Abstract
Histoplasmosis, a systemic mycosis caused by the dimorphic fungus Histoplasma capsulatum var capsulatum and Histoplasma capsulatum var duboisii is endemic to many parts of the world. The clinical manifestations range from acute or chronic pulmonary infection to a progressive disseminated disease. After initial exposure to the fungus, the infection is self-limited and restricted to the lungs in 99% of healthy individuals. The remaining 1%, however, progress to either disseminated or chronic disease involving the lungs, liver, spleen, lymph nodes, bone marrow or rarely, the skin and mucous membranes. Mucocutaneous histoplasmosis is frequently reported in patients with acquired immune deficiency syndrome (AIDS), but it is rare in immunocompetent hosts. A 60-year-old male presented with asymptomatic swelling of the hard palate and crusted papules and nodules over the extremities, face and trunk. Clinically, the diagnoses of cutaneous cryptococcosis versus histoplasmosis was considered in this patient. A chest X-ray revealed hilar lymphadenopathy. Enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV) was nonreactive. Skin biopsy revealed multiple tiny intracellular round yeast forms with a halo in the mid-dermis. Culture of the skin biopsy in Sabouraud's dextrose agar showed colonies of Histoplasma capsulatum. Despite an investigation including no evidence of underlying immunosuppression was found, he was started on IV amphotericin-B (0.5 mg/kg/day). However, the patient succumbed to his disease 2 days after presentation. We report a rare case of disseminated cutaneous histoplasmosis in an immunocompetent individual.
Keywords: Histoplasmosis, histoplasma capsulatum, immunocompetent, mucocutaneous lesions
Introduction
Classic Histoplasmosis is also called Darling's disease.[1] It is a deep mycotic infection caused by one of two species. Histoplasma capsulatum is found in the Americas and the tropics, particularly the Ohio and Mississippi river valleys of North America.[2,3] Histoplasma dubosii is prevalent in Africa.[4] In India, endemic cases of histoplasmosis have been reported in West Bengal (eastern India)[2,3] and sporadic cases have been reported in southern India.[5,6] Further reports of histoplasmosis in nonendemic regions is very rare.[7]
The spores of this saprophyte are found in soil and bird droppings.[8,9] Pulmonary histoplasmosis and disseminated histoplasmosis involving the skin is very common in patients with advanced acquired immune deficiency syndrome (AIDS). It can be a major cause of morbidity and mortality for these patients.[10] Although histoplasmosis occurs most commonly in immunosuppressed patients,[11] there are a few case reports of this disease in immunocompetent hosts.[12,13] We hereby report a case of disseminated histoplasmosis in an immunocompetent individual from a nonendemic region of central India.
Case Report
A 60-year-old male farmer, resident of Barhanpur (Madhya Pradesh, India), presented with a noduloulcerative growth on the hard palate. He complained of difficulty swallowing for 6 months. He also had numerous skin colored papules and nodules on his head, trunk, and extremities for the past 5 months. He reported that the lesion on the palate started as a small swelling which increased in size over a period of 6 months and then ulcerated. One month after the onset of the oral lesion, he developed a generalized eruption of painful small elevated skin colored papules and nodules. Some of these lesions increased in size and ulcerated.
He had a persistent low-grade fever, weight loss, productive cough and shortness of breath for 1 month prior to presentation. On inquiry, he gave history of frequenting caves and forts with other tourists in the area around his home, but there was no history of travel to other parts of India or abroad. He had no history of unprotected sexual exposure, diabetes mellitus, or tuberculosis.
