Abstract
Background:
Propofol is one of the widely used intravenous (i.v.) anaesthetics, although pain on injection still remains a considerable concern for the anaesthesiologists. A number of techniques has been tried to minimize propofol-induced pain with variable results. Recently, a 5-HT3 antagonist, ondansetron pre-treatment, has been shown to reduce propofol-induced pain. The aim of our randomized, placebo-controlled, double-blinded study was to determine whether pre-treatment with intravenous granisetron, which is routinely used in our practice for prophylaxis of post-operative nausea and vomiting, would reduce propofol-induced pain.
Methods:
Eighty-two women, aged 18–50 years, American society of Anaesthesiologist grading (ASA) I–II, scheduled for various surgeries under general anaesthesia were randomly assigned to one of the two groups. One group received 2 mL 0.9% sodium chloride while the other group received 2 mL granisetron (1 mg/mL), and were accompanied by manual venous occlusion for 1 min. Then, 2 mL propofol was injected through the same cannula. Patients were asked by a blinded investigator to score the pain on injection of propofol with a four-point scale: 0=no pain, 1=mild pain, 2=moderate pain, 3=severe pain.
Results:
Twenty-four patients (60%) complained of pain in the group pre-treated with normal saline as compared with six (15%) in the group pre-treated with granisetron. Pain was reduced significantly in the granisetron group (P<0.05). Severity of pain was also lesser in the granisetron group compared with the placebo group (2.5% vs. 37.5%).
Conclusion:
We conclude that pre-treatment with granisetron along with venous occlusion for 1 min for prevention of propofol-induced pain was highly successful.
Keywords: Intravenous (I.V). granisetron, pain, pre-treatment, propofol injection
INTRODUCTION
With the decrease in morbid adverse events after surgery, patient satisfaction with perioperative care is assuming more importance. Pain on injection of anaesthetic is an important source of patient dissatisfaction and is a recognized adverse effect of propofol.[1] Among 33 low-morbidity clinical outcomes, considering clinical importance and frequency, pain during injection of propofol was ranked as the seventh most important problem of current clinical anaesthesiology.[2] The reported incidence of pain on injection of propofol varies between 28% and 90% in adults if a vein on the dorsum of the hand is used.[3,4] Several techniques have been proposed over the years to reduce the incidence and severity of such pain. However, all have variable results.[4–13]
It has been demonstrated that ondansetron, a specific 5-hydroxytryptamine (5HT3) receptor antagonist, provided numbness when injected under the skin.[14] It has been further demonstrated that ondansetron successfully relieved pain following propofol injection without any adverse effects in a significant number of patients.[8]
In our practice, granisetron is routinely administered as pre-medication to prevent post-operative nausea and vomiting in patients following general anaesthesia. Granisetron is a serotonin 5HT3 receptor antagonist and demonstrates superior efficacy and longer duration to ondansetron. We postulated that intravenous granisetron, being a potent 5HT3 antagonist, might decrease pain on injection of propofol. In a randomized, double–blinded study, we used granisetron pre-treatment to determine whether it might decrease the pain of propofol injection.
METHODS
Institutional ethical committee approval was obtained and informed consent was taken from all the patients. All adult women, ASA I or II, aged between 18 and 50 years presenting for elective surgery under general anaesthesia were candidates for inclusion in the study. Patients were explained about the procedure during the pre-anaesthetic visit. Those patients with difficulty in communication were excluded from the study. Patients who had a history of allergic response to either propofol or 5HT3 receptor antagonist, or received any analgesic or sedative drugs within 24 h prior to surgery, were also excluded from this study.
Eighty-two patients were studied, but two patients were excluded as they received analgesic medication within 24 h of surgery. All patients were fasted for 8 h. Patients received either granisetron pre-treatment 2 mg in a total volume of 2 mL (n=40) or 2 mL 0.9% saline pre-treatment as a placebo (n=40) 60 s before the administration of propofol according to a computer-generated randomization list. All drugs were prepared at operating room temperature (21–23°C) by an anaesthesiologist not involved in induction of anaesthesia. The investigator did not know the content of the solutions. No patient was given any pre-medication before the pre-treatment injection.
