Abstract
Objective
To review methods of measuring racial/ethnic health care disparities.
Study Design
Identification and tracking of racial/ethnic disparities in health care will be advanced by application of a consistent definition and reliable empirical methods. We have proposed a definition of racial/ethnic health care disparities based in the Institute of Medicine's (IOM) Unequal Treatment report, which defines disparities as all differences except those due to clinical need and preferences. After briefly summarizing the strengths and critiques of this definition, we review methods that have been used to implement it. We discuss practical issues that arise during implementation and expand these methods to identify sources of disparities. We also situate the focus on methods to measure racial/ethnic health care disparities (an endeavor predominant in the United States) within a larger international literature in health outcomes and health care inequality.
Empirical Application
We compare different methods of implementing the IOM definition on measurement of disparities in any use of mental health care and mental health care expenditures using the 2004–2008 Medical Expenditure Panel Survey.
Conclusion
Disparities analysts should be aware of multiple methods available to measure disparities and their differing assumptions. We prefer a method concordant with the IOM definition.
The term “disparity,” when referring to the quality and access to health care among population groups, connotes not only a difference but also inequality and unfairness. Applying this term to differences in health care between non-Latino whites and racial/ethnic minority groups is thus inherently controversial, and it necessitates explicit choices about what types of racial/ethnic differences are justifiable and those that are not. The definition of disparity elected should determine the analytical methods that are used to measure disparities.
We focus in this article on racial/ethnic disparities in utilization of health care, under which we subsume differences in access and quality measures of receipt of appropriate services.1 Definitions for racial/ethnic health care disparities have not been consistent in the health services research literature. In this article, we (1) summarize the definitions and methods used in this literature, arguing for a definition proposed by a report of the Institute of Medicine (IOM 2003); (2) describe and compare methods for implementing this IOM definition; (3) illustrate how IOM-concordant methods may be used to assess underlying mechanisms of disparities; and (4) explore how lessons learned from the development of IOM-concordant methods may be relevant to studies of health care inequality and fairness.
Varying Definitions of Racial/Ethnic Disparity
We can identify three commonly used definitions of racial/ethnic health care disparities, each associated with corresponding statistical methods (Table 1). The first focuses on the race/ethnicity coefficient in a multivariate regression model after adjustment for all other factors available to the researcher, including socioeconomic status (SES) variables; we call this estimator the “residual direct effect” (RDE). This definition makes no distinction between variables which may be legitimate sources of differences in utilization (e.g., health status) and those which may represent race-related disadvantage whose effects on utilization are of concern (e.g., education, income, and other measures of SES). Controlling for the latter tends to “absorb” some of the effect of race/ethnicity, so the RDE estimates only that part of racial differences not mediated through measurable disadvantage.
Table 1.
Summary of Three Main Definitions and Methods of Disparities Measurement with Examples, Pros, and Cons
| Definition | Method | Example | Pros | Cons |
|---|---|---|---|---|
| Residual direct effect | Compare mean white health care use with mean health care use in a counterfactual group that is similar to the white group in all aspects except having racial/ethnic minority identity | Logit results for models of any reported ambulatory visits by year 1997 (reported as odds ratios with whites as comparison group). Black OR = 0.46 (0.35, 0.59); Latino OR = 0.7 (0.56, 0.89) (Guevara et al. 2006) | Readily interpreted from standard regression output. Identifies independent effect of race | Adjusts for racial/ethnic differences in care that are due to SES variables such as income, insurance, and education |
| Disparities equal to unadjusted means | Compare mean white health care use with mean health care use of racial/ethnic minority group | Percentage of people who had an office-based or outpatient department visit in the calendar year, by race and ethnicity, 2007. White 75.3% versus black 65.7% versus Hispanic 59.1% versus Asian 62.7% (AHRQ 2010) | Easily computable and understandable comparison | Does not account for health status and age differences between populations |
| Institute of Medicine (IOM) definition | Compare mean white health care use with mean health care use of a counterfactual group that has the SES characteristics and racial/ethnic identity of the racial/ethnic group but the health status of the white group | Predicted probability of having any mental health care use in the last year, 2007. 15.7% Whites versus 7.0% blacks versus 8.3% Latinos (Cook et al. 2010) | Accounts for racial/ethnic differences by health status, age, and gender | Uses a rank and replace prediction method that is more computationally intensive than other methods |
Another definition is exemplified in both Healthy People 2010 (USDHHS 2000) and the AHRQ National Healthcare Disparities Reports (NHDR) (AHRQ 2004, p. 7): “In pursuit of the overarching goal of eliminating health disparities, all differences among populations in measures of health and health care are considered evidence of disparities.” This definition is implemented by simply assessing differences in group means. A limitation of this definition is that racial/ethnic group differences that many would consider to be appropriate in an equitable health care system because of intergroup differences in need (e.g., as being due to differences in distributions of age or health status) are included in these differences in utilization.
We prefer a third definition of racial/ethnic health care disparity based on the definition put forth in the Unequal Treatment report (IOM 2003): disparities are differences in health care services received by the two groups that are not due to differences in the underlying health care needs or preferences of members of the groups.2 Differences that are considered to be disparities include differences due to the operation of health care systems, the legal and regulatory climate, discrimination, or other factors (Figure). We focus here on the IOM definition because (1) we believe it correctly parses out the differences that are just and unjust, and (2) implementation of the IOM definition requires statistical methods that are not as familiar to the health services research field as methods of implementing the major alternative definitions.
Figure 1.