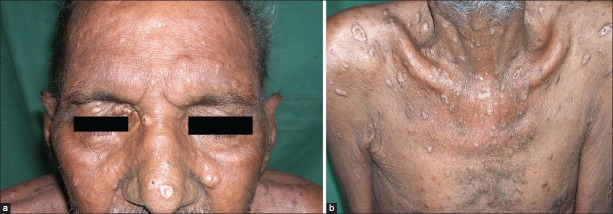
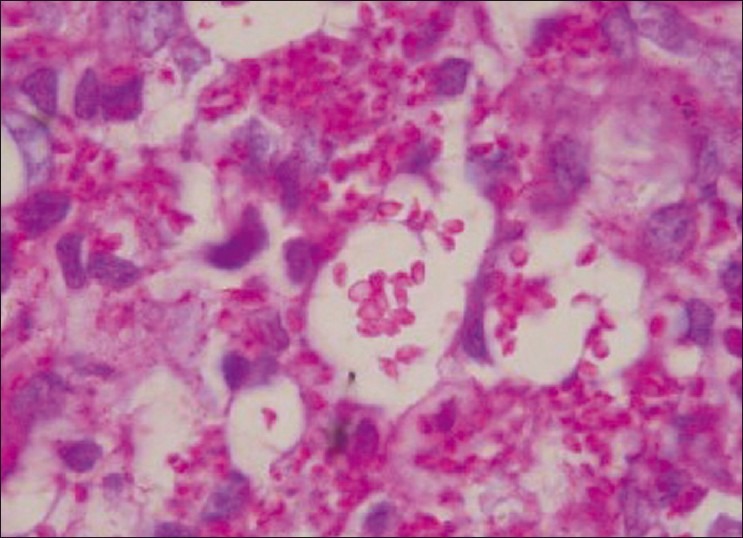
He was a chronic alcoholic and a smoker. Physical examination revealed an undernourished, ill-appearing cachectic man with pallor, significant generalized lymphadenopathy, and generalized xerosis. Systemic examination was normal. Cutaneous examination revealed multiple skin-colored umbilicated papules and nodules ranging in size from 0.5 to 1.5 cm distributed on the scalp, face, neck, trunk, upper and lower extremities. A few of these lesions had a hemorrhagic crust [Figures 1a–b]. There was an irregularly shaped, firm ulcerated nodule on the hard palate, about 2 × 2 × 0.5 cm3 [Figure 2]. Routine hematological parameters were normal except ESR was 50 mm/h and a chest X-ray revealed bilateral hilar lymphadenopathy. enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV) was nonreactive. His CD4 count was normal at 720/mm3. Pathology of oral and skin biopsies showed multiple tiny intracellular round yeast forms surrounded by a halo on PAS and GMS staining [Figures 3a–c]. Fine needle aspiration cytology (FNAC) of an inguinal lymph node revealed macrophages containing intracytoplasmic, oval, noncapsulated yeast cells. Culture from the skin tissue specimen grew white cottony colonies suggestive of Histoplasma capsulatum [Figure 4]. A test for dimorphism was conclusive for histoplasmosis [Figure 5]. The patient was treated with Itraconazole 400 mg/day for 4 weeks. However, he presented after completing 4 weeks of therapy with new skin lesions, persistent fever, productive cough and dyspnea. On systemic examination, there is decreased air entry on right side with crepitation on further investigation, a chest X-ray showed consolidation of right middle lobe and pleural effusion. He was started on intravenous amphotericin-B (0.5 mg/kg/day). However, the patient succumbed to his disease 2 days later from cardiorespiratory failure.
Figure 1.
(a-b) Multiple skin-colored papules and nodules over the chest and face
Figure 2.

Irregular firm and indurated nodular growth on the hard palate
Figure 3a.