On arrival in the operation theatre, a 20G cannula was inserted into a vein on the dorsum of the patient's non-dominant hand and lactated Ringer's solution was infused. Heart rate and non-invasive blood pressure were measured. Heart rate, blood pressure and peripheral O2 saturation were recorded before injecting propofol and at 1 and 3 min after. Each patient received 2 mL of the pre-treatment solution for a period of 5 s 5 min after i.v. cannulation (time taken for applying monitors) while the venous drainage was occluded manually at mid-arm by an assistant. One minute after intravenous injection of pre-treatment solution, the occlusion was released and anaesthesia was induced with propofol 2.5 mg/kg. The initial 2 mL bolus was given over 4 s; 15 seconds later, the patient was asked to rate immediately any sensation of pain during injection of propofol. The grading of pain was similar to the method used in previous studies,[5,8,10] and was explained to the patients at the pre-anaesthetic visit as well as before giving propofol injection. An anaesthesiologist blinded to the study protocol evaluated pain during injection of propofol using a verbal rating scale: 0=none (negative response to questioning), 1=mild pain (pain reported only in response to questioning without any behavioural signs), 2=moderate pain (pain reported in response to questioning and accompanied by a behavioural sign or pain reported spontaneously without questioning) or 3=severe pain (strong vocal response or response accompanied by facial grimacing, arm withdrawal or tears). The patients as well as the anaesthesiologist were unaware of the nature of the test drug. Adverse effects, if any, were noted. Induction of anaesthesia was achieved with propofol. Tracheal intubation was facilitated with atracurium besylate and anaesthesia was maintained with nitrous oxide, oxygen and sevoflurane supplemented with fentanyl and intermittent positive pressure ventilation (IPPV).
Power calculation indicated that recruitment of 40 patients in each group would be significant to demonstrate a reduction of pain score of one at a level of significance of P<0.05 and power of 99.3%. The results were analyzed statistically using unpaired Student's ‘t’ test and Chi-square test with Yate's correction when appropriate. Results were considered statistically significant when a P value of <0.05 was obtained.
RESULTS
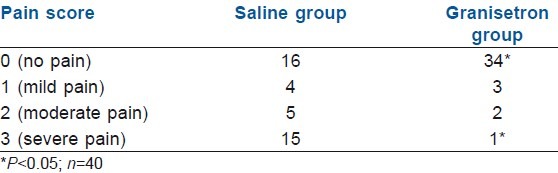
Patients’ age, weight and ASA physical status are presented in Table 1. There were no statistically significant differences between the groups. The number of patients who experienced pain or discomfort in either group is shown in Table 2. The overall incidence of pain in the saline group was 24 (60%), compared with 6 (15%) in the granisetron group (P<0.05). Fewer patients in the granisetron group experienced severe pain (2.5% vs. 37.5%; P<0.05) [Table 2]. The number of patients who experienced mild to moderate pain was nine and five in the saline and granisetron groups, respectively. No patient in either group experienced pain or discomfort during the injection of pre-treatment solution. There was transient rise in heart rate in patients suffering from pain of verbal rating scale (VRS) score 2–3 in both the groups, but no changes in blood pressure were noted.
Table 1.
Patients’ characteristics, values are mean (SD) where appropriate
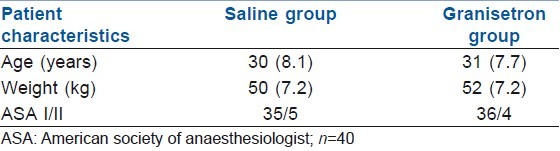
Table 2.
Number of patients with the pain scores shown after 2 mL intravenous propofol (1%) injection following pre-treatment solution
After propofol injection, no significant adverse reaction was seen in any group that needed active intervention.