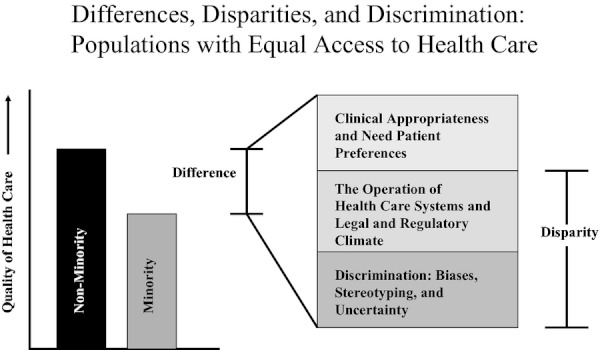
The Institute of Medicine (IOM 2003, p. 4) Definition of Racial/Ethnic Healthcare Disparities
An important contribution of the IOM definition is that it explicitly specifies the sources of racial/ethnic health care differences, distinguishing which should be considered to contribute to a disparity. Exclusion of differences due to clinical need and appropriateness (assessed by health status variables) from disparities reflects the normative stance that these differences are allowable. For example, in some analyses we found the Latino group to be healthier than non-Hispanic whites (younger on average and with lower rates of illness based on available diagnostic variables) and therefore to have a clinically predictable lesser need for care (Cook, McGuire, and Zuvekas 2009a; Cook et al. 2010). The health care system should therefore not be faulted for providing them with less care commensurate with their predicted difference in needs. On the other hand, in many analyses blacks have more severe illness than a white comparison group. In this case, a health care system that provides the same amount of services to blacks as whites would be providing disparate care according to the IOM definition given the greater clinical needs of the black population. In these examples, adjustment of health status operates differently for the two populations. Adjusting for health status and age, the Latino use would move from lower use than whites to zero difference, whereas black use would move from zero difference to lower use than whites.
The IOM definition includes as part of the disparity differences that are due to SES and other individual characteristics other than health status, reflecting a view that differences in care provided due to SES factors such as income and education are unjustifiable and health systems should be accountable for such differences. In many of our prior studies, we have found both Latinos and blacks to have lower SES characteristics than whites and that the lower SES groups receive less treatment than whites. These differences are not warranted and should contribute to the disparity according to the IOM.
The introduction of the IOM definition of health care disparities into the racial/ethnic health care disparities literature has been criticized on two grounds. The first is that the IOM definition does not isolate “racial” disparities. According to this critique, differences due to socioeconomic factors should not be included in the disparity calculation, so the residual race effect (i.e., the RDE from above), after adjustment for these factors, should be the measure of disparity (Klick and Satel 2006). Like Bloche (2004), we counter that health care systems should not be providing poorer treatment to individuals in lower SES categories, and hence mediation of racial/ethnic differences by income, wealth, insurance, and other socioeconomic factors does not negate racial/ethnic disparities. Rather, identification of SES as a mediator is policy relevant and may help to identify approaches to ameliorate the racial/ethnic disparities.
The second critique conversely objects to adjustment for health status in the IOM definition because differences in health status have systematic historical and structural causes that should be addressed. We counter that our analyses are intended to measure the current performance of health care systems for the population. The equity of health care systems should be evaluated by a definition that tracks their performance with clinically comparable groups of patients of different races/ethnicities, unaffected by differences in the current case mix of patients due to factors not controlled by the system under evaluation.
The debate on the correct definition of racial/ethnic health care disparity not only has a significant impact on disparities measurement and results but also is of policy significance given the large number of private and government institutions funding initiatives and research on reducing disparities. Implementing a consistent definition with suitable methods is key to establishing baseline rates of health care use and quality, tracking disparities, and evaluating policy and systems interventions.
Implementing the IOM Definition of Health Care Disparities
Implementing the IOM definition of racial/ethnic health care disparities requires a method that adjusts for some variables but not others, unlike the RDE and unadjusted methods, distinguishing between differences that are due to one set of characteristics (clinical need/appropriateness and patient preferences) and differences due to all other factors.
Implementation Issue 1: Identifying Datasets with Appropriate Health Status, Preferences, and SES Variables
Nationally representative datasets are commonly used to measure health care disparities; a number of these provide sufficient data to assess disparities at the national level (Sequist and Schneider 2006). Examples include the Medical Expenditure Panel Survey (MEPS) (Kirby, Taliaferro, and Zuvekas 2006; Cook, McGuire, and Zuvekas 2009a), the National Latino and Asian American Survey (Alegria et al. 2008), the National Epidemiologic Survey on Alcohol and Related Conditions (Blanco et al. 2007), Healthcare Cost and Utilization Project (Coffey, Andrews, and Moy 2005), and Medicare claims data (Jha et al. 2005). For example, the annually released MEPS records the health and health care use of approximately 16,500 new respondents each year, with detailed information on every family member's income, employment, public program participation and eligibility, health insurance coverage, and other sociodemographic characteristics. These datasets are useful for disparities studies because of large sample sizes of racial/ethnic minorities and their extensive health care utilization and health status data. Limitations of these datasets include the difficulty of drawing conclusions about geographic differences due to small local-area sample sizes.
To apply the IOM definition in these large, national health care datasets, the researcher must decide how to match survey variables with the constructs identified in the IOM definition (see Figure). We typically use variables describing health status, health conditions, or characteristics predictive of health status such as age and sex to represent clinical appropriateness and need. Subsets of these variables are readily available in administrative and nationally representative survey datasets in the United States and other countries (e.g., Bago d'Uva, Jones, and van Doorslaer 2009) and provide a basis for predicting optimal levels of care. We capture the operation of health care systems and the legal and regulatory climate using SES variables such as educational attainment, employment status, income, and health insurance, considering these variables to be possible predictors of differential treatment by the health care system. For example, individuals of lower SES may have more difficulty paying for health care and navigating the complexities of the health care system to receive appropriate treatment. If this leads to poorer health care, and minorities are disproportionately represented in lower SES categories, then the operation of the health care system creates racial disparities through SES. Discrimination due to biases may independently influence health care through discriminatory practices by providers or health services organizations that lead to disparate access to care and rates of utilization. In the absence of discrimination measures in most national health care databases, we capture discrimination using race/ethnicity indicator variables, as is common in the labor economics literature (Baldwin and Johnson 1996; Oaxaca and Ransom 1999; Kim 2010), recognizing that this residual effect may include the effect of other important unmeasured variables that differ by race/ethnicity (National Research Council 2004). The list of unmeasured variables varies by survey but satisfaction with prior care and health beliefs are constructs that are rarely measured and may be relevant to utilization independent of discrimination.