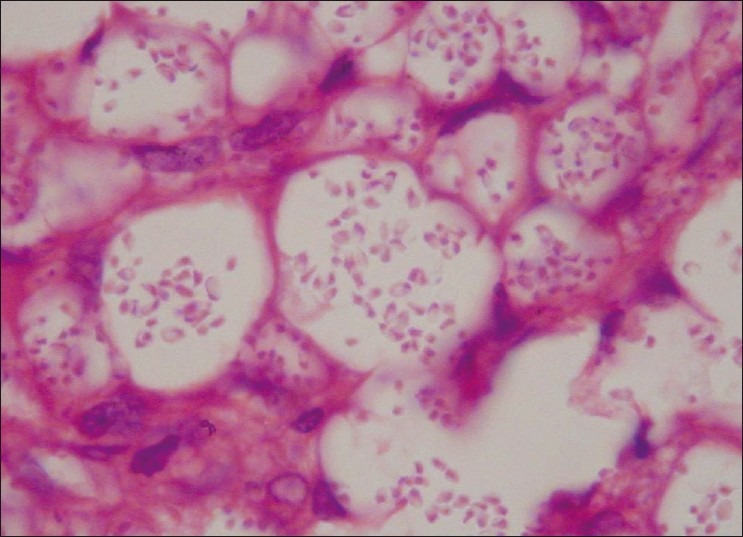
Multiple intracellular rounded yeasts surrounded with the halo in dermis, ×400 H and E
Figure 3c.
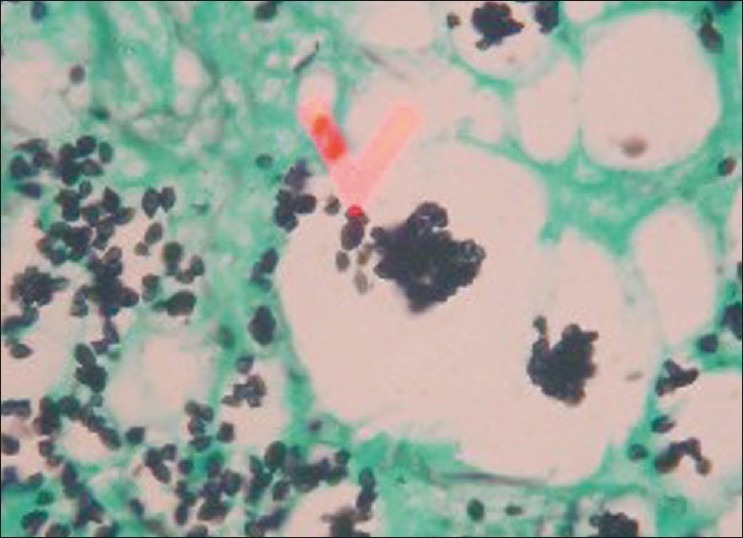
Multiple intracellular rounded yeasts surrounded with the halo in dermis, ×400 GMS (3c)
Figure 4.

Culture from the skin tissue specimens grew white cottony colonies of histoplasmosis
Figure 5.

Test of dimorphism was positive suggestive of Histoplasma capsulatum
Figure 3b.
Multiple intracellular rounded yeasts surrounded with the halo in dermis, ×400 PAS stain(3b)
Discussion
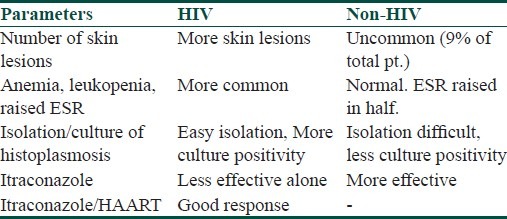
Disseminated histoplasmosis is rare in the immunocompetent host. Histoplasmosis is an uncommon disease caused by Histoplasma capsulatum var capsulatum and Histoplasma capsulatum var duboisii.[14,15] In India, histoplasmosis is rare, as it is thought to be endemic only in small regions in West Bengal in western India.[2,3] However, sporadic cases from southern India are frequently reported. Our patient was a resident of a nonendemic region of central India,[7] but frequented many caves and forts that are often inhabited by bats.[16] We believe that our patient contracted the disease via inhalation of conidia of Histoplasma capsulatum present in the soil contaminated by excreta of bats or birds.[16] Inhalation of either fungal conidia or mycelial fragments is the primary mode of infection for histoplasmosis. Once inhaled, these fungal elements transform into yeast forms and may disseminate systemically. Primary pulmonary histoplasmosis in the vast majority (approximately 90%) of cases is asymptomatic or presents with subclinical disease.[17,18] Symptomatic hosts with primary pulmonary histoplasmosis often present with nonspecific symptoms of fever, chest pain and cough that are self limited. Immunocompetent hosts are able to control and limit infections of Histoplasma; however, hosts with defective cell-mediated immunity, including patients with hematolymphoid malignancies, solid-organ transplants, and those exposed to chemotherapeutic and immunosuppressive agents, are at risk of developing progressive disseminated histoplasmosis involving the reticuloendothelial system, including the liver, spleen, kidney, lymph nodes, bone marrow and mucocutaneous tissues. It is also recognized as an AIDS-defining illness.[17] Histoplasmosis infection is often categorized as being present in an HIV positive or HIV negative individual, as there are differences in presentation and response to therapy. The major differences are enlisted in Table 1.
