 mm in the 2 jaw group and 1.3 mm in the mandible-only group, largely because a decrease in overjet was controlled to the extent possible during post-surgical orthodontics. A greater upward movement of the chin for the 2-jaw group would be expected to cause a greater mean increase in overbite, and the fact that this did not occur indicates the degree of orthodontic control of overbite postsurgically.
Although the mean change in chin position in the two groups and the different contribution of vertical changes to the change in chin prominence can be visualized clearly in the composite tracings, it is important to keep the variation within the sample in mind. The standard deviations in Table 2 indicate relatively large variations around the mean; the composite tracings are based only on the mean change and give no indication of the variations within the sample. In these patients, as is typical of treatment outcome studies, some of the patients had most of the change, so looking only at mean changes can be misleading.
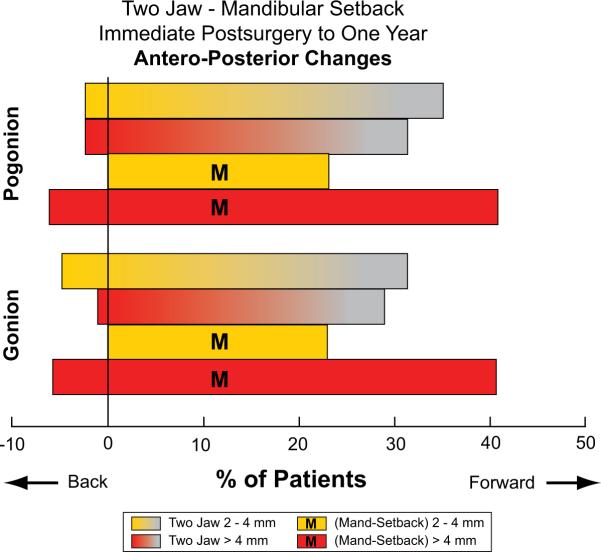
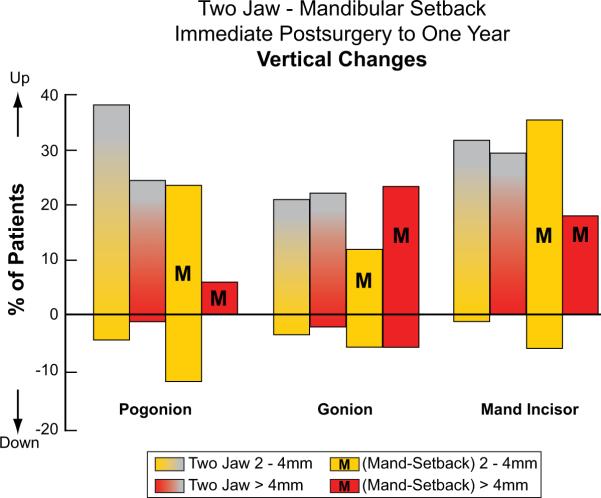
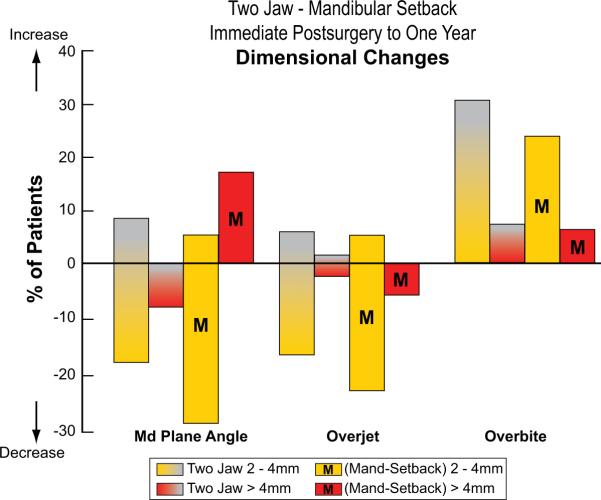
In cephalometric studies of changes during treatment, it is convenient to classify the amount of change as clinically insignificant (<2 mm or 2°), clinically significant (>2 mm or 2°), and highly clinically significant (>4 mm or 4°). The percentage of patients in each group with clinically significant postsurgical change for selected landmarks and dimensions is shown in Figures 3 and 4. Note that about 60% of both groups had >2 mm forward movement of the chin; vertical changes were similar; and the mandible-only group had higher percentages with changes in the mandibular plane angle, overjet and overbite.
Figure 3.
Percentage of patients with clinically significant changes in the antero-posterior location of the mandible, postsurgery to one year. M indicates mandible-only surgery.
Figure 4.
Percentage of patients with clinically significant changes in the vertical position of pogonion, gonion and the mandibular incisor, postsurgery to one year. M indicates mandible-only surgery.
There were statistically significant correlations between change in the position of the chin (Pg), and both forward movement at Go (0.42, p <.0001) and change in the NS-ArGo angle that reflects ramus inclination (−0.23, p <.02). Because there were no significant differences between the wo groups, the data were combined for this analysis.