Identifying variables related to preferences is more problematic. These variables are rarely or incompletely measured in national surveys. For example, in the MEPS, respondents are asked whether they believe illness can be overcome without medical help. Other possible proxies for preferences are items on risk aversion, but these often hypothetical questions may not provide information specific enough to be useful. Some smaller scale surveys have used more targeted measures of preferences. For example, Cooper et al. (2003) elicited preferences for antidepressant medications and counseling among depressed primary care users and Ayanian et al. (1999) assessed preferences for renal transplantation among individuals with end-stage renal disease.
Implementation Issue 2: What Differences Should Count as a Disparity?
Deciding which variables are acceptable sources of differences may be ambiguous and context-dependent. Four such categories of problematical variables are preferences, geography, insurance status, and comorbidities.
In addition to the absence of patient preference measures in national datasets (as described above), analysts also must grapple with the problematical classification of preferences as an “allowable” source of differences according to the IOM definition. Patients are rarely “fully informed” about their clinical options when deciding to access health care (Ashton et al. 2003; IOM 2003). Braddock et al. (1999) found that only 9 percent of clinical decisions met this demanding standard. Minority patients may be even less likely than whites to be fully informed because of language and cultural barriers to communication with providers, leading to inaccurate assumptions about the risks and benefits of certain procedures (Katz 2001). Further complicating the treatment of preferences is that they may themselves have been shaped by historic and current group experiences of inferior care and discrimination, which could affect trust in providers and expectations regarding the efficacy of care (Cooper-Patrick et al. 1997; Katz 2001). The problem here is a version of the “adaptive preferences” argument addressed by philosophers, such as Sen (1999) and Nussbaum (2001). Members of racial/ethnic minorities may have negative, distrustful attitudes toward health care that manifests as a “preference” for less or different treatments. It is not clear that differences due to preferences that are due in part to past discrimination, for example, should be excluded from a disparity estimate.
Should effects of differing geographical distributions of racial/ethnic groups be adjusted away when assessing health care disparities, or are geography-based differences unfair? The relationship between geographical and racial/ethnic disparities has received significant attention in health services literature (White, Haas, and Williams in press). Racial/ethnic disparities in a number of health care procedures can be largely explained by the concentration of minority patients in areas with poorer care, while within those areas minority-white disparities do not exist (Skinner et al. 2003; Baicker et al. 2004; Baicker, Chandra, and Skinner 2005). In some respects, geographical concentration of minorities is like a preference, and similarly problematical when concentration in underserved areas is a consequence of residential segregation (Massey and Denton 1993), underfunding of minority areas, and the historical legacy of slavery. When possible, researchers should assess the contribution of geographical differences by estimating disparities with and without adjustment for geography (Zaslavsky and Ayanian 2005). This is important for policy makers given that different interventions might be required to reduce disparities within and between regions.
Minorities and whites differ on insurance status (i.e., blacks and Latinos are more likely than whites to be enrolled in Medicaid), and health insurance tends to have large effects on rates of use. Insurance status is typically regarded as a systems-level variable, but it can be strongly correlated with unmeasured aspects of health status. In one study (McGuire et al. 2006), individuals with Medicaid were actually more likely to receive mental health care than those in more generous private insurance plans, suggesting that the Medicaid population was sicker and used more mental health care, even after adjustment for numerous physical and mental health status measures. Insurance status, in this case, seemed to be a proxy for unmeasured health status variables and we therefore considered insurance status in both categories (as a health status variable and a SES variable) in an analysis of the sensitivity of disparities estimates to these alternative interpretations.
Comorbidities, diseases other than the one under study, are among the variables typically adjusted for in disparities analyses. This may be appropriate—comorbidities confound the relationship between race/ethnicity and health care use because they are correlated with race and are related to severity of need for health care use. For example, an individual with depression and a physical health comorbidity may need more mental health care because of a greater severity of illness than an individual with depression only. Another pathway by which a comorbidity might affect health care use is that comorbidities increase the likelihood and number of primary care provider visits, making the illness under study more likely to be diagnosed in primary care (Cook et al. 2011). The relationship among illnesses is reciprocal in this respect—treatment of any illness may increase the likelihood of recognition of other illnesses. Health care treatment of any form should probably be regarded as endogenous in empirical models incorporating comorbidities. If it is clear that persons with comorbidity use more care for the illness under study not because their need is greater, but because the system is more likely to recognize them, the interpretation of the racial difference due to comorbidity should change from a need to a system variable. Cook et al. (2011) found that adjusting for comorbidities decreased estimates of black/white mental health care disparities and increased estimated Latino/white mental health care disparities compared to analyses that did not adjust for comorbidities.
To show how these adjustment considerations differ in practice, we empirically compare estimates of disparities for two mental health care variables (any mental health care and mental health care expenditures) adjusting for the following: (1) no variables, (2) need, (3) need and region, (4) need and Medicaid or Medicare enrollment, (5) need minus physical health comorbidities, and (6) all variables, using data from adult respondents of the 2004–2008 MEPS (see Table 2). While this should only be considered as a single application of these methods, one can glean from this example the influence of the choice of method and choice of need variables on the magnitude of disparity estimates. While disparities were significant in all analyses, their magnitude varied by method (significantly so in some cases). Whether adjustment for need increased or decreased disparity estimates depended on the response variable and racial/ethnic group being studied. Comparing only the four IOM-concordant analyses, the magnitude of change in disparity estimates was considerable in some cases although not statistically significant. For example, considering Medicaid and Medicare enrollment as a need variable substantially increased black/white disparities in mental health care expenditures and decreased Latino/white disparities in any mental health care. Considering comorbidities as a system-level variable rather than a need variable decreased black/white disparities in any mental health care.