Table 1.
Differences between histoplasmosis in HIV and non-HIV patients
Mucocutaneous histoplasmosis is frequently reported in AIDS patients,[19] but when it is rarely reported in immunocompetent individuals.[20] it is usually associated with the severe disseminated form of histoplasmosis.[21] Disseminated histoplasmosis with oral involvement in an immunocompetent patient has rarely been described around the world.[22] We present a case of chronic disseminated histoplasmosis in a HIV negative, chronic alcoholic, without other evidence of underlying disease. Only a few cases of disseminated histoplasmosis are reported in immunocompetent individuals.[20]
Frequently, in cases of disseminated infection, such oral lesions appear as the initial clinical manifestation. Mucocutaneous histoplasmosis in patients without detectable systemic involvement has been reported.[22] Oral lesions can manifest in a variety of forms, such as ulcers, erythematous or vegetative nodules or wart-like growths. Many reports show development of ulcerating, indurated, and painful ulcers.[23] The palate, gingival, and oropharynx are the most frequent sites of oral histoplasmosis. In nodular or noduloulcerative oral lesions, the differential diagnosis should include squamous cell carcinoma, lymphoma, and other systemic mycoses, in addition to histoplasmosis, irrespective of immune status of the patient. Histoplasmosis should be especially suspected when cutaneous lesions are also present. Our case highlights the occurrence of disseminated histoplasmosis in an immunocompetent patient.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Hay RJ, Moore M. Mycology. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook/Wilkinson/Ebling Textbook of dermatology. 6th ed. Oxford: Oxford Blackwell Science; 1998. pp. 1363–6. [Google Scholar]
- 2.Sanyal M, Thammaya Skin sensitivity to histoplasmin in Calcutta and its neighborhood. Indian J Dermatol Venereol Leprol. 1980;46:94–8. [PubMed] [Google Scholar]
- 3.Mukherjee AM, Khan KP, Sanyal M, Basu N. Histoplasmosis in India with report of two cases. J Ind Med Assoc. 1971;56:121–5. [PubMed] [Google Scholar]
- 4.Gugnani HC. Histoplasmosis in Africa Indian. J Chest Dis Allied Sci. 2000;42:271–7. [PubMed] [Google Scholar]
- 5.Saoji AM, Grover S, Mene AR, Patoria NK, Sharma KD. Histoplasmosis. J Indian Med Assoc. 1976;66:37–8. [PubMed] [Google Scholar]
- 6.Nair SP, Vijayadharan M, Vincent M. Primaty cutaneous histoplasmosis. Indian J Dermatol Venereol Leprol. 2000;66:151–3. [PubMed] [Google Scholar]
- 7.Taylor GD, Fanning EA, Ferguson JP. Disseminated histoplasmosis in a Nonendemic area. Can Med Assoc J. 1985;33:763–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Radhakrishnan S, Vanchilingam S, Subramaniam S, Venkatraman IT. Acute disseminated histoplasmosis with unusual features. An autopsy report. J Assoc Phys India. 1982;30:45–8. [PubMed] [Google Scholar]