Discussion
Although the total Class III correction was much greater in the 2-jaw than mandible-only group, the amount of mandibular setback was quite similar. Our data suggest answers to two clinically important questions:
1) Has there been an improvement in the stability of mandibular setback since the importance of controlling ramus position was recognized 20 years ago?
In 1991, we reported that for mandibular setback, replacing wire fixation with rigid internal fixation (RIF) made relapse worse.5 With BSSO setback and wire fixation, the mean relapse at pogonion was 2.6 mm and 25% had >4 mm change; with rigid fixation it was 4.2 mm and 55%. Komori et al had previously reported that suspension wires to maintain the mandibular position during healing tended to reduce relapse tendencies, and suggested that this allowed repositioning of the ramus in the short term postsurgically.12 We concluded that when the surgeon pushed gonion posteriorly, RIF prevented recovery of ramus inclination without also moving the chin forward.
In modern setback surgery, RIF is used routinely because it allows early function and is more comfortable for patients. Has better control of ramus inclination at surgery reduced the stability problem in isolated mandibular setback? At UNC, the mean 2.8 mm relapse in more recent patients with RIF is similar to what it was with wire fixation before RIF was introduced and better than the 4.2 mm when RIF was first used in this surgery,5 so the answer appears to be yes, but the relapse still is clinically significant. In 2-jaw Class III surgery now, the chance of clinically significant posterior movement of gonion is much smaller, and the component of relapse due to this also is smaller. Control of ramus position apparently is easier for the surgeons when repositioning of both jaws is being carried out.
2) With modern surgical technqiues, is there a significant difference in stability between 2-jaw and mandible-only Class III correction?
In answering this question, it is important to keep the distinction between statistically significant and clinically significant in mind. We found statistically significant postsurgical changes in landmark positions and dimensions in both surgery types, and surgery type was not a statistically significant effect on mandibular outcomes after controlling for gender. Looking at the percentages of patients with clinically significant changes gives a different picture—with mandible-only surgery, a larger percentage had highly clinically significant change and the type of change was different (compare Figures 3c and 4c). Those patients would have required more postsurgical orthodontic treatment to prevent significant changes in the dental occlusion. Time in postsurgical orthodontic treatment was not measured in this study, so there is no way to be sure, but it is likely that it was longer for the mandible-only patients.
It also is important to realize that there is a relationship between the amount of mandibular setback and postsurgical stability—all other things being equal, the greater the setback, the greater the amount of postsurgical change in the position of the change.13 One can conclude, therefore, that for patients requiring a large change in jaw relationships, restricting the amount of mandibular setback by simultaneously advancing the maxilla contributes to stability—although this appears to be balanced out by upward movement of the maxilla that allows upward and forward rotation of the mandible.
Comparison with other outcome studies
The data from previous studies of isolated mandibular setback,5–7,10–12 which include a systematic review going back 20 years or more, uniformly document a considerable degree of post-treatment instability and relapse. Eggensperger et al compared relapse after mandibular advancement to mandibular setback,6 and confirmed that mandibular setback was significantly less stable and predictable than mandibular advancement. The same investigators published a 12-year follow-up of long-term changes in patients with isolated mandibular setback,14 documenting that forward movement of the mandible continued long after the surgery.
A number of studies of stability after a combination of maxillary advancement and mandibular setback have reported the same conclusion: the maxillary advancement component is relatively stable, while larger mandibular changes occur.15–17 Jakobsone et al evaluated bimaxillary surgery stability on three-year recall, noted that mandibular stability was not as good as maxillary stability, and suggested that the major risk factors for mandibular relapse were a large setback and inferior repositioning of the posterior maxilla.18 None of these investigators looked at changes in mandibular ramus inclination as a potential relapse factor.
We would interpret the data somewhat differently: as with isolated mandibular setback, control of the inclination of the ramus is an important step in obtaining good stability in 2-jaw Class III surgery, and the magnitude of the setback is a factor in stability primarily because the farther the mandible is set back, the greater the chance of pushing the gonial angle back and uprighting the ramus while doing so. Limiting the amount of setback by obtaining much of the correction with maxillary advancement, therefore, does decrease the amount of postsurgical change in the position of the chin.
Both this study and the other recent publications make it clear that although, on average, better mandibular stability is obtained with 2-jaw surgery than with isolated setback, stability of the setback component of the 2-jaw surgery still leaves something to be desired. If the ramus is pushed posteriorly at surgery, the muscles will put it back at its original inclination, and forward movement of the chin is inevitable as that occurs. The data suggest that it is easier to prevent this from happening during 2-jaw surgery, but an emphasis on maintaining ramus inclination appears o be an important part of improving the stability of 2-jaw surgery as well as isolated setback.
Conclusions
Changes in surgical techniques in mandibular setback have reduced, but not eliminated relapse problems related to postsurgical return of the ramus to its original inclination. The gonial angle is likely to be pushed posteriorly when the mandible is set back, and recovery of the ramus inclination change is the major component of forward movement of the chin after mand-only surgery. In 2-jaw surgery, there is better control of ramus inclination and less relapse related to this, but upward movement of the maxilla that allows the chin to rotate upward and forward brings ts total forward movement to about the same level as with mand-only surgery.