Table 2.
Comparison of Racial/Ethnic Disparities in Mental Health Care Adjusting for Different Sets of Variables
| Non-Latino White | Black/White Disparity | Hispanic/White Disparity | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | |
| Any mental health care | ||||||
| Unadjusted differences | 16.61% | 0.3% | 8.74% | 0.5% | 8.46% | 0.6% |
| IOM concordant | ||||||
| Adjusting for need* | 16.61% | 0.4% | 9.83% | 0.5% | 8.06% | 0.4% |
| Adjusting for need and region | 16.61% | 0.4% | 9.79% | 0.5% | 8.10% | 0.5% |
| Adjusting for need and Medicaid, Medicare enrollment | 16.61% | 0.4% | 9.79% | 0.5% | 7.23% | 0.5% |
| Not adjusting for comorbid physical health conditions | 16.61% | 0.4% | 9.58% | 0.5% | 8.59% | 0.5% |
| Adjustment for full set of covariates† | 16.61% | 0.4% | 9.27% | 0.5% | 5.64% | 0.6% |
| Mental health care expenditure ($FY 2008) | ||||||
| Unadjusted differences | 209.92 | 6.9 | 49.56 | 21.2 | 105.81 | 10.8 |
| IOM concordant | ||||||
| Adjusting for need* | 210.26 | 7.3 | 91.55 | 17.6 | 104.77 | 12.1 |
| Adjusting for need and region | 210.26 | 7.3 | 87.85 | 18.1 | 104.47 | 11.9 |
| Adjusting for need and Medicaid, Medicare enrollment | 210.26 | 7.3 | 104.35 | 15.8 | 102.43 | 12.0 |
| Not adjusting for comorbid physical health conditions | 210.26 | 7.3 | 83.22 | 12.2 | 106.88 | 16.2 |
| Adjustment for full set of covariates† | 210.26 | 35.5 | 141.42 | 53.1 | 135.41 | 78.3 |
Note. IOM-concordant prediction method incorporates coefficients from a model with a full set of covariates and adjusted need variables (using the rank-and-replace methodology).
Need variables include self-reported physical and mental health, physical and mental health scores on the SF-12, diagnosis of diabetes, coronary heart disease, angina, asthma, high blood pressure, myocardial infarction, stroke, emphysema, joint pain, arthritis, other heart disease, three or more of the above conditions, five or more of the above conditions, age, sex, and marital status.
Other variables entered into this model are education (<high school [HS: referent], HS graduate, any college, college graduate), interactions between race/ethnicity and education, income (<100% federal poverty level [FPL: referent], 100–125% FPL, 125–200% FPL, 200–400% FPL, 400%+ FPL), insurance status (private [referent] Medicaid, Medicare, other public, uninsured), and HMO enrollment. IOM-concordant and full adjustment predictions are based in regression models (logistic regression model for any mental health care and two-part generalized linear model for mental health care expenditure).
Source: 2004–2008 Medical Expenditure Panel Survey (MEPS).
Implementation Issue 3: Choosing a Statistical Method to Implement the IOM Definition
Assuming that the analyst is able to identify sets of variables that accurately represent the constructs in the IOM definition, we have proposed four methods to implement the definition, with the objective of adjusting for racial/ethnic differences due to health status variables but not differences due to SES variables (Table 3 and citations therein). Each of these methods in effect modifies data to construct comparison minority and white populations that have similar distributions of health status (and preferences, if included) but maintain (exactly or approximately) the observed differences in SES variables. Comparisons of mean predicted service utilization (overall, or particular services that can be regarded as quality of measures) are then conducted between these artificial (counterfactual) comparison groups. Adjustment for health status variables in linear models is straightforward because the predicted mean equals the prediction when the mean of each variable is substituted into the prediction equation; thus, minority group means can be replaced with white group means for each health status variable (or vice versa). The four methods described in Table 3 are intended for use in nonlinear models where replacement of the entire distribution, not just substitution of means, is necessary.
Table 3.
Methods for Implementing the IOM Definition of Health Care Disparities
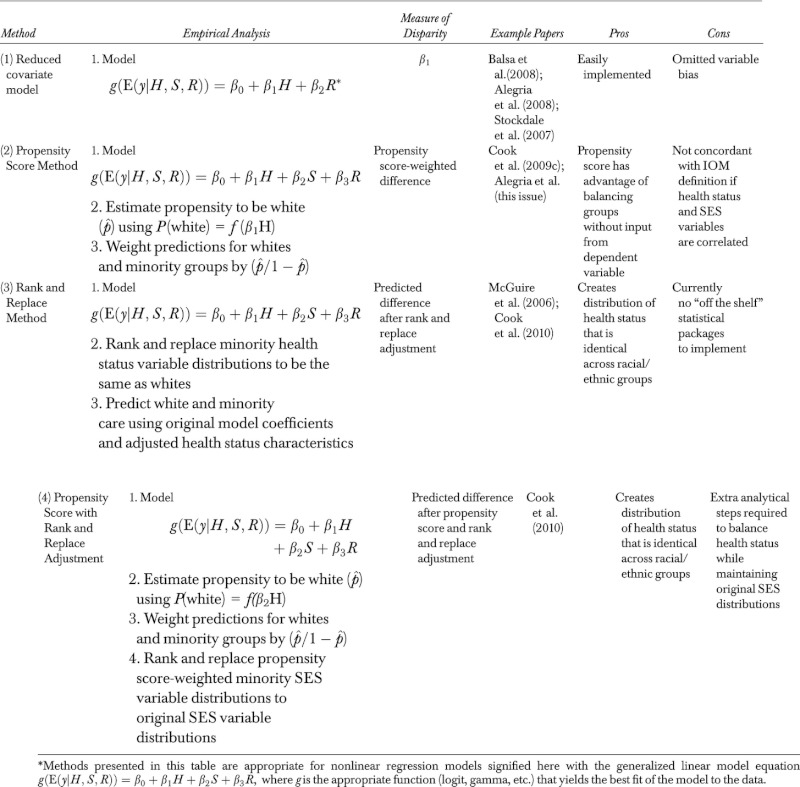 |
Methods (3) and (4)—the rank and replace and propensity score with rank and replace adjustment methods—maintain the SES distributions of each group, and we therefore consider them fully concordant with the IOM definition. The first two methods are less computationally intensive and adjust for health status but also modify the minority group's SES distribution. More detail on the implementation of these methods is available in the Appendix SA2 and in previous publications (McGuire et al. 2006; Cook et al. 2009c, 2010).