- 9.Rippon JW. The Pathogenic fungi and the pathogenic actinomycetes. 3rd ed. Philadelphia: WB Saunders; 1988. pp. 381–417. [Google Scholar]
- 10.Kalter CD, Tschen JA, Klima N. Maculopapular rash in a patient with acquired immunodeficency syndrome. Arch Dermatol. 1985;121:1454–7. [PubMed] [Google Scholar]
- 11.Sayal SK, Prasad PS, Sanghi S. Disseminated histoplasmosis: Cutaneous presentation. Indian J Dermatol Venereol Leprol. 2003;69:90–1. [Google Scholar]
- 12.Sharma S, Kumari N, Ghosh P, Aggarwal A. Disseminated histoplasmosis in an immunocompetent individual-a case report. Indian J Pathol Microbiol. 2005;48:204–6. [PubMed] [Google Scholar]
- 13.Alcure ML, Di Hipólito Júnior O, Almeida OP, Bonilha H, Lopes MA. Oral histoplasmosis in an HIV-negative patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:33–6. doi: 10.1016/j.tripleo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 14.Mendell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingstone Inc; 1995. [Google Scholar]
- 15.Tewari RP, Wheat LJ, Ajello L. Agents of histoplasmosis. In: Ajello L, Hay J, editors. Topley and Wison's Microbiology and Microbial Infections. 9th ed. Vol. 4. London: Arnold; 1998. pp. 373–93. [Google Scholar]
- 16.Nygård K, Brantsaeter A, Feruglio S, Ravn J, Dotevall L, Hasle G, et al. Histoplasmosis among travellers to Central America. Tidsskr Nor Laegeforen. 2006;126:2838–42. [PubMed] [Google Scholar]
- 17.O’Hara CD, Allegretto MW, Taylor GD, Isotalo PA. Epiglottic histoplasmosis presenting in a nonendemic region: a clinical mimic of laryngeal carcinoma. Arch Pathol Lab Med. 2004;128:574–7. doi: 10.5858/2004-128-574-EHPIAN. [DOI] [PubMed] [Google Scholar]
- 18.Severo LC, Oliveira FM, Irion K, Porto NS, Londero AT. Histoplasmosis in Rio Grande do Sul, Brazil: a 21-year experience. Rev Inst Med Trop S. Paulo. 2001;43:183–187. doi: 10.1590/s0036-46652001000400001. [DOI] [PubMed] [Google Scholar]
- 19.Rocha MM, Severo LC. Disseminated histoplasmosis in patients with acquired immunodeficiency syndrome (AIDS). Study of 25 cases. Rev Inst Med Trop Sao Paulo. 1994;36:167–70. [PubMed] [Google Scholar]
- 20.Souza Filho FJ, Lopen M, Almeida OP, Scully C. Mucocutaneous histoplasmosis in AIDS. Br J Dermatol. 1995;33:472–4. doi: 10.1111/j.1365-2133.1995.tb02681.x. [DOI] [PubMed] [Google Scholar]
- 21.Cobb CM, Shultz RE, Brewer JH, Dunlap CL. Chronic pulmonary histoplasmosis with an oral lesion. Oral Surg Oral Med Oral Pathol. 1989;67:73–76. doi: 10.1016/0030-4220(89)90305-8. [DOI] [PubMed] [Google Scholar]
- 22.Mignogna MD, Fedele S, Lo Russo L, Ruoppo E, Lo Muzio L. A case of oral localized histoplasmosis in an immunocompetent patient. Eur J Clin Microbiol Infect Dis. 2001;20:753–5. doi: 10.1007/s100960100592. [DOI] [PubMed] [Google Scholar]
- 23.Coiffier T, Roger G, Beust L, Quinet B, Adam D, Dupont B, et al. Pharyngo-laryngeal histoplasmosis: one case in an immunocompetent child. Int J Pediatr Otorhinolaryngol. 1998;45:177–81. doi: 10.1016/s0165-5876(98)00099-8. [DOI] [PubMed] [Google Scholar]