Figure 5.
Percentage of patients with clinically significant changes in the mandibular plane angle, overjet and overbite. M indicates mandible-only surgery.
Acknowledgements
This study was supported in part by NIH grant DE-05221 from the National Institute of Dental and Craniofacial Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. We thank Debora Price for her exemplary management of the data base and SAS programming.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bailey LJ, Proffit WR, White RP. Trends in surgical Class III treatment. Int J Adult Orthod Orthogn Surg. 1995;10:108–118. [PubMed] [Google Scholar]
- 2.Proffit WR, White RP., Jr. Surgical-Orthodontic Treatment. Mosby; St Louis: 1991. [Google Scholar]
- 3.Abdelrahman TE, Takahashi K, Tamura K, Nakao K, Hassanein KM, et al. Impact of different surgery modalities to correct Class III jaw deformities on the pharyngeal airway space. J Craniofac Surg. 2011;22:1598–601. doi: 10.1097/SCS.0b013e31822e5fc2. [DOI] [PubMed] [Google Scholar]
- 4.Hasebe D, Kobayashi T, Hasegawa M, Iwamoto T, et al. Changes in oropharyngeal airway and respiratory function during sleep after orthognathic surgery in patients with mandibular prognathism. Int J Oral Maxillofac Surg. 2011;40:584–92. doi: 10.1016/j.ijom.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Proffit WR, Phillips C, Dann C, IV, Turvey TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. I. Mandibular setback. Int J Adult Orthod Orthogn Surg. 1991;6:7–18. [PubMed] [Google Scholar]
- 6.Eggensperger N, Smolka W, Rahal A, Iizuka T. Skeletal relapse after mandibular advancement and setback in single-jaw surgery. J Oral Maxillofac Surg. 2004;62:1486–96. doi: 10.1016/j.joms.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Chou JI, Fong HJ, Kuang SH, Gi LY, Hwang FY, Lai YC, Chang RC, Kao SY. A retrospective analysis of the stability and relapse of soft and hard tissue change after bilateral sagittal split osteotomy for mandibular setback of 64 Taiwanese patients. J Oral Maxillofac Surg. 2005;63:355–61. doi: 10.1016/j.joms.2004.05.228. [DOI] [PubMed] [Google Scholar]
- 8.Proffit WR, Phillips C, Turvey TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. III. Combined maxillary and mandibular procedures. Int J Adult Orthod Orthogn Surg. 1991;6:211–225. [PubMed] [Google Scholar]
- 9.Costa F, Robiony M, Sembronio S, Polini F, Politi M. Stability of skeletal Class III malocclusion after combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg. 2001;16:179–92. [PubMed] [Google Scholar]
- 10.Cho HJ. Long-term stability of surgical mandibular setback. Angle Orthod. 2007;77:851–6. doi: 10.2319/052306-209.1. [DOI] [PubMed] [Google Scholar]
- 11.Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy setback surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2008;66:1634–43. doi: 10.1016/j.joms.2008.01.046. [DOI] [PubMed] [Google Scholar]
- 12.Komori E, Aigase K, Sugiski M, Tanabe H. Cause of early skeletal relapse after mandibular setback. Am J Orthod Dentofac Orthop. 1989;95:29–36. doi: 10.1016/0889-5406(89)90132-7. [DOI] [PubMed] [Google Scholar]
- 13.Franco JE, van Sickels JE, Thrash W. Factors contributing to relapse in rigidly fixed mandibular seteback. J Oral Maxillofac Surg. 1989;47:451–6. doi: 10.1016/0278-2391(89)90276-0. [DOI] [PubMed] [Google Scholar]
- 14.Eggensperger N, Raditsch T, Taghizadeh F, Iizuka T. Mandibular setback by sagittal split ramus osteotomy: a 12-year follow-up. Acta Odontol Scand. 2005;63:183–8. doi: 10.1080/00016350510019892. [DOI] [PubMed] [Google Scholar]
- 15.Arpornmaeklong P, Shand JM, Heggie AA. Stability of combined Le Fort I maxillary advancement and mandibular reduction. Australian Orthod J. 2003;19:57–66. [PubMed] [Google Scholar]
- 16.Mucedero M, Coviello A, Baccetti T, Franchi L, Cozza P. Stability factors after double-jaw surgery in Class III malocclusion. A systematic review. Angle Orthod. 2008;78:1141–52. doi: 10.2319/101807-498.1. [DOI] [PubMed] [Google Scholar]
- 17.Abeltins A, Jakobsone G, Urtane I, Bigestans A. The stability of bilateral sagittal ramus osteotomy and vertical ramus osteotomy after bimaxillary correction of class III malocclusion. J Craniomaxillofac Surg. 2011;39:583–7. doi: 10.1016/j.jcms.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Jakobsone G, Stenvik A, Sandvik L, Espeland L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: stability and risk factors for relapse. Am J Orthod entofacial Orthop. 2011;139:80–9. doi: 10.1016/j.ajodo.2009.03.050. [DOI] [PubMed] [Google Scholar]