The magnitude of disparity estimates can depend on the method used (Cook, McGuire, and Zuvekas 2009a; Cook et al. 2009c, 2010). In most of our empirical analyses, the greatest disparities were identified using unadjusted mean comparisons and the smallest disparities were calculated using the RDE methods with the IOM method in the middle of those two estimates. Comparing within the four IOM-concordant methods described above, there were differences in magnitude across most comparisons (e.g., black/white disparities in total health care expenditures were $1,125, $1,285, $1,407, and $1,454 using methods 1–4, respectively; Cook et al. 2009c). Rarely, the significance, but not direction, of the disparity also changed depending on the method used (Cook et al. 2009c, 2010). The latter two adjustment methods provide a counterfactual comparison between the health care use of a counterfactual racial/ethnic minority group and the use of a factual white group. The selection of this counterfactual population is a normative act and slight variants to the counterfactual groups can be plausibly argued and implemented, which would change the results of disparity calculations.
These methods identify differences between racial/ethnic groups at the mean, potentially obscuring very different magnitudes of disparities at the upper ends of the distributions of utilization. Persistent or growing disparities at the upper tails of expenditures may be of policy importance, suggesting either undertreatment of minorities with the greatest need for care or wasteful overspending in the white comparison group. Using quantile regression to assess disparities in the upper tail of the distribution of medical care expenditures (Cook and Manning 2009), we have identified persistent disparities in the upper tail of expenditures for both blacks and Latinos.
Another fundamental limitation of all of these methods is that they can only assess differences between treatment received by patients with similar clinical conditions in two groups but cannot detect whether care for diseases and conditions disproportionately affecting a group is generally at an adequate and equitable level. Assessing this type of equity requires a more substantive consideration of needs, benefits, and resource allocation.
Identifying Underlying Pathways of Disparities Using Cross-Sectional Data
The persistence of disparities identified in a number of studies (Blanco et al. 2007; Cook, McGuire, and Miranda 2007; Cook, McGuire, and Zuvekas 2009a; Horvitz Lennon et al. 2009) suggests the importance of moving beyond description to improving the understanding of the underlying pathways leading to disparities to inform policy and clinical interventions. Decomposition methods developed in implementing the IOM definition hold promise for identifying these pathways and provide an alternative to other decomposition methods used in the labor economics and increasingly in the health services literature (Hargraves and Hadley 2003; Hudson, Miller, and Kirby 2007; Kirby, Hudson, and Miller 2010).
Once statistical models of health care use or health care disparities are established, decomposition methods can be used to split racial/ethnic differences into differences of means and differences of coefficients for each predictor variable. The differences in means inform us of the contribution of underlying characteristics to the disparity (e.g., part of the disparity is due to the greater likelihood that blacks are in lower income groups than whites), while the differences in coefficients inform us of the racial/ethnic differences in the “responses” of the health care system to the underlying characteristics (e.g., the positive returns of higher education on mental health care use may be greater for whites than blacks). These methods have been widely used in linear regression models (Blinder 1973; Oaxaca 1973), and numerous applications have grappled with the difficulties inherent in applying decomposition methods in nonlinear models (Yun 2004; Fournier 2005; Fairlie 2005). The rank and replace and propensity score methods potentially provide an alternative to nonlinear decomposition techniques. Predicting differences with and without adjustment for a variable or set of variables can help to isolate the impact of certain factors on differences in health or health care (Cook, McGuire, and Zuvekas 2009a. For example, in a paper identifying pathways underlying the paradox that immigrants have poorer SES but greater mental health status, Cook et al. (2009b) used the rank and replace technique to identify the independent contribution of a number of factors (discrimination, ethnic identity, intergenerational conflict) on mental health differences between Latino immigrants and U.S.-born Latinos. These decomposition methods have the advantage of allowing us to view the contribution of each variable of interest to the disparity estimate. While acknowledging that these methods do not demonstrate causal relationships, they do provide evidence for policy makers and clinicians as to the most malleable targets for disparities reduction.
Looking Ahead
We propose a method of measuring and understanding disparities that is grounded in a theoretically driven definition that explicitly excludes differences due to clinical appropriateness and need. This exclusion carries with it normative judgments not only for what constitutes a disparity but also indirectly identifies what should be done to address disparities. A focus on alleviating disparities that are not caused by health status posits that the health care system is responsible for reducing the disparities among the patients as they see them now, not for the cumulative effects of prior socioeconomic or discriminatory events that have led to their current health status. We recognize that disparities stem from persistent social inequalities in jobs, education, and other factors, and fundamental changes in social policy, not just health policy, may be necessary to eliminate disparities in health care. The broad IOM definition is not without critics, and the methods that we have developed to implement this definition continue to evolve. However, we firmly believe that disparities analysts should use an explicit definition of disparities and align their statistical methods with that definition so that studies can be compared, and health care disparities can be consistently tracked and monitored moving forward.