DISCUSSION
The incidence of pain caused by propofol injection was reported to range from 28% to 90% in adults if a vein on the dorsum of the hand is used.[3,4] Therefore, considering the extensive use of propofol in clinical practice, the pain frequently reported on induction of anaesthesia cannot be neglected. Although the underlying mechanisms are still not fully understood,[15] the explanation for the pain include endothelial irritation, osmolality differences, unphysiological pH and the activation of pain mediators.[6] The initial component of pain, involving immediate stimulation of nociceptors and free nerve endings,[9] seems to be associated mainly with the concentration of free drug within the aqueous phase of the emulsion.[16] The delayed component of pain, appearing within half a minute, is also believed to result from interaction with nociceptors and free nerve endings[9]; however, promoted by local vasodilatation and hyperpermeability induced by bradykinin[17,18] and possibly also prostaglandin E2.[17,19]
Many methods have been used to reduce the incidence of pain on propofol injection with variable results. Lignocaine added to or given before injection of propofol is widely employed, although protection is not complete, with a failure rate of between 13% and 44%.[20,21] Cooling the propofol to 4°C reduces its injection pain possibly by delaying the activation of enzymatic cascade of pain mediators.[5] Injecting into a large forearm vein also reduces the pain, probably by reducing contact between drug and endothelium. Diluting propofol with intralipid[6] and the application of eutectic mixture of local anaesthetic cream to the skin before venepuncture have also been reported to reduce the incidence of propofol injection pain.[22] Metoclopromide shares the structural and physiochemical properties with lignocaine[23] and is a weak local anaesthetic.[24] It has been shown to be as effective as lignocaine in reducing propofol injection pain.[25] Opioids may also reduce the incidence of pain, and alfentanil has shown to reduce the incidence of pain following propofol injection from 84% to 36%.[12] Pre-treatment with some intravenous induction agents like ketamine,[9] thiopentone[10] and even propofol[13] itself in subanaesthetic doses have shown some promise in reducing the incidence and severity of propofol injection pain but not with ketamine pre-mixed with propofol.[26]
The incidence of pain in our study using dorsal hand vein was reduced from 60% to 15% by granisetron pre-treatment when the venous drainage was occluded manually at mid-arm by an assistant for 1 min after intravenous injection of pre-treatment solution. This compares favourably with other methods.
Ondansetron had been shown to relieve pain by its multifaceted actions as a Na channel blocker, a 5HT3 receptor antagonist and mu opioid agonist.[14,27] We presume that granisetron, a more refined 5HT3 antagonist,[27] therefore relieved pain by a similar mechanism.
We routinely use granisetron at the time of induction of anaesthesia for prevention of post-operative nausea and vomiting. This study was designed to ascertain whether pre-treatment with granisetron could alleviate the pain produced by an intravenous propofol injection. Manual compression of venous drainage for 1 min after injection of granisetron was allowed for its action to begin.[28] Pain was assessed 15 s after giving the propofol injection as the pain during propofol injection can be immediate or delayed, with the latter having a latency of between 10 and 20 s.[29]