Improved interdisciplinary dialog is needed between researchers focused on racial/ethnic health care disparities and other inequality researchers. Three fields of research in particular have grappled with the issue of identifying variables that are justified and not justified when measuring inequality. First, the health care inequalities literature has developed and refined a “concentration index” that distills the equality of allocation of resources across the SES distribution to a single number (e.g., Wagstaff and Van Doorslaer 2000; van Doorslaer and Van Ourti 2011). This line of scholarship mirrors the development of disparities methods in that it attempts to identify partial indicators that measure the independent influence of a selected individual characteristic (SES) and has grappled with the identification of which partial inequalities are a cause for concern (e.g., because they are factors that are beyond the control of the individual; Roemer 2002), and which are ethically legitimate (Fleurbaey and Schokkaert, 2012). Methods used in this literature share characteristics with the rank and replace and propensity score methods (though they are applied to continuous SES variables rather than categorical racial/ethnic group indicator variables) in that they adjust groups’ health status levels to be standardized or equalized across groups. They also attempt to overcome the same fundamental hurdle that justifiable differences and unjustifiable differences are themselves correlated. The treatment of these correlations thus becomes essential to identifying plausible methods of implementation in nonlinear settings (Gravelle 2003; van Doorslaer, Koolman, and Jones 2004).
A contribution of the inequality literature is to integrate partial indicators to assess overall inequality, explicitly tackling the creation of a summary that combines partial indicators to compare nations (or other entities) on the inequality of their overall health or health care systems. Racial/ethnic differences are but a partial difference if we were to compare inequality across geographic areas (nations, states, counties) or health care systems or hospitals. Whereas the IOM definition explicitly incorporates differences due to SES factors into racial/ethnic disparities calculations, an alternative would be to create more holistic metrics of inequality that explicitly analyze the independent and interactive effects of race, SES, and gender differences (Williams 2011). In fact, there is a danger in focusing on one of these differences given the potential consequence that class or gender differences may be disguised (Kawachi, Daniels, and Robinson 2005).
Second, the literature on racial disparities in health care also shares characteristics and has important insights to lend to the literature on measuring disparities in health outcomes. As with studies of health care disparities, researchers conducting studies of disparities in health outcomes have to make a decision as to which racial/ethnic differences are justifiable in the disparities calculation and which are not. Taking mortality from cancer as a general example, when comparing death rates across groups, analysts typically adjust for age to avoid confounding due to the fact that the different populations have different age distributions and the risk of the disease also varies by age. Direct and indirect standardization are often used to adjust health outcomes for age and gender (Gordis 1996), but these methods are more difficult to implement if the analyst wishes to standardize rates across multiple independent variables.
Third, there has been considerable debate over the roles of genetic and social influences in racial/ethnic health disparities (Shields and Crown in press), a debate that raises similar methodological concerns related to decomposition and adjustment. Some genetics researchers assert the importance of genetic differences among racial groups to racial disparities in health (e.g., Edwards 2003; Leroi 2005), contrary to the now-dominant view that race is a social construction, dating back to Lewontin (1972) who identified greater genetic variation within race than between races. Critical reactions to this geneticist view include the argument that health disparities should be attributed to social factors differentially activating gene expression, not to underlying genetic differences (Krieger 2006). At least in some cases, racial/ethnic disparities are diminished with adjustment for SES indicators and disappear completely (in the case of black/white differences in low birthweight) with additional adjustment for self-reported experiences with discrimination (Collins et al. 2000). As genetic data become more available in national datasets, the decomposition methods described above may help to resolve this debate. Furthermore, an emphasis on being explicit in the definition of health disparities (choosing those differences that are justifiable) may help to more carefully target policies focused on reducing health disparities.
The methods of identifying racial/ethnic health care disparities can benefit from cross-fertilization with researchers from these other areas of inequality research. We encourage this work given the seeming intractability of health care disparities in the United States and the rising inequality in many areas of the world. While accurate and consistent measurement will not reduce inequalities, it will greatly assist in tracking inequality over time and evaluating the allocation of resources that are being deployed to reduce these inequalities.
Notes
Disparities and unfairness can be measured across other dimensions as well. A significant body of work exists in geographic (e.g., Fisher et al. 2008) and socioeconomic status health care disparities (e.g., Braveman et al. 2010), and there are important interactions among these partial contributors to overall health care inequality (Baicker, Chandra, and Skinner 2005; White, Haas, and Williams in press; Fleurbaey and Schokkaert, 2012).
An issue that arises immediately upon considering this definition is whether health status and preferences may be affected by disparities in access to health care in the past. We consider this point later.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Methods for Implementing the Institute of Medicine Definition of Racial/Ethnic Health Care Disparities.
Please note:Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- AHRQ. National Healthcare Disparities Report, 2004. Rockville, MD: Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- AHRQ. National Healthcare Disparities Report, 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- Alegria M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Jackson J, Meng XL. “Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States”. Psychiatric Services. 2008;59((11)):1264. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Chen C-C, Cook BL, Duan N, Meng X-L. “Disparities in Mental Health Services: Results from the Collaborative Psychiatric Epidemiological Survey.”. Health Services Research. In press. [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O'Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL., Jr “Racial and Ethnic Disparities in the Use of Health Services: Bias, Preferences, or Poor Communication?”. Journal of General Internal Medicine. 2003;18((2)):146–52. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayanian J, Cleary P, Weissman J, Epstein A. “The Effect of Patients’ Preferences on Racial Differences in Access to Renal Transplantation”. New England Journal of Medicine. 1999;341((22)):1661–9. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- Bago d'Uva T, Jones A, van Doorslaer E. “Measurement of Horizontal Inequity in Health Care Utilisation Using European Panel Data”. Journal of Health Economics. 2009;28((2)):280–9. doi: 10.1016/j.jhealeco.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner J. “Geographic Variation in Health Care and the Problem of Measuring Racial Disparities”. Perspectives in Biology and Medicine. 2005;48(1 suppl):S42–53. [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner JS, Wennberg JE. “Who You Are and Where You Live: How Race and Geography Affect the Treatment of Medicare Beneficiaries”. Health Affairs (Millwood) 2004 doi: 10.1377/hlthaff.var.33. Suppl Web Exclusives: VAR33-44. [accessed February 7, 2012]. Available at http://content.healthaffairs.org/content/early/2004/10/07/hlthaff.var.33.citation. [DOI] [PubMed] [Google Scholar]
- Baldwin ML, Johnson WG. “The Employment Effects of Wage Discrimination against Black Men”. Industrial and Labor Relations Review. 1996;49:302–16. [Google Scholar]
- Balsa AI, Cao Z, McGuire TG. “Does Managed Health Care Reduce Health Care Disparities between Minorities and Whites?”. Journal of Health Economics. 2007;26:101–121. doi: 10.1016/j.jhealeco.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Blanco C, Patel S, Liu L, Jiang H, Lewis-Fernandez R, Schmidt A, Liebowitz M, Olfson M. “National Trends in Ethnic Disparities in Mental Health Care”. Medical Care. 2007;45((11)):1012–9. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- Blinder A. “Wage Discrimination: Reduced Form and Structural Elements”. Journal of Human Resources. 1973;8((4)):436–55. [Google Scholar]
- Bloche MG. “Erasing Racial Data Erased Report's Truth”. Washington Post. 2004 February 15. [Google Scholar]
- Braddock CH, III, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. “Informed Decision Making in Outpatient Practice: Time to Get Back to Basics”. Journal of the American Medical Association. 1999;282((24)):2313–20. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. “Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us”. American Journal of Public Health. 2010;100((S1):S186. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey RM, Andrews RM, Moy E. “Racial Ethnic, and Socioeconomic Disparities in Estimates of AHRQ Patient Safety Indicators”. Medical Care. 2005;43((3)):I48–I57. doi: 10.1097/00005650-200503001-00008. [DOI] [PubMed] [Google Scholar]
- Collins JW, Jr, David RJ, Symons R, Handler A, Wall SN, Dwyer L. “Low-Income African-American Mothers’ Perception of Exposure to Racial Discrimination and Infant Birth Weight”. Epidemiology. 2000;11:337–9. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- Cook BL, Manning WG. “Measuring Racial/Ethnic Disparities across the Distribution of Health Care Expenditures”. Health Services Research. 2009;44((5p1):1603–21. doi: 10.1111/j.1475-6773.2009.01004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B, McGuire T, Miranda J. “Measuring Trends in Mental Health Care Disparities, 2000–2004”. Psychiatric Services. 2007;58((12)):1533–9. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zuvekas SH. “Measuring Trends in Racial/Ethnic Health Care Disparities”. Medical Care Research and Review. 2009a;66((1)):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, Alegria M, Guo J, Lin JY. “Pathways and Correlates Connecting Exposure to the U.S. and Latinos’ Mental Health”. American Journal of Public Health. 2009b;99((12)):2247–54. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zaslavsky AM, Meara E. “Adjusting for Health Status in Non-Linear Models of Health Care Disparities”. Health Services Outcomes and Research Methodology. 2009c;9((1)):1–21. doi: 10.1007/s10742-008-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire T, Lock K, Zaslavsky A. “Comparing Methods of Racial and Ethnic Disparities Measurement across Different Settings of Mental Health Care”. Health Services Research. 2010;45((3)):825–47. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B, McGuire T, Alegria M, Normand SLT. “Crowd-out and Exposure Effects of Physical Comorbidities on Mental Health Care Use: Implications for Racial-Ethnic Disparities in Access”. Health Services Research. 2011;46:1259–80. doi: 10.1111/j.1475-6773.2011.01253.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. “The Acceptability of Treatment for Depression among African-American, Hispanic, and White Primary Care Patients”. Medical Care. 2003;47:9–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe N, Jenckes M, Gonzales J, Levine D, Ford D. “Identification of Patient Attitudes and Preferences Regarding Treatment of Depression”. Journal of General Internal Medicine. 1997;12((7)):431–8. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doorslaer E, Koolman X, Jones A. “Explaining Income-Related Inequalities in Doctor Utilisation in Europe”. Health Economics. 2004;13:629–47. doi: 10.1002/hec.919. [DOI] [PubMed] [Google Scholar]
- van Doorslaer E, Van Ourti T. “Measuring Inequality and Inequity in Health and Health Care”. In: Glied S, Smith P, editors. Oxford Handbook on Health Economics. Oxford, England: Oxford University Press; 2011. pp. 837–69. [Google Scholar]
- Edwards AW. “Human Genetic Diversity: Lewontin's Fallacy”. Bioessays. 2003;25:798–801. doi: 10.1002/bies.10315. [DOI] [PubMed] [Google Scholar]
- Fairlie R. “An Extension of the Blinder-Oaxaca Decomposition Technique to Logit and Probit Models”. Journal of Economic and Social Measurement. 2005;30:305–316. [Google Scholar]
- Fisher ES, Goodman DC, Chandra A, Bronner KK. Disparities in Health and Health Care among Medicare Beneficiaries. Princeton, NJ: Robert Wood Foundation; 2008. [Google Scholar]