Our results demonstrated an unacceptably high incidence of pain or discomfort in 60% of cases, which was decreased to 15% after granisetron pre-treatment. This may have been the result of a peripheral local anaesthetic action, which attenuated the afferent pain pathway rather than a central analgesic effect, similar to the mechanism of ondansetron. Although granisetron pre-treatment did not relieve the pain in all patients, it was successful in decreasing pain in 85% of the patients in our study in comparison with the study with ondansetron pre-treatment (50%).[8]
CONCLUSION
We conclude that pre-treatment with granisetron along with venous occlusion for 1min for prevention of propofol-induced pain is highly successful. Moreover, prevention of post-operative nausea and vomiting may be achieved along with alleviation of propofol-induced pain with a single agent that may be used especially in day-care surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Smith I, White PF, Nathanson M, Gouldson R. Propofol: An update on its clinical use. Anesthesiology. 1994;81:1005–43. [PubMed] [Google Scholar]
- 2.Macario A, Weinger M, Truong P, Lee M. Which clinical anesthesia outcomes are both common and important to avoid.The perspective of a panel of expert anesthesiologists? Anesth Analg. 1999;88:1085–91. doi: 10.1097/00000539-199905000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Hynynen M, Korttila K, Tammisto T. Pain on IV injection of propofol (ICI 35868) in emulsion formulation: Short communication. Acta Anaesthesiol Scand. 1985;29:651–2. doi: 10.1111/j.1399-6576.1985.tb02274.x. [DOI] [PubMed] [Google Scholar]
- 4.King SY, Davis FM, Wells JE, Murchinson DJ, Pryor PJ. Lidocaine for the prevention of pain due to injection of propofol. Anesth Analg. 1992;74:246–9. doi: 10.1213/00000539-199202000-00013. [DOI] [PubMed] [Google Scholar]
- 5.McCrirrick A, Hunter S. Pain on injection of propofol: The effect of injectate temperature. Anaesthesia. 1990;45:443–4. doi: 10.1111/j.1365-2044.1990.tb14329.x. [DOI] [PubMed] [Google Scholar]
- 6.Stokes DN, Robson N, Hutton P. Effect of diluting propofol on the incidence of pain on injection and venous sequelae. Br J Anaesth. 1989;62:202–3. doi: 10.1093/bja/62.2.202. [DOI] [PubMed] [Google Scholar]
- 7.McCulloch MJ, Lees NW. Assessment and modification of pain on injection with propofol (Diprivan) Anaesthesia. 1985;40:1117–20. doi: 10.1111/j.1365-2044.1985.tb10615.x. [DOI] [PubMed] [Google Scholar]
- 8.Ambesh SP, Dubey PK, Sinha PK. Ondansetron pretreatment to alleviate pain on propofol injection: A randomized, controlled, double-blind study. Anesth Analg. 1999;89:197–9. doi: 10.1097/00000539-199907000-00035. [DOI] [PubMed] [Google Scholar]
- 9.Tan CH, Onsiong MK, Kua SW. The effect of ketamine pretreatment on propofol injection pain in 100 women. Anaesthesia. 1998;53:296–304. doi: 10.1046/j.1365-2044.1998.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal A, Ansari MF, Gupta D, Pandey R, Raza M, Singh PK, et al. Pretreatment with thiopental for prevention of pain associated with propofol injection. Anesth Analg. 2004;98:683–6. doi: 10.1213/01.ane.0000103266.73568.18. [DOI] [PubMed] [Google Scholar]
- 11.Liaw WJ, Pang WW, Chang DP, Hwang MH. Pain on injection of propofol: The mitigating influence of metoclopramide using different techniques. Acta Anaesthesiol Scand. 1999;43:24–7. doi: 10.1034/j.1399-6576.1999.430106.x. [DOI] [PubMed] [Google Scholar]
- 12.Fletcher JE, Seavell CR, Bowen DJ. Pretreatment with alfentanil reduces pain caused by propofol. Br J Anaesth. 1994;72:342–4. doi: 10.1093/bja/72.3.342. [DOI] [PubMed] [Google Scholar]