- Fleurbaey M, Schokkaert E. “Equity in Health and Health Care”. In: Pauly MV, McGuire TG, Barros PP, editors. Handbook of Health Economics. Vol. 2. Waltham, MA: North Holland; 2012. pp. 1003–92. [Google Scholar]
- Fournier M. “Exploiting Information from Path Dependence in Oaxaca-Blinder Decomposition Procedures”. Applied Economics Letters. 2005;12:669–72. [Google Scholar]
- Gordis L. Epidemiology. Philadelphia, PA: W.B. Saunders Company; 1996. [Google Scholar]
- Gravelle H. “Measuring Income Related Inequality in Health: Standardisation and the Partial Concentration Index”. Health Economics. 2003;12:803–19. doi: 10.1002/hec.813. [DOI] [PubMed] [Google Scholar]
- Guevara JP, Mandell DS, Rostain AL, Zhao H, Hadley TR. “Disparities in the Reporting and Treatment of Health Conditions in Children: An Analysis of the Medical Expenditure Panel Survey”. Health Services Research. 2006;41((2)):532–49. doi: 10.1111/j.1475-6773.2005.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargraves J, Hadley J. “The Contribution of Insurance Coverage and Community Resources to Reducing Racial/Ethnic Disparities in Access to Care”. Health Services Research. 2003;38((3)):809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvitz Lennon M, McGuire TG, Alegria M, Frank RG. “Racial and Ethnic Disparities in the Treatment of a Medicaid Population with Schizophrenia”. Health Services Research. 2009;44((6)):2106–22. doi: 10.1111/j.1475-6773.2009.01041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, Miller GE, Kirby JB. “Explaining Racial and Ethnic Differences in Children's Use of Stimulant Medications”. Medical Care. 2007;45((11)):1068–75. doi: 10.1097/MLR.0b013e31806728fa. [DOI] [PubMed] [Google Scholar]
- IOM. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. “Racial Trends in the Use of Major Procedures among the Elderly”. New England Journal of Medicine. 2005;353((7)):683–91. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- Katz JN. “Patient Preferences and Health Disparities”. Journal of the American Medical Association. 2001;286((12)):1506–9. doi: 10.1001/jama.286.12.1506. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Daniels N, Robinson DE. “Health Disparities by Race and Class: Why Both Matter”. Health Affairs. 2005;24((2)):343. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- Kim CH. “Decomposing the Change in the Wage Gap between White and Black Men Over Time, 1980–2005: An Extension of the Blinder-Oaxaca Decomposition Method”. Sociological Methods & Research. 2010;38((4)):619–51. [Google Scholar]
- Kirby JB, Hudson J, Miller GE. “Explaining Racial and Ethnic Differences in Antidepressant Use among Adolescents”. Medical Care Research and Review. 2010;67:342–63. doi: 10.1177/1077558709350884. [DOI] [PubMed] [Google Scholar]
- Kirby JB, Taliaferro G, Zuvekas SH. “Explaining Racial and Ethnic Disparities in Health Care”. Medical Care. 2006;44(5 suppl):I64–72. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- Klick J, Satel S. The Health Disparities Myth. Washington, DC: American Enterprise Institute; 2006. [Google Scholar]
- Krieger N. “If “Race” Is the Answer, What Is the Question—On “Race,” Racism, and Health: A Social Epidemiologist's Perspective. 2006. Social Service Research Council. Is Race “Real”? An Web Forum [accessed on November 15, 2011]. Available at http://raceandgenomics.ssrc.org/Krieger/
- Leroi AM. “A Family Tree in Every Gene”. New York Times. 2005 doi: 10.1007/BF02715883. March 14 [accessed on November 15, 2011]. Available at http://www.nytimes.com/2005/03/14/opinion/14leroi.html. [DOI] [PubMed] [Google Scholar]
- Lewontin R. “The Apportionment of Human Diversity”. Evolutionary Biology. 1972;6:391–98. [Google Scholar]
- Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. “Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care”. Health Services Research. 2006;41((5)):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. “Statistical Analysis of Observational Data”. In: Blank RM, Dabady M, Citro CF, editors. Measuring Racial Discrimination. Washington, DC: National Academy Press; 2004. pp. 121–61. [Google Scholar]
- Nussbaum MC. “Symposium on Amartya Sen's Philosophy: 5 Adaptive Preferences and Women's Options”. Economics and Philosophy. 2001;17((1)):67–88. [Google Scholar]
- Oaxaca R. “Male-Female Wage Differentials in Urban Labor Markets”. International Economic Review. 1973;14((3)):693–709. [Google Scholar]
- Oaxaca R, Ransom M. “Identification in Detailed Wage Decompositions”. Review of Economics and Statistics. 1999;81((1)):154–7. [Google Scholar]
- Roemer J. “Equality of Opportunity: A Progress Report”. Social Choice and Welfare. 2002;19((2)):455–71. [Google Scholar]
- Sen A. Development as Freedom. Oxford, England: Oxford University Press; 1999. [Google Scholar]
- Sequist TD, Schneider EC. “Addressing Racial and Ethnic Disparities in Health Care: Using Federal Data to Support Local Programs to Eliminate Disparities”. Health Services Research. 2006;41((4p1):1451–68. doi: 10.1111/j.1475-6773.2006.00549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields AE, Crown WH. “Incorporating Genomic Information into Disparities Research Methods: Reducing Measurement Error and Selection Bias”. Health Services Research. doi: 10.1111/j.1475-6773.2012.01413.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J, Weinstein JN, Sporer SM, Wennberg JE. “Racial Ethnic, and Geographic Disparities in Rates of Knee Arthroplasty among Medicare Patients”. New England Journal of Medicine. 2003;349((14)):1350–9. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. “Racial and Ethnic Disparities in Detection and Treatment of Depression and Anxiety Among Psychiatric and Primary Health Care Visits.” 1995–2005. Medical Care. 2008;46:668–77. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHHS. Healthy People 2010: Understanding and Improving Health. 2nd Edition. Washington, DC: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- Wagstaff A, Van Doorslaer E. “Income Inequality and Health: What Does the Literature Tell Us?”. Annual Review of Public Health. 2000;21((1)):543–67. doi: 10.1146/annurev.publhealth.21.1.543. [DOI] [PubMed] [Google Scholar]
- White K, Haas JS, Williams D. “Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation”. Health Services Research. doi: 10.1111/j.1475-6773.2012.01410.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. “Intersectionality of Race, SES and Gender in Health Disparities”. Health Services Research. In press. [Google Scholar]
- Yun M. “Decomposing Differences in the First Moment”. Economics Letters. 2004;82:275–80. [Google Scholar]
- Zaslavsky AM, Ayanian JZ. “Integrating Research on Racial and Ethnic Disparities in Health Care over Place and Time”. Medical Care. 2005;43((4)):303–7. doi: 10.1097/01.mlr.0000159975.43573.8d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