- 13.Liljeroth E, Karlsson A, Lagerkranser M, Akeson J. Low dose propofol reduces the incidence of moderate to severe local pain induced by the main dose. Acta Anaesthesiol Scand. 2007;51:460–3. doi: 10.1111/j.1399-6576.2006.01255.x. [DOI] [PubMed] [Google Scholar]
- 14.Ye JH, Mui WC, Ren J, Hunt TE, Wu WH, Zbuzek VK. Ondansetron exhibits the properties of a local anesthetic. Anesth Analg. 1997;85:1116–21. doi: 10.1097/00000539-199711000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Akeson J. Pain on injection of propofol- why bother ?[editorial] Acta Anaesthesiol Scand. 2008;52:591–3. doi: 10.1111/j.1399-6576.2008.01628.x. [DOI] [PubMed] [Google Scholar]
- 16.Doenicke A, Roizen M, Rau J, Kellerman W, Babl J. Reducing pain during propofol injection: The role of the solvent. Anesth Analg. 1996;82:472–4. doi: 10.1097/00000539-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Nishiyama T. How to decrease pain at rapid injection of propofol: Effectiveness of flurbiprofen. J Anesth. 2005;19:273–6. doi: 10.1007/s00540-005-0331-3. [DOI] [PubMed] [Google Scholar]
- 18.Ohmizo H, Obara S, Iwama H. Mechanism of injection pain with long and long-medium chain triglyceride emulsive propofol. Can J Anaesth. 2005;52:595–9. doi: 10.1007/BF03015768. [DOI] [PubMed] [Google Scholar]
- 19.Ando R, Watanabe C. Characteristics of propofol-evoked vascular pain in anaesthetized rats. Br J Anaesth. 2005;95:384–92. doi: 10.1093/bja/aei184. [DOI] [PubMed] [Google Scholar]
- 20.Nathanson MH, Gajraj NM, Russell JA. Prevention of pain on injection of propofol: A comparison of lidocaine with alfentanyl. Anesth Analg. 1996;82:469–71. doi: 10.1097/00000539-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Lyons B, Lohan D, Flynn C, McCarroll M. Modification of pain on injection of propofol: A comparison of pethidine and lignocaine. Anaesthesia. 1996;51:394–5. doi: 10.1111/j.1365-2044.1996.tb07756.x. [DOI] [PubMed] [Google Scholar]
- 22.Valtonen M, Iisalo E, Kanto J, Rosenberg P. Propofol as an induction agent in children: Pain on injection and pharmacokinetics. Acta Anaesthesiol Scand. 1989;33:152–5. doi: 10.1111/j.1399-6576.1989.tb02879.x. [DOI] [PubMed] [Google Scholar]
- 23.Desmond PV, Watson KJ. Metoclopromide- a review. Med J Aus. 1986;144:366–9. doi: 10.5694/j.1326-5377.1986.tb115923.x. [DOI] [PubMed] [Google Scholar]
- 24.Albibi R, McCallum RW. Metoclopromide-Pharmacology and clinical application. Ann Int Med. 1983;93:86–95. doi: 10.7326/0003-4819-98-1-86. [DOI] [PubMed] [Google Scholar]
- 25.Mecklem DW. Propofol injection pain: Comparing the addition of lignocaine or metoclopramide. Anaesth Intensive Care. 1994;22:568–70. doi: 10.1177/0310057X9402200511. [DOI] [PubMed] [Google Scholar]
- 26.Hwang J, Park HP, Lim YJ, Do SH, Lee SC, Jeon YT. Preventing pain on injection of propofol: A comparison between peripheral ketamine pre-treatment and ketamine added to propofol. Anaesth Intensive Care. 2009:37584–7. doi: 10.1177/0310057X0903700404. [DOI] [PubMed] [Google Scholar]
- 27.Gregory RE, Ettinger DS. 5HT3 receptor antagonists for the prevention of chemotherapy-induced nausea and vomiting: A comparison of their pharmacology and clinical efficacy. Drugs. 1998;55:173–89. doi: 10.2165/00003495-199855020-00002. [DOI] [PubMed] [Google Scholar]
- 28.Porteous R. Pain-free intravenous injections [letter] Anaesthesia. 1987;42:1021. doi: 10.1111/j.1365-2044.1987.tb05391.x. [DOI] [PubMed] [Google Scholar]
- 29.Briggs LP, Clarke SJ, Dundee JW, Moore J, Bahar M, Wright PJ. Use of di-isopropyl phenol as main agent for short procedures. Br J Anaesth. 1981;53:1197–202. doi: 10.1093/bja/53.11.1197. [DOI] [PubMed] [Google Scholar